Visual Abstract
Dr Arora discloses a financial relationship with Mallickrodt Pharmaceuticals, Abbott Nutrition, and Edwards Lifesciences.
The Thoracic Surgery Social Media Network (TSSMN) was formed in 2015 as a collaborative effort between The Annals of Thoracic Surgery and The Journal of Thoracic and Cardiovascular Surgery.1 The primary goals of the initiative were to bring social media attention to key publications from both journals and to highlight major accomplishments in cardiothoracic surgery. TSSMN has established a presence in the social media community, achieving its goals through the activity of delegates who tweet content related to recent journal publications, live-tweet the specialty’s annual meetings, and host live TweetChats featuring key articles published in cardiothoracic surgery to engage manuscript authors, readers, and the virtual community in scholarly discussion. 2, 3, 4, 5
Given the unprecedented global impact of the novel coronavirus disease 2019 (COVID-19), TSSMN pivoted from its usual TweetChats focusing on manuscript discussion to focus on supporting cardiothoracic surgeons during the pandemic (declared March 11, 2020). A 1-hour TweetChat was held on March 29, 2020, at which time, there were more than 750,000 confirmed cases worldwide with a death toll of more than 36,000. Themes and questions for discussion were crowd sourced during the preceding days from the TSSMN community through social media and were summarized into topics to be addressed during the TweetChat. The TweetChat drew 7.5 million impressions, 2587 tweets, and 273 participants, with most of the respondents from the United States (56%), followed by Canada (25%), Europe (13%), and Asia (6%) (Table 1 ).
Table 1.
Thoracic Surgery Social Media Network COVID-19 TweetChat Analytics
| Variables | Definition | Number |
|---|---|---|
| Tweets | Message originating from an individual | 2587 |
| Tweets/participant (average) | Average number of messages per individual | 9 |
| Participants | Participants of TweetChat that joined by tweeting #TSSMN during the #COVID19 TweetChat | 273 |
| Impressions | Number of unique views of tweets from the TweetChat | 7.5 million |
COVID-19, novel coronavirus disease 2019; TSSMN, Thoracic Surgery Social Media Network.
TweetChat topics included (1) triaging of patients for cardiothoracic surgery, (2) surgical education during COVID-19, (3) overcoming limited resources and personal protective equipment (PPE), (4) tips and tricks to keep one’s home and family safe from COVID-19, and (5) the role of the cardiothoracic surgery community in combating the COVID-19 pandemic. Given the debatable aspects of issues raised, 24 separate Twitter polls (Table 2 ) were used during the TweetChat to form a consensus and generate discussion surrounding practice patterns and opinions as we navigate these uncharted waters together.
Table 2.
Twitter Pollsa
| Crowd-Sourced Topics | Poll Question | Respondents, No. |
|---|---|---|
| Demographics | Geographic location | 32 |
| Career/training status | 25 | |
| Triaging patients during the pandemic | Ambulatory clinic | 60 |
| Delayed surgical management of early staged lung cancer | 35 | |
| Diversion of early staged lung cancer patients to other modalities | 24 | |
| Appropriateness of heart/lung transplantations | 113 | |
| Management of left main coronary artery disease | 32 | |
| Management of symptomatic severe valvular disease | 41 | |
| Management of symptomatic severe aortic aneurysmal disease | 37 | |
| Surgical education | Impact on residency, fellowship, and job interviews | 34 |
| Impact on licensing examinations | 21 | |
| Preferred approach to licensing examinations | 18 | |
| Impact on didactic sessions | 35 | |
| Impact on clinical/operative educational experiences | 32 | |
| Limited resources | Availability of PPE | 34 |
| Policies surrounding use of PPE | 49 | |
| N95 respirator use recommendations | 94 | |
| Types of aerosolizing procedures | 39 | |
| Preoperative COVID-19 testing | 38 | |
| Availability of hospital resources | 32 | |
| Ventilatory strategies | 19 | |
| Keeping family and home safe | Changes to living space | 26 |
| Plans for self-isolation | 68 | |
| Format of TSSMN chat | Usefulness of chat | 13 |
COVID-19, novel coronavirus disease 2019; PPE, personal protective equipment; TSSMN, Thoracic Surgery Social Media Network.
Full responses to the Twitter polls are available at the following link: https://threadreaderapp.com/thread/1244659611166097414.html.
