Abstract
Background
Cardiovascular disease is the leading cause of death in India. Previously it was thought to be a disease of the elderly but now an epidemiological transition is being seen with increasing incidence in the very young adults as well. Such patterns are not well studied in the South East Asian population.
Objective
To study the epidemiological profile of very young (≤35 years) adults presenting with an acute myocardial infarction (AMI) in comparison with an older cohort.
Methodology
The present study included all patients presenting with AMI to the emergency or to the out-patient department of the G B Pant Institute of Postgraduate Medical Education and Research (GIPMER), New Delhi between January 2014 and October 2015. A total of 102 subjects ≤35 years with AMI comprised the study subjects (cases) and were compared with 104 subjects >35 years old with AMI (Controls).
Results & conclusion
Most of the very young AMI patients presented with an anterior wall ST segment elevation myocardial infarction, a stable hemodynamic profile, single vessel disease and better left ventricular ejection fraction as compared with controls. Most of the patients were from urban and semi-urban areas, middle and lower middle socioeconomic status and were smokers but lacked other traditional risk factors.
Keywords: Very young adults, Acute myocardial infarction, Risk factors, Management, Epidemiology
Abbreviations: ACS, Acute Coronary Syndromes; AMI, Acute Myocardial Infarction; AWMI, Anterior Wall Myocardial Infarction; CAG, Invasive Coronary Angiography; CVD, Cardio Vascular Disease; CAD, Coronary Artery Disease; ER, Emergency Room; FMC, First Medical Contact; h/o, History Of; IHD, Ischemic Heart Disease; IWMI, Inferior Wall Myocardial Infarction; LWMI, Lateral Wall Myocardial Infarction; OPD, Out-patient Department; PCI, Percutaneous Coronary Intervention; PWMI, Posterior Wall Myocardial Infarction; STEMI, ST Segment Elevation Myocardial Infarction; TIMI, Thrombolysis in Myocardial Infarction; STK, Streptokinase; TNK, Tenecteplase; RTP, Reteplase; VT, Ventricular Tachycardia; VF, Ventricular Fibrillation; CHB, Complete Heart Block; LVEF, Left Ventricular Ejection Fraction; LAD, Left Anterior Descending Artery; RCA, Right Coronary Artery; DM, Diabetes Mellitus
1. Introduction
Cardiovascular disease (CVD) is the leading cause of death globally1 and causes 12 million deaths throughout the world each year, in accordance with the third monitoring report of the World Health Organization.2 CVD is the leading cause of death in India, with coronary artery disease (CAD) accounting for a majority of the deaths.1,2 Based on the Treatment and outcomes of acute coronary syndromes (ACSs) in India (CREATE) registry3 published in 2008, the mean age of presentation with an ACSs was 57.5 years, which is 7–11 years younger than reports from the Western literature.
Traditionally CAD is considered to be a disease of the elderly. The cutoff age of 45 years has been used in most studies to define “young” patients with CAD or an acute myocardial infarction (AMI).4 Patient subgroups ≤35 years with CAD are at times referred to as “very young”5 CAD in the very young was found in only 1.5% of all patients with CAD.6 Clinical observation suggests that CAD in the very young is increasing in India. Many very young patients in India present with none or a single risk factor.7 Stable angina is uncommon, and the first presentation of CAD in the very young is usually a fully evolved MI.8 Presentation with an AMI in the very young shows a different clinical, angiographic and pathophysiological profile compared with the older cohorts.9 As classic coronary atherosclerotic plaque rupture is not common during the early decades of life, uncommon aetiologies may be considered.9 The limited angiographic data available seems to suggest a higher prevalence of single vessel CAD and less of multivessel CAD in the very young.10
The CREATE registry has previously reported that patients with ST elevation MI (STEMI) took a much longer time to reach the hospital and hence fewer patients received definitive treatment for MI in India compared with developed countries. All-cause mortality was higher in Indian patients, and more so in patients with poor socioeconomic status.3
STEMI in very young patients has devastating consequences and causes a huge loss to the economy and productivity. However, data regarding demographic, clinical and angiographic profile of this population is lacking in India as also in the western literature and characteristics of presentation with AMI in very young patients has been inadequately studied.11
The objective of our study was to assess the demographic, clinical, echocardiographic and angiographic profile and risk factor pattern of patients with AMI in ≤35 years of age in comparison with those >35 years of age.
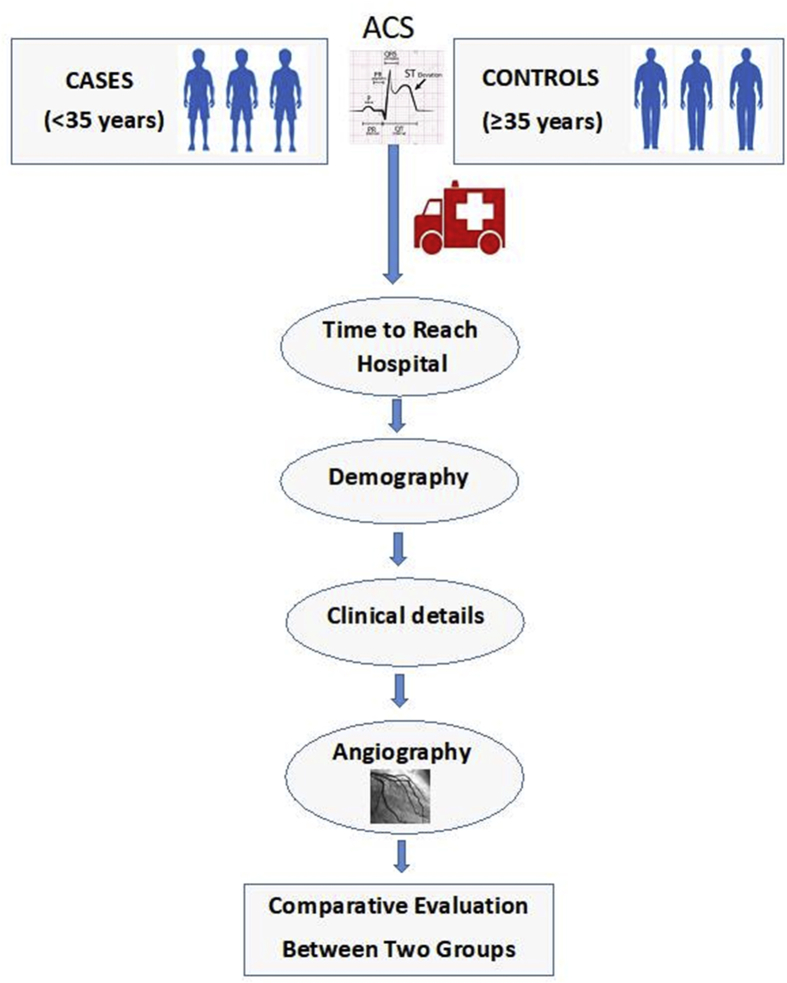
2. Materials and methods (Fig. 1)
Fig. 1.
