Abstract
Hospitals play a critical role in providing communities with essential medical care during all types of disaster. Depending on their scope and nature, disasters can lead to a rapidly increasing service demand that can overwhelm the functional capacity and safety of hospitals and the healthcare system at large. Planning during the community outbreak of coronavirus disease 2019 (Covid-19) is critical for maintaining healthcare services during our response. This paper describes, besides general measures in times of a pandemic, also the necessary changes in the invasive diagnosis and treatment of patients presenting with different entities of acute coronary syndromes including structural adaptations (networks, spokes and hub centres) and therapeutic adjustments.
Keywords: Covid-19, pandemic, medical response actions, preparedness
The general approach
Critical preparedness, readiness and response actions for Covid-19
Pandemic preparedness is an integral part of preparedness to threats to human health caused by any emergency; for example, incapacitating outbreaks of any disease or the occurrence of natural disasters or chemical incidents. Pandemic plans are typically developed to prepare for, or respond to, an influenza (‘flu’) epidemic.1,2 Pandemic influenza has the potential to place an unprecedented strain on our healthcare system.2 Throughout history, they have led to widespread illness and death.3 The newly emerged coronavirus (now called SARS-CoV-2, causing corona virus disease 2019 (Covid-19)) is a respiratory disease that is much like the flu, but worse.4–6 Each response is different, even if the same basic principles apply.7,8
Planning for a community outbreak of coronavirus disease 2019 (Covid-19) is critical for maintaining healthcare services during a response. Flexibility is essential to any pandemic influenza planning effort, as plans will need to be easily and quickly adapted to the specific needs of an evolving pandemic, as epidemiological and laboratory data emerge.5 In the end, the impact of this epidemic depends on the number of people infected, the infection’s transmissibility, including the role that asymptomatic or presymptomatic infected people play in transmitting the virus to others, and the full spectrum of disease severity.9,10 While the majority of cases (up to 80%) of Covid-19 are milder respiratory infections and pneumonias, severe illness and death is more common among the elderly with other chronic underlying conditions, with these risk groups accounting for the majority of severe disease and fatalities to date.11,12 Forecasting, modelling and planning tools facilitate dynamic estimates of pandemic virus spread, burden and impact.9,10,13–15
The impact and risk assessment on health system capacity can be mediated by the application of effective infection prevention and control and surge capacity measures.9 Measures taken at this stage should ultimately aim at protecting the most vulnerable population groups from severe illness and fatal outcomes by reducing transmission and reinforcing healthcare systems.16 Community mitigation measures are the first line of defence against pandemic influenza, and may help reduce the spread of other respiratory infectious diseases, and improve awareness and implementation of non-pharmaceutical interventions by the general public and in key community settings (schools, childcare settings, workplaces, mass gatherings) to slow the spread of disease.9 Several countries have demonstrated that Covid-19 transmission from one person to another can be slowed.9,17 This critical time should allow the healthcare system (prehospital and inhospital) enough time to adapt their response appropriately, to organise (pre-)emergency care triage and deploy a maximum hospital capacity on healthcare units designated to care for Covid-19 cases, with a special focus on intensive care. Because of differences among hospitals (e.g. size of the hospital/community, scope of services), each hospital will need to adapt its response to meet its unique needs and circumstances.
True pandemic preparedness will require engaging the entire healthcare community, including and especially our first line response (i.e. general practitioners), and healthcare assets from across the spectrum of care will have to be prepared to meet the increased demands.18 The prevention and control of Covid-19 in hospitals and long-term care facilities (separate ‘clean areas’ from ‘dirty areas’) is an immediate priority in order to minimise the export of cases to other healthcare facilities and the community, to safeguard populations vulnerable to severe outcomes of infection (the non-cases), and to protect healthcare workers that provide care.18 Hospitals should ensure their staff are trained, equipped and capable of practices needed to prevent the spread of Covid-19 within the facility, to identify and isolate patients with possible Covid-19 (cases), to care for a limited to a large number of patients in the context of an escalating outbreak while maintaining adequate care for other patients (the non-cases).
