Abstract
Background
Paclitaxel (PTX) resistance is a main obstacle for the treatment of triple-negative breast cancers (TNBC). Evidences have shown that miR-153-5p could induce the apoptosis of breast cancer cells. Thus, this study aimed to investigate the effect of miR-153-5p on PTX-resistance TNBC cells.
Methods
Cell Counting Kit-8, flow cytometry and wound healing assays were used to detect the viability, apoptosis and migration of MDA-MB-231/PTX cells, respectively. The luciferase reporter assay was used to explore the potential binding targets of miR-153-5p. The expressions of CDK1, cyclin B1 and p-Akt in MDA-MB-231/PTX cells were detected with Western blot. In vivo animal study was performed finally.
Results
In this study, the inhibitory effects of PTX on the proliferation and migration of MDA-MB-231/PTX cells were significantly enhanced following transfection with miR-153-5p. In addition, overexpression of miR-153-5p markedly enhanced the pro-apoptotic effect of PTX on MDA-MB-231/PTX cells. Luciferase reporter assay validated that cyclin-dependent kinase 1 (CDK1) was a potential binding target of miR-153-5p. Moreover, overexpression of miR-153-5p prominently increased PTX-induced cell cycle arrest at G2/M phase in MDA-MB-231/PTX cells via downregulation of CDK1, cyclin B1 and p-Akt. In vivo experiments confirmed that overexpression of miR-153-5p notably enhanced PTX sensitivity in MDA-MB-231/PTX xenograft model.
Conclusion
We found that overexpression of miR-153-5p could reverse PTX resistance in PTX-resistant TNBC cells via inducing G2/M phase arrest, indicating that miR‑153-5p may be a promising agent for patients with PTX-resistant TNBC.
Keywords: triple-negative breast cancer, paclitaxel, miR-153-5p, CDK1, cell cycle
Introduction
Breast cancer is the most common type of malignant cancer in women worldwide.1 Breast cancer is a complex and heterogeneous disease, which is comprised of molecularly various subtypes.2 The four subtypes of breast cancer are luminal A, luminal B, HER2 positive and triple-negative breast cancers (TNBC), depending on the expressions of estrogen receptor (ER), progesterone receptor (PR), and epidermal growth factor receptor 2 (HER2) in tumor.2,3 TNBC is the most aggressive form of breast cancer, which is defined as lacking expressions of the ER, PR and HER2.4 In addition, TNBC is characterized by lack of effective targeted therapies and a worse prognosis.5 Moreover, the chemo-resistance of TNBC is the primary cause leading to the recurrence of disease and ultimate death.6 Paclitaxel (PTX) is used as a common chemotherapeutic drug for the treatment of multiple solid tumors, such as breast cancer and ovarian cancer.7,8 However, drug resistance is a great obstacle, which notably limit the clinical usage of PTX.9 Therefore, explore novel treatment approaches to prevent drug resistance during chemotherapy are important for patient with TNBC.
MicroRNAs (miRNAs) are a class of endogenous non-coding RNAs of ~21 nucleotides in length, which could regulate target gene expression via targeting the 3′ untranslated region (UTR) of the target genes.10,11 In addition, miRNAs play important roles in a number of biological processes including differentiation, apoptosis, proliferation and tumorigenesis.12 Moreover, miRNAs function as tumor inhibitor genes or oncogenes, and exhibit a vital role in the progression of TNBC.13,14 Wu et al revealed that miR-153-5p could induce the apoptosis of breast cancer cells through targeting HECTD3.15 However, the biological function of miR-153-5p in PTX-resistance TNBC cells remains unclear. In this study, we aimed to investigate the underlying mechanisms of miR-153-5p in regulating the sensitivity of TNBC cells to PTX.
Materials and Methods
Cell Culture
Human normal breast epithelial cell line MCF10A and human breast cancer cell line MDA-MB-231 were purchased from Type Culture Collection of the Chinese Academy of Sciences (Shanghai, China). PTX-resistant cell line (MDA-MB-231/PTX) was established by continuous exposure of MDA-MB-231 cells to a stepwise gradually concentration of PTX for more than 3 months, as previously described.16 Cells were maintained in Dulbecco’s Modified Eagle medium (DMEM, Thermo Fisher Scientific, Waltham, MA, USA) with 10% heat-inactivated fetal bovine serum (Thermo Fisher Scientific) containing penicillin-streptomycin (Sigma Aldrich, St. Louis, MO, USA), and incubated at 37°C in a humidified atmosphere containing 5% CO2.
CCK-8 Assay
The proliferation of MDA-MB-231, MDA-MB-231/PTX and MCF10A cells was examined using the Cell Counting kit-8 (CCK-8, Dojindo, Kumamoto, Japan). Cells were plated onto 96-well culture plates at a density of 5 × 103 cells. Cell proliferation was measured at 72 h using CCK-8 reagent at 37°C according to manufacturer’s instruction. The absorbance was detected at 450 nm using a microplate reader (BioTek, Winooski, VT, USA).