Basic design of the study.
2.1. Study design, period and area
A descriptive comparative study with longitudinal design was carried out from January 2014 to October 2015 in the emergency room (ER) and out-patient department of the Gobind Ballabh Pant institute of Postgraduate Medical Education and Research (GIPMER), New Delhi.
2.2. Study subjects
A total of 102 consecutive patients aged ≥18years and ≤35years (cases) diagnosed to have AMI during our study period were included in our study. One hundred four patients >35 years diagnosed to have AMI were evaluated as the comparative group (controls) to study the differences in clinical risk factors, demographics, echocardiographic and angiographic findings and outcomes. Patients suspected to have myocarditis (diagnosed clinically by history of (h/o) viral prodrome, h/o fever preceding for days to weeks, atypical or nonanginal chest pain, global hypokinesia on echocardiography) were excluded from our study.
2.3. Data collection
MI was diagnosed in accordance with the Third Universal Definition of MI.12 Patient's history was documented in detail and brief focused clinical examination was performed. Current smoking was defined as a personal h/o smoking in the past 12 months. Family h/o CAD was defined as a h/o ischemic heart disease (IHD) in first-degree relatives (men <55 years of age or women <65 years of age). Outside food consumption besides home cooking was considered to be present if outside food was consumed at least once a week. The chain of events from symptom onset to arrival in ER was serially recorded. Socioeconomic status categorization was carried out in accordance with the updated B G Prasad socioeconomic classification 2014.13 Psychosocial history was recorded as per parameters used in Effect of Potentially Modifiable Risk Factors Associated with Myocardial Infarction INTERHEART study group14 that included stress at home, stress at work place, financial stress and depression. Two-dimensional echocardiography was performed in all of the study subjects before thrombolysis or percutaneous coronary intervention (PCI) using the Philips SONOS 5500 machine. Invasive coronary angiography (CAG) via femoral arterial access was performed in most of the patients either as a part of primary/rescue PCI or before discharge if patient was already thrombolyzed or managed conservatively.
Data regarding thrombolysis in MI flow characteristics, presence of calcium, and presence of thrombus was recorded. Obstructive CAD was considered to be present if ≥ 75% diameter stenosis was present on visual assessment in one of the major epicardial coronary arteries. Multivessel disease was defined as ≥ 50% stenosis of ≥2 major epicardial coronary arteries. Patients were treated in accordance with the latest MI management guidelines.15 Routine blood investigations were performed at the time of admission. Informed consent was obtained from all subjects and controls as per the existing norms of institutional ethics committee.
2.4. Statistical analysis
Continuous variables were expressed as mean and standard deviation, whereas categorical variables were expressed as numbers and percentages. Continuous variables were compared between cases and controls using an unpaired t-test and categorical variables using chi-squared or Fisher's exact test. Statistical tests were performed using Statistical Package for Social Sciences (SPSS) 20 and a 2-sided p value ≤ 0.05 was considered statistically significant.
3. Results
Between January 2014 and October 2015, a total of 206 patients with AMI who met the study criteria were enrolled and followed up.
3.1. Demographic profile of the study subjects (Table 1)
Table 1.
Distribution of study subjects and controls in accordance with demographic parameters.
| Variables | ≤35years (102) n (%) | >35 years (104) n (%) | p value |
|---|---|---|---|
| Mean Age | 28.52 ± 4.18 | 52.38 ± 9.65 | |
| Gender | |||
| Male | 99 (97.1) | 90 (86.5) | 0.006∗ |
| Female | 3 (2.9) | 14 (13.5) | |
| Education | |||
| Illiterate | 10 (9.8) | 23 (22.1) | 0.054 |
| Upto middle school | 36 (35.3) | 31 (29.8) | |
| Above middle school | 56 (54.9) | 50 (48.1) | |
| Occupation | |||
| Employed | 74 (68.2) | 77 (82.9) | 0.216 |
| Unskilled | 13 (17.1) | 25 (20.8) | |
| Unemployed | 15 (16.7) | 22 (20.3) | |
| Socioeconomic status | |||
| Upper + upper middle | 16 (16.8) | 18 (17.2) | 0.002∗ |
| Middle | 44 (32.7) | 22 (33.3) | |
| Lower middle + lower | 42 (52.5) | 64 (53.5) | |
| Domicile | |||
| Urban | 51 (50%) | 38 (36.5%) | 0.146 |
| Semiurban | 33 (32.4%) | 44 (42.3%) | |
| Rural | 18 (17.6%) | 22 (21.2%) | |
p <0.05 signifies bold.
