Abstract
Aim
Heart failure is a global problem that is increasing in prevalence. We undertook the initiative to compile the Vellore Heart Failure Registry (VHFR) to assess the clinical profile, mortality, risk factors and economic burden of heart failure by conducting a prospective, observational, hospital-based cohort study in Vellore, Tamil Nadu.
Methods and results
This study was a prospective observational cohort study conducted at the Christian Medical College and Hospital, Vellore, between January 2014 and December 2016. A total of 572 patients who satisfied the Boston criteria for “definite heart failure” were included and the primary outcome was all-cause mortality. The median duration of hospital stay was eight days and the in-hospital, one, three and six month mortalities were 13.25%, 27.3%, 32.53% and 38.15%, respectively. The median duration of survival was 921 days. Readmission for heart failure constituted 42%, and the most common cause of decompensation was an infection(31.5%). The presence of cyanosis at admission, history of previous stroke or transient ischemic attack, and American College of Cardiology (ACC)/American Heart Association (AHA) stage D at the time of discharge were independently associated with mortality at six months. The median total direct cost of admission was INR 84,881.00 ($ 1232.34)
Conclusion
The VHFR cohort had younger, more diabetic, and fewer hypertensive subjects than most cohorts. Admission for heart failure is a catastrophic health expenditure. Attempts should be made to ensure a reduction in readmission rates by targeting goal-directed therapy. As the most common cause of acute decompensation is pneumonia, vaccinating all patients before discharge may also help in this regard.
Keywords: Heart failure, Mortality, Cohort study
1. Introduction
1.1. Background
The Framingham study places the incidence of heart failure at 564 per 100,000 person-years in men and 327 per 100000 person-years in women.1 In accordance with the 2018 American Heart Association (AHA) update on heart disease and stroke statistics, 6.5 million Americans above the age of 20 years are living with heart failure, with a prevalence of 19.89 per 1000 individuals.2 Most heart failure cohorts in developing countries have issues with nonuniform definitions and exclusion of patients with heart failure with preserved ejection fraction.3, 4, 5, 6 The AHA estimates that heart failure costs the country 30.7 billion dollars every year .7 The estimated lifetime cost incurred by an individual after a diagnosis of heart failure has been estimated as $109,541 per person.8 The economic impact in a developing country such as India is not well documented. We undertook the Vellore Heart Failure Registry (VHFR) to assess the clinical profile, mortality, risk factors and economic burden of heart failure by conducting a prospective, observational, hospital-based cohort study in Vellore, Tamil Nadu.
1.2. Objectives
The primary objective of the study was to determine the incidence density of mortality of patients admitted with acute decompensated heart failure to our hospital. The secondary objectives were to identify the predictors of mortality and the direct cost incurred by patients admitted with acute decompensated heart failure.
2. Methods
2.1. Study design
This study was a prospective observational cohort study of patients admitted with clinically diagnosed acute decompensated heart failure. The study was approved by the institutional review board before its commencement (No. 10416). The investigation protocol complied with the Good Clinical Practices and the Declaration of Helsinki. The results were reported by following the Strengthening the Reporting of Observational Studies in Epidemiology guidelines for reporting observational studies.9
2.2. Setting
This study was conducted in the Christian Medical College and Hospital, Vellore, a 2858 bedded university teaching institute in South India. This hospital receives patients predominantly from the southern and northeastern states of India, belonging to all socio-economic classes.
2.3. Participants
The recruitment of participants took place between 1st January 2014 and 31st December 2017. Patient recruitment between January 2014 and December 2016 was retrospective, whereas the recruitment for the rest was prospective. Irrespective of the recruitment, all patients were followed prospectively till 30th June 2018. In our hospital, patients presenting with acute decompensated heart failure are seen in the emergency department (ED) or outpatient clinics. After stabilization, patients in the ED are then admitted to either the intensive care unit or ward. The patients admitted were included in the study if they were 18 years or older and fulfilled the “definite heart failure” criteria of the Boston Criteria.10
2.4. Variables
The primary outcome was all-cause mortality (in-hospital, at one month, at three months and six months) and the secondary outcomes were survival time, Minnesota Living with Heart Failure Questionnaire (MLHFQ) score, International Physical Activity Questionnaire score and the direct medical cost of admission.11, 12, 13 The socio-economic status was assessed using the Kuppuswamy socio-economic class.14 Guideline-based therapy, which was defined as being prescribed a beta-blocker along with either an angiotensin-converting enzyme (ACE) inhibitor, angiotensin receptor blocker (ARB) or both isosorbide-mononitrate and hydralazine (regardless of ejection fraction on echocardiogram), at the time of discharge.