In the aged Covid-19 resources and capacity are limited.19 Rational approaches should be implemented to prioritise high-yield actions, including the rational use of confirmatory testing, the rational use of personal protective equipment (PPE; see below) and hospitalisation and ventilator capacity.19,20 The highest priority for the use of N95 respirators (FFP2/3) is for healthcare workers, in particular those performing aerosol-generating procedures, including swabbing, intubation and aspiration (intensive care). In circumstances with capacity shortage, and strict implementation of social distancing measures (‘lock down’), surveillance should focus on severe acute or deteriorating respiratory infections, sentinel surveillance in outpatient clinics (separating cases, and non-cases), and (pro-)active telephone consultations especially focusing vulnerable populations (e.g. heart failure patients, immune compromised patients, the elderly).
Critical aspects from the hospital response plans
Hospital response plans have been described, and are relatively similar with respect to the main tasks of organisation, but may differ in detail depending on the individual situation in countries and regions.
Placement of patients in spatial separation
Frontline services (preferably before the patient enters the hospital: pre-triage by general practitioners, emergency department) serve for the early triage of patients with Covid-19 to prevent transmission to healthcare-workers and other patients.
Spatial area separation (‘patient cohorting’, isolating cases in the same designated unit, one or ward) is applied to separate acute respiratory infection from other patients. Strict policies (public, healthcare workers, patients) for access to the healthcare facilities and specific wards dedicated to Covid-19 should be applied to separate flows of cases and non-cases.18 Only cases that are proved negative will be transferred to non-Covid-19 wards, while patients tested positive will undergo special care.
Patients are encouraged in the use of respiratory hygiene during coughing and sneezing and are equipped with a surgical (FFP1) mask to reduce the dispersal of respiratory secretions containing potentially infectious particles.
Recommendations for the use of PPE and fit-testing of respirators
The constant availability and use of PPE (much of which is disposable) is essential during an outbreak, including the following: N95 respirators fitted tightly to the face (certified FFP2 or FFP3 masks, the latter for during aerosol-generating procedures: endotracheal intubation, cardiopulmonary resuscitation, bronchoscopy; if the mask gets wet or dirty with secretions, it must be changed immediately), goggles or face shields, long-sleeved gowns or scrub suits and disposable gloves.18 Adequate supplies of essential items required for PPE should be stocked, or easily made available. Healthcare workers’ compliance with the proper use of PPE should be monitored.
Clear policies and procedures are needed for putting on and removing PPE during an outbreak. Staff has to be trained and educated on every aspect of contaminated infectious diseases, including the proper use of PPE, risks to themselves and their families, and infection-control policies and procedures (e.g. train-the-trainer model, quality assurance monitoring).
For example, in the case of Covid-19, before entering a patient’s room, a staff member wears a N95 respirator, goggles, face shield, a gown over scrubs and two pairs of gloves. The order in which PPE is removed when a staff member exits a patient’s room is exact. For example, inside the room by the door, the first pair of gloves is removed, followed by the face shield and the second pair of gloves; next, hands are washed with quick-drying antiseptic solution and the gown is carefully removed; then the hands are washed again before the staff member leaves the room. In the hallway, hands are washed, goggles removed and disposed of, hands washed again, respirators removed, and finally hands are washed again, and eventually a new N95 respirator is donned.18
Psychological and psychosocial management
Hospitals should respond fast to the psychological pressures on staff, and detailed psychological intervention plans should be part of the hospital disaster preparedness tools.6
Transport of patients inside and outside the healthcare facilities
The movement and transport of cases out of the isolation room or area should be avoided unless medically necessary. If transport is necessary, use designated routes of transport that minimise the exposures of staff, other patients and visitors to potential infection. Always notify the receiving area of the patient’s diagnosis and precautions that will be required before the patient’s arrival. Encourage the use of medical masks (FFP1) by patients with an acute respiratory infection during transport or when care is necessary outside of the isolation room or area. Clean and disinfect surfaces that the patient comes into contact with (e.g. bed) after use.
