Abstract
Sudden sensorineural hearing loss (SSNHL) is an enigmatic entity, with obscure pathophysiology and debatable efficacy of the treatment agents used. An underlying cause is identified in only 10–15% of cases. The management of the remaining patients, classified as ‘idiopathic’, is empirical, and is conventionally with systemic steroids, vasodilator therapy, rheological agents, and antioxidants, to list a few amongst the host of the agents employed for the treatment. The availability of conflicting outcomes and lack of conclusive evidence has resulted in the propagation of consensus-based treatment protocols. In the present review, we discuss the various controversial issues and newer developments in the management of idiopathic SSNHL. The current review aims to present a narrative outlook of the updated evidence base available from PUBMED, augmented with relevant designated publications.
Keywords: Hearing loss, Sudden, Sensorineural, Instillation, Drug, Dexamethasone, Prognosis
1. Introduction
Sudden sensorineural hearing loss (SSNHL) is a frightening experience for the patient and is perceived as an otologic emergency. It has been defined as a loss of at least 30 dB over at least three frequencies in audiogram within three days(Stachler et al., 2012). The incidence varies from two to 30 per 1,00,000 adult individuals. However, an incidence of as high as 160 per 1,00,000 individuals per year has been reported from Germany(Kleyn, 1944). Usually affected age group is fifth and sixth decade, although the range is quite wide. There is no apparent gender predilection. It can occur as a part of systemic disorder or without any identifiable systemic or local abnormality. The latter being termed ‘idiopathic’ (ISSNHL).
At the initial presentation, a diagnosis is reached at in only 10–15% of the patients. Prolonged follow up reveals the underlying etiology in up to 1/3rd of cases(Stachler et al., 2012). Despite a plethora of scientific studies regarding the subject in literature, it’s surprising how little the studies agree regarding etiopathogenesis, management and even outcome measures.
1.1. Natural history
Idiopathic SSNHL has been observed to recover in 32–65% of patients spontaneously. The spontaneous recovery tends to occur within first two weeks(Byl, 1984; Mattox and Simmons, 1977; Nosrati-Zarenoe and Hultcrantz, 2012; Wilson et al., 1980). The prospects of spontaneous recovery are minimal beyond a period of three months(Byl, 1984; Fetterman et al., 1996; Nosrati-Zarenoe and Hultcrantz, 2012; Zadeh et al., 2003). Majority of the patients present with unilateral hearing loss. However, up to 2–3% of the patients experience bilateral hearing loss which usually is sequential, but may occur simultaneously(Fetterman et al., 1996; Wilson et al., 1980). Approximately 4–8% of patients have been noted to develop Meniere’s disease over the ensuing years(Byl, 1984; Hallberg, 1956).
1.2. Clinical evaluation
Differentiating conductive from sensorineural hearing loss is of utmost importance since the presentation of the two may be similar but the treatment implications are poles apart. A history of associated tinnitus, vertigo, focal neurological signs and previous history of recurring hearing loss should be specifically enquired. The local ear examination involves otoscopic inspection to look for impacted cerumen and the condition of tympanic membrane (presence of otitis media with effusion should be specifically looked for). Clinical examination is followed by a detailed audiometric evaluation with pure tone audiometry and speech audiometry.
1.3. Laboratory investigations
Routine laboratory blood tests including complete blood counts, coagulation profile, serum electrolytes, erythrocyte sedimentation rate are commonly performed. However, the yield is poor and routine blood profiling is not recommended as per the American academy of otorhinolaryngology and head and neck surgery (AAO-HNS) clinical practice guidelines(Stachler et al., 2012). Serological tests for infectious causes should not be done routinely, but directed by clinical and epidemiological scenarios. An autoimmune workup and metabolic panel work up for diabetes, hyperlipidemia and thyroid dysfunction is reasonable to look for specific etiology and the metabolic risk factors management. Hypercholesterolemia has been reported in 35–40% of SSNHL patients and deranged blood sugars in 18–37% of patients(Narozny et al., 2006; Oiticica and Bittar, 2010).
1.4. Imaging
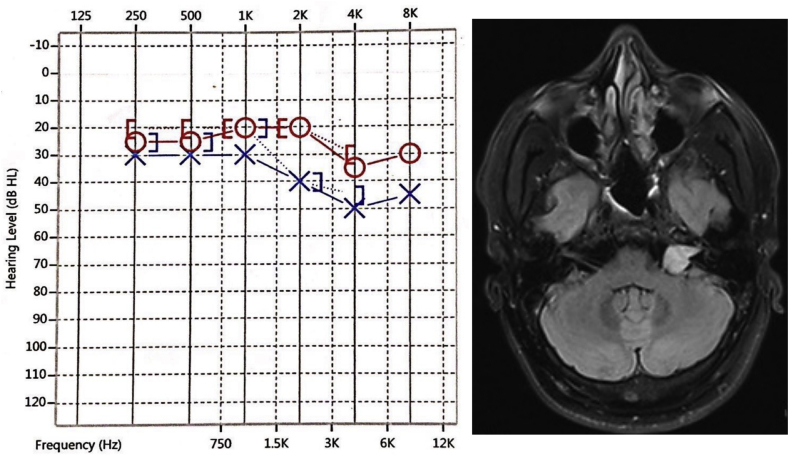
One of the most important aspect of work up for SSNHL remains ruling out a retrocochlear pathology. A vestibular schwannoma has been identifies in 1.4–6.1% of the patients presenting with SSNHL in various series(Carrier and Arriaga, 1997; Ramos et al., 2005) and 10–20% of vestibular schwannomas can present with sudden drop in hearing(Lawrence and Thevasagayam, 2015) (Fig. 1). The spontaneous or post-treatment recovery of the hearing loss does not rule out an underlying mass lesion. Imaging modality of choice remains contrast-enhanced MRI (CE-MRI) of brain with specific attention to cerebello-pontine angle (CPA), internal auditory canal and the inner ear apparatus. The sensitivity and specificity of the CE-MRI for Vestibular schwannomas >3 mm remains close to 100%(Cueva, 2004; Fortnum et al., 2009). In addition to the CPA tumors, labyrinthine hemorrhage, demyelinating diseases and stroke may be identified as potential underlying etiological element. An MRI reveals abnormal findings in 10%–57% patients of SSNHL(Chau et al., 2012).