Among the patients enrolled in the study, 102 were ≤35years (cases) and 104 were >35 years (controls). Age varied from 18 to 35 years with a mean age of 28.52 ± 4.18 years among the cases and 36–75 years with a mean age of 52.38 ± 9.65 years among the controls. Males were likely to be younger than females in both groups (among the cases: mean age of males-28.45 ± 4.12 years and mean age of females-30.6 ± 4.16 years, among controls: mean age of males-52.07 ± 9.3 years and mean age of females- 54.29 ± 10.55 years). Among the total subjects, 91.7% (189/206) were males, with a larger proportion of males among the cases (97.1% among cases and 86.5% among control group) and the difference was found to be statistically significant (p = 0.006). MI in general affected significantly greater number of males compared with females (p = 0.006).
All of the subjects among the cases and controls were of South East Asian origin. Most of the subjects among the cases belonged to the urban and most of the controls belonged to the semi-urban domicile. The representation of the rural domicile was low among both groups.
Approximately 9.8% of subjects were illiterate and 54.9% were educated above middle school among the cases. Among the controls 22.1% were illiterates and 48.1% were educated above middle school. This difference in the educational status did not reach statistical significance. A majority of the cases were employed and the situation was similar among the controls. Among the cases 16.8% subjects belonged to the upper and upper middle class, 32.7% belonged to the middle class and 52.5% belonged to the lower and lower middle class of socioeconomic status. Among the controls 17.2% belonged to the upper and upper middle class, 33.3% belonged to the middle class and 53.5% belonged to the lower middle and lower class. Around 60% of the cases belonged to either upper or middle class, whereas almost 80% of the controls belonged to lower or middle class. Half of the cases were urban, whereas 36.5% of the controls were urban; 32.4% and 17.5% of the cases and 42.3% and 21.2% of the controls belonged to the semi-urban and rural domicile, respectively. The difference was not statistically significant.
3.2. Traditional risk factors of CAD (Table:2)
Table 2.
Distribution of study subjects and controls in accordance with various traditional risk factors.
| Risk factors | ≤35years (102) n (%) | >35 years (104) n (%) | p value | |
|---|---|---|---|---|
| Diabetes mellitus | 6 (5.9) | 22 (21.2) | 0.001∗ | |
| Hypertension | 10 (9.8) | 25 (24.0) | 0.007∗ | |
| Smoking (current) | 70 (68.6) | 64 (61.5) | 0.286 | |
| Mean BMI (kg/m2) | 24.74 | 24.78 | 0.771 | |
| Tobacco chewer | 11 (10.8) | 5 (4.8) | 0.109 | |
| Past h/o IHD/CAD/TIA/ISCHEMIC STROKE | 7 (6.9) | 3 (2.9) | 0.293 | |
| Family h/o IHD/CAD | 28 (27.5) | 21 (20.2) | 0.058 | |
| Psychosocial stress | 49 (48) | 86 (82.7) | 0.0001∗ | |
| Type of diet | Veg | 24 (23.5) | 58 (55.8) | 0.0001∗ |
| Nonveg/mixed | 78 (76.5) | 46 (44.2) | ||
| Cooking oil | Mustard oil | 61 (59.8) | 67 (64.4) | 0.07 |
| Sunflower oil | 32 (31.4) | 35 (33.7) | ||
| Others | 9 (8.8) | 2 (1.9) | ||
| Outside food (at least once per week) | 64 (62.7) | 43 (41.3) | 0.001∗ | |
IHD, ischemic heart disease; CAD, coronary artery disease.
p <0.05 signifies bold.
The prevalence of Diabetes mellitus and hypertension among cases was 5.9% and 9.8%, respectively which was in contrast to 21.2% and 24.0%, respectively among controls. This difference was statistically significant. Around two-third (68.6%) of the cases and 61.5% of controls were current smokers. This difference was not statistically significant. Tobacco chewers represented 10.8% of cases and 4.8% of control, respectively. Cases more frequently had a family h/o IHD (27.5%) as compared with controls (20.5%) but the difference did not attain statistical significance. The mean body mass index (BMI) was 24.74 ± 4.3 kg/m2 in both the groups. Around half (48%) of the cases had psychosocial stress, whereas 82.7% of controls had some form of psychosocial stress and this difference was highly significant (p = 0.0001). Approximately 34.6% (17/49) of cases and 37.2% (32/86) of controls who had positive psychosocial history had more than one psychosocial stress parameters present.
A majority (76.5%) of the cases were nonvegetarians, whereas a majority of the controls were vegetarians (55.8%) (p = 0.0001) and around 60% of both cases and controls used mustard oil as the main cooking oil. Food from outside of home was consumed at least once per week among 62.7% of cases and 41.3% of controls. This difference was statistically significant.
3.3. Clinical and management profile of the study subjects (Table 3, Table 4)
Table 3.
Clinical profile of study subjects and controls.