Prehospital care and transport outside healthcare facilities
After prehospital care or (inter-hospital) transport has been provided, follow recommended procedures for waste disposal, and for cleaning and disinfecting emergency vehicles and reusable patient care equipment.
Avoid crowding of patients during examination and in outpatient treatment areas. Notify the receiving facility as soon as possible before arrival that a patient with suspected Covid-19 is due to arrive, and indicate whether additional precautions are required.
Specific management of patients with acute coronary syndromes
General aspect of cardiovascular symptoms and myocardial injury
It has been demonstrated that during the Covid-19 infection, especially following the restrictions to leave home, fewer patients than usual call for help or visit emergency departments than before. So, the number of ST-segment elevation myocardial infarction (STEMI) cases has been halved and the number of non-ST-segment elevation myocardial infarction (NSTEMI) cases is less than one-third.
Possible causes of reductions in presentation include mainly the reluctance of patients to present to the emergency departments, but also a delay in response of an overloaded emergency medical service during the Covid-19 pandemic with respect to the transfer times that may occur.21 Further reasons have been discussed including less air pollution due to a massive reduction in public traffic, less physical exercise at home and less stress in business. By consequence, an increasing number of patients might not receive the optimal treatment, with the expected consequences of increased morbidity and mortality. It is therefore essential that patients be informed not to neglect symptoms of heart disease during the Covid-19 pandemic. Worsening chest pain during exercise or chest pain at rest, shortness of breath, palpitations, or fainting, should induce a call into the emergency services providers who then can help to decide whether a transfer to an emergency department is obligatory.
Circulating cardiac troponin is a marker of myocardial injury, including but not limited to myocardial infarction (MI) or myocarditis. The clinical relevance of this distinction has never been so clear as with Covid-19. An increase of cardiac troponins has been shown in up to 20% of patients hospitalised for Covid-19 infections consisting of either type-1 MI based on pre-existing or new coronary disease or type-2 MI in patients with lung infection and related respiratory distress.21,22 Troponin elevation may also exist as a consequence of right ventricular pressure increase in pulmonary embolism (frequently associated with a Covid-19 infection due to an increased prothrombotic milieu), tachyarrhythmia, coronary microvascular disease, stress cardiomyopathy, or a rare case of viral myocarditis during Covid-19 infection.21–25
The use of invasive diagnosis and treatment for Covid-19-positive patients or non-tested patients should be restricted to those in whom type-1 MI is suspected from ECG changes and/or clinical judgement.
Diagnosis and treatment of different entities of acute coronary syndromes
Patients presenting with acute STEMI or very high-risk NSTEMI with known or suspected Covid-19 infection need an urgent invasive diagnosis and treatment under optimal protection of the catheter personnel.26,27 As a result of the fact that test results are not immediately available in STEMI or high-risk NSTEMI patients, such patients should be managed assuming positive Covid-19 status. The maximum time from STEMI diagnosis to reperfusion of 120 minutes should continue to represent the goal for reperfusion therapy, primary percutaneous coronary intervention (PCI) should remain the reperfusion therapy of choice within this time frame and performed in facilities approved for the treatment of Covid-19 cases under optimal protection for healthcare providers and other patients. Only if this target time cannot be guaranteed should fibrinolysis become first line therapy if not contraindicated.
In patients with NSTEMI, risk stratification should be based on the criteria of the current European Society of Cardiology (ESC) guidelines.26,28 Patients presenting with NSTEMI can have a stable presentation, with a good response to optimal medical treatment alone, or a more severe course with clinical instability leading to an invasive management within 24–72 hours, thus allowing the time to test the patients for Covid-19 infection before the intervention. Criteria for very high-risk NSTEMI include among others haemodynamic instability or cardiogenic shock, recurrent or ongoing chest pain refractory to medical therapy, life-threatening arrhythmias, acute heart failure, or recurrent intermittent ST-elevation, respectively.
In patients with out of hospital cardiac arrest prognostic assessment is essential in order to avoid unnecessary intubation in order to avoid intensive care unit saturation at times when the resources might be limited. Here again, delays to emergency medical services arrival might be increased due to the overloading by Covid-related infections. In such cases the prognostic impact of the delays is even more substantial compared to STEMIs.