2.5. Data sources and bias
Data were recorded on a case report form (CRF) that was designed before the commencement of the study. The outcome of death was confirmed through hospital records or telephonic confirmation with the immediate family members. Some of the required data were collected from the electronic medical records of the hospital.
2.6. Sample size
The required sample size to show a mortality of 17% was 217 patients with 5% precision and 5% alpha error.15 We assumed a 20% drop out rate and arrived at a sample size of 271.
2.7. Statistical methods
Data entry was done by the principal investigator from the CRF into Epidata, version 3.1. This data was then exported to SPSS 25(IBM, Armonk, NY). All categorical baseline data were described using numbers and percentages. Continuous data were described using mean and standard deviation. Person time was calculated in months for all the patients, and the incidence density with a 95% confidence interval was calculated. Time to event data was performed by using the Kaplan–Meier estimate. Unadjusted analyses were carried out to predict mortality, followed by Cox-proportional hazard regression analyses.
3. Results
3.1. Participants
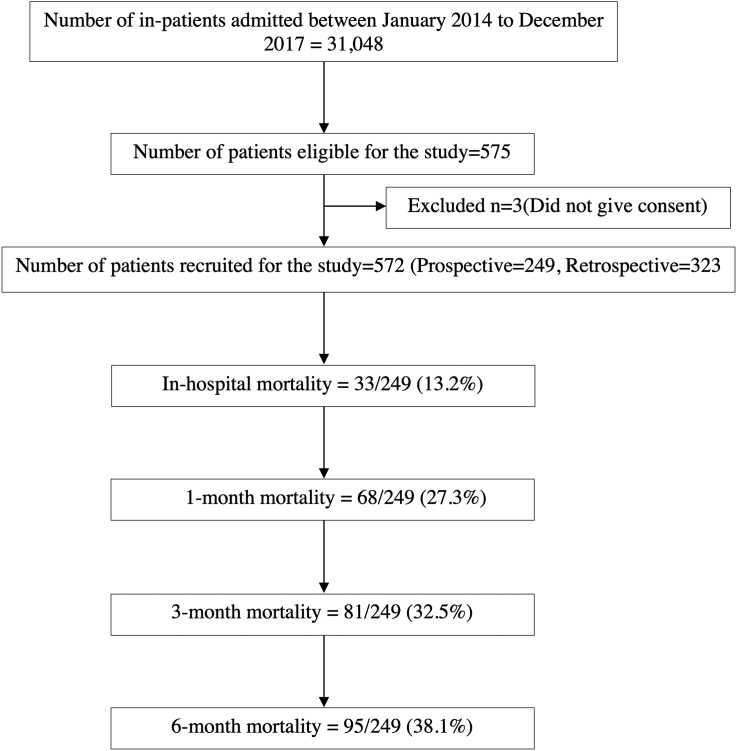
A total of 575 patients were assessed for eligibility for this study [Fig. 1]. Of these, three were excluded as they did not give consent. A total of 572 patients were included in the final analysis. Of the 249 patients recruited prospectively, 21 patients were lost to follow-up. The demographic details and baseline characteristics of the participants are given in Supplementary Table 1. The proportion of men and women were almost the same. Most of the participants belonged to the lower-middle/upper-lower socio-economic class. Diabetes mellitus and hypertension were the most common comorbid conditions in these patients. Smokers constituted 17.8%, whereas 15.6% were alcohol consumers. The most common presenting complaints were dyspnea (92.8%), orthopnea (60.8%) and cough (48.2%), whereas the most common examination findings were crepitations (85.5%), elevated jugular venous pulse(68%) and pedal edema (58.4%). Most had very high NT-ProBNP levels. Nearly 40% each had heart failure with preserved and reduced ejection fraction respectively, while 20% had heart failure with mid-range ejection fraction [Supplementary Table 2].
Fig. 1.
STROBE diagram. STROBE, Strengthening the Reporting of Observational Studies in Epidemiology.