| Variables | ≤35years (102) n (%) | >35 years (104) n (%) | p value | |||
|---|---|---|---|---|---|---|
| Type of STEMI | AW/AS/AL MI | 68 (73.1) | 46 (48.4) | 0.005∗ | ||
| IWMI | 21 (22.6) | 44 (46.3) | ||||
| PWMI | 1 (1.1) | 0 (0) | ||||
| LWMI | 5 (5.4) | 5 (5.3) | ||||
| NSTEMI | 9 (8.8) | 9 (8.7) | ||||
| First symptom | Chest pain | 99 (97.1) | 94 (90.4) | 0.048∗ | ||
| Others | 3 (2.9) | 10 (9.6) | ||||
| Time of onset | 8pm to 8am | 62 (60.8) | 54 (58.56) | 0.2 | ||
| 8 AM to 8PM | 40 (39.2) | 50 (45) | ||||
| Preceding activity | Sleep Nonexertional activity exertional activity |
25 (24.5) | 38 (36.5) | 0.173 | ||
| 56 (54.9) | 48 (46.2) | |||||
| 21 (20.6) | 18 (17.3) | |||||
| First Medical Contact | Clinic | 60 (58.8) | 86 (82.7) | <0.01∗ | ||
| Hospital Without PCI | 40 (39.2) | 0 | ||||
| Hospital With PCI | 2 (2) | 18 (17.3) | ||||
| Median time taken for FMC (mins) | 30 (10–720) | 40 (10–120) | ||||
| Reason for delay (FMC >30 min) (N=46) | Misinterpretation of Symptoms | 28 (58.3) | 23 (33.8) | 0.004∗ | ||
| Lack Of Medical Facility | 6 (12.5) | 16 (23.5) | ||||
| Lack Of Transport | 1 (2.1) | 14 (20.6) | ||||
| Ignorance | 13 (27.1) | 15 (22.1) | ||||
| Median Time taken to reach final ER (hours) | 5 | 6 | ||||
| Killip class | I | 89 (87.3) | 78 (75) | 0.07 | ||
| II | 11 (10.8) | 21 (20.2) | ||||
| III | 1 (1) | 4 (3.8) | ||||
| IV | 1 (1) | 1 (1) | ||||
STEMI, ST segment elevation myocardial infarction; LWMI, lateral wall myocardial infarction; PWMI, posterior wall myocardial infarction.
p <0.05 signifies bold.
Table 4.
Management profile of study subjects.
|
Medications Received before presenting to ER |
≤35years (102) n (%) |
>35 years (104) n (%) |
|
| None | 27 (26.5%) | 32 (30.8%) | |
| Aspirin ± Statin | 14 (13.7%) | 21 (20.2%) | |
| Aspirin + Clopidogrel | 10 (9.8%) | 17 (16.3%) | |
| Aspirin + Clopidogrel + Statin | 45 (44.1%) | 26 (25%) | |
| Aspirin + Clopidogrel + Statin + Antithrombotics |
6 (5.9%) |
8 (7.7%) |
|
| The p-value is .06. | |||
|
Mode of Treatment At ER for STEMI patients |
≤ 35years (93) n (%) |
>35 years (95) n (%) |
|
| Thrombolysis | 30 (32.3%) | 24 (25.3%) | |
| Agent used for thrombolysis | STK | 21 (70%) | 12 (50%) |
| RTP | 4 (13.3%) | 8 (33.3%) | |
| TNK | 5 (16.7%) | 4 (16.7%) | |
| Primary PCI | 34 (36.6%) | 25 (26.3%) | |
| Conservative Management | 29 (31.2%) | 46 (48.4%) | |
| Reason for Conservative management | Not mentioned | 14 (48.3%) | 20 (43.5%) |
| Resolution of symptoms | 5 (17.2%) | 7 (15.2%) | |
| Not willing for admission | 4 (13.8%) | 4 (8.7%) | |
| OWP |
6 (20.7%) |
15 (32.6%) |
|
| The p-value is .05307. | |||
|
Medications received before discharge from hospital |
≤ 35years (102) n (%) |
>35 years (104) n (%) |
|
| Aspirin | 102 (100%) | 104 (100%) | |
| Thienopyridines | Clopidogrel | 97 (95.1%) | 104 (100%) |
| Prasugrel | 6 (5.9%) | 0 | |
| Statin | 102 (100%) | 104 (100%) | |
| ACEIs | 90 (88.2%) | 96 (92.3%) | |
| Β-blockers | 92 (90.2%) | 93 (89.4%) | |
| Anticoagulants | UFH | 4 (3.9%) | 13 (12.5%) |
| LMWH | 87 (85.3%) | 87 (83.6) | |
STEMI, ST segment elevation myocardial infarction; PCI, percutaneous coronary intervention; TNK, tenecteplase; RTP, reteplase.
STEMI accounted for a majority of presentation in both cases (91.2%) and controls (91.3%) as compared with non ST elevation myocardial infacrtion (NSTEMI). Among the cases, 91.2% were diagnosed to have STEMI and 8.8% as NSTEMI. A majority of the cases (73.1%) had anterior wall MI (AWMI) followed by inferior wall MI (IWMI) (22.6%). This was significantly different from the controls where 48.4% had AWMI and 46.3% had IWMI (p = 0.001). Only a minor percentage was formed by lateral wall MI and posterior wall MI among both groups. Chest pain (97.1%) was the most common symptom among the cases, as well as controls (97.1% among cases and 90.4% among controls). This difference was marginally significant. Dyspnea, palpitations, and syncope were the first symptoms in very small number of cases and controls. Most cases (60.8%), as well as controls (54%) had symptoms between 8 PM and 8AM. Nonexertional activity preceded the symptoms in 54.9% and 46.2% of cases and controls, respectively. Symptoms during sleep occurred in 24.5% of cases and 36.5% of controls, respectively. Exertional activity preceded symptoms in 20.6% and 17.3% of cases and controls, respectively. First medical contact (FMC) was at a clinic in 58.8% of cases and in 82.7% of the controls. This difference was statistically significant. Only 2% of cases and 17.3% of controls had FMC with a hospital where PCI facility was available. Median time taken for the patient to reach the first health care point of contact after onset of symptoms (FMC) was 30 min in cases and 40 min for controls. There was a significant difference in the number of cases vs. controls who achieved delayed FMC (defined as >30min from onset of symptoms); the most common reason for delay among both cases and controls was misinterpretation of symptoms (58.3% among cases and 33.8% among controls, p = 0.004). The median time taken to reach final ER for cases was 6 h and 5 h for controls.