If not tested before, all patients presenting with an acute coronary syndrome should be tested for Covid-19 as soon as possible and irrespective of reperfusion strategy, and all measures of precaution (i.e. special wards for suspected, still unknown infections) should be taken to avoid potential infection of other patients and healthcare personnel until the result of the test is known.
Hospital networks for diagnosis and optimal treatment of acute coronary syndromes
With an increasing Covid-19 pandemic routine, diagnostic and elective interventions have to be drastically reduced and spoke and hub hospitals should focus on patients with clinical urgency and at high risk only. Some healthcare systems have identified specific Covid-19 hospitals or wards in an attempt to concentrate and isolate confirmed Covid-19 patients, and most importantly in order to prevent the spread-out of the pandemic.29
Specific Covid-19 hospitals or wards are frequently large community tertiary hospitals serving as STEMI hubs with intensive care and/or coronary care units and a 24/7 catheter laboratory activity. After invasive diagnosis and treatment non-infected patients are usually transferred to Covid-19-free hospitals or wards (within a hub centre). With a pandemic widespread attempts to distribute patients into separate Covid-19 hospitals or wards might become more difficult, in some cases even impossible, as the identification of suspected Covid-19 patients to date depends mostly on clinical symptoms or epidemiological assumptions, and as testing for symptom-free patients who might be carriers of the virus is frequently not possible due to lack of material, personal resources, and/or time. Healthcare providers should use all available protective measures in the management of patients presenting with an acute coronary syndrome as if they were Covid-19 positive. Until test results become available patients should be kept in protected environments and receive the best available treatment until contagion is ruled out. This may take hours.
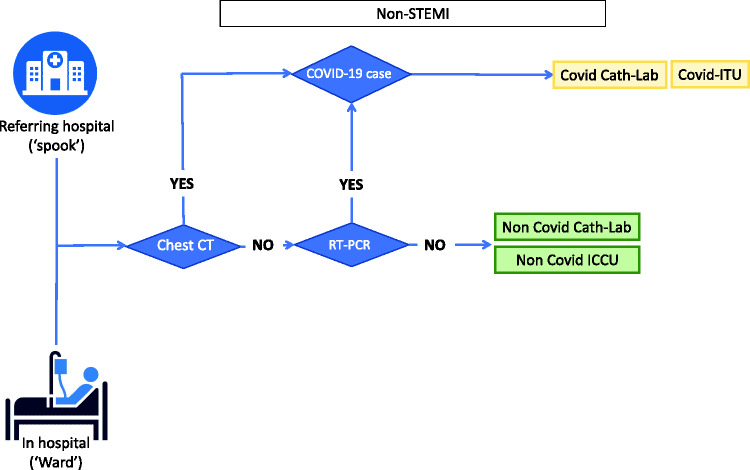
Potential Covid-19 transmission through asymptomatic carriers is a challenge to containment and adds to the logistic complexity in separating Covid-19 cases from non-cases in acute (cardiac) care.30 In general, test results occur hours after the acute intervention (i.e. primary PCI) has been performed. Moreover, there remains an issue on test sensitivity, more than specificity. The definitive test for SARS-CoV-2 is the real-time reverse transcriptase polymerase chain reaction (RT–PCR) test. It is believed to be highly specific, but with sensitivity reported as low as 60–70%.31–35 Thus, false negatives are a real clinical problem, and several negative tests might be required in a single case to be confident about excluding the disease. Here, chest computed tomography (CT) to detect Covid-19, even in asymptomatic patients, may become an asset.36,37 The sensitivity of chest CT is reported to be higher than RT–PCR (98% vs. 71%, respectively, P<0.001) and may be a valuable initial screening tool for Covid-19.35,38,39 Combining RT–PCR with chest CT may be an appropriate test strategy to separate Covid-19 cases from no-cases in centres performing invasive coronary diagnosis and treatment (Figures 1 and 2).
Figure 1.