The median duration of hospital stay was eight days. More than half of the patients (58%) presented with de novo heart failure, while 42% were readmissions. Ischemic heart disease was the most common cause of pre-existing heart failure. The most common reasons for decompensation were an infection (31.5%) and acute coronary syndrome (31.1%). Among infections, pneumonia was the most common, followed by pyelonephritis and infective exacerbation of chronic obstructive pulmonary disease. Noninvasive ventilation was required by 26.9% of patients and invasive ventilation by 7.2% of patients in the acute setting [Supplementary Table 3]. Only 3.1% of the patients received influenza and pneumococcal vaccination before discharge. Guideline-based therapy was provided to 41.9% of patients.
3.2. Outcome
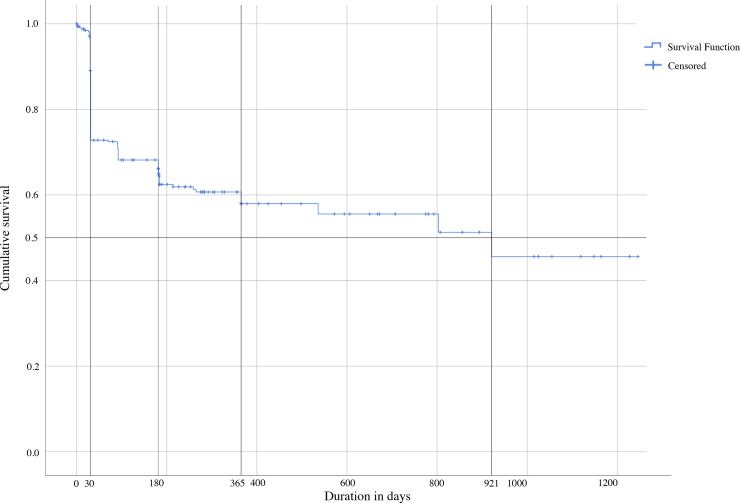
The in-hospital mortality was 33 (13.25%). The cumulative mortality at the end of one, three, and six months were 68 (27.3%), 81 (32.53%) and 95 (38.15%), respectively. The incidence density of mortality was 6.47 deaths per 100 person-months of follow-up. The Kaplan–Meir survival estimate showed that most deaths occur within the first month, and the survival remains stable after that [Fig. 2]. Hence, those who survive the first one month after discharge tend to have a good life expectancy. After a total follow-up duration of 4580.6 person-months, the mean survival time was found to be 704.51 days (standard deviation (SD): 43.11, 95% CI: 620–789), and the median duration of survival was 921 days. The mean MLHFQ score at discharge was 52.12 (SD: 19.14). The Cox-proportional hazards model identified that the presence of cyanosis at admission (HR: 5.95, 95% CI: 1.13–31.41), history of previous stroke or transient ischemic attack (HR: 2.27, 95% CI: 1–5.19) and ACC/AHA stage D (HR: 5.25, 95% CI: 2.54–10.83) at the time of discharge were independently associated with mortality at 6 months[Supplementary Table 4].
Fig. 2.
Kaplan–Meier survival estimate. Duration of survival in days is given along the x-axis. Cumulative survival is plotted along the y-axis. The median duration of survival is 921 days.
The median cost for an admission to the hospital with decompensated heart failure was INR 50,990 (inter-quartile range (IQR) INR 29,536–81,184)($740.30, IQR $428.82 - $1178.67) [Table 1]. The median drug cost, cost of accommodation for by-standers, and cost of food for by-standers were INR 27,837 (IQR INR 14,745–72,011)($404.15, IQR $214.07 - $1045.49), INR 2500 (IQR INR 775–5000)($36.30, IQR $11.25 - $72.59) and INR 2000 (IQR INR 1000–5000)($29.04, IQR $14.52 - $72.59), respectively. The mean total direct cost of admission was INR 1,18,690.94 ($1723.21) (median cost INR 84,881 ($1232.34), IQR 50,216–1,50,083 ($729.06-$2178.98).
Table 1.