Cell Transfection
MiR-153-5p agonist and agonist negative control (agonist NC) were obtained from GenePharma (Shanghai, China). The miR-153-5p agonist and agonist NC were transfected into MDA-MB-231 cells with Lipofectamine 2000 (Thermo Fisher Scientific) according to the manufacturer’s protocol.
Reverse Transcription-Quantitative PCR (RT-qPCR)
The total RNA from cells was extracted using the TRIzol reagent (Thermo Fisher Scientific). Reverse transcription was performed using EntiLink™ 1st Strand cDNA Synthesis Kit (ELK Biotechnology, Wuhan, China). For CDK1 determination, cDNA was synthesized using the RNA PCR Kit (Takara Bio Inc. Shiga, Japan). Then, real-time quantitative PCR was performed using the EnTurbo™ SYBR Green PCR SuperMix kit (ELK Biotechnology) on a StepOne™ Real-Time PCR system (Thermo Fisher Scientific). The levels of miR-153-5p and CDK1 mRNA were normalized to U6 and actin, respectively, and calculated using the 2−ΔΔCt method. The primer sequences were described in Supplementary Table 1.
Flow Cytometry Analysis
For cell apoptosis assay, Annexin V–fluorescein isothiocyanate (FITC) apoptosis detection kit (Thermo Fisher Scientific) was used to detect cell apoptosis. MDA-MB-231/PTX cells were washed twice with pre-cold PBS, and then stained with 5 μL of Annexin V-FITC and 5 μL of propidium Iodide (PI) in the dark for 30 min. Apoptosis rate was determined by a flow cytometer (BD FACSCanto II, BD Bioscience, Franklin Lake, NJ, USA).
For cell cycle assay, MDA-MB-231/PTX cells were washed twice with pre-cold PBS, and then stained with PI solution in the dark for 30 min. Cell cycle distribution was determined by a flow cytometer (BD Bioscience).
Western Blot Assay
Total protein was quantified using BCA method (Beyotime Institute of Biotechnology, Beijing, China). Equal proteins (30 μg per lane) were electrophoresed on 10% SDS-PAGE, and then transferred onto polyvinylidene difluoride (PVDF) membranes (Millipore, Billerica, MA, USA). The membrane was then blocked in 5% skimmed milk in TBST at room temperature for 1 h. After that, the membrane was incubated in primary antibodies against Bax (1:1000, Abcam), Bcl-2 (1:1000, Abcam), cleaved caspase 3 (1:1000, Abcam), CDK1 (1:1000, Abcam), cyclin B1 (1:1000, Abcam), p-Akt (1:1000, Abcam), Akt (1:1000, Abcam), and anti-β-actin (1:1000, Abcam) at 4°C overnight. Later on, the membranes were incubated with the secondary antibody (1:5000 Abcam) at room temperature for 1 h. Finally, the membrane was visualized using an electrochemiluminescence (Thermo Fisher Scientific). β-actin was acted as the internal control.
Wound Healing Assay
MDA-MB-231/PTX cells (2×105 cells per well) were seeded onto a 12-well culture plate overnight at 37°C. At 80% confluence, a wound area was generated with a 20 μL pipette tip. After that, cells were transfected with 10 nM miR-153-5p agonist for 48 h at 37°C. Then, cells were imaged at 0 h and 48 h using the fluorescence microscope (Olympus CX23 Tokyo, Japan), and the wound closure was conducted on an ImageJ software.
Dual-Luciferase Reporter Assay
The 3′-UTR sequences of CDK1 containing the predicted wild-type (WT) or mutant (MT) miR-153-5p binding sequences were ligated into the psiCHECK-2 vector (Promega, Madison, WI, USA). PsiCHECK-2-WT-CDK1-3′-UTR or psiCHECK-2-MT-CDK1-3′-UTR was co-transfected with miR-153-5p agonist in MDA-MB-231/PTX cells using Lipofectamine 2000 (Thermo Fisher Scientific). The luciferase activity in cell lysate was detected at 48 h using Dual-Luciferase Reporter Assay System (Promega Madison, WI) according to the manufacturer’s protocol with renilla luciferase activity as endogenous control.
Animal Study
4-6-weeks old BALB/c nude mice were purchased from the Shanghai SLAC Animal Center (Shanghai, China) and were randomized into four groups (n = 7): blank, PTX, miR-153-5p agonist group and PTX + miR-153-5p agonist group. 1 × 107 MDA-MB-231/PTX cells (in 100 μL of PBS) were injected subcutaneously into the left flank of nude mice. When the tumors reach about 100 mm3, 50 nM miR-153-5p agonist was directly injected into the tumors twice a week. Tumor volume was monitored every week with a caliper and tumor size was calculated using the formula V = (length x width2)/2 (Width < Length). After 28 days of treatment, mice were sacrificed, and the entire tumors were weighed. All animal experiments were approved by the Institutional Ethical Committee of Weifang People’s Hospital, and animals were maintained following the guidelines of the Institutional Animal Care and Use Committee.