Fig. 1.
Pure tone audiogram (left panel) of a patient who presented with sudden ear blockade sensation on left side without vestibular or focal neurological deficits. A Contrast Enhanced MRI brain (right panel) revealed a 1.5 × 1.1 cm (extrameatal part) intensely enhancing schwannoma involving the left internal acoustic canal and cerebellopontine angle with typical ice-cream cone appearance.
If contrast administration is contraindicated (GFR<30 ml/min; risk of nephrogenic systemic fibrosis), a constructive interference in steady state (CISS) sequence may be undertaken. The sensitivity and specificity of CISS sequences for the tumor size >5 mm reaches close to 100%(Fortnum et al., 2009).
In patients with ferromagnetic implants, metallic ocular foreign body or claustrophobia, performing an MRI may not be possible. In such situations, an auditory brainstem response (ABR) can be used with a sensitivity and specificity of 85.8% and 82%, respectively, for lesions <1 cm in size(Koors et al., 2013) (sensitivity for the larger lesions {>1cm} reaches 95%). A stacked-ABR can give better sensitivity and specificity of 95% and 88%, respectively, for similar sized (<1cm) tumors(Don et al., 2005).
2. Treatment
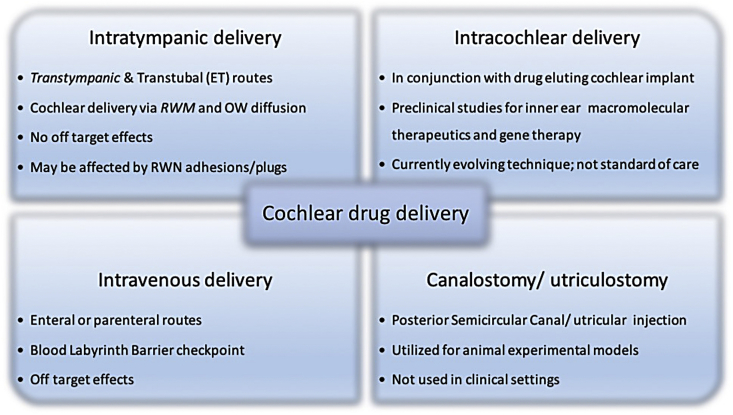
The various routes of intracochlear drug deposition are depicted in Fig. 2(Nyberg et al., 2019). In view of the high rates of spontaneous recovery and lack of conclusive understanding about the underlying etiology, the relative efficacy of various treatment modalities needs to be interpreted cautiously.
Fig. 2.
Various routes of inner ear drug delivery. (ET-Eustachian Tube; RWM-Round Window Membrane; OW-Oval Window; RWN-Round Window Niche).
2.1. Systemic corticosteroids
Oral corticosteroids remain the first line of therapy for the heterogeneous population of SSNHL. Despite being used commonly, the evidence base for the efficacy of steroids remains contradictory at best. As per AAO-HNS guidelines, the physician may offer oral corticosteroids as first line therapy to the patient after discussing the limited documented evidence for their efficacy(Stachler et al., 2012). The first and perhaps the best favorable evidence for the oral steroid comes from the randomized controlled trial (RCT) by Wilson and colleagues(Wilson et al., 1980), comparing steroids versus placebo in a total of 67 patients. However, the results have not been replicated in other RCTs by Cinamon et al. (2001) and Nosrati-Zarenoe et al.(Nosrati-Zarenoe and Hultcrantz, 2012) Serious methodological flaws have been noted in these trials. A systemic review/meta-analysis by Conlin and Parnes(Conlin and Parnes, 2007a, 2007b), and Cochrane review(Wei et al., 2013) reached the conclusion that the value of oral steroids in ISSNHL remains unproven.
Dose of steroids and effect of timings to start therapy remain equally contentious. A double-blinded RCT comparing 70 mg prednisolone (with 10 mg daily tapering) and 300 mg intravenous (IV) methylprednisolone pulse for three days followed by four days of placebo concluded that the pulse therapy was equally efficacious as standard oral prednisolone therapy for ISSNHL(Westerlaken et al., 2007). Similar results were obtained in a recent RCT including 67 patients treated for 14 days (Study group: 500 mg IV methylprednisolone daily for three days followed by 1 mg/kg/day of oral prednisolone for 11 days; Control group: 1 mg/kg/day oral prednisolone for 14 days)(Eftekharian and Amizadeh, 2016). However, there is some evidence from retrospective studies regarding treatment advantage for high dose systemic steroids therapy(Alexiou et al., 2001; Egli Gallo et al., 2013). Niedermeyer et al. showed that the level of cortisol in human perilymph was significantly higher after 250 mg intravenous prednisolone compared to 125 mg dose. The latter group had cortisol levels similar to the controls, who did not receive steroids(Niedermeyer et al., 2003). The German Association of Scientific Medical Societies (AWMF) guidelines advocate high dose (250 mg) intravenous steroid treatment and currently a triple-blind, multicenter national RCT (HODOKORT trial) is ongoing in Germany to compare the high dose steroid regimen with the standard doses of steroids for ISSNHL(Plontke, 2017).
Regarding the timing of therapy in relation to the onset of symptoms, it has been a traditional practice to starts primary treatment with steroids as soon as possible (within 1–2 weeks) since the results from various studies suggest the increasing time between onset of symptoms and treatment to be an adverse prognostic factor(Byl, 1984; Fetterman et al., 1996; Megighian et al., 1986). Rates of recovery in the patients who approached the physician and got the audiograms performed in the first week of disease onset, within two weeks and beyond three months are 87%, 52% and <10%, respectively.(Byl, 1984; Fetterman et al., 1996; Nosrati-Zarenoe and Hultcrantz, 2012; Simmons, 1973; Zadeh et al., 2003) However, there are studies which contradict the therapeutic benefits of urgent intervention and indicate that the apparent benefits of early presentation to physician are more of ‘sham effects’ correlating with the natural history of the disease(Huy and Sauvaget, 2005; Liebau et al., 2017; Tran Ba Huy and Sauvaget, 2007). The AAO-HNS guidelines suggest an early treatment with steroids within two weeks(Stachler et al., 2012).