3.4. Medical therapy among cases and controls
Less than half (44.1%) of the cases and only 25% of the controls received dual antiplatelet therapy (with aspirin and clopidogrel or prasugrel) and statin before arriving to ER. Antithrombotic therapy in form of low-molecular-weight heparin was received by 5.9% and 7.7% of cases and controls, respectively. A substantial number of cases (26.5%) and controls (30.8%) did not receive any medication before arriving to ER. A majority of cases (87.3%) and controls (75%) were in Killip Class I. Among cases with STEMI (n = 93) 62.7% received definitive treatment (thrombolysis 29.4%, primary PCI 33.3%), whereas 47.1% of controls with STEMI (n = 95) received definitive treatment (thrombolysis 23.1%, primary PCI 24%) of controls (p = 0.01). More controls were treated conservatively as compared with cases (48.4%Vs 31.2%, p = 0.01). The major reason for the conservative therapy was that both cases, as well as controls were either out of window period and symptom free at presentation or they did not consent for either thrombolysis or PCI.
In 70% of the cases, thrombolytic agent used was streptokinase (STK) followed by tenecteplase (TNK) (16.7%) and reteplase (RTP) (13.3%). Among the controls, the use of STK was 50%, 33.3% RTP and 16.7% TNK. All of our study patients including cases and controls received aspirin, clopidogrel or prasugrel and statins before discharge.
3.5. Complications of MI (Table .6)
Table 6.
Complications among cases and controls.
| COMPLICATION | CASES(n = 102) | CONTROLS (n = 104) | p value |
|---|---|---|---|
| None | 95 (93.13%) | 93 (89.40%) | 0.13 |
| Acute MR (moderate/severe) | 0 | 0 | |
| VSR/FWR | 0 | 0 | |
| VT/VF | 3 (2.93%) | 4 (3.85%) | |
| Acute LVF | 4 (3.9%%) | 5 (4.80%) | |
| High-grade A-V block/CHB | 0 | 2 (1.93%) | |
| Deaths | 3 (2.93%) | 7 (6.7%) |
VT/VF, ventricular tachycardia/ventricular fibrillation; LVF, left ventricular failure; CHB, complete heart block.
Among all cases, complications occurred in only seven patients: 3 patients had ventricular tachycardia/ventricular fibrillation (VT/VF) and four patients developed acute left ventricular failure (LVF). Among the controls, 11 patients had complications (5 had LVF, 4 developed VT/VF and 2 developed Complete Heart Block (CHB)). There were 3 deaths among the cases and 7 deaths among the controls. The differences were not statistically significant for any of the complications.
4. Left ventricular ejection fraction
The mean left ventricular ejection fraction (LVEF) among cases was 41.8% compared with 34.9% among controls (p = 0.0001). When only patients with STEMI were considered, the mean LVEF among cases was 40.6% compared with 34.9% among controls.
5. Angiographic details (Table 5)
Table 5.
Angiographic findings of the study subjects and controls.
| VARIABLES | ≤35years(N=97) | >35 years (104) n (%) | p value | |
|---|---|---|---|---|
| CAG Findings | Normal | 3 (3.1%) | 6 (5.8%) | 0.0001∗ |
| Recanalised/nonobstructive CAD | 16 (16.5%) | 0 (0%) | ||
| Obstructive CAD | 42 (43.3%) | 43 (41.3%) | ||
| Total occlusion | 36 (37.1%) | 55 (52.9%) | ||
| No. of deceased vessels | SVD | 83 (85.6%) | 67 (64.4%) | 0.02∗ |
| MVD | 14 (14.4%) | 37 (36.6%) | ||
| Artery involved∗(N = 97) | LAD | 81 (83.5%) | 65 (62.5%) | 0.03∗ |
| LCX | 11 (11.3%) | 31 (29.8%) | 0.004∗ | |
| RCA | 16 (16.5%) | 50 (48.1%) | 0.0001∗ | |
| DIAGONAL | 4 (4.1%) | 7 (6.7%) | 0.3 | |
CAD, coronary artery disease; CAG, coronary angiography; SVD, single vessel disease; LAD, left anterior descending; RCA, right coronary artery.
p <0.05 signifies bold.
CAG was performed in 95.1% (97/102) of the cases and all 104 of controls. Normal or recanalised arteries was seen among 19.6% of cases and 5.8% of controls (p = 0.0001). Total occlusion of the infarct-related artery was found among 37.1% of cases and 52.9% of controls. Single vessel disease (SVD) was significantly more common (85.6%) than multi vessel disease (MVD) (14.4%) among the cases and controls but the percentage of SVD was lower (64.4% vs 85.5%) among the controls and MVD higher (36.6% vs 14.4%) as compared with cases. The most common artery involved was left anterior descending (LAD) among the cases (83.5%) and controls (62.5%). Right coronary artery (RCA) involvement was seen in 16.5% of cases and 48.1% of the controls.
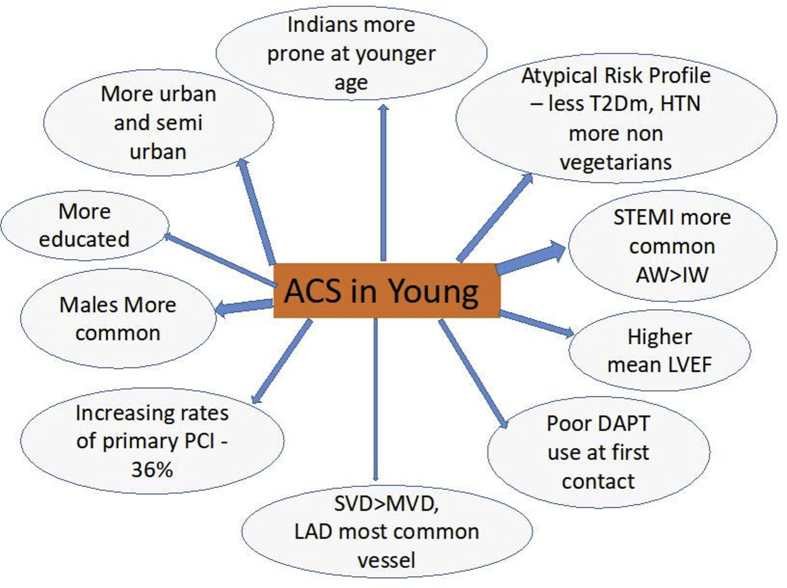
6. Discussion (Fig. 2)
Fig. 2.