Statistical Analysis
All data were repeated in triplicate. Data are presented as the mean ± standard deviation (S.D.). All statistical analyses were performed using GraphPad Prism software (version 7.0, La Jolla, CA, USA). One-way analysis of variance (ANOVA) and Tukey’s tests were carried out for multiple group comparisons. The results were considered significant at *P < 0.05.
Results
Overexpression of miR-153-5p Enhanced the Cytotoxic Effect of PTX in PTX-Resistant TNBC Cells
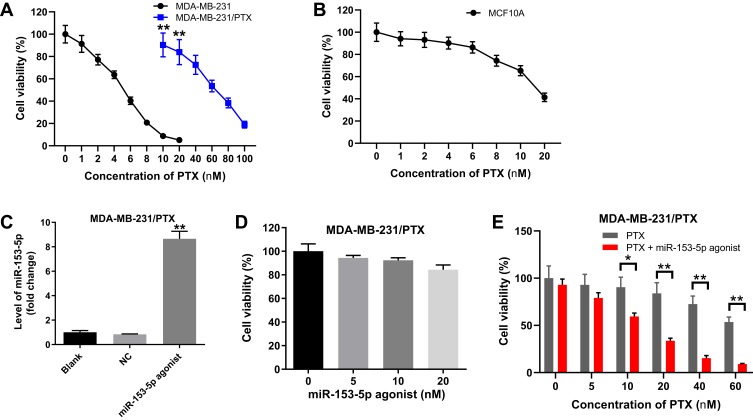
To determine the effects of PTX on the viability of PTX-sensitive or -resistance TNBC cells, CCK-8 assay was applied. As shown in Figure 1A, PTX inhibited the viability of MDA-MB-231 cells in a dose-dependent manner (IC50 value: 4.10 nM). In addition, PTX inhibited the viability of MCF10A cells (IC50 value: 17.92 nM), indicating that TNBC cell line MDA-MB-231 was more sensitive to PTX compared with normal breast epithelial cell line MCF10A (Figure 1B). Furthermore, PTX suppressed the cell viability of MDA-MB-231/PTX cells dose-dependently, and IC50 value of PTX was 61.38 nM in MDA-MB-231/PTX cells (Figure 1A). The IC50 value of PTX in MDA-MB-231/PTX cells were 14.97-fold greater than that in MDA-MB-231 cells, which confirmed that MDA-MB-231/PTX cells were resistant to PTX compared with MDA-MB-231 parental cells.
Figure 1.
Overexpression of miR-153-5p enhanced the cytotoxic effect of PTX in PTX-resistant TNBC cells. (A) MDA-MB-231 and MDA-MB-231/PTX cells were treated with 0, 1, 2, 4, 6, 8 10 or 20 nM PTX for 72 h, respectively. CCK-8 assay was used to detect the viability of MDA-MB-231 or MDA-MB-231/PTX cells. **P < 0.01, compared with the MDA-MB-231 group. (B) MCF10A cells were treated with 0, 1, 2, 4, 6, 8 10 or 20 nM PTX for 72 h, respectively. CCK-8 assay was used to detect the cell viability. (C) MDA-MB-231/PTX cells were transfected with miR-153-5p agonist for 72 h. RT-qPCR was applied to measure the level of miR-153-5p in cells. **P < 0.01, compared with the NC group. (D) MDA-MB-231/PTX cells were transfected with miR-153-5p agonist (0, 5, 10 or 20 nM) for 72 h. CCK-8 assay was used to detect the cell viability. (E) MDA-MB-231/PTX cells were treated with miR-153-5p agonist (0, 10 nM) plus different concentrations of PTX (0, 5, 10, 20, 40, 60 nM) for 72 h. CCK-8 assay was used to detect the cell viability. *P < 0.05, **P < 0.01, compared with the PTX group.
Abbreviations: PTX, paclitaxel; NC, negative control; TNBC, triple-negative breast cancers; CCK-8, Cell Counting Kit-8.
Next, to investigate the role of miR-153-5p in PTX-resistance TNBC cells, miR-153-5p agonist was used. As indicated in Figure 1C, overexpression of miR-153-5p significantly upregulated the level of miR-153-5p in MDA-MB-231/PTX cells, compared with NC group. In addition, miR-153-5p agonist (5, 10, 20 nM) had very limited effect on the viability of MDA-MB-231/PTX cells (Figure 1D). When MDA-MB-231/PTX cells were treated with PTX combined with miR-153-5p agonist (10 nM), the IC50 value of PTX was decreased to 13.67 nM in (Figure 1E). Meanwhile, the viability of MDA-MB-231/PTX cells treated with (10 or 20 nM) PTX was about 90% and 84%, which decreased to 60% and 34% in the presence of 10 nM miR-153-5p agonist. In addition, combination of miR-153-5p agonist with 20 nM PTX exhibited higher cytotoxicity in MDA-MB-231/PTX cells. Therefore, 20 nM PTX was utilized in the following experiments. These data indicated that overexpression of miR-153-5p could enhance the cytotoxic effect of PTX in MDA-MB-231/PTX cells.
