Abstract
Midgut volvulus complicating congenital malrotation is a rare but life-threatening condition that can occur in pregnancy. We present a case of intestinal infarction resulting from midgut volvulus in a healthy 32-week pregnant woman who underwent emergency laparotomy and small bowel resection in the setting of fetal death in utero. This case highlights several challenging issues in diagnosing and managing this uncommon condition which leads to increased adverse perinatal outcomes. Prompt investigation and definitive surgical treatment are required when pregnant women present with bilious vomiting and new-onset abdominal or back pain especially beyond the first trimester.
Keywords: pregnancy, gastrointestinal surgery
Background
Bowel obstruction is rare in pregnancy with an approximate incidence of 1 in 10 000.1 The first case of intestinal obstruction in pregnancy secondary to sigmoid volvulus was described in 1885 where the patient delivered a stillborn infant and she passed away 2 days later.2 Although uncommon, volvulus is the second leading cause of intestinal obstruction in pregnancy, occurring in up to 25% of cases, as compared with its involvement in only 3%–5% non-pregnant women, due to gravid uterus.2
Intestinal malrotation is a congenital abnormality that results from the failure of complete intestinal rotation and its subsequent fixation during early fetal development. This leads to the midgut mesentery being long and narrow-based in its attachment to the retroperitoneum, thus allowing the midgut to twist with relative ease around the superior mesenteric vascular pedicle. If left untreated, midgut volvulus results in a closed-loop mechanical small bowel obstruction and infarction of tissues supplied by the superior mesenteric artery. This condition typically presents in children.3 4 It is uncommonly seen in adulthood, let alone in pregnancy.
Here, we describe a rare case of midgut volvulus secondary to congenital malrotation in late pregnancy, which resulted in extensive infarction of the small and large bowel, as well as fetal death in utero (FDIU).
Case presentation
A 27-year-old G1P0 woman of 32 weeks’ gestation presented to our birthing suite with gradual onset of back pain associated with nausea and bilious vomiting. Her medical history was unremarkable aside from hyperemesis gravidarum during her first trimester of pregnancy. She has been complaining of intermittent back pain and nausea and vomiting antenatally but these were always regarded as normal pregnancy symptoms.
On presentation, she described a 2-week history of worsening nausea and vomiting, which became bilious 3 days prior to her hospital admission. This was associated with increasing anorexia, back pain and irregular bowel actions. Importantly, she denied recent trauma, abdominal pain, per vaginal discharge or fevers.
On examination, she appeared dehydrated, although her vital signs were all within normal limits. Her abdomen was soft and not tender. A gravid uterus appropriate for her gestational age was palpable. Her back was not tender to touch. A healthy fetal heart rate was confirmed on cardiotocography (CTG). She remained in the birthing suite for observation and was treated with intravenous fluids, antiemetics and analgesia.
Five hours later, she developed new-onset acute abdominal pain. Her abdomen was tender to palpation and worse in the epigastrium. Speculum examination was performed and revealed a closed and uneffaced cervix with no evidence of vaginal loss. Fetal fibronectin test was also negative.
However, the patient remained distressed with abdominal pain despite oral analgesia. An hour later, her abdomen appeared distended and peritonitic. She deteriorated haemodynamically with an elevated heart rate of 150 beats/min, an increased respiratory rate of 24 breaths/min and a fall in blood pressure to 100/80 mm Hg. A surgical review was immediately consulted. Intravenous crystalloid, intramuscular morphine and betamethasone were promptly administered. CTG was reapplied but failed to detect a fetal heart rate. Unfortunately, a bedside ultrasound confirmed FDIU.
Investigations
Full blood examination, liver function test, renal function test, lipase and C-reactive protein (CRP) on admission were all unremarkable.
Serial blood tests which were performed 5 hours later revealed metabolic acidosis (pH 7.13), elevated lactate of 10.2 mmol/L, leucocytosis of 21.1×109/L, CRP of 13 mg/L and evidence of acute kidney injury (creatinine: 130 mmol/L, estimated glomerular filtration rate: 49 mL/min/1.73 m2). Random blood glucose level was also elevated at 12 mmol/L. Her haemoglobin and liver function remained normal.