2.2. Intratympanic steroids
Intratympanic (IT) steroid instillation has several advantages compared to the systemic steroid treatment as listed in Table-1. The various methods of Intratympanic drug delivery are described in Table-2.
Table 1.
Advantages of intratympanic therapy over systemic steroid treatment.
|
Table 2.
Methods of intratympanic drug delivery.
|
IT injections (using a 22 to 27-gauge spinal needle) remain the most convenient and commonest method used. Various concentrations of the drug solutions have been used including dexamethasone (dexa) 4 mg/ml, 5 mg/ml, 10 mg/ml, 24 mg/ml, and 40 mg/ml; prednisolone (62.5 mg/ml)(Filipo et al., 2010); and methylprednisolone 30 mg/ml, 40 mg/ml, 62.5 mg/ml, and 80 mg/ml; with 0.4–0.8 ml solution being deposited intratympanically every day (for up to eight sessions), every other day, three times a week, twice a week, to weekly injections for 3–4 sessions(El Sabbagh et al., 2017; Gussen, 1976). No single protocol has been found to be superior to another, and the treatment preference is largely influenced by surgeon and institutional policies, and the local availability of the steroid preparation(Spear and Schwartz, 2011). Maximum recovery rates with IT steroid therapy has been reported by Filipo et al. (2010), who reported improvement in 91% of the patients, however, it was a retrospective study, and no control arm was included. The outcomes of studies with a higher level of evidence are discussed subsequently.
Intratympanic drug instillation can be carried out in the following three scenarios:
-
•
Primary therapy
-
•
Adjuvant/combination therapy
-
•
Salvage/sequential therapy
In view of the heterogeneity of the study protocols as well as criteria to define and classify the recovery, the conclusions are difficulty to consolidate regarding the optimal steroid delivery methods. The non-inferiority RCT by Rauch and colleagues, comparing Oral steroids and IT steroids for patients presenting within two weeks of onset of SSNHL concluded that the IT route was not inferior to the oral route of drug delivery(Rauch et al., 2011). A recent meta-analysis revealed that there was no statistically significant difference in the recovery parameters obtained using IT steroid (alone) or oral/systemic therapy (alone)(Lai et al., 2017). Similar results have been reported by other authors comparing IT dexa with oral steroid as primary therapy for SSNHL(Dispenza et al., 2011; Ermutlu et al., 2017; Hong et al., 2009; Lim et al., 2013). Kosyakov et al.(“Kosyakov S, Atanesyan A, Gunenkov A, Ashkhatunyan E, Kurlova A. Intratympanic steroids for sudden sensorineural hearing loss. Int Adv Otol. 2011; 7:323–32.,” n.d.) studied the effect of long term administration of the intratympanic steroids (over six months using grommet), and concluded that the long term use of IT steroids led to a statistically significant recovery compared to standard short course intravenous steroid therapy. Kakehata et al. (2006) showed that the mean hearing improvement and the proportion of the patients with >10 dB hearing improvement was statistically higher in the patients who received IT dexa compared to IV dexa therapy. The systemic reviews by Vlastarakos et al. (2012) and by Spear and Schwartz(Spear and Schwartz, 2011) concluded that IT steroid therapy is effective in both primary and salvage settings. Given as primary treatment, IT therapy was at least as effective as the oral therapy and the benefits in the salvage setting were potentially additive to the benefits of primary oral treatment. However, no clear consensus could be made regarding the superiority of combined oral and Intratympanic treatment. The study by Battaglia et al. (2008), showed that the combined IT and oral steroid therapy was superior to the oral therapy alone, in terms of word recognition scores, however, the results were not statistically different between the oral alone and IT alone arms, and the study had to be prematurely terminated in view of poor patient recruitment. Ahn et al. (2008) concluded that addition of IT dexa to oral corticosteroids does not result in superior outcome compared to oral therapy alone.
Given the low risk of side effects and complications (local pain, transient vertigo, small risk of otitis media and tympanic membrane perforation), and non-inferiority of the IT steroid instillation compared with the systemic route, the former has clear advantages and favorable applicability compared to the systemic route. Combination therapy (with IT and systemic steroids) does not appear to be superior to single modality treatment.
2.3. Other treatment modalities
The combination of steroids with antivirals has been shown to be non-superior to oral steroids alone in multiple RCTs(Stokroos et al., 1998; Westerlaken et al., 2003) and by a Cochrane review(Awad et al., 2012), and hence, antivirals are not routinely prescribed for ISSNHL.
Hyperbaric oxygen therapy (HBOT) has been used with the intent to increase oxygen supply to the possibly ischemic cochlear structures in SSNHL. A Cochrane review performed in 2012 identified seven RCTs evaluating the role of HBOT in SSNHL. It was inferred that five patients of SSNHL will need to be treated with HBOT to bring about 25% hearing improvement in one patient. The methodological limitations of these trials made the authors warn about interpreting the results with caution(Bennett et al., 2012). Another RCT by Cekin et al. did not show any statistical significant benefits of HBOT in treating SSNHL(Cekin et al., 2009). The possible benefits of HBOT need to be weighed against availability, cost constraints and side effects associated with the therapy. AAO-HNS recommends HBOT as an optional therapy to be used within three months of onset of SNHL(Stachler et al., 2012). A recent meta-analysis including three RCTs and 16 nonrandomized studies, pooling 2401 patients, revealed that compared to medical therapy alone, HBOT combined with medical therapy may be more efficacious for the patients:
-
1)
treated in a salvage setting,
-
2)
with severe to profound (≥70 dB HL) hearing loss,
-
3)
treated for a total treatment duration of at least 1200 min(Rhee et al., 2018).