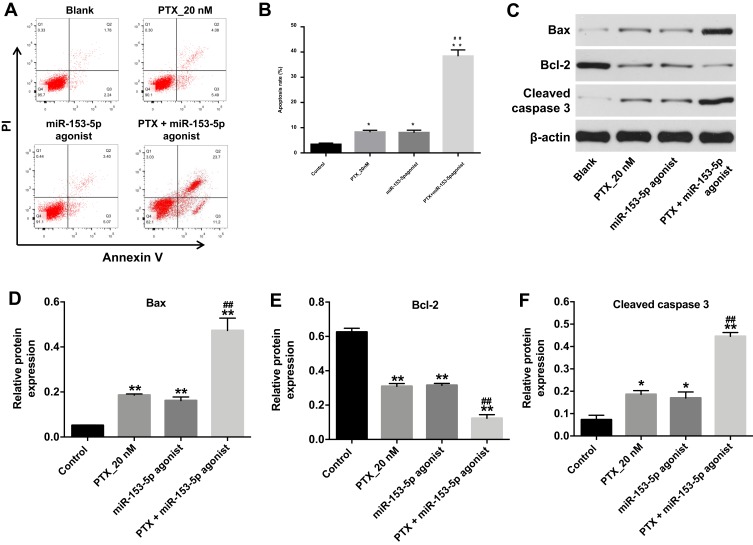
Overexpression of miR-153-5p Enhanced the Pro-Apoptotic Effect of PTX in PTX-Resistant TNBC Cells
To investigate the effect of miR-153-5p and PTX on the apoptosis of PTX-resistant TNBC cells, flow cytometric assay was used. As indicated in Figure 2A and B, PTX treatment or miR-153-5p agonist led to a marked increase in cell apoptosis. As expected, combination of PTX with miR-153-5p agonist induced a substantial fraction of apoptosis in MDA-MB-231/PTX cells, compared with PTX treatment group (Figure 2A and B). In addition, combination treatment significantly upregulated the expressions of pro-apoptotic proteins Bax and cleaved caspase 3, but markedly downregulated the level of anti-apoptotic protein Bcl-2 in MDA-MB-231/PTX cells, compared with PTX treatment group (Figure 2C–F). These data indicated that overexpression of miR-153-5p could enhance the pro-apoptotic effect of PTX in MDA-MB-231/PTX cells.
Figure 2.
Overexpression of miR-153-5p enhanced the pro-apoptotic effect of PTX in PTX-resistant TNBC cells. MDA-MB-231/PTX cells were treated with PTX (20 nM) or/and miR-153-5p agonist (10 nM) for 72 h. (A, B) Apoptotic cells were detected with Annexin V and PI double staining. (C) Expression levels of Bax, Bcl-2 and cleaved caspase 3 in MDA-MB-231/PTX cells were detected with Western blotting. (D, E, F) The relative expressions of Bax, Bcl-2 and cleaved caspase 3 in cells were quantified via normalizing to β-actin. *P<0.05, **P<0.01 compared with control group; ##P<0.01 compared with PTX_20 nM group.
Abbreviations: PI, propidium iodide; PTX, paclitaxel; Bax, BCL2-associated X; Bcl-2, B-cell lymphoma 2; TNBC, triple-negative breast cancers.
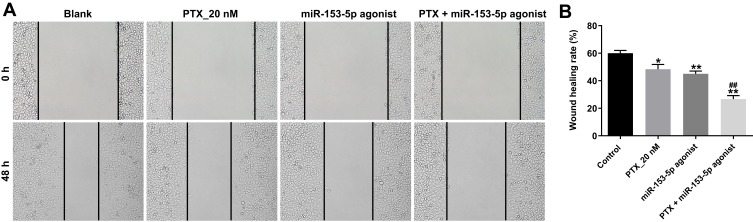
Overexpression of miR-153-5p Enhanced the Anti-Migratory Effect of PTX in PTX-Resistant TNBC Cells
Next, the effect of miR-153-5p agonist combined with PTX on cell migration was detected with wound healing assay. As shown in Figure 3A and B, PTX significantly inhibited the migration ability of MDA-MB-231/PTX cells and anti-migration effect to PTX was further enhanced following transfection with miR-153-5p agonist. These data suggested that overexpression of miR-153-5p could enhance the inhibitory effect of PTX on the migration of MDA-MB-231/PTX cells.
Figure 3.
Overexpression of miR-153-5p enhanced the anti-migratory effect of PTX in PTX-resistant TNBC cells. MDA-MB-231/PTX cells were treated with PTX (20 nM) or/and miR-153-5p agonist (10 nM) for 48 h. (A, B) Cell migration ability was assessed with wound healing assay. *P<0.05, **P<0.01 compared with control group; ##P<0.01 compared with PTX_20 nM group.
Abbreviations: PTX, paclitaxel; TNBC, triple-negative breast cancers.