Cost of admission with heart failure.
| Cost in rupees ($) | Mean ± SD | Median | Interquartile Range |
|---|---|---|---|
| Bill amount (n = 249) INR | ₹69,746.70 ± 68,579.40 | ₹50,990.00 | ₹29,536–₹81,184 |
| $ | $1012.61 ± -$995.67 | $740.30 | $428.82–$1178.67 |
| Pharmacy bill (n = 209) INR | ₹53,651.27 ± 61,770.17 | ₹27,837.00 | ₹14,745–₹72,011 |
| $ | $778.93 ± 896.81 | $404.15 | $214.07–$1045.49 |
| Cost of accommodation INR | ₹5121.43 ± 6889.73 | ₹2500.00 | ₹775–₹5000 |
| (n = 98) $ | $74.36 ± -$100.03 | $36.30 | $11.25–$72.59 |
| Cost of food (n = 130) INR | ₹3631.54 ± 4725.70 | ₹2000.00 | ₹1000–₹5000 |
| $ | $52.72 ± 68.61 | $29.04 | $14.52–$72.59 |
| Total direct cost (n = 249) INR | ₹1,18,690.94 ± 1,12,485.50 | ₹84,881.00 | ₹50,216–₹1,50,083 |
| $ | $1723.21 ± $1633.12 | $1232.34 | $729.06–$2178.98 |
4. Discussion
The VHFR is the second-largest cohort study of patients with heart failure from India and gives a fresh insight into the clinical profile, risk factors and survival of patients with heart failure. In addition, VHFR is the only study from India, which has attempted to estimate the economic impact of heart failure.
Our cohort of patients with acute decompensated heart failure included nearly 60% who had de novo heart failure. This also means that nearly 40% of the patients were being readmitted for heart failure. Unlike other diseases in cardiology where a single procedure can give most patients a near-normal quality of life, heart failure is a chronic disease with multiple episodes of decompensation and readmission to the hospital. This incurs a massive psychological and financial burden to the patient and the family members. The chronic nature of the disease has to be explained to the patient and relatives in detail, and a holistic approach with a multidisciplinary team is essential in the management of heart failure. Our mortality rates are comparable with those from Indian cohorts and higher than those in western cohorts [Table 2 and Table 3]. These could be due to differences in disease severity and comorbidities as we discuss in the following context.
Table 2.
Comparison of mortality and duration of hospitalization between global cohorts and our study.
| Cohort | Rotterdam | EHFS I | EHFS II | EFFECT | ADHERE | OPTIMIZE-HF | ATTEND | THESUS-HF | ALARM-HF | ASIAN-HF | VHFR |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patients number | 7983 | 11327 | 3580 | 2450 | 105388 | 48612 | 4842 | 1006 | 4953 | 5276 | 572 |
| In-hospital mortality, % | 6.90% | 6.70% | 4% | 4% | 6.40% | 4.20% | 11% | 13.25% | |||
| 30-day mortality, % | 14% | 6.40% | 4% | 11.20% | 27.3% | ||||||
| 60-day mortality, % | 9% (60–90 days) | 10.60% | |||||||||
| 90-day mortality, % | 6.60% | 8.10% | 32.53% | ||||||||
| 180-day mortality, % | 17.80% | 6.9% | 38.15% | ||||||||
| 1-year mortality, % | 37% | 20.50% | 24.20% | ||||||||
| Hospital stay, median days | 11 | 9 | 4 | 4 | 21 | 7 | 6 | 8 |
Rotterdam: The prognosis of heart failure in the general population: The Rotterdam Study, EHFS I, EuroHeart Failure Survey I; EHFS II, Euro Heart Failure Survey II; EFFECT, Enhanced Feedback for Effective Cardiac Treatment; ADHERE, Acute Decompensated Heart Failure National Registry; OPTIMIZE-HF, Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure; ATTEND, Acute decompensated heart failure syndromes registry; THESUS-HF, The Sub-Saharan Africa Survey of Heart Failure; ALARM-HF, Acute Heart Failure Global Survey of Standard Treatment; ASIAN-HF, Asian heart failure registry; VHFR, Vellore Heart Failure Registry.
Table 3.