Differential diagnosis
When the patient first presented, she was managed as having normal back pain and vomiting in pregnancy. Her admission blood tests were completely normal and therefore she was managed conservatively.
When the patient developed new onset of abdominal pain 5 hours later and subsequently deteriorated with shock in the setting of FDIU, intra-abdominal haemorrhage was suspected with uterine rupture and massive concealed placenta abruption considered as the most likely preliminary diagnosis. However, the absence of per vaginal bleeding and a drop in the haemoglobin level did not support that differential diagnosis.
Acute fatty liver of pregnancy and acute pancreatitis were ruled out due to normal liver function test, blood glucose level and lipase. Ruptured splenic artery aneurysm was also considered as an important differential diagnosis requiring exclusion due to severe epigastric pain and haemodynamic instability.
Despite being afebrile, abnormally elevated lactate and significant tachycardia, tachypnoea and hypotension raised suspicion of occult sepsis.
Treatment
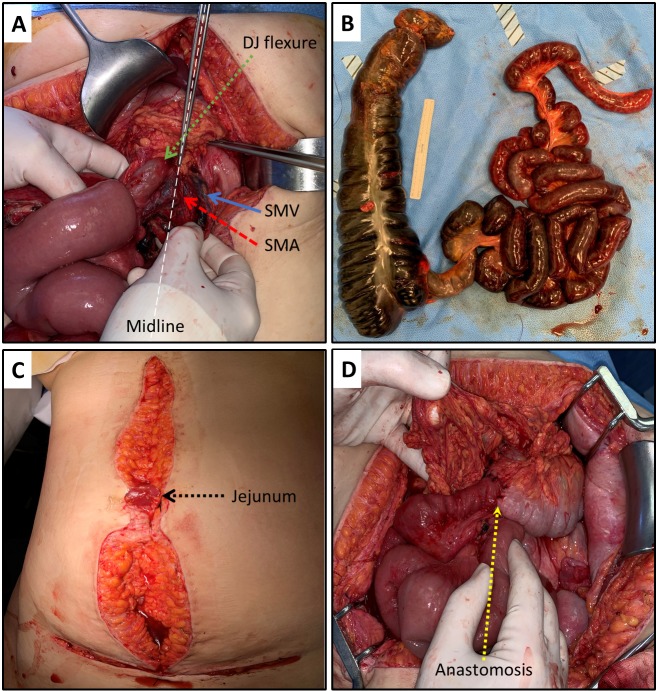
Given the presence of an acute abdomen, the patient was promptly transferred to theatre under the care of obstetrics and general surgery teams. A lower uterine segment caesarean section was performed to deliver a stillborn female infant of 2070 g. There was no evidence of abruption, uterine rupture or frank haemoperitoneum. However, malodourous peritoneal fluid and infarcted bowel were detected necessitating a formal midline laparotomy. This revealed midgut volvulus in the setting of congenital malrotation (figure 1A). Following manual detorsion and active warming of the small and large intestine, 6 m of infarcted bowel extending from mid-jejunum to distal transverse colon was resected (figure 1B). Due to the patient’s ongoing haemodynamic instability and the potential of further ischaemic-reperfusion injury to the remaining intestines, a primary anastomosis was not attempted. Instead, her abdomen was closed with a cusp of jejunum exposed at the skin level to facilitate monitoring (figure 1C) in the intensive care unit (ICU).
Figure 1.
Operative management of midgut volvulus in pregnancy. (A) Laparotomy demonstrating the presence of congenital malrotation. White dotted line corresponds to the axis of forceps demonstrating the midline. Green dotted arrow identifies the duodenojejunal (DJ) flexure located to the right of the midline. The superior mesenteric artery (SMA, red broken arrow) is located to the right of the superior mesenteric vein (SMV, blue solid arrow). (B) Six metres of infarcted small and large bowel resected due to midgut volvulus in the setting of congenital malrotation. (C) Cusp of jejunum brought up to the laparotomy wound demonstrating the viability of the residual small bowel. (D) Dotted yellow arrow demonstrating the jejunocolonic anastomosis fashioned following relook laparotomy.