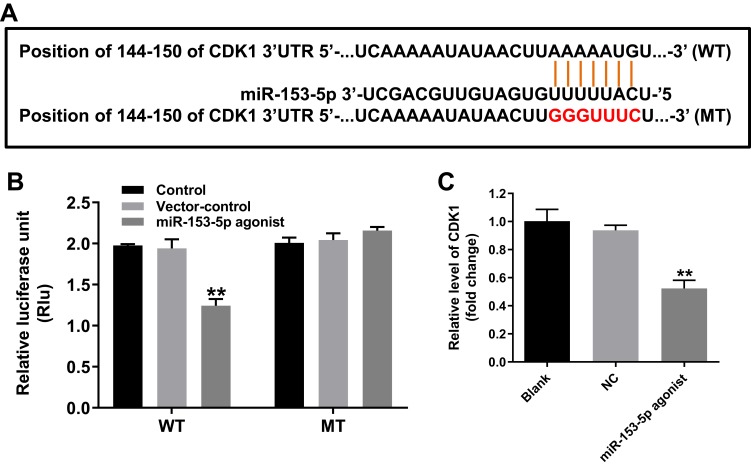
CDK1 Was a Directly Binding Target of miR-153-5p
TargetScan dataset (http://www.targetscan.org/vert_71/) was performed to predict the potential binding target of miR-153-5p. The data revealed that CDK1 might be a potential binding target of miR-153-5p (Figure 4A). In addition, dual-luciferase reporter assay validated that luciferase activity was obviously lower in MDA-MB-231/PTX cells following co-transfected with the WT-CDK1 segment and miR-153-5p agonist, compared to vector-control group (Figure 4B). Moreover, overexpression of miR-153-5p significantly decreased the level of CDK1 in MDA-MB-231/PTX cells, compared with NC group (Figure 4C). These results illustrated that CDK1 was a direct binding target of miR-153-5p.
Figure 4.
CDK1 was a direct binding target of miR-153-5p. (A) The 3ʹ‐UTR of CDK1 harbors miR-153-5p cognate sites. (B) Relative luciferase activity of reporter plasmids carrying WT- or MT-CDK1 3ʹ‐UTR in MDA-MB-231/PTX cells following co‐transfecting with miR-153-5p was detected using dual-luciferase reporter assay. (C) MDA-MB-231/PTX cells were transfected with miR-153-5p for 72 h. RT-qPCR was applied to measure the level of CDK1 in cells. **P<0.01 compared with vector-control group.
Abbreviations: WT, wild-type; MT, mutant; NC, negative control.
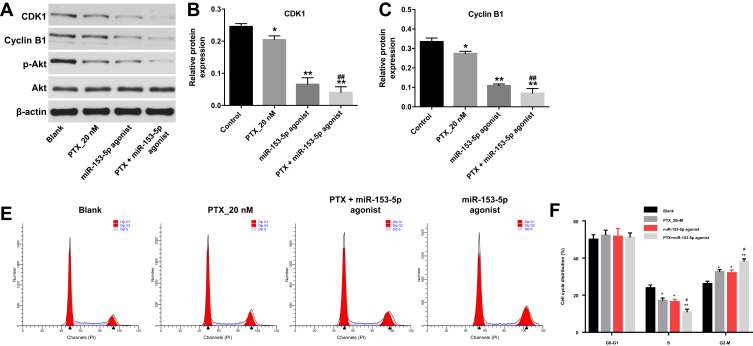
Overexpression of miR-153-5p Enhanced the Sensitivity of MDA-MB-231/PTX Cells to PTX via Inducing Cell Cycle Arrest
To explore the mechanism by which miR-153-5p regulated PTX resistance in TNBC, the expressions of CDK1, cyclin B1 and p-Akt were detected by Western blotting assay. As indicated in Figure 5A–D, PTX alone treatment significantly downregulated the expressions of CDK1, cyclin B1 and p-Akt in MDA-MB-231/PTX cells. These proteins expressions were further decreased following transfection with miR-153-5p agonist. In addition, flow cytometry assay indicated that combination of PTX with miR-153-5p agonist caused significant S phase decrease in MDA-MB-231/PTX cells, and inhibited DNA replication activity (Figure 5E and F). Meanwhile, combination treatment markedly induced G2/M phase arrest in MDA-MB-231/PTX cells, compared with PTX treatment group (Figure 5E and F). These data indicated that overexpression of miR-153-5p could enhance the sensitivity of MDA-MB-231/PTX cells to PTX via inducing G2/M arrest.
Figure 5.
Overexpression of miR-153-5p enhanced the sensitivity of MDA-MB-231/PTX cells to PTX via inducing cell cycle arrest. MDA-MB-231/PTX cells were treated with PTX (20 nM) or/and miR-153-5p agonist (10 nM) for 72 h. (A) Expression levels of CDK1, cyclin B1 and p-Akt in MDA-MB-231/PTX cells were detected with Western blotting. (B, C, D) The relative expressions of CDK1, cyclin B1 and p-Akt in cells were quantified via normalization to β-actin. (E, F) Flow cytometry was used to determine cell cycle distribution. *P<0.05, **P<0.01 compared with control group; #P<0.05, ##P<0.01 compared with PTX_20 nM group.