A myriads of other therapies have been used to treat ISSNHL including volume expanders, vasodilators and vasoactive substances (including carbogen therapy, calcium channel blockers, pentoxifyllin, prostaglandin E1, naftidrofuryl), thrombolytics, antioxidants, histamines, magnesium, diuretics, intravenous diatrizoate and herbal remedies. In view of either the lack of apt evidence base, or evidence against the use of these modalities, their use is not supported by literature(Bravenboer de Sousa et al., 2017; Conlin and Parnes, 2007a, 2007b; Lan et al., 2018).
Keeping in mind the lack of unequivocal efficacy of the available agents, a search for newer agents with definite evidence of efficacy is still on. Nakagawa et al. (2012) described topical instillation of Insulin like growth factor-1 (IGF-1) using gelatin hydrogel into the middle ear in the patients refractory to systemic steroids. The hearing recovery (overall 11.9 dB over five frequencies; 0.25, 0.5, 1, 2 and 4 kHz) was significant at low frequencies but not at high frequency and the level of improvement was not superior to the results of IT steroid application mentioned in the literature.
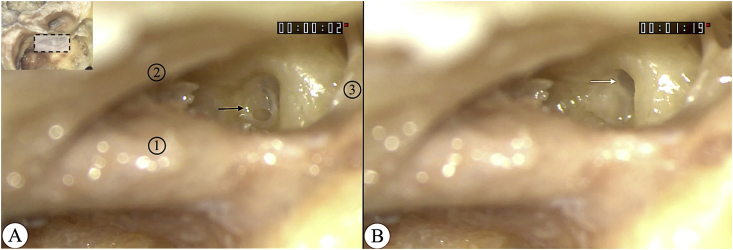
RWN Drilling and steroid instillation has been proposed to be advantageous over IT delivery by maximizing the inner ear drug delivery. Si et al. (2018) carried out the drilling of the round window niche (RWN) via a posterior tympanotomy window to maximise the drug-round window membrane (RWM) contact area for effective drug diffusion into the inner ear, for the patients failed on systemic intravenous and injectable IT steroid therapy. They suggested that the removal of the false RWM and an increase of the absolute area of exposure would lead to more uniform and meaningful delivery of the steroid to the inner ear (Fig. 3). Statistically significant hearing improvement was observed in the patients in whom the intratympanic steroid injection was performed after drilling of the RWN compared to the control group (mean improvement of 20.38 dB and 2.11 dB, respectively; P = 0.019).
Fig. 3.
Cadaveric temporal bone dissection showing the exposure of round window niche via posterior tympanotomy in a left sided temporal bone. (A) False round window membrane (black arrow) obscuring the view of true round window membrane. (B) Removal of false membrane reveals the true membrane (white arrow) located deep in the round window niche. (Inset shows the region of the dissected temporal bone {shaded rectangle} shown as magnified image in panel A and B; 1-Vertical part of facial nerve; 2-Chorda Tympani; 3-Pyramidal Process; original magnification X25).
2.4. Neuro-rehabilitation therapy
Neuroplasticity targeted interventions are emerging as a potentially effective, safe and economic adjunct therapeutic strategy for the treatment of SSNHL. The evidence base at present, however, is limited(López-González et al., 2012; Okamoto et al., 2014). Constraint induced sound therapy (CIST), as proposed by Okamoto et al., explores the effect of sound deprivation (constraint) in the normal ear along with musical stimulation (sound therapy) to the effected ear. The therapy aims at preventing/reversing the maladaptive auditory cortex reorganization occurring as a result of unilateral sudden SNHL. The authors administered CIST in addition to the gold standard treatment with systemic steroids to a subset of their cohort with hearing loss ≤50 dB presenting within five days of onset of hearing loss. Compared to the subjects who received only steroid therapy, the subjects treated with CIST as an add on therapy demonstrated statistically significant improvement in the final hearing recovery at a mean follow up of 63 days. Further studies employing randomized methodology are awaited to substantiate the utility of neuro-rehabilitative strategy for these patients.
2.5. Prognostic factors
In general, up to 65% of the patients recover hearing to varying extent. The various factors related to the likelihood of the recovery are as follows:
-
1.
Age – has been the most consistent adverse factor, with the elderly patients having significantly lower rates of recovery(Byl, 1984; Fetterman et al., 1996; Nosrati-Zarenoe and Hultcrantz, 2012; Wilson et al., 1980; Zadeh et al., 2003).
-
2.
Associated features – Presence of vertigo has been reported in some studies to be associated with poor prognosis(Ben-David et al., 2002; Byl, 1984; Chang et al., 2005; Huy and Sauvaget, 2005). However, it has not been a universal observation(Fetterman et al., 1996; Nosrati-Zarenoe and Hultcrantz, 2012; Zadeh et al., 2003). Tinnitus has been reported as a good(Danino et al., 1984), bad(Ben-David et al., 2002), and neutral(Chang et al., 2005) prognostic factor in various studies.
-
3.
Duration of hearing loss – The patients presenting to the physician within a week are more likely to have a better recovery rate compared to the late presenters(Byl, 1984; Fetterman et al., 1996; Nosrati-Zarenoe and Hultcrantz, 2012; Zadeh et al., 2003). This occurrence may not be related to early onset of treatment, but rather to the fact that a longer duration of hearing loss lessens the chances of recovery.
-
4.
Severity of hearing loss at presentation – the patients presenting with profound hearing loss have a significantly lesser probability of recovery than the patients presenting with milder hearing loss(Byl, 1984; Laird and Wilson, 1983).
-
5.
Pattern of hearing loss – Among the patients with a mild-severe degree of hearing loss, the prospects of hearing recovery are lesser for the flat audiogram configuration. For the non-flat configuration, an ascending audiogram has a better prognosis than the descending type(Chang et al., 2005; Huy and Sauvaget, 2005; Mattox and Simmons, 1977; Nosrati-Zarenoe and Hultcrantz, 2012; Zadeh et al., 2003).
-
6.
Systemic comorbidities – the presence of diabetes mellitus, hyperlipidemia and hypertension have been variably associated with a poorer outcome in various studies(Capaccio et al., 2007; Chau et al., 2010).Metabolic syndrome has been documented to be an independent risk factor for SSNHL(Chien et al., 2015). The rate of recovery has been shown to be lower in patients with metabolic syndrome, with poorer results associated with four or more features of the syndrome(Jung et al., 2018).