Comparison of mortality and duration of hospitalization between Indian cohorts and our study.
| O.s et ala | AFAR | Roby et alb | MHFR |
THFR | VHFR | ||
|---|---|---|---|---|---|---|---|
| LVSD | PSF | ||||||
| Patients Number | 287 | 90 | 169 | 128 | 122 | 1205 | 572 |
| In-hospital mortality, % | 8.01% | 30.80% | 13.01% | 20% | 6% | 8.50% | 13.25% |
| 30-day mortality, % | 15.80% | 12.50% | 27.3% | ||||
| 60-day mortality, % | 18.10% | ||||||
| 90-day mortality, % | 14.3% | 26.30% | 32.53% | ||||
| 1-year mortality, % | 30.20% | ||||||
| 2-year mortality, % | 37.60% | ||||||
| Hospital stay, median days | 6 | 7 | 6 | 8 | |||
S. O.S., et al, Long-term outcomes of patients admitted with heart failure in a tertiary care center in India, Indian Heart J (2018), https://doi.org/10.1016/j.ihj.2018.01.016; AFAR, Acute failure registry study.
Roby A, Ahammed N. Clinical Profile of Acute Heart Failure in rural Trivandrum. Academic Medical Journal of India. 2014 Nov 20; 2(3):99–101; MHFR, Manipal Heart failure Registry; THFR, Trivandrum Heart Failure Registry; VHFR, Vellore Heart Failure Registry.
The mean age of 59.1 years was about ten years lesser than the mean age of 70 years, of participants in most worldwide cohorts of patients with heart failure.16,17 We had an equal proportion of men and women. In comparison, in the Asian heart failure registry, the percentage of men was 78.2%, and the mean age was 59.6 years.18 In the Trivandrum heart failure study too, there were more men (69.2%), and the mean age was 61.2 years.15 A subgroup analysis showed that there were more men than women with HFrEF and HFmrEF, while the opposite was seen in patients with HFpEF.
Most patients with previously diagnosed heart failure had ischemic heart disease as the etiology (70.8%), followed by rheumatic heart disease (16.7%), dilated cardiomyopathy (11.3%), and others. In the Trivandrum heart failure registry, ischemic heart disease contributed to 71.8%, dilated cardiomyopathy to 12.9%, and rheumatic heart disease to 7.8% of the patients with heart failure.15 This suggests that rheumatic heart disease still contributes to a large proportion of the cases of heart failure in India. More than one-quarter of the patients had normal BMI or were underweight. This can probably be attributed to cardiac cachexia, causing weight loss after the patient develops overt heart failure. 85.8% and 11.5% of the participants presented with NYHA class IV and III symptoms respectively more severely symptomatic at presentation, which could represent referral bias to a tertiary care center.
Our cohort had nearly 30% more diabetics, and about 20% fewer hypertensives when compared to global cohorts. We had meager rates of atrial fibrillation (5.2%) when compared to the OPTIMIZE-HF and ATTEND cohorts, in which, 31% and 40% of the participants, respectively, had atrial fibrillation.17,19 In the Asian heart failure registry, this percentage stood at 17.9%; it was 14.7% in the Trivandrum heart failure registry.15,18 It would seem that atrial fibrillation has a lesser contribution to heart failure in India and Asia when compared with the west. This may be due to the reduction in the prevalence of rheumatic valvular heart disease as a result of improvement in sanitation, reduction in overcrowding and effective rheumatic heart disease prophylaxis therapy. We also had fewer patients with a history of past stroke or transient ischemic attack (5.6%) when compared with other Asian cohorts such as the Trivandrum heart failure registry (6.2%) and the Asian heart failure registry (6.4%).15,18 The ADHERE study noted that 17% of its participants had recorded such a past history.20 Only 1.4% of patients in our study were human immunodeficiency virus (HIV) positive as compared with the 13% of patients were HIV-positive in the THESUS-HF study. This may merely reflect the difference in the local prevalence of HIV disease between sub-Saharan Africa and India.
Heart failure with reduced ejection fraction was seen in 39.3% of our patients, 21.4% heart failure with mid-range ejection fraction, and 39.3% had heart failure with preserved ejection fraction. In comparison, 46% of patients in the EHFS II and 57% of patients in the ATTEND trial had left ventricular ejection fraction less than 40%, whereas 45.1% of patients in the Trivandrum heart failure registry had left ventricular ejection fraction less than 35%.15,17,21
The Asian heart failure registry demonstrated a dose-dependent improvement in 1-year composite outcome with adherence to guideline-based therapy and guideline-recommended dosage of medications.22 Only 21.41% of patients in the Trivandrum heart failure registry received optimal guideline-based therapy, which was defined as receiving a combination of beta-blockers, ACE inhibitors or ARBs, and aldosterone receptor blockers in patients with left ventricular systolic dysfunction (LVSD, EF <45%).15 Our definition mentioned in the methods was slightly different and was seen in 41.9% of patients. Patients who presented with acute decompensated heart failure often have a cardiorenal syndrome that necessitates the discontinuation of ACE inhibitors, ARBs or aldosterone antagonists. This is one of the reasons why less than half of the patients were discharged on guideline-based therapy. Nevertheless, an attempt to restart these medications must be made at the earliest available opportunity once the creatinine falls. Actively trying to maximize the number of patients on guideline-based therapy represents an opportunity to improve management and outcome in patients with heart failure.