We aim to share the key content from this chat with the readership of The Annals and summarize the discussion of each of the crowd-sourced TweetChat topics, along with the collectively generated potential solutions to the challenges encountered by the cardiothoracic surgical TSSMN online community. Those findings and ideas that are reported reflect those of the online chat participants and may include anecdotal comments or suggestions that lack evidence and warrant further study.
Triaging of Patients for Cardiothoracic Surgery
Depending on the phase of COVID-19 prevalence in hospitals (preparatory, potential or real surge, or overwhelmed), we have needed to evaluate methods for triaging and scheduling patients for cardiothoracic surgery.
Clinic Conduct
In response to questions regarding how cardiothoracic surgeons were conducting their ambulatory clinics, most stated that they were using telehealth (65%), whereas, the remaining respondents were still conducting clinic as usual (12%) or had canceled clinic completely (17%) (n = 60 respondents for poll). Some surgeons indicated that they were taking urgent referrals only, deferring all nonurgent referrals. Further comments from surgeons during the chat addressed the utility of telehealth in successfully shifting patient care to be more patient-centered and safe during COVID-19.
Thoracic Surgical Procedures
For patients with stage I or II lung cancer, of the 35 cardiothoracic surgeons who addressed this question, 20 (57%) opted to delay surgery for 2 to 3 months, 10 (29%) felt that surgery should not be postponed, with 7 of 10 (70%) operating at their next available slot. The remaining respondents would advocate for diversion to alternative treatment modalities (ie, stereotactic body radiation therapy, etc). Comments from surgeons include the importance of multidisciplinary discussions and shared decision making to ensure that the treatment approach selected aligns with the patients’ values and wishes, taking into account heightened risk for contracting COVID-19 if operating now vs progression of oncologic disease if delayed vs risks and benefits of nonstandard of care. More information regarding thoracic oncology surgery triage was cited from the consensus statement from the Thoracic Surgery Outcomes Research Network.6
Regarding the scenario of COVID-19 developing in a postoperative patient with continued air leak, respondents recognized that this would be high-risk with the potential for aerosol generation. Options proposed by respondents include early discharge home with a chest tube drain and reservoir with outpatient chest tube removal with full PPE, or use of digital chest drainage systems with built-in hydrophilic filters.
Adult Cardiac Surgical Procedures
Thirty-two respondents provided their recommendations for patients with left-main coronary artery disease, most whom (20 [63%]) would opt for urgent coronary artery bypass grafting surgery, followed by percutaneous coronary intervention (19%), elective surgery (9%), and medical management (9%). Responses were more disparate regarding management of patients with symptomatic valvular disease: among 41 respondents, 39% preferred urgent surgery, whereas 32% suggested transcatheter therapy, 20% delayed surgery, and 10% opted instead for medical management. Similar responses were provided for symptomatic aortic aneurysms, for which, among 37 surgeons, 60% continued with urgent surgical repair, whereas 32% picked transcatheter therapy, if feasible, and 8% waited for elective surgery.
In terms of heart and lung transplantations, 59% (67 of 113) of poll respondents opted to put these operations on hold. For those respondents who felt that transplantations should continue during the COVID-19 pandemic, additionally provided comments hit on key nuances, addressing the need to prioritize only the most urgent of patients, taking into consideration the risks posed to the health care team during the procurement and operation as well as those to the recipients during their postoperative recoveries in an immunocompromised state and concomitant obligate use of intensive care facilities and resources. More information regarding adult cardiac surgery and congenital surgery triage is available in consensus statements published in The Annals.7 , 8
Surgical Education During the COVID-19 Pandemic
The need for physical distancing has led to the discontinuation of in-person medical school courses, cancellation of educational conferences and licensing examinations, a decline in operative volumes, and modifications to resident scheduling to both limit exposure of personnel and redeploy trainees to areas of need. As the impact of COVID-19 permeates throughout the health care system, surgical education has been put in a state of flux and uncertainty.
Interviews and Examinations
Participants responded that in terms of residency, fellowship, and job interviews, most activities are now held virtually (62%), with the remaining having been canceled (n = 34 respondents for the poll). Among 21 individuals commenting on licensing examinations, 76% stated that their examinations had been put on hold, with fewer numbers continuing on the original timeline (10%) or being held virtually (5%). When trainees were polled regarding the modality and timeline they would prefer for licensing examinations amidst the COVID-19 pandemic, 33% wished to take the examinations remotely on the regular timeline, 33% preferred remotely but with a delay of more than 3 months, 23% would rather delay for 1 year until the next sitting, whereas only 11% desired the examinations to be held in person as usual (n = 18 respondents for the poll).