Principle study findings depicting differences in profile of very young patients versus older patients presenting with ACS. ACSs, acute coronary syndromes.
In a first such report from northern India, the present study compared the demographic, clinical and coronary angiographic profiles of very young patients aged ≤35 years with those >35 years of age who presented with AMI at a large, high volume, academic, tertiary referral center. Both of the groups comprised mainly of North Indian patients.
The mean age of cases in the present study was 28.52 years which was lower compared with a retrospective French series that described 40 patients under 36 years of age presenting with MI.16 Mean age in this series was 31.3 years. It is interesting to note that CAD affects the Indian population at younger age compared with the western population even among the very young.
Consistent with prior literature, the present study found a preponderance of males among those presenting with AMI even among the very young.16, 17, 18 The CREATE registry also had a male preponderance with 81.5% of patients with STEMI being male.3 Similarly, the Kerala ACS registry also had a male preponderance with 77.5% of patients with STEMI being males.19 Females in this age group are usually protected from CAD. Other important reasons for the under representation of females might be the underutilization of health-care services in the society for female patients.
Our study found that MI in the very young mainly manifests as STEMI, in particular AWMI. However, we found a significantly higher number of patients with STEMI when compared with the CREATE registry and the Kerala ACS registry. In CREATE registry, 60.6% presented with STEMI, whereas in Kerala ACS registry19 37% of total patients with ACS presented with STEMI. And in Global Registry of Acute Coronary Events (GRACE) study, STEMI cases ranged between 30 and 40%.20 In the present study, most of the cases (73.1%) had AW/AS/AL MI and 22.6% had IWMI, whereas among the controls 48.4% had AWMI and 46.3% had IWMI. This difference is worth noting as very young MI seem to have a predilection for AWMI. Similar results were seen in other studies from Spain and Israel.18,21
Illiterate status was lower and graduates were more among cases and the reverse was true for controls. This difference tended towards statistical significance. This is interesting and reflects the role of education in seeking health care and also might reflect higher stress among cases. This aspect of demography was not examined in the CREATE Registry. In the Kerala ACS registry STEMI patients formed 37% of the total subjects and among the patients with STEMI, 22.5% patients were illiterate and 18.4% patients had primary education (class 1–7), 40.7% had secondary education (class 8–11) and 18.3% were secondary graduate and higher.19
Subjects with middle and lower middle socioeconomic group were significantly higher among cases, as well as controls. In the CREATE registry, three-fourth of the patients were also from lower middle and poor socioeconomic status.3 The reasons might include unhealthy food habits, addictions such that to tobacco and psychosocial stress which are more prevalent in middle and lower socioeconomic class.
Urban and semi-urban populations were predominant in the present study, as well as in the CREATE registry (Table 1). The main reason for this might be better access to health care for urban and semi-urban population and also a higher incidence of CAD among the urban population due to unhealthy food and lifestyle. Rural population might be under represented in the studies due to negligence and misinterpretation of the symptoms and also due lack of health-care facilities around the clock and a weak referral system including a lack of transportation facilities.
The proportion of patients presenting with AMI and coexistent DM or hypertension were significantly fewer among the cases as compared with controls. This suggests that the very young patient with AMI does not have a typical risk profile as compared with older adults. The percentage of smokers was similar among both groups (68.6% among cases and 61.5% among controls) and family h/o IHD was also not significantly different among the two groups. The proportions of DM and HTN among the cases were comparable with other studies.22 Previous studies have shown mixed results regarding the presence of a significant family h/o CAD.11,17 Even the mean BMI was also just above normal in overweight category for Asians. In the CREATE registry where 60.6% patients presented with STEMI, 26.9% patients were known diabetics and 31.4% patients were known hypertensives which is significantly different from the risk factor profile of our very young MI group. Almost 44.7% patients in the STEMI subgroup of CREATE registry were current or past smoker,3, whereas the percentage was higher in our study indicating that the prevalence of smoking has increased or it may be more prevalent in this part of the country. The rates of DM, HTN, and smoking in Kerala ACS registry were 34%, 55%, and 36%, respectively.19
The numbers of nonvegetarians were significantly higher in our study among the cases as compared with the controls. Meat (especially red meat) has high content of cholesterol and saturated fatty acids, both of which have been shown to be positively associated with plasma low-density lipoprotein concentrations and the risk of CAD. Almost 60% of the patients among both cases and controls used mustard oil in their diet. There was use of other oils along with mustard oil. Mustard oil being economical still forms the major part of oil consumption. The amount of erucic acid in the mustard oil used by patients is also not known.23 The higher content of long chain monounsaturated fatty acids has been associated with cardiac steatosis and has a possible increase in incident congestive heart failure.24
Almost half of the cases and more than three-fourths of the controls had a h/o psychosocial stress in some form. Even in the INTERHEART study, odds of any form stress whether at work or home or financial and major life events was higher among cases than among the control group.14 This reflects the drawbacks of the typical urban stressful and demanding lifestyle.