3. Conclusion
-
•
ISSNHL may recover spontaneously in up to 65% of the patients.
-
•
Work up for SSNHL must include CE-MRI of brain with especial emphasis on CP angle, IAC and inner ear. Investigations for specific infective etiologies (Syphilis, Lyme disease) should be directed as per individual risk assessment and epidemiologic profile.
-
•
In the absence of adequate evidence favoring high dose steroid therapy, the standard dose oral steroid regimen (1 mg/kg/day for 7–10 days followed by tapering) continues as the routinely prescribed therapeutic regimen for ISSNHL worldwide. An early intervention, preferably within two weeks carries a favorable prognostication in terms of hearing recovery.
-
•
In a treatment naïve patient with contraindications to the use of systemic steroids, intratympanic therapy remains the treatment of choice. Patients with inadequate benefits with systemic treatment should be treated with salvage intratympanic therapy.
-
•
HBOT may be prescribed for a patient presenting within three months of onset of SNHL after explaining about limited evidence and cost/side effect issues. Use of antivirals, rheological agents, vasoactive substances, antioxidants and other therapies is not recommended.
Conflicts of interest
None declared.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
None.
Footnotes
Peer review under responsibility of PLA General Hospital Department of Otolaryngology Head and Neck Surgery.
References
- Ahn J.H., Yoo M.H., Yoon T.H., Chung J.W. Can intratympanic dexamethasone added to systemic steroids improve hearing outcome in patients with sudden deafness? The Laryngoscope. 2008;118:279–282. doi: 10.1097/MLG.0b013e3181585428. [DOI] [PubMed] [Google Scholar]
- Alexiou C., Arnold W., Fauser C., Schratzenstaller B., Gloddek B., Fuhrmann S., Lamm K. Sudden sensorineural hearing loss: does application of glucocorticoids make sense? Arch. Otolaryngol. Head Neck Surg. 2001;127:253–258. doi: 10.1001/archotol.127.3.253. [DOI] [PubMed] [Google Scholar]
- Awad Z., Huins C., Pothier D.D. Antivirals for idiopathic sudden sensorineural hearing loss. Cochrane Database Syst. Rev. 2012 doi: 10.1002/14651858.CD006987.pub2. CD006987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Battaglia A., Burchette R., Cueva R. Combination therapy (intratympanic dexamethasone + high-dose prednisone taper) for the treatment of idiopathic sudden sensorineural hearing loss. Otol. Neurotol. 2008;29:453–460. doi: 10.1097/MAO.0b013e318168da7a. [DOI] [PubMed] [Google Scholar]
- Ben-David J., Luntz M., Podoshin L., Sabo E., Fradis M. Vertigo as a prognostic sign in sudden sensorineural hearing loss. Int. Tinnitus J. 2002;8:127–128. [PubMed] [Google Scholar]
- Bennett M.H., Kertesz T., Perleth M., Yeung P., Lehm J.P. Hyperbaric oxygen for idiopathic sudden sensorineural hearing loss and tinnitus. Cochrane Database Syst. Rev. 2012;10:CD004739. doi: 10.1002/14651858.CD004739.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bravenboer de Sousa M., Cazemier S., Stegeman I., Thomeer H. Use of vasodilators in idiopathic sudden sensorineural hearing loss: a systematic review. J. Int. Adv. Otol. 2017;13:399–403. doi: 10.5152/iao.2017.2966. [DOI] [PubMed] [Google Scholar]
- Byl F.M. Sudden hearing loss: eight years’ experience and suggested prognostic table. The Laryngoscope. 1984;94:647–661. [PubMed] [Google Scholar]
- Capaccio P., Ottaviani F., Cuccarini V., Bottero A., Schindler A., Cesana B.M., Censuales S., Pignataro L. Genetic and acquired prothrombotic risk factors and sudden hearing loss. The Laryngoscope. 2007;117:547–551. doi: 10.1097/MLG.0b013e31802f3c6a. [DOI] [PubMed] [Google Scholar]
- Carrier D.A., Arriaga M.A. Cost-effective evaluation of asymmetric sensorineural hearing loss with focused magnetic resonance imaging. Otolaryngol. Head Neck Surg. 1997;116:567–574. doi: 10.1016/S0194-59989770229-8. [DOI] [PubMed] [Google Scholar]
- Cekin E., Cincik H., Ulubil S.A., Gungor A. Effectiveness of hyperbaric oxygen therapy in management of sudden hearing loss. J. Laryngol. Otol. 2009;123:609–612. doi: 10.1017/S0022215109004277. [DOI] [PubMed] [Google Scholar]
- Chang N.-C., Ho K.-Y., Kuo W.-R. Audiometric patterns and prognosis in sudden sensorineural hearing loss in southern Taiwan. Otolaryngol. Head Neck Surg. 2005;133:916–922. doi: 10.1016/j.otohns.2005.09.018. [DOI] [PubMed] [Google Scholar]
- Chau J.K., Cho J.J.W., Fritz D.K. Evidence-based practice: management of adult sensorineural hearing loss. Otolaryngol. Clin. N. Am. 2012;45:941–958. doi: 10.1016/j.otc.2012.06.002. [DOI] [PubMed] [Google Scholar]
- Chau J.K., Lin J.R.J., Atashband S., Irvine R.A., Westerberg B.D. Systematic review of the evidence for the etiology of adult sudden sensorineural hearing loss. The Laryngoscope. 2010;120:1011–1021. doi: 10.1002/lary.20873. [DOI] [PubMed] [Google Scholar]
- Chien C.-Y., Tai S.-Y., Wang L.-F., Hsi E., Chang N.-C., Wu M.-T., Ho K.-Y. Metabolic syndrome increases the risk of sudden sensorineural hearing loss in Taiwan: a case-control study. Otolaryngol. Head Neck Surg. 2015;153:105–111. doi: 10.1177/0194599815575713. [DOI] [PubMed] [Google Scholar]