Abbreviations: PTX, paclitaxel; CDK1, cyclin-dependent kinase 1; Akt, protein kinase B; p-Akt, phosphorylation of Akt; G0-G1, Gap 0-Gap 1; S, synthesis, G2-M, Gap 2-mitosis, PI, propidium iodide.
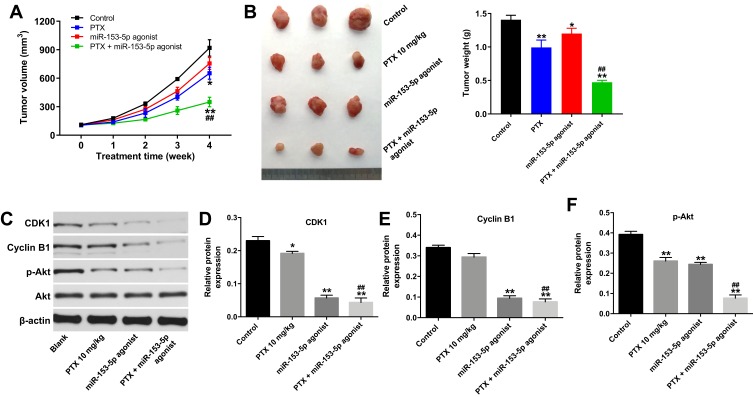
Overexpression of miR-153-5p Enhanced the Sensitivity of MDA-MB-231/PTX Cells to PTX in vivo
Next, we further investigate the effect of PTX combined with miR-153-5p agonist in xenograft model of MDA-MB-231/PTX. As revealed in Figure 6A and B, and supplementary Figure 1, PTX treatment slightly reduced the tumor volume and tumor weight, compared with control group. As expected, combination of PTX with miR-153-5p agonist markedly decreased the tumor volume and tumor weight, compared with PTX treatment group. In addition, combination treatment significantly downregulated the expressions of CDK1, cyclin B1 and p-Akt in tumor tissues, compared with PTX treatment group (Figure 6C–F). These results indicated that overexpression of miR-153-5p could enhance the sensitivity of MDA-MB-231/PTX cells to PTX in vivo via inducing cell cycle arrest.
Figure 6.
Overexpression of miR-153-5p enhanced the sensitivity of MDA-MB-231/PTX cells to PTX in vivo. MDA-MB-231/PTX cells were injected subcutaneously into nude mice to form subcutaneous tumors. (A) Tumor volumes of mice were monitored weekly. (B) MDA-MB-231/PTX xenograft tumors in each group was pictured and weighted on day 28. (C) Expression levels of CDK1, cyclin B1 and p-Akt in tumor tissues were detected with Western blotting. (D, E, F) The relative expressions of CDK1, cyclin B1 and p-Akt in tumor tissues were quantified via normalizing to β-actin. *P<0.05, **P<0.01 compared with control group; ##P<0.01 compared with PTX_20 nM group.
Abbreviations: PTX, paclitaxel; CDK1, cyclin-dependent kinase 1; Akt, protein kinase B; p-Akt, phosphorylation of Akt.
Discussion
Drug resistance in cancer chemotherapy is the main obstacle in cancer therapy.17 Investigating how to improve drug sensitivity is an important method for treating cancer.18 In the present study, we explored the role of miR-153-5p in PTX-resistance TNBC cells. We found that overexpression of miR-153-5p could enhance the sensitivity of PTX-resistance TNBC cells to PTX.
Recently, miRNAs have received much attention as potential treatment targets in chemo-resistance in tumors.14 Han et al found that miR-338-5p reversed 5-Fluorouracil resistance in esophageal squamous cell carcinoma cells via suppression of Id-1.19 Chai et al reported that overexpression of miR-101 enhanced the sensitivity of liver cancer cells to cisplatin via inhibiting the activation of DNA-PKcs signaling pathway.20 Sun et al indicated that inhibition of miR-4262 reduced PTX resistance in lung cancer cells.21 In addition, evidences have been shown that miR-153 functioned as a tumor suppressor in several cancers including lung cancer, acute lymphoblastic leukemia and breast cancer.22–24 In this study, we found that overexpression of miR-153-5p significantly induced the apoptosis of MDA-MB-231/PTX cells. In addition, the inhibitory effects of PTX on the proliferation and migration of MDA-MB-231/PTX cells were enhanced by miR-153-5p overexpression. Meanwhile, overexpression of miR-153-5p obviously enhanced the anti-apoptotic effect of PTX on MDA-MB-231/PTX cells. Mei et al indicated that upregulation of miR-5195 significantly reduced the chemo-resistance to PTX in TNBC cells, which was consistent with our results.14 These data indicated that overexpression of miR-153-5p could enhance the sensitivity of MDA-MB-231/PTX cells to PTX.