Organisation of STEMI/high-risk NSTEMI care in the age of Covid-19
CT: computed tomography; EMS: emergency medical services; ICCU: cardiac intensive care unit; ITU: intensive care unit; STEMI: ST-segment elevation myocardial infarction; RT–PCR: reverse transcriptase polymerase chain reaction.
Figure 2.
Organisation of non-high risk NSTEMI care in the age of Covid-19
CT: computed tomography; ICCU: cardiac intensive care unit; ITU: intensive care unit; non-STEMI: non-ST-segment elevation myocardial infarction; RT–PCR: reverse transcriptase polymerase chain reaction.
Organisation of emergency departments and inter or inhospital transfer
The emergency room should be divided into areas for receiving suspected Covid-19-infected patients (those with specific symptoms such as fever and dyspnoea) and for patients with other emergencies. Although not possible to organise for all emergency departments, a dedicated entry point and triage for cardiovascular emergencies (chest pain unit) might prove advantageous to accelerate diagnosis and treatment. Separate teams providing care in each of these areas might reduce the risk of cross-contaminations as important as maintaining separate areas throughout the hospital for both Covid-19-positive and negative patients for further care. If organised differently, Covid-19-positive patients should be transferred to intensive care units, coronary care units or wards in Covid-19 hospitals depending on their clinical status and presentation.
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Einav S, Hick J L, Hanfling D, et al. Surge capacity logistics: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest 2014; 146(4 Suppl): e17S–e43S. [DOI] [PubMed] [Google Scholar]
- 2. Eccleston-Turner M, Phelan A, Katz R Preparing for the next pandemic – the WHO’s global influenza strategy. N Engl J Med 2019; 381: 2192–2194. [DOI] [PubMed] [Google Scholar]
- 3. Jones D S. History in a crisis – lessons for Covid-19. N Engl J Med 2020; 382: 1681–1683. [DOI] [PubMed] [Google Scholar]
- 4. Gates B. Responding to Covid-19 – a once-in-a-century pandemic? N Engl J Med 2020; 382: 1677–1679. [DOI] [PubMed] [Google Scholar]
- 5. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 2020; 382: 1199–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wang C, Horby P W, Hayden F G, et al. A novel coronavirus outbreak of global health concern. Lancet (London, England) 2020; 395: 470–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Roy C J, Milton D K Airborne transmission of communicable infection–the elusive pathway. N Engl J Med 2004; 350: 1710–1712. [DOI] [PubMed] [Google Scholar]
- 8. Hick J L, Biddinger P D Novel coronavirus and old lessons – preparing the health system for the pandemic. N Engl J Med 2020. Epub ahead of print. DOI: 10.1056/NEJMp2005118. [DOI] [PubMed] [Google Scholar]
- 9. Ferguson N M, Laydon D, Nedjati-Gilani G, et al. ; Imperial College COVID-19 Response Team. Report 9: Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-NPI-modelling-16-03-2020.pdf (2020, Accessed 18 April 2020).