Similar to the findings in previous studies, a majority of cases, as well as controls had chest pain as first symptom of MI in the present study.10 Dyspnea and palpitations formed only a minor percentage of the symptoms. In addition, similar to that in other studies, symptoms occurred in most of the subjects (both cases and controls) during sleep or nonexertional activity and less during exertion.25 The median time taken to visit FMC for cases was 30 min and for controls it was 40 min and median time taken from first presentation to final ER was 5 h for cases and 6 h for controls. The difference between the cases and the control group was not significant which implies that age of the patients did not trigger a faster response from both patients and immediate caregivers and patients took almost a similar time to reach the FMC and the final ER. It was comparable to that in the CREATE registry (median 5 h).3 It is worth mentioning here that despite a decade having passed since the CREATE registry (2008) and a tremendous advancement in the understanding of MI and need for early revascularization, the time for final ER presentation for definitive treatment of a patient with STEMI remains 5 h. This is a finding of great significance because it reflects the low level of awareness in the general public about the symptoms and also emphasizes the importance and role of small health centers and clinics for early referral of the patients. Although the western world has managed to enforce and achieve strict timelines for STEMI management through coordinated efforts through administrative changes, legislative efforts and health-care services, India lags way behind. Most of the patients used self-mode of transport for transfer to hospital which was also the case in CREATE3 and Kerala ACS registry.19 In our study, the most common mode of transport for the cases was self (52.9%), whereas in the control group it was the ambulance (34.6%). This difference was statistically significant. Ambulance use was very low among the cases. Good Emergency Medical Services services form the backbone of the STEMI response team for rapid revascularization. It is quite evident from our study, as well as the CREATE and Kerala ACS registries that we desperately need a fast and responsive fleet of ambulance services and Emergency Response Teams for a dedicated STEMI program.
Less than half (44%) of the cases and only one-fourth of the controls received dual antiplatelet at the FMC before presenting to the final ER. This is a dismal number and reflects a lack of awareness among physicians at different levels of healthcare. This could be due to failure to recognize ACS/STEMI, lack of knowledge about the first aid in a patient with STEMI, or possibly non availability of these essential medications at the peripheral centers. However, the difference between cases and controls receiving DAPT and statin was significant possibly because of higher education and socioeconomic status and urban origin of the cases. At discharge, all patients including cases and controls received DAPT and statins. However, use of ACEIs and beta blockers was much higher when compared with CREATE and Kerala ACS registries.
There were numerically fewer in-hospital deaths in the cases group as compared with the control group (Table 6) (three among cases and seven among controls) signifying that younger patients may have a better prognosis in case of STEMI. The 30-day mortality in patients with STEMI in the CREATE registry was 9%3 and in Kerala ACS registry it was 8.2%.19 Although no follow up was carried out at 30 days in our study similar to that in CREATE and Kerala ACS registry, but inference can be drawn from the in-hospital data with fair confidence that “very young MI” patients perform better as compared with older patients. This observation can be considered hypothesis generating and should be tested in a larger sample size. There was no significant difference among the two groups with respect to other complications such as LVF, VT/VF, and AV Blocks.
The mean LVEF was 41.8% among cases and 34.9% among the controls. This is of great importance because in spite of having more number of STEMI and in particular ST elevation AWMI patients, LVEF is higher among the young MI group. This might be a unique feature of young MI or partly explained by the fact that a greater number of patients in the young MI group presented earlier to the ER and received definitive treatment for MI and less frequently had multivessel involvement. Similar to the present study, another Swiss study of STEMI patients <30 years showed higher LVEF.5 Similar to that in previous studies, left anterior descending artery was the most common vessel involved in both groups followed by RCA.11 Multivessel disease was less frequent (14.4% among cases and 36.6% among controls) as compared with other (western) studies involving very young patients with MI (≤35 years).
Relatively more cases underwent primary PCI (36% vs. 26%) as compared with the controls. This might be due to younger age of presentation, better decision making and better level of education and higher socioeconomic class. The rates of primary PCI in the CREATE registry were 8%. The findings of our study represent a major advance in identifying the patterns of STEMI management. STK was the most common thrombolytic agent used (rather than TNK or RTP) in both the groups. This might be due to more widespread availability and low cost of STK. Around 20% of the patients had recanalized coronary arteries. The prevalence of MI with nonobstructive CAD is between 5% and 25%, and it is quiet common among young patients.22
6.1. Study limitations
This is the first study of very young patients with MI from northern India. However, small sample size, single-centre study, lack of follow-up beyond outcomes at index hospitalization are major limitations of this study. The results cannot be generalized to other populations.
7. Conclusions
This is the first study from south east Asia that describes demographic, clinical and coronary angiographic profile in very young patients ≤35 years presenting with AMI. Our study suggests that the major modifiable risk factor for MI in very young patients appears to be smoking. Hence focused efforts should be made to modify these risk factors in this population through education and behavioral modification. Further, a significant improvement in health-care delivery systems at all levels is required to improve management of this subgroup of patients which could have major societal implications. The findings of this study should set the stage for a larger registry which will provide greater insights into the unique profile of CAD in India in general and young CAD in particular.
Funding
None.
Conflict of interest
The authors declare that they have no conflicts of interest with respect to the present submission.