A relook laparotomy was conducted the next day following normalisation of physiological parameters. Given the lack of further ischaemia to the small bowel, a jejunocolonic anastomosis was fashioned to restore gastrointestinal continuity (figure 1D). In total, 2.5 m of the intestine (2 m of the small bowel, 0.5 m of the large bowel) remained in situ.
Outcome and follow-up
Following 3 days in ICU, the patient was transferred to the surgical ward with input from allied health teams. She was weaned off total parental nutrition over the following 2 weeks with minimal evidence of short gut syndrome. She received nutritional, psychological as well as social support and made an unremarkable recovery.
Discussion
Currently, there are no consensus guidelines describing the management of bowel obstruction and in particular, midgut volvulus in pregnancy. To the best of our knowledge, this is the first case of midgut volvulus in third trimester where extensive small and large bowel resection has been performed with an excellent maternal outcome. Despite this, FDIU was encountered and potentially avoidable. The diagnosis of midgut volvulus and congenital malrotation in pregnancy is challenging and not always immediately apparent until surgery as demonstrated in our case. This is due to several reasons. First, the symptoms of midgut volvulus, abdominal pain, nausea, vomiting and constipation are shared with most normal pregnancies.5–7 In retrospect, symptoms of intermittent volvulus were suggested by new-onset back pain and vomiting. This was initially rationalised to be consistent with normal pregnancy symptoms. The transition to bilious vomiting 3 days prior to hospital presentation is in keeping with worsening small bowel obstruction secondary to progressive midgut volvulus. This subtle but critical piece of information was, however, not appreciated on clinical assessment. The abrupt onset of severe abdominal pain, distension, peritonism and deranged biochemistry are late manifestations of bowel infarction secondary to complete mesenteric torsion.7
Second, the normal physiological changes that occur in pregnancy could mask the early signs of bowel obstruction.5 For instance, leucocytosis and raised inflammatory markers are expected in a well pregnant woman, whereas this would usually heighten suspicion for sepsis in non-pregnant individuals. Similarly, tachycardia is very common especially in late gestation due to increased cardiac output from the gravid uterus. In our case, false reassurance was created as the patient had a completely normal blood test and stable haemodynamic at presentation.
Third, the hesitation of using radiological investigations in pregnancy is a major barrier to achieving a diagnosis. The main reason is the fear of radiation exposure to the fetus.8 9 MRI, CT and abdominal X-rays have all been reported to be useful in diagnosing bowel obstruction and its underlying aetiology in the general population as well as in pregnancy.3–8 Diagnostic features of midgut volvulus on imaging include (1) a ‘whirlpool sign’ of the superior mesenteric pedicle and (2) closed-loop small bowel obstruction.8 Characteristic features of intestinal malrotation on imaging include (1) location of the duodenojejunal flexure to the right of the spinal column, (2) the superior mesenteric artery located to the right of its associated vein, (3) the caecum located to the left of the spinal column, (4) small bowel loops that are predominately found in the right side of the abdomen and (5) colon that is predominately found in the left side of the abdomen. Pregnant women need to be adequately informed that the radiation exposure for all these studies is well below 10 rad which is the current maximum radiation dose that a fetus can be safely exposed to.9
In conclusion, despite a lack of consensus detailing the optimal management of midgut volvulus in pregnancy, awareness of this rare but life-threatening condition is critical. The combination of meticulous clinical assessment, short-interval serial observations and judicious use of radiological investigations will facilitate prompt diagnosis and treatment. Timely surgical intervention is necessary to avoid devastating perinatal outcomes.10
Patient’s perspective.
This was my first ever pregnancy. My pregnancy seemed to be going ‘normal’ until approximately 24 weeks gestation when I started to experience abdominal discomfort and upper to mid back pain which was associated with severe nausea and vomiting when I was lying in bed one night. I also experience hot and cold flushes, shaking and sweating. I was taken to the hospital two times during weeks 24 and 25 of my pregnancy. I was told the symptoms I was experiencing was ‘normal’ and was subsequently sent home with antinausea medication.