- Cinamon U., Bendet E., Kronenberg J. Steroids, carbogen or placebo for sudden hearing loss: a prospective double-blind study. Eur. Arch. Oto-Rhino-Laryngol. 2001;258:477–480. doi: 10.1007/s004050100366. [DOI] [PubMed] [Google Scholar]
- Conlin A.E., Parnes L.S. Treatment of sudden sensorineural hearing loss: I. A systematic review. Arch. Otolaryngol. Head Neck Surg. 2007;133:573–581. doi: 10.1001/archotol.133.6.573. [DOI] [PubMed] [Google Scholar]
- Conlin A.E., Parnes L.S. Treatment of sudden sensorineural hearing loss: II. A Meta-analysis. Arch. Otolaryngol. Head Neck Surg. 2007;133:582–586. doi: 10.1001/archotol.133.6.582. [DOI] [PubMed] [Google Scholar]
- Cueva R.A. Auditory brainstem response versus magnetic resonance imaging for the evaluation of asymmetric sensorineural hearing loss. The Laryngoscope. 2004;114:1686–1692. doi: 10.1097/00005537-200410000-00003. [DOI] [PubMed] [Google Scholar]
- Danino J., Joachims H.Z., Eliachar I., Podoshin L., Ben-David Y., Fradis M. Tinnitus as a prognostic factor in sudden deafness. Am. J. Otolaryngol. 1984;5:394–396. doi: 10.1016/s0196-0709(84)80054-x. [DOI] [PubMed] [Google Scholar]
- Dispenza F., Amodio E., De Stefano A., Gallina S., Marchese D., Mathur N., Riggio F. Treatment of sudden sensorineural hearing loss with transtympanic injection of steroids as single therapy: a randomized clinical study. Eur. Arch. Oto-Rhino-Laryngol. 2011;268:1273–1278. doi: 10.1007/s00405-011-1523-0. [DOI] [PubMed] [Google Scholar]
- Don M., Kwong B., Tanaka C., Brackmann D., Nelson R. The stacked ABR: a sensitive and specific screening tool for detecting small acoustic tumors. Audiol. Neuro. Otol. 2005;10:274–290. doi: 10.1159/000086001. [DOI] [PubMed] [Google Scholar]
- Eftekharian A., Amizadeh M. Pulse steroid therapy in idiopathic sudden sensorineural hearing loss: a randomized controlled clinical trial. The Laryngoscope. 2016;126:150–155. doi: 10.1002/lary.25244. [DOI] [PubMed] [Google Scholar]
- Egli Gallo D., Khojasteh E., Gloor M., Hegemann S.C.A. Effectiveness of systemic high-dose dexamethasone therapy for idiopathic sudden sensorineural hearing loss. Audiol. Neuro. Otol. 2013;18:161–170. doi: 10.1159/000346938. [DOI] [PubMed] [Google Scholar]
- El Sabbagh N.G., Sewitch M.J., Bezdjian A., Daniel S.J. Intratympanic dexamethasone in sudden sensorineural hearing loss: a systematic review and meta-analysis: intratympanic Dexamethasone for SSNHL. The Laryngoscope. 2017;127:1897–1908. doi: 10.1002/lary.26394. [DOI] [PubMed] [Google Scholar]
- Ermutlu G., Süslü N., Yılmaz T., Saraç S. Sudden hearing loss: an effectivity comparison of intratympanic and systemic steroid treatments. Eur. Arch. Oto-Rhino-Laryngol. 2017;274:3585–3591. doi: 10.1007/s00405-017-4691-8. [DOI] [PubMed] [Google Scholar]
- Fetterman B.L., Saunders J.E., Luxford W.M. Prognosis and treatment of sudden sensorineural hearing loss. Am. J. Otol. 1996;17:529–536. [PubMed] [Google Scholar]
- Filipo R., Covelli E., Balsamo G., Attanasio G. Intratympanic prednisolone therapy for sudden sensorineural hearing loss: a new protocol. Acta Otolaryngol. 2010;130:1209–1213. doi: 10.3109/00016481003793766. [DOI] [PubMed] [Google Scholar]
- Fortnum H., O’Neill C., Taylor R., Lenthall R., Nikolopoulos T., Lightfoot G., O’Donoghue G., Mason S., Baguley D., Jones H., Mulvaney C. The role of magnetic resonance imaging in the identification of suspected acoustic neuroma: a systematic review of clinical and cost effectiveness and natural history. Health Technol. Assess. 2009;13 doi: 10.3310/hta13180. iii–iv, ix–xi, 1–154. [DOI] [PubMed] [Google Scholar]
- Gussen R. Sudden deafnfess of vascular origin: a human temporal bone study. Ann. Otol. Rhinol. Laryngol. 1976;85:94–100. doi: 10.1177/000348947608500117. [DOI] [PubMed] [Google Scholar]
- Hallberg O.E. Sudden deafness of obscure origin. The Laryngoscope. 1956;66:1237–1267. doi: 10.1288/00005537-195610000-00001. [DOI] [PubMed] [Google Scholar]
- Hong S.M., Park C.H., Lee J.H. Hearing outcomes of daily intratympanic dexamethasone alone as a primary treatment modality for ISSHL. Otolaryngol. Head Neck Surg. 2009;141:579–583. doi: 10.1016/j.otohns.2009.08.009. [DOI] [PubMed] [Google Scholar]
- Huy P.T.B., Sauvaget E. Idiopathic sudden sensorineural hearing loss is not an otologic emergency. Otol. Neurotol. 2005;26:896–902. doi: 10.1097/01.mao.0000185071.35328.6d. [DOI] [PubMed] [Google Scholar]
- Jung S.Y., Shim H.S., Hah Y.M., Kim S.H., Yeo S.G. Association of metabolic syndrome with sudden sensorineural hearing loss. JAMA Otolaryngol. Head Neck Surg. 2018;144:308–314. doi: 10.1001/jamaoto.2017.3144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kakehata S., Sasaki A., Oji K., Futai K., Ota S., Makinae K., Shinkawa H. Comparison of intratympanic and intravenous dexamethasone treatment on sudden sensorineural hearing loss with diabetes. Otol. Neurotol. 2006;27:604–608. doi: 10.1097/01.mao.0000224092.79635.ee. [DOI] [PubMed] [Google Scholar]