The most common cause of precipitation of heart failure was infection (31.5%), followed by acute coronary syndrome (31.1%). Among infections, pneumonia was the most common cause. Influenza A/B was the etiological agent in 9.5% of patients with community-acquired pneumonia and 23.1% of patients with an infective exacerbation of chronic obstructive pulmonary disease. It is difficult to prove whether influenza causes decompensation by causing direct injury to the myocardium or as a side effect of altered heart–lung interaction leading to increased preload and afterload—association does not imply causality. This is an interesting question that can be answered in a future study. It is also important to note that only 3.1% of patients received influenza and pneumococcal vaccination before discharge. Therefore, influenza vaccination is another opportunity to improve the outcome of patients with heart failure.
A previous history of stroke or transient ischemic attack was one of the independent risk factors for mortality that were identified by the study. A past stroke or transient ischemic attack may indicate atherosclerotic disease in the carotid vessels and other vessels of the cerebral circulation. The pathophysiology of this disease is similar to that of coronary artery disease and is predominantly driven by diabetes mellitus, dyslipidaemia, and hypertension. The increased prevalence of diabetes mellitus in our population, which accelerates atherosclerosis in both arterial territories, explains why the presence of previous stroke or transient ischemic attack emerged as an independent predictor of mortality at six months in our study. ACC/AHA Stage D indicates irreversible pump failure, which is persistent at the time of discharge.
To the best of our knowledge, ours is the first study in the country to look at the financial burden associated with admission for acute decompensated heart failure. We found a median total direct cost of INR 84,881 ($1232.34), which is a substantial amount. To put this into perspective, as of 2011, 21.9% of the population in India lives below the poverty line, and 21.2% of the employed population are below $1.9 in purchasing power parity per day. The major contributors to cost were the hospital bill and purchase of medications. We have not calculated the indirect costs associated with hospital admission. Therefore, ours is an underestimation of the actual financial burden associated with this disease. Eighty-eight per cent of our patients have a monthly family income less than INR 22,000. This means that admission for acute decompensated heart failure incurs a cost that is almost four times the monthly income of most of the patients. When out-of-pocket payments for health-care services take up such a large portion of a household's available income and the family may be pushed into poverty as a result of the same, the health-care expenditure is called a catastrophic health expenditure (CHE).23 The cutoff for CHE has been defined both as 10% of total household expenditure and 40% of the household's capacity to pay.24,25 Admission for acute decompensated heart failure is a CHE. Forty-two per cent of our patients were admitted more than once during the study period. Patients with heart failure face difficulty finding and engaging in employment if they are symptomatic. Perhaps now, we can begin to appreciate the real economic burden of this crippling disease.
5. Conclusion
The VHFR cohort had younger, more diabetic, and fewer hypertensive subjects than most cohorts. The incidence density of mortality of patients was 6.47 deaths per 100 person-months. The median survival time was 921 days. The presence of cyanosis at admission, a history of previous stroke/TIA and ACC/AHA stage D at the time of discharge were associated with 6-month mortality and reduced survival time. The median total direct cost of admission was INR 84,881($1232.34) and is a CHE. Attempts should be made to ensure a reduction in readmission rates, which currently stands at 42%. This can be achieved by targeting goal-directed therapy and vaccinating all patients against influenza and pneumococcus before discharge as the most common cause of decompensation is pneumonia.
6. Limitations and generalizability
The study was performed in a tertiary care hospital and hence is prone to referral bias. Some patients with heart failure and other severe organ dysfunction or coexistent systemic disease, who were admitted to other specialty units were not included in this study, although we believe that this would unlikely to influence the results. Finally, we were not able to calculate the indirect costs associated with admission for acute decompensated heart failure. Therefore, we might have underestimated the actual financial burden of admission for the same. These limitations have to be kept in mind before interpreting the results of the study and applying it to clinical practice.