Didactic and Operative Curriculum
Academic sessions have been put on hold (54%) or are held virtually (43%), according to 35 respondents on this poll. The comments provided touched on the benefit of technology for streaming didactics live and on-demand as well as for providing modified clinical educational experiences, such as virtual rounds to engage remote learners and patient families, while minimizing exposure for all. Among 32 poll participants, 25 (78%) stated that operative experience had decreased due to lessened case-volume or modification to trainee schedule, or both, to minimize exposure, with the remaining trainees having been redeployed to areas of need in the care of patients with COVID-19. A number of additional comments were provided, and the needs for re-education and proper training for those in new or alternative roles, care, and protection of those who become ill, flexibility and adaptation of current educational milestones, and providing psychosocial support to trainees were emphasized.
Overcoming Limited Resources and PPE
The pandemic raises concerns regarding limited resource allocation, including the rationing of resources. These carry significant implications for the well-being of patients and providers alike.
PPE and Testing
Of 34 respondents, 62% stated that there was a perceived lack of PPE at their institutions, whereas those who denied experiencing a shortage still indicated that their institutions were rationing resources. PPE policies at the institutions of poll participants varied greatly, with 45% (22 of 49) needing to wear surgical masks everywhere in the hospital, and 37% indicating that N95 respirator use was reserved for aerosol-generating procedures.
Respondents also had varying experiences with regard to routine preoperative testing of cardiothoracic surgical patients. Among 38 respondents to this poll, 42% emphasized the importance of testing, given the high rates of asymptomatic carriers, whereas 50% reported inadequate availability of such tests. However, others cautioned that false-negative test results could be inappropriately reassuring and that the sensitivity of the test may be affected by the low viral load of asymptomatic carriers.
Ultimately, the need to protect health care workers through availability of N95 respirators and full PPE for aerosol-generating procedures for all patients, regardless of COVID-19 status, was emphasized.
Methods to resterilize contaminated PPE with ultraviolet radiation, heat, and vaporized hydrogen peroxide, among other methods, were discussed, although whether these strategies are effective remains to be determined, and the evidence is rapidly evolving. More information regarding mask reuse strategies was cited from the Society of American Gastrointestinal and Endoscopic Surgeons (https://www.sages.org/n-95-re-use-instructions).
In addition, the members of the TweetChat community commented on an evolving role for the use of smoke evacuation systems or air-seal devices in the use of cautery and any carbon dioxide insufflation due to the potential of aerosol generation, with possible transitions away from minimally invasive procedures among some chat participants. For open airway procedures, there was a clear consensus to avoid the use of thoracic-abdominal (TA) staplers or, if the TA stapler was deemed necessary, to use a “double stapling” technique. Again, we note that those were opinions of participants, and evidence supporting the avoidance of minimally invasive procedures, such as robotic lung surgery in the setting of COVID-19, has not been demonstrated.
Shortage of Hospital Resources
Among the 32 respondents, 72% stated that there was concern regarding the number of key hospital resources required in the treatment of patients with COVID-19, including ventilators, hospital beds, and intensive care unit beds. Participants highlighted the need for transparency in reporting of availability of health care resources as well as prediction of health care resource utilization for COVID-19 to identify capacity constraints and need for support. In addition, they emphasized the importance of a coordinated response to prepare for the surge, to secure access to the various supply chains, as well as utilize innovative ways to augment hospital capacity (eg, repurposing of public facilities). Furthermore, the need to protect health care workers to ensure sustainability of our workforce as well as early detection, isolation, and testing were highlighted to combat the rapid spread of COVID-19.
More information regarding infection mitigation strategies in the operating room and surgical recovery is available in a consensus statement published in The Annals. 9
Tips and Tricks to Keep One’s Home and Family Safe From COVID-19
In our care of patients with COVID-19 as health care providers, we inadvertently risk exposing our families to the virus. When asked how one’s living situation has changed with COVID-19, most respondents stated that it had not changed (65%), although a large proportion stated that they self-isolate in their own room (31%), and a small minority (4%) were choosing to stay at the hospital or live in a hotel (n = 26 respondents for poll). Interestingly, responses shifted significantly when participants were asked what they would do if they were exposed to a patient with COVID-19 with no PPE and were asymptomatic. Among 68 respondents, 41% would self-isolate within their home, 32% would quarantine away from home, and the remainder would use PPE at home if unable to self-isolate.