- Kleyn A.D. Sudden complete or partial loss of function of the octavus-system in apparently normal persons. Acta Otolaryngol. 1944;32:407–429. doi: 10.3109/00016484409119921. [DOI] [Google Scholar]
- Koors P.D., Thacker L.R., Coelho D.H. ABR in the diagnosis of vestibular schwannomas: a meta-analysis. Am. J. Otolaryngol. 2013;34:195–204. doi: 10.1016/j.amjoto.2012.11.011. [DOI] [PubMed] [Google Scholar]
- Kosyakov S., Atanesyan A., Gunenkov A., Ashkhatunyan E., Kurlova A. Intratympanic steroids for sudden sensorineural hearing loss. Int. Adv. Otol. 2011;7:323–332. (n.d) [Google Scholar]
- Lai D., Zhao F., Jalal N., Zheng Y. Intratympanic glucocorticosteroid therapy for idiopathic sudden hearing loss: meta-analysis of randomized controlled trials. Medicine (Baltim.) 2017;96 doi: 10.1097/MD.0000000000008955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laird N., Wilson W.R. Predicting recovery from idiopathic sudden hearing loss. Am. J. Otolaryngol. 1983;4:161–164. doi: 10.1016/s0196-0709(83)80038-6. [DOI] [PubMed] [Google Scholar]
- Lan W.-C., Wang C.-Y., Lin C.-D. Pentoxifylline versus steroid therapy for idiopathic sudden sensorineural hearing loss with diabetes. J. Int. Adv. Otol. 2018;14:176–180. doi: 10.5152/iao.2018.4690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence R., Thevasagayam R. Controversies in the management of sudden sensorineural hearing loss: an evidence-based review. Clin. Otolaryngol. 2015;40:176–182. doi: 10.1111/coa.12363. [DOI] [PubMed] [Google Scholar]
- Lefebvre P.P., Staecker H. Steroid perfusion of the inner ear for sudden sensorineural hearing loss after failure of conventional therapy: a pilot study. Acta Otolaryngology. 2002;122(7):698–702. PMID:12484644. [PubMed] [Google Scholar]
- Liebau A., Pogorzelski O., Salt A.N., Plontke S.K. Hearing changes after intratympanically applied steroids for primary therapy of sudden hearing loss: a meta-analysis using mathematical simulations of drug delivery protocols. Otol. Neurotol. 2017;38:19–30. doi: 10.1097/MAO.0000000000001254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim H.J., Kim Y.T., Choi S.J., Lee J.B., Park H.Y., Park K., Choung Y.-H. Efficacy of 3 different steroid treatments for sudden sensorineural hearing loss: a prospective, randomized trial. Otolaryngol. Head Neck Surg. 2013;148:121–127. doi: 10.1177/0194599812464475. [DOI] [PubMed] [Google Scholar]
- López-González M.A., Cambil E., Abrante A., López-Fernández R., Esteban F. [Sound therapy in sudden deafness] Acta Otorrinolaringol. Esp. 2012;63:165–172. doi: 10.1016/j.otorri.2011.09.004. [DOI] [PubMed] [Google Scholar]
- Mattox D.E., Simmons F.B. Natural history of sudden sensorineural hearing loss. Ann. Otol. Rhinol. Laryngol. 1977;86:463–480. doi: 10.1177/000348947708600406. [DOI] [PubMed] [Google Scholar]
- Megighian D., Bolzan M., Barion U., Nicolai P. Epidemiological considerations in sudden hearing loss: a study of 183 cases. Arch. Oto-Rhino-Laryngol. 1986;243:250–253. doi: 10.1007/BF00464440. [DOI] [PubMed] [Google Scholar]
- Nakagawa T., Ogino-Nishimura E., Hiraumi H., Sakamoto T., Yamamoto N., Ito J. Audiometric outcomes of topical IGF1 treatment for sudden deafness refractory to systemic steroids. Otol. Neurotol. 2012;33:941–946. doi: 10.1097/MAO.0b013e31825f251a. [DOI] [PubMed] [Google Scholar]
- Narozny W., Kuczkowski J., Mikaszewski B. Thyroid dysfunction--underestimated but important prognostic factor in sudden sensorineural hearing loss. Otolaryngol. Head Neck Surg. 2006;135:995–996. doi: 10.1016/j.otohns.2006.05.753. [DOI] [PubMed] [Google Scholar]
- Niedermeyer H.P., Zahneisen G., Luppa P., Busch R., Arnold W. Cortisol levels in the human perilymph after intravenous administration of prednisolone. Audiol. Neuro. Otol. 2003;8:316–321. doi: 10.1159/000073516. [DOI] [PubMed] [Google Scholar]
- Nosrati-Zarenoe R., Hultcrantz E. Corticosteroid treatment of idiopathic sudden sensorineural hearing loss: randomized triple-blind placebo-controlled trial. Otol. Neurotol. 2012;33:523–531. doi: 10.1097/MAO.0b013e31824b78da. [DOI] [PubMed] [Google Scholar]
- Nyberg S., Abbott N.J., Shi X., Steyger P.S., Dabdoub A. Delivery of therapeutics to the inner ear: the challenge of the blood-labyrinth barrier. Sci. Transl. Med. 2019;11 doi: 10.1126/scitranslmed.aao0935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oiticica J., Bittar R.S.M. Metabolic disorders prevalence in sudden deafness. Clinics. 2010;65:1149–1553. doi: 10.1590/S1807-59322010001100017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okamoto H., Fukushima M., Teismann H., Lagemann L., Kitahara T., Inohara H., Kakigi R., Pantev C. Constraint-induced sound therapy for sudden sensorineural hearing loss--behavioral and neurophysiological outcomes. Sci. Rep. 2014;4:3927. doi: 10.1038/srep03927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plontke S.K. Diagnostics and therapy of sudden hearing loss. GMS Curr. Top. Otorhinolaryngol., Head Neck Surg. 2017;16:Doc05. doi: 10.3205/cto000144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plontke S.K., Glien A., Rahne T., Mäder K., Salt A.N. Controlled release dexamethasone implants in the round window niche for salvage treatment of idiopathic sudden sensorineural hearing loss. Otol Neurotol. 