Although miR-153-5p has been suggested to function as a tumor suppressor, the underlying mechanism by which miR-153-5p-mediated gene expression involved in chemotherapy resistance in MDA-MB-231/PTX cells remains unclear. Bioinformatics analysis tool TargetScan and luciferase reporter assay were used to predict and verify potential binding targets of miR-153-5p. The data illustrated that CDK1 was a potential binding target of miR-153-5p. CDK1 is an important member in cell cycle regulation, which is reported to contribute to tumor progression.25 CDK1 is a G2/M cell cycle regulatory protein, also known as M-phase promoting factor.26 When the cell passes through the G2/M phase, the CDK1/cyclin B complex is synthesized largely.27 Decreased expression of the CDK1/cyclin B complex was able to induce G2/M phase cell cycle arrest.28 Meanwhile, CDK1 also has been reported to affect the PI3K/Akt pathway, knockdown of CDK1 could inhibit the expression of Akt.29 In this study, we found that combination treatment markedly induced G2M phase arrest in MDA-MB-231/PTX cells via downregulation of the expressions of CDK1, cyclin B1 and Akt, which were consistent with previous study. Furthermore, it has been shown that overexpressed CDK1/cyclin B complex is predictive of chemo-resistance and poor survival in cancers.30 These data indicated that overexpression of miR-153-5p could reverse PTX resistance in MDA-MB-231/PTX cells via inducing G2M phase arrest.
Conclusion
Collectively, miR-153-5p could reverse PTX resistance in PTX-resistant TNBC cells via inducing G2/M phase arrest. Therefore, PTX combined with miR-153-5p might be considered as a novel therapeutic method for the treatment of PTX-resistant TNBC.
Disclosure
The authors declare no competing financial interests.
References
- 1.Liu C, Min L, Kuang J, et al. Bioinformatic Identification of miR-622 key target genes and experimental validation of the miR-622-RNF8 axis in breast cancer. Front Oncol. 2019;9:1114. doi: 10.3389/fonc.2019.01114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dai X, Zhang S, Cheng H, et al. FA2H exhibits tumor suppressive roles on breast cancers via cancer stemness control. Front Oncol. 2019;9:1089. doi: 10.3389/fonc.2019.01089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bao C, Lu Y, Chen J, et al. Exploring specific prognostic biomarkers in triple-negative breast cancer. Cell Death Dis. 2019;10(11):807. doi: 10.1038/s41419-019-2043-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dent R, Trudeau M, Pritchard KI, et al. Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res. 2007;13(15 Pt 1):4429–4434. doi: 10.1158/1078-0432.CCR-06-3045 [DOI] [PubMed] [Google Scholar]
- 5.Gluz O, Liedtke C, Gottschalk N, et al. Triple-negative breast cancer–current status and future directions. Ann Oncol. 2009;20(12):1913–1927. doi: 10.1093/annonc/mdp492 [DOI] [PubMed] [Google Scholar]
- 6.Li Y, Liang Y, Sang Y, et al. MiR-770 suppresses the chemo-resistance and metastasis of triple negative breast cancer via direct targeting of STMN1. Cell Death Dis. 2018;9(1):14. doi: 10.1038/s41419-017-0030-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zasadil LM, Andersen KA, Yeum D, et al. Cytotoxicity of paclitaxel in breast cancer is due to chromosome missegregation on multipolar spindles. Sci Transl Med. 2014;6(229):229ra243. doi: 10.1126/scitranslmed.3007965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Armstrong DK, Bundy B, Wenzel L, et al. Intraperitoneal cisplatin and paclitaxel in ovarian cancer. N Engl J Med. 2006;354(1):34–43. doi: 10.1056/NEJMoa052985 [DOI] [PubMed] [Google Scholar]
- 9.Liao WS, Ho Y, Lin YW, et al. Targeting EGFR of triple-negative breast cancer enhances the therapeutic efficacy of paclitaxel- and cetuximab-conjugated nanodiamond nanocomposite. Acta Biomater. 2019;86:395–405. doi: 10.1016/j.actbio.2019.01.025 [DOI] [PubMed] [Google Scholar]
- 10.Krol J, Loedige I, Filipowicz W. The widespread regulation of microRNA biogenesis, function and decay. Nat Rev Genet. 2010;11(9):597–610. doi: 10.1038/nrg2843 [DOI] [PubMed] [Google Scholar]