- 10. Chen T M, Rui J, Wang Q P, et al. A mathematical model for simulating the phase-based transmissibility of a novel coronavirus. Infect Dis Poverty 2020; 9: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fauci A S, Lane H C, Redfield R R Covid-19 – navigating the uncharted. N Engl J Med 2020; 382: 1268–1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet (London, England) 2020; 395: 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lipsitch M, Cohen T, Cooper B, et al. Transmission dynamics and control of severe acute respiratory syndrome. Science (New York, NY) 2003; 300: 1966–1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Munster V J, Koopmans M, van Doremalen N, et al. A novel coronavirus emerging in China – key questions for impact assessment. N Engl J Med 2020; 382: 692–694. [DOI] [PubMed] [Google Scholar]
- 15. Wu J T, Leung K, Leung G M Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet (London, England) 2020; 395: 689–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bootsma M C, Ferguson N M The effect of public health measures on the 1918 influenza pandemic in U.S. cities. Proc Natl Acad Sci USA 2007; 104: 7588–7593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 2020; 382: 1199–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. World Health Organization. Infection prevention and control of epidemic-and pandemic-prone acute respiratory infections in health care. WHO guidelines. https://www.who.int/csr/bioriskreduction/infection_control/publication/en/ (2014, accessed 26 March 2020). [PubMed]
- 19. Emanuel E J, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med 2020; Epub ahead of print. DOI: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 20. Christian M D, Sprung C L, King M A, et al. Triage: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest 2014; 146 (4 Suppl): e61S–e74S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tam C F, Cheung K S, Lam S, et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circulation Cardiovasc Qual Outcome 2020; 13: e006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chapman A R, Hesse K, Andrews J, et al. High-sensitivity cardiac troponin I and clinical risk scores in patients with suspected acute coronary syndrome. Circulation 2018; 138: 1654--1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chapman A R, Bularga A, Mills N L High-sensitivity cardiac troponin can be an ally in the fight against COVID-19. Circulation 2020. Epub ahead of print. DOI: 10.1161/CIRCULATIONAHA.120.047008. [DOI] [PubMed] [Google Scholar]
- 24. Inciardi R M, Lupi L, Zaccone G, et al. . Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020. Epub ahead of print. DOI: 10.1001/jamacardio.2020.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Madjid M, Safavi-Naeini P, Solomon S D, et al. . Potential Effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol 2020. Epub ahead of print. DOI: 10.1001/jamacardio.2020.1286. [DOI] [PubMed] [Google Scholar]
- 26. Neumann F J, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 2019; 40: 87–165. [DOI] [PubMed] [Google Scholar]
- 27. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Revista espanola de cardiologia (English ed) 2017; 70: 1082. [DOI] [PubMed] [Google Scholar]
- 28. Roffi M, Patrono C, Collet J P, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 2016; 37: 267–315. [DOI] [PubMed] [Google Scholar]
- 29. Stefanini G G, Azzolini E, Condorelli G Critical organizational issues for cardiologists in the COVID-19 outbreak: a frontline experience from Milan, Italy. Circulation 2020. Epub ahead of print. DOI: 10.1161/CIRCULATIONAHA.120.047070. [DOI] [PubMed] [Google Scholar]
- 30. Yu X, Yang R COVID-19 transmission through asymptomatic carriers is a challenge to containment. Influenza Other Respir Virus 2020; In progress. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Chan J F, Yip C C, To K K, et al. Improved molecular diagnosis of COVID-19 by the novel, highly sensitive and specific COVID-19-RdRp/Hel real-time reverse transcription-polymerase chain reaction assay validated in vitro and with clinical specimens. J Clin Microbiol 2020; 58: e00310–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Liu R, Han H, Liu F, et al. Positive rate of RT-PCR detection of SARS-CoV-2 infection in 4880 cases from one hospital in Wuhan, China, from Jan to Feb 2020. Clin Chim Acta; International Journal of Clinical Chemistry 2020; 505: 172–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Pfefferle S, Reucher S, Norz D, et al. Evaluation of a quantitative RT-PCR assay for the detection of the emerging coronavirus SARS-CoV-2 using a high throughput system. Euro Surveillance: bulletin Europeen sur les maladies transmissibles = European communicable disease bulletin 2020; 25. In progress. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tang Y W, Schmitz J E, Persing D H, et al. The laboratory diagnosis of COVID-19 infection: current issues and challenges. J Clin Microbiol 2020. Epub ahead of print. DOI: 10.1128/JCM.00512-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Guan W J, Ni Z Y, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med 2020; 382: 1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Chan J F, Yuan S, Kok K H, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet (London, England) 2020; 395: 514–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lee EY P, Ng M Y, Khong P L COVID-19 pneumonia: what has CT taught us? Lancet Infect Dis 2020; 20: 384–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Fang Y, Zhang H, Xie J, et al. Sensitivity of chest CT for COVID-19: comparison to RT–PCR. Radiology 2020; Epub ahead of print. DOI: 10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ai T, Yang Z, Hou H, et al. Correlation of chest CT and RT–PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology 2020; Epub ahead of print. DOI: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]