What is already known?
-
1.
Heart failure is a significant cause of mortality and morbidity.
-
2.
The social and economic impact of this disease is expected to rise as the population ages.
What this study adds:
-
1.
Admission for heart failure is a catastrophic health expenditure.
-
2.
Attempts should be made to ensure a reduction in readmission rates by targeting goal-directed therapy.
Author contributions
K.J.J., T.V.P., M.K., V.K.C., L.J., V.J., J.V.P., M.K., G.C., K.G. and T.D.S. contributed to the conceptual design of the study. K.J.J., F.M., N.J.N., and A.J. contributed to the conduction of study and data collection. L.J., V.J., A.N., K.J.J., T.V.P., and T.D.S. contributed to the interpretation of data. K.J.J., T.V.P., L.J., A.N., and T.D.S. contributed to write-up and submission of the study. T.V.P., A.M. and T.D.S. reviewed the final manuscript. All authors reviewed and agreed with the final content of the article. T.D.S. was responsible for the oversight of the study and final approval of manuscript before submission.
Funding
The study was funded by a research grant from the Christian Medical College, Vellore [No. 10416].
Conflict of interest
The authors report no relationships that could be construed as a conflict of interest.
Acknowledgment
The authors would like to thank Prof. Varghese John for reviewing the manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ihj.2020.03.005.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Levy D., Kenchaiah S., Larson M.G. Long-term trends in the incidence of and survival with heart failure. N Engl J Med. 2002 Oct 31;347(18):1397–1402. doi: 10.1056/NEJMoa020265. [DOI] [PubMed] [Google Scholar]
- 2.Benjamin E.J., Virani S.S., Callaway C.W. Heart disease and stroke statistics—2018 update: a report from the American heart association. Circulation. 2018 doi: 10.1161/CIR.0000000000000558. https://www.ahajournals.org/doi/10.1161/CIR.0000000000000558# [Internet]. Mar [cited 2018 Sep 22]; Available from: [DOI] [PubMed] [Google Scholar]
- 3.Lam C.S.P., Anand I., Zhang S. Asian sudden cardiac death in heart failure (ASIAN-HF) registry. Eur J Heart Fail. 2013 Aug 1;15(8):928–936. doi: 10.1093/eurjhf/hft045. [DOI] [PubMed] [Google Scholar]
- 4.S O.s., V G., M A.r. Long-term outcomes of patients admitted with heart failure in a tertiary care center in India. Indian Heart J. 2018 Jul 1;70:S85–S89. doi: 10.1016/j.ihj.2018.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seth S., Khanal S., Ramakrishnan S., Gupta N., Bahl V. Epidemiology of acute decompensated heart failure in India : the Afar study (Acute failure registry study) J Pract Cardiovasc Sci. 2015;1(1):35. [Google Scholar]
- 6.Roby A., Ahammed N. Clinical profile of acute heart failure in rural Trivandrum. Acad Med J India. 2014 Nov 20;2(3):99–101. [Google Scholar]
- 7.Heidenreich P.A., Trogdon J.G., Khavjou O.A. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011 Mar 1;123(8):933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 8.Dunlay S.M., Shah N.D., Shi Q. Lifetime costs of medical care after heart failure diagnosis. Circ Cardiovasc Qual Outcomes. 2011 Jan 1;4(1):68–75. doi: 10.1161/CIRCOUTCOMES.110.957225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.von Elm E., Altman D.G., Egger M. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008 Apr;61(4):344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 10.The Criteria Committee of the New York Heart Association . 9th ed. Little & Brown; Boston, Mass: 1994. Nomenclature and Criteria for Diagnosis of Diseases of the Heart and Great Vessels. [Google Scholar]
- 11.Rector T.S., Cohn J.N. Assessment of patient outcome with the Minnesota Living with Heart Failure questionnaire: reliability and validity during a randomized, double-blind, placebo-controlled trial of pimobendan. Pimobendan Multicenter Research Group. Am Heart J. 1992 Oct;124(4):1017–1025. doi: 10.1016/0002-8703(92)90986-6. [DOI] [PubMed] [Google Scholar]