References
- 1.Lopez A.D., Mathers C.D., Ezzati M., Jamison D.T., Murray C.J.L. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006 May 27;367(9524):1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 2.Reddy K.S. Cardiovascular diseases in India. World Health Stat Q. 1993;46(2):101–107. [PubMed] [Google Scholar]
- 3.Xavier D., Pais P., Devereaux P.J. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008 Apr 26;371(9622):1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 4.Gupta R., Joshi P., Mohan V., Reddy K.S., Yusuf S. Epidemiology and causation of coronary heart disease and stroke in India. Heart. 2008 Jan 1;94(1):16–26. doi: 10.1136/hrt.2007.132951. [DOI] [PubMed] [Google Scholar]
- 5.Puricel S., Lehner C., Oberhänsli M. Acute coronary syndrome in patients younger than 30 years--aetiologies, baseline characteristics and long-term clinical outcome. Swiss Med Wkly. 2013;143:w13816. doi: 10.4414/smw.2013.13816. [DOI] [PubMed] [Google Scholar]
- 6.Wolfe M.W., Vacek J.L. Myocardial infarction in the young. Angiographic features and risk factor analysis of patients with myocardial infarction at or before the age of 35 years. Chest. 1988 Nov;94(5):926–930. doi: 10.1378/chest.94.5.926. [DOI] [PubMed] [Google Scholar]
- 7.Dwivedi S., Dwivedi G., Chaturvedi A., Sharma S. Coronary artery disease in the young : Heredofamilial or faulty life style or both. J Indian Acad Clin Med. 2000;1(3):8. [Google Scholar]
- 8.Schoenenberger A.W., Radovanovic D., Stauffer J.-C. Acute coronary syndromes in young patients: presentation, treatment and outcome. Int J Cardiol. 2011 May 5;148(3):300–304. doi: 10.1016/j.ijcard.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 9.Garoufalis S., Kouvaras G., Vitsias G. Comparison of angiographic findings, risk factors, and long term follow-up between young and old patients with a history of myocardial infarction. Int J Cardiol. 1998 Nov 30;67(1):75–80. doi: 10.1016/s0167-5273(98)00194-6. [DOI] [PubMed] [Google Scholar]
- 10.Gaeta G., De Michele M., Cuomo S. Arterial abnormalities in the offspring of patients with premature myocardial infarction. N Engl J Med. 2000 Sep 21;343(12):840–846. doi: 10.1056/NEJM200009213431203. [DOI] [PubMed] [Google Scholar]
- 11.Zimmerman F.H., Cameron A., Fisher L.D., Grace N. Myocardial infarction in young adults: angiographic characterization, risk factors and prognosis (coronary artery surgery study registry) J Am Coll Cardiol. 1995 Sep;26(3):654–661. doi: 10.1016/0735-1097(95)00254-2. [DOI] [PubMed] [Google Scholar]
- 12.Kristian Thygesen, Alpert Joseph S., Jaffe Allan S., Simoons Maarten L., Chaitman Bernard R., White Harvey D. Third universal definition of myocardial infarction. Circulation. 2012 Oct 16;126(16):2020–2035. doi: 10.1161/CIR.0b013e31826e1058. [DOI] [PubMed] [Google Scholar]
- 13.Mangal A., Kumar V., Panesar S., Talwar R., Raut D., Singh S. Updated BG Prasad socioeconomic classification, 2014: a commentary. Indian J Publ Health. 2015 Jan 1;59(1):42. doi: 10.4103/0019-557X.152859. [DOI] [PubMed] [Google Scholar]
- 14.Yusuf S., Hawken S., Ounpuu S. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004 Sep 11;364(9438):937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 15.O'Gara Patrick T., Kushner Frederick G., Ascheim Deborah D. ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary. Circulation. 2013;127(4):529–555. doi: 10.1161/CIR.0b013e3182742c84. 2013 Jan 29. [DOI] [PubMed] [Google Scholar]
- 16.Gallet B., Leroy G., Saudemont J.P. [Myocardial infarction in the young subject: a medium-term clinical and coronary angiographic study in 40 patients under 36 years of age. Comparison with coronary angiographic data of myocardial infarction in patients after 50 years of age] Arch Mal Coeur Vaiss. 1984 Jan;77(1):27–36. [PubMed] [Google Scholar]
- 17.Glover M.U., Kuber M.T., Warren S.E., Vieweg W.V. Myocardial infarction before age 36: risk factor and arteriographic analysis. Am J Cardiol. 1982 May;49(7):1600–1603. doi: 10.1016/0002-9149(82)90234-x. [DOI] [PubMed] [Google Scholar]
- 18.Weinberger I., Rotenberg Z., Fuchs J., Sagy A., Friedmann J., Agmon J. Myocardial infarction in young adults under 30 years: risk factors and clinical course. Clin Cardiol. 1987 Jan;10(1):9–15. doi: 10.1002/clc.4960100104. [DOI] [PubMed] [Google Scholar]
- 19.Mohanan P.P., Mathew R., Harikrishnan S. Presentation, management, and outcomes of 25 748 acute coronary syndrome admissions in Kerala, India: results from the Kerala ACS Registry. Eur Heart J. 2013 Jan;34(2):121–129. doi: 10.1093/eurheartj/ehs219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fox K.a.A., Eagle K.A., Gore J.M., Steg P.G., Anderson F.A. GRACE and GRACE2 investigators. The global registry of acute coronary events, 1999 to 2009--GRACE. Heart. 2010 Jul;96(14):1095–1101. doi: 10.1136/hrt.2009.190827. [DOI] [PubMed] [Google Scholar]
- 21.Badui E., Rangel A., Valdespino A. [Acute myocardial infarct in young adults. A report of 142 cases] Arch Inst Cardiol Mex. 1993 Dec;63(6):529–537. [PubMed] [Google Scholar]
- 22.Kaul U., Dogra B., Manchanda S.C., Wasir H.S., Rajani M., Bhatia M.L. Myocardial infarction in young Indian patients: risk factors and coronary arteriographic profile. Am Heart J. 1986 Jul;112(1):71–75. doi: 10.1016/0002-8703(86)90680-0. [DOI] [PubMed] [Google Scholar]
- 23.Rastogi T., Reddy K.S., Vaz M. Diet and risk of ischemic heart disease in India. Am J Clin Nutr. 2004 Apr 1;79(4):582–592. doi: 10.1093/ajcn/79.4.582. [DOI] [PubMed] [Google Scholar]
- 24.Imamura F., Lemaitre R.N., King I.B. Long-chain monounsaturated fatty acids and incidence of congestive heart failure in two prospective cohorts. Circulation. 2013 Apr 9;127(14):1512–152218. doi: 10.1161/CIRCULATIONAHA.112.001197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Matthias A.T., de Silva D.K.N., Indrakumar J., Gunatilake S.B. Physical activity levels of patients prior to acute coronary syndrome – experience at a tertiary care hospital in Sri Lanka. Indian Heart J. 2018 May 1;70(3):350–352. doi: 10.1016/j.ihj.2017.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]