2014;35(7):1168–1171. doi: 10.1097/MAO.0000000000000434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos H.V.L., Barros F.A., Yamashita H., Penido N. de O., Souza A.C.V. de, Yamaoka W.Y. Magnetic resonance imaging in sudden deafness. Braz. J. Otorhinolaryngol. 2005;71:422–426. doi: 10.1016/s1808-8694(15)31193-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rauch S.D., Halpin C.F., Antonelli P.J., Babu S., Carey J.P., Gantz B.J., Goebel J.A., Hammerschlag P.E., Harris J.P., Isaacson B., Lee D., Linstrom C.J., Parnes L.S., Shi H., Slattery W.H., Telian S.A., Vrabec J.T., Reda D.J. Oral vs intratympanic corticosteroid therapy for idiopathic sudden sensorineural hearing loss: a randomized trial. J. Am. Med. Assoc. 2011;305:2071–2079. doi: 10.1001/jama.2011.679. [DOI] [PubMed] [Google Scholar]
- Rhee T.M., Hwang D., Lee J.S., Park J., Lee J.M. Addition of hyperbaric oxygen therapy vs medical therapy alone for idiopathic sudden sensorineural hearing loss: a systematic review and meta-analysis. JAMA Otolaryngol. Head Neck Surg. 2018 doi: 10.1001/jamaoto.2018.2133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Si Y., Jiang H.L., Chen Y.B., Chu Y.G., Chen S.J., Chen X.M., He W.H., Zheng Y.Q., Zhang Z.G. Round window niche drilling with intratympanic steroid is a salvage therapy of sudden hearing loss. Audiol. Neuro. Otol. 2018;23:309–315. doi: 10.1159/000493086. [DOI] [PubMed] [Google Scholar]
- Simmons F.B. Sudden idiopathic sensori-neural hearing loss: some observations. The Laryngoscope. 1973;83(8):2112–2117. doi: 10.1288/00005537-197308000-00005. https://onlinelibrary.wiley.com/doi/abs/10.1288/00005537-197308000-00005 [WWW Document], n.d. (accessed 7.18.18) [DOI] [PubMed] [Google Scholar]
- Spear S.A., Schwartz S.R. Intratympanic steroids for sudden sensorineural hearing loss: a systematic review. Otolaryngol. Head Neck Surg. 2011;145:534–543. doi: 10.1177/0194599811419466. [DOI] [PubMed] [Google Scholar]
- Stachler R.J., Chandrasekhar S.S., Archer S.M., Rosenfeld R.M., Schwartz S.R., Barrs D.M., Brown S.R., Fife T.D., Ford P., Ganiats T.G., Hollingsworth D.B., Lewandowski C.A., Montano J.J., Saunders J.E., Tucci D.L., Valente M., Warren B.E., Yaremchuk K.L., Robertson P.J., American Academy of Otolaryngology-Head and Neck Surgery Clinical practice guideline: sudden hearing loss. Otolaryngol. Head Neck Surg. 2012;146:S1–S35. doi: 10.1177/0194599812436449. [DOI] [PubMed] [Google Scholar]
- Stokroos R.J., Albers F.W., Tenvergert E.M. Antiviral treatment of idiopathic sudden sensorineural hearing loss: a prospective, randomized, double-blind clinical trial. Acta Otolaryngol. 1998;118:488–495. doi: 10.1080/00016489850154603. [DOI] [PubMed] [Google Scholar]
- Tran Ba Huy P., Sauvaget E. Idiopathic sudden sensorineural hearing loss is not, at this time, an otologic emergency. Ann. Otolaryngol. Chir. Cervicofac. 2007;124:66–71. doi: 10.1016/j.aorl.2006.12.003. [DOI] [PubMed] [Google Scholar]
- Vlastarakos P.V., Papacharalampous G., Maragoudakis P., Kampessis G., Maroudias N., Candiloros D., Nikolopoulos T.P. Are intra-tympanically administered steroids effective in patients with sudden deafness? Implications for current clinical practice. Eur. Arch. Oto-Rhino-Laryngol. 2012;269:363–380. doi: 10.1007/s00405-011-1738-0. [DOI] [PubMed] [Google Scholar]
- Wei B.P.C., Stathopoulos D., O’Leary S. Steroids for idiopathic sudden sensorineural hearing loss. Cochrane Database Syst. Rev. 2013;CD003998 doi: 10.1002/14651858.CD003998.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westerlaken B.O., de Kleine E., van der Laan B., Albers F. The treatment of idiopathic sudden sensorineural hearing loss using pulse therapy: a prospective, randomized, double-blind clinical trial. The Laryngoscope. 2007;117:684–690. doi: 10.1097/mlg.0b013e3180316d3b. [DOI] [PubMed] [Google Scholar]
- Westerlaken B.O., Stokroos R.J., Dhooge I.J.M., Wit H.P., Albers F.W.J. Treatment of idiopathic sudden sensorineural hearing loss with antiviral therapy: a prospective, randomized, double-blind clinical trial. Ann. Otol. Rhinol. Laryngol. 2003;112:993–1000. doi: 10.1177/000348940311201113. [DOI] [PubMed] [Google Scholar]
- Wilson W.R., Byl F.M., Laird N. The efficacy of steroids in the treatment of idiopathic sudden hearing loss. A double-blind clinical study. Arch. Otolaryngol. 1980;106:772–776. doi: 10.1001/archotol.1980.00790360050013. [DOI] [PubMed] [Google Scholar]
- Zadeh M.H., Storper I.S., Spitzer J.B. Diagnosis and treatment of sudden-onset sensorineural hearing loss: a study of 51 patients. Otolaryngol. Head Neck Surg. 2003;128:92–98. doi: 10.1067/mhn.2003.50. [DOI] [PubMed] [Google Scholar]