Ultimately, participants echoed that one’s response to exposure depends on context and consequences. If one had a high-risk exposure or lived with vulnerable individuals at home, then one ought to weigh those issues into their consideration of self-isolation. Overarching chat recommendations included making contingency plans if physicians or their family members were to become infected and, further, to have advanced care directives in place.
Anecdotal tips shared for decontamination routines after working at the hospital included bringing only disposable containers, changing or showering, or both, before going home (or immediately upon arrival), wiping down all personal belongings, distancing from high-risk family members, leaving shoes outside, and setting up a contaminated and noncontaminated area in one’s home, if possible. In addition, participants stated the need to minimize use of any personal items that may act as fomites for COVID-19 transmission, including but not limited to, use of the laptops, bags, white coat, stethoscope, ties, and personal accessories, and to use telemedicine alternatives wherever appropriate.
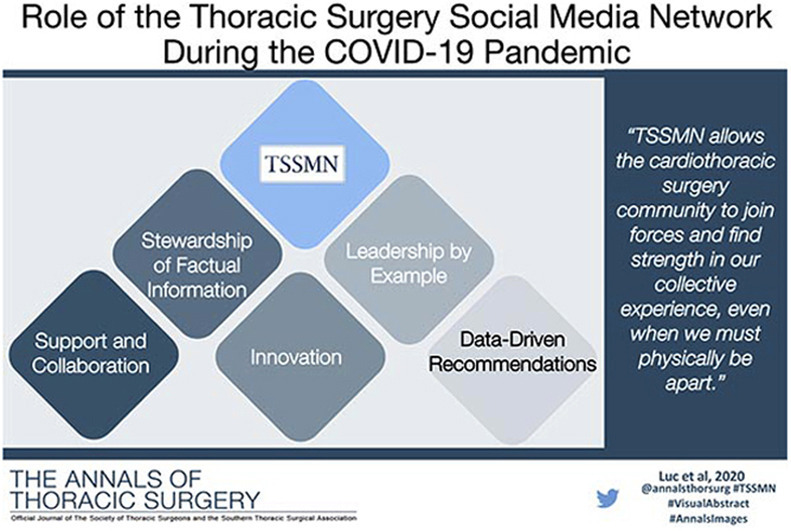
The Role of the Cardiothoracic Surgery Community and TSSMN in the COVID-19 Pandemic
The following themes emerged during the TweetChat in the discussion regarding the role of TSSMN in the COVID-19 pandemic.
Community Support and Collaboration
TSSMN has a role in uniting the global cardiothoracic surgery community to foster collaboration and sharing of information, resources, and research opportunities. Given the potential physical, emotional, and mental stress of this pandemic, it may be advantageous to rely on the collective experience of our cardiothoracic surgical community to learn together from each other, rather than apart. Health care is a team sport.
Stewardship of Factual Information
To mitigate harm to population health, TSSMN serves a role to combat misinformation through the dissemination of critical postpublication scholarly peer reviewed literature on COVID-19. This includes, but is not limited to, those put forth in cardiothoracic surgical journals and from cardiothoracic surgical societies, including ethical guidelines10 and tiered triage guidelines for adult cardiac surgery,7 congenital cardiac surgery,8 and thoracic malignancies.6 The promotion of transparent and trustworthy information can aid in public education, empowerment, and ultimately, individual responsibility in the treatment and prevention of COVID-19.
Innovation
Now is the time for our collective community to collaborate and be creative in ways to scale up and innovate to solve the problems. TSSMN may help facilitate such efforts to help propel and amplify open-source hackathons to address shortages in necessary medical equipment (eg, #BuildForCOVID19), raise awareness of challenges faced by health care workers (eg, #GetMePPE), and empower the public to take charge of their own health and safety of others (eg, #StayHomeSaveLives). In addition, TSSMN may aid virtual learning and education techniques for trainees and surgeons through streaming of didactics and facilitating study/discussion groups beyond the regular TSSMN activities of TweetChats and live-tweeting of meetings.