- 12.Garin O., Herdman M., Vilagut G. Assessing health-related quality of life in patients with heart failure: a systematic, standardized comparison of available measures. Heart Fail Rev. 2014 May;19(3):359–367. doi: 10.1007/s10741-013-9394-7. [DOI] [PubMed] [Google Scholar]
- 13.Craig C.L., Marshall A.L., Sjöström M. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003 Aug;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 14.Sharma R. Revised Kuppuswamy's socioeconomic status scale: explained and updated. Indian Pediatr. 2017 Oct;54(10):867–870. [PubMed] [Google Scholar]
- 15.Harikrishnan S., Sanjay G., Anees T. Clinical presentation, management, in-hospital and 90-day outcomes of heart failure patients in Trivandrum, Kerala, India: the Trivandrum Heart Failure Registry. Eur J Heart Fail. 2015 Aug;17(8):794–800. doi: 10.1002/ejhf.283. [DOI] [PubMed] [Google Scholar]
- 16.Fonarow G.C., Abraham W.T., Albert N.M. Influence of beta-blocker continuation or withdrawal on outcomes in patients hospitalized with heart failure: findings from the OPTIMIZE-HF Program. J Am Coll Cardiol. 2008 Jul 15;52(3):190–199. doi: 10.1016/j.jacc.2008.03.048. [DOI] [PubMed] [Google Scholar]
- 17.Sato N., Kajimoto K., Asai K. Acute decompensated heart failure syndromes (ATTEND) registry. A prospective observational multicenter cohort study: rationale, design, and preliminary data. Am Heart J. 2010 Jun 1;159(6):949–955.e1. doi: 10.1016/j.ahj.2010.03.019. [DOI] [PubMed] [Google Scholar]
- 18.Lam C.S.P., Teng T.-H.K., Tay W.T. Regional and ethnic differences among patients with heart failure in Asia: the Asian sudden cardiac death in heart failure registry. Eur Heart J. 2016 Nov 1;37(41):3141–3153. doi: 10.1093/eurheartj/ehw331. [DOI] [PubMed] [Google Scholar]
- 19.Fonarow G.C., Stough W.G., Abraham W.T. Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF Registry. J Am Coll Cardiol. 2007 Aug 21;50(8):768–777. doi: 10.1016/j.jacc.2007.04.064. [DOI] [PubMed] [Google Scholar]
- 20.Yancy C.W., Lopatin M., Stevenson L.W., De Marco T., Fonarow G.C. ADHERE Scientific Advisory Committee and Investigators. Clinical presentation, management, and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: a report from the Acute Decompensated Heart Failure National Registry (ADHERE) Database. J Am Coll Cardiol. 2006 Jan 3;47(1):76–84. doi: 10.1016/j.jacc.2005.09.022. [DOI] [PubMed] [Google Scholar]
- 21.Nieminen M.S., Brutsaert D., Dickstein K. EuroHeart Failure Survey II (EHFS II): a survey on hospitalized acute heart failure patients: description of population. Eur Heart J. 2006 Nov 1;27(22):2725–2736. doi: 10.1093/eurheartj/ehl193. [DOI] [PubMed] [Google Scholar]
- 22.Teng T.-H.K., Tromp J., Tay W.T. Prescribing patterns of evidence-based heart failure pharmacotherapy and outcomes in the ASIAN-HF registry: a cohort study. Lancet Global Health. 2018 Sep 1;6(9):e1008–e1018. doi: 10.1016/S2214-109X(18)30306-1. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization . Geneva : World Health Organization; Geneva: 2005. Distribution of Health Payments and Catastrophic Expenditures Methodology.http://apps.who.int/iris/handle/10665/69030 [Internet] [cited 2018 Oct 7]. Report No.: EIP/FER/DP.05.2. Available from: [Google Scholar]
- 24.WHO . 2018 Oct 7. Trends in Catastrophic Health Expenditure in India: 1993 to 2014.http://www.who.int/bulletin/volumes/96/1/17-191759/en/ [Internet]. WHO. [cited. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bonu S., Bhushan I., Rani M., Anderson I. Incidence and correlates of ‘catastrophic’ maternal health care expenditure in India. Health Pol Plann. 2009 Nov 1;24(6):445–456. doi: 10.1093/heapol/czp032. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.