However, my symptoms persisted and they would mostly appear during the night while I was lying or sitting in bed. I had made sure to tell the midwives at all my antenatal appointments of my symptoms and what I was experiencing as I was unsure of this being my first pregnancy.
I began to experience the symptoms more frequently in the 2 weeks prior to my hospital admission at 32 weeks which also then included severe constipation. The weekend of my admission at 32 weeks, I had been vomiting yellow bile and was feeling extremely unwell. On the day of my admission, I was vomiting green bile and the pain in my back and abdomen had become excruciating despite the pain killers. Looking back, it ‘felt’ like I was dying. Everything was far from normal.
I would have gladly had tests and scans done were they recommended and deemed safe for my baby. I truly believe my ‘now condition’ and circumstances could have been different had the imaging been performed.
Learning points.
Pregnant women presenting with abdominal pain, bilious vomiting and obstipation should always prompt further investigation to exclude small bowel obstruction and its underlying aetiology such as a midgut volvulus.
Bowel obstruction in pregnancy is rare and limited diagnostic reassurance can be derived from a patient’s normal blood test and haemodynamic stability.
Pregnancy itself should not limit the use of imaging studies if there is a high suspicion of intra-abdominal pathologies as early diagnosis could significantly decrease perinatal mortality and morbidity.
Acknowledgments
The authors would like to acknowledge Mr. Krinal Mori, a general surgeon at the Northern Hospital, for providing his valuable insight into this case report.
Footnotes
Contributors: EC: gathered data and prepared the manuscript. DSL: made critical revisions to the manuscript. NS and VR: responsible for the overall supervision of the project.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Redlich A, Rickes S, Costa S-D, et al. Small bowel obstruction in pregnancy. Arch Gynecol Obstet 2007;275:381–3. 10.1007/s00404-006-0262-8 [DOI] [PubMed] [Google Scholar]
- 2.Perdue PW, Johnson HW, Stafford PW. Intestinal obstruction complicating pregnancy. Am J Surg 1992;164:384–8. 10.1016/S0002-9610(05)80910-9 [DOI] [PubMed] [Google Scholar]
- 3.Hwang SM, Na YS, Cho Y, et al. Midgut volvulus as a complication of intestinal malrotation in a term pregnancy. Korean J Anesthesiol 2014;67:S98–9. 10.4097/kjae.2014.67.S.S98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gião Antunes AS, Peixe B, Guerreiro H. Midgut volvulus as a complication of intestinal malrotation in pregnancy. ACG Case Rep J 2017;4:e9. 10.14309/crj.2017.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cong Q, Li X, Ye X, et al. Small bowel volvulus in mid and late pregnancy: can early diagnosis be established to avoid catastrophic outcomes? Int J Clin Exp Med 2014;7:4538–43. [PMC free article] [PubMed] [Google Scholar]
- 6.Constanthin PE, Darouichi M. Volvulus of the small bowel due to malrotation during pregnancy: a Case-Report. J Dig Dis Diagnos 2017;1:34–40. 10.14302/issn.2574-4526.jddd-17-1497 [DOI] [Google Scholar]
- 7.Mahdavi A, Yunesi N. Small bowel volvulus in a primigravida woman: case report. J Fam Reprod Health 2001;1:51–4. [Google Scholar]
- 8.Kouki S, Fares A, Alard S. MRI whirpool sign in midgut volvulus with malrotation in pregnancy. JBR-BTR 2013;96:360–1. 10.5334/jbr-btr.460 [DOI] [PubMed] [Google Scholar]
- 9.Committee on Obstetric Practice Committee opinion no. 723: guidelines for diagnostic imaging during pregnancy and lactation. Obstet Gynecol 2017;130:e210–6. 10.1097/AOG.0000000000002355 [DOI] [PubMed] [Google Scholar]
- 10.Webster PJ, Bailey MA, Wilson J, et al. Small bowel obstruction in pregnancy is a complex surgical problem with a high risk of fetal loss. Ann R Coll Surg Engl 2015;97:339–44. 10.1308/003588415X14181254789844 [DOI] [PMC free article] [PubMed] [Google Scholar]