Leading by Example
TSSMN can help share ways in which cardiothoracic surgeons across the globe are leading by example and finding ways to contribute their skills. Opportunities include serving on the team to perform much needed procedures to expedite patient care, assuming or assisting in alternative roles, and dynamic health system restructuring within the ever-evolving hospital environment. We are ultimately serving humanity. Everyone is in a unique battle against COVID-19. One very important role of a surgeon in a pandemic is to help grow hospital capacity by triaging elective operations and thereby preserving personnel and hospital resources.
Disseminate Content That is Data-Driven and Evidence-Based
Social media is useful for disseminating and promoting not only evidence-based practices but also tools for collecting and reporting data relating to COVID-19. TSSMN can encourage greater use of The Society of Thoracic Surgeons’ National Database tracking surgical outcomes of cardiothoracic surgery patients with and without COVID-19 as well as distribute resource utilization prediction tools.
Limitations
This study is subject to a number of limitations that should be considered. Owing to the nature of Twitter polls and their anonymous and voluntary nature, they are subject to responder bias and lack internal and external validity. In addition, TSSMN is an online community, thereby excluding those who are not engaged in social media.
Conclusion
We have demonstrated the feasibility of TSSMN to facilitate communication among the global cardiothoracic surgery community in an unprecedented time of public health crisis, enabling us to join forces, collaborate, and find strength from our collective experiences with COVID-19, even when we must physically be apart.
Acknowledgments
Dr Arora has received an unrestricted educational grant from Pfizer Canada Inc.
References
- 1.Antonoff M.B. Thoracic Surgery Social Media Network: bringing thoracic surgery scholarship to Twitter. Ann Thorac Surg. 2015;100:383–384. doi: 10.1016/j.athoracsur.2015.06.049. [DOI] [PubMed] [Google Scholar]
- 2.Luc J.G.Y., Varghese T.K., Antonoff M.B. Participating in TweetChat: practical tips from The Thoracic Surgery Social Media Network (#TSSMN) Ann Thorac Surg. 2019;107:e229–e233. doi: 10.1016/j.athoracsur.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 3.Luc J.G.Y., Antonoff M.B. Live tweet The Society of Thoracic Surgeons annual meeting: how to leverage Twitter to maximize your conference experience. Ann Thorac Surg. 2018;106:1597–1601. doi: 10.1016/j.athoracsur.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 4.Luc J.G.Y., Ouzounian M., Bender E.M. The Thoracic Surgery Social Media Network: early experience and lessons learned. Ann Thorac Surg. 2019;108:1248–1255. doi: 10.1016/j.athoracsur.2019.06.011. [DOI] [PubMed] [Google Scholar]
- 5.Ni hlci T., Archer M., Harrington C., Luc J.G.Y., Antonoff M.B. The Trainee Thoracic Surgery Social Media Network: a pilot study in social media use. Ann Thorac Surg. 2020;109:285–290. doi: 10.1016/j.athoracsur.2019.05.083. [DOI] [PubMed] [Google Scholar]
- 6.Thoracic Surgery Outcomes Research Network, Inc COVID-19 guidance for triage of operations for thoracic malignancies: a consensus statement from Thoracic Surgery Outcomes Research Network. Ann Thorac Surg. 2020;110:692–696. doi: 10.1016/j.athoracsur.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haft J.W., Atluri P., Ailawadi G. Adult cardiac surgery during the COVID-19 pandemic: a tiered patient triage guidance statement. Ann Thorac Surg. 2020;110:697–700. doi: 10.1016/j.athoracsur.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stephens E.H., Dearani J.A., Guleserian K.J. COVID-19: crisis management in congenital heart surgery. Ann Thorac Surg. 2020;110:701–706. doi: 10.1016/j.athoracsur.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Engelman D.T., Lother S., George I. Adult cardiac surgery and the COVID-19 pandemic: aggressive infection mitigation strategies are necessary in the operating room and surgical recovery. Ann Thorac Surg. 2020;110:707–711. doi: 10.1016/j.athoracsur.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Drake D., Morrow C.D., Kinlaw K., De Bonis M., Zangrillo A., Sade R.M. Cardiothoracic surgeons in pandemics: ethical considerations. Ann Thorac Surg. 2020;110:355–358. doi: 10.1016/j.athoracsur.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]