- 11.Xu W, Li J, Tian H, et al. MicroRNA1865p mediates osteoblastic differentiation and cell viability by targeting CXCL13 in nontraumatic osteonecrosis. Mol Med Rep. 2019;20(5):4594–4602. doi: 10.3892/mmr.2019.10710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wei D, Yu G, Zhao Y. MicroRNA-30a-3p inhibits the progression of lung cancer via the PI3K/AKT by targeting DNA methyltransferase 3a. Onco Targets Ther. 2019;12:7015–7024. doi: 10.2147/OTT.S213583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang G, Dong Y, Liu H, et al. Loss of miR-873 contributes to gemcitabine resistance in triple-negative breast cancer via targeting ZEB1. Oncol Lett. 2019;18(4):3837–3844. doi: 10.3892/ol.2019.10697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu M, Gong C, Xu R, Chen Y, Wang X. MicroRNA-5195-3p enhances the chemosensitivity of triple-negative breast cancer to paclitaxel by downregulating EIF4A2. Cell Mol Biol Lett. 2019;24(1):47. doi: 10.1186/s11658-019-0168-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu X, Li L, Li Y, Liu Z. MiR-153 promotes breast cancer cell apoptosis by targeting HECTD3. Am J Cancer Res. 2016;6(7):1563–1571. [PMC free article] [PubMed] [Google Scholar]
- 16.Wee ZN, Yatim SM, Kohlbauer VK, et al. IRAK1 is a therapeutic target that drives breast cancer metastasis and resistance to paclitaxel. Nat Commun. 2015;6(1):8746. doi: 10.1038/ncomms9746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yao J, Yao X, Tian T, et al. ABCB5-ZEB1 axis promotes invasion and metastasis in breast cancer cells. Oncol Res. 2017;25(3):305–316. doi: 10.3727/096504016X14734149559061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang Y, Sui Y, Tao Y. Gambogic acid increases the sensitivity to paclitaxel in drug-resistant triple-negative breast cancer via the SHH signaling pathway. Mol Med Rep. 2019;20(5):4515–4522. doi: 10.3892/mmr.2019.10697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Han L, Cui D, Li B, et al. MicroRNA-338-5p reverses chemoresistance and inhibits invasion of esophageal squamous cell carcinoma cells by targeting Id-1. Cancer Sci. 2019;110(12):3677–3688. doi: 10.1111/cas.14220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chai Z, Yin X, Chen J, et al. MicroRNA-101 modulates cisplatin chemoresistance in liver cancer cells via the DNA-PKcs signaling pathway. Oncol Lett. 2019;18(4):3655–3663. doi: 10.3892/ol.2019.10674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sun H, Zhou X, Bao Y, et al. Involvement of miR-4262 in paclitaxel resistance through the regulation of PTEN in non-small cell lung cancer. Open Biol. 2019;9(7):180227. doi: 10.1098/rsob.180227 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 22.Wang L, Lv X, Fu X, et al. MiR-153 inhibits the resistance of lung cancer to gefitinib via modulating expression of ABCE1. Cancer Biomark. 2019;25(4):361–369. doi: 10.3233/CBM-190094 [DOI] [PubMed] [Google Scholar]
- 23.Jiang J, Liu Y, Zhao Y, Tian F, Wang G. miR-153-3p suppresses inhibitor of growth protein 2 expression to function as tumor suppressor in acute lymphoblastic leukemia. Technol Cancer Res Treat. 2019;18:1533033819852990. doi: 10.1177/1533033819852990 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 24.Zuo Z, Ye F, Liu Z, Huang J, Gong Y. MicroRNA-153 inhibits cell proliferation, migration, invasion and epithelial-mesenchymal transition in breast cancer via direct targeting of RUNX2. Exp Ther Med. 2019;17(6):4693–4702. doi: 10.3892/etm.2019.7470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li Y, Quan J, Chen F, et al. MiR-31-5p acts as a tumor suppressor in renal cell carcinoma by targeting cyclin-dependent kinase 1 (CDK1). Biomed Pharmacother. 2019;111:517–526. doi: 10.1016/j.biopha.2018.12.102 [DOI] [PubMed] [Google Scholar]
- 26.Luo L, Ran R, Yao J, et al. Se-enriched cordyceps militaris inhibits cell proliferation, induces cell apoptosis, and causes G2/M phase arrest in human non-small cell lung cancer cells. Onco Targets Ther. 2019;12:8751–8763. doi: 10.2147/OTT.S217017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang Y, Xue K, Li Z, et al. c-Myc regulates the CDK1/cyclin B1 dependentG2/M cell cycle progression by histone H4 acetylation in Raji cells. Int J Mol Med. 2018;41(6):3366–3378. doi: 10.3892/ijmm.2018.3519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pan Z, Zhang X, Yu P, et al. Cinobufagin induces cell cycle arrest at the G2/M phase and promotes apoptosis in malignant melanoma cells. Front Oncol. 2019;9:853. doi: 10.3389/fonc.2019.00853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang XQ, Lo CM, Chen L, et al. CDK1-PDK1-PI3K/Akt signaling pathway regulates embryonic and induced pluripotency. Cell Death Differ. 2017;24(1):38–48. doi: 10.1038/cdd.2016.84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tsuyoshi H, Wong VKW, Han Y, et al. Saikosaponin-d, a calcium mobilizing agent, sensitizes chemoresistant ovarian cancer cells to cisplatin-induced apoptosis by facilitating mitochondrial fission and G2/M arrest. Oncotarget. 2017;8(59):99825–99840. doi: 10.18632/oncotarget.21076 [DOI] [PMC free article] [PubMed] [Google Scholar]