Abstract
A 26-year-old woman presented after an intentional ingestion of 20 g of caffeine. She suffered a profound respiratory alkalosis with metabolic acidosis, hypokalaemia and sustained polymorphic ventricular tachycardia. She was treated with intravenous intralipid and haemodialysis, and her arrhythmia was controlled using magnesium sulphate. Once invasively ventilated and unable to hyperventilate the patient became acidotic and required intravenous bicarbonate to correct her acid–base status. Two days following the overdose the patient was extubated, haemodialysis was stopped and norepinephrine was weaned off. The patient was discharged after a further 7 days. Serial caffeine levels were taken during this patient’s care; the highest measured caffeine concentration 7 hours after ingestion was 147.1 mg/L. The known lethal dose of caffeine is 80 mg/L. Intralipid and haemodialysis represent a new and viable treatment in life-threatening caffeine overdose. Intravenous magnesium may terminate unstable arrhythmias in caffeine-poisoned patients.
Keywords: arrhythmias, cardiovascular system, poisoning, adult intensive care, toxicology
Background
Approximately 90% of adults in the western world report regular caffeine use, most commonly through drinking coffee or tea, with an average daily intake of 223 mg/day for caffeine users.1
Caffeine has 99% oral bioavailability within 45 min of ingestion, with no significant first-pass effect. Peak plasma concentrations are reached within 30 min of ingestion.2 Caffeine is eliminated via first-order kinetics, with half-lives showing significant intrasubject variation from 2.3 to 9.9 hours.
It is generally accepted that caffeine doses below 400 mg/day are safe and associated with agreeable effects such as alertness, concentration and relaxation. Sublethal overdoses of around 7–10 mg/kg cause anxiety, irritability, nausea, tremor, palpitations, flushing and headache.3 Caffeine ingestions of greater than 1–2 g cause significant toxic effects. Fatal caffeine overdoses have occurred following ingestions of >5 g4 or with blood caffeine concentrations >80 mg/L.5 6 The toxic effects of caffeine vary, including hypotension and hypertension, malignant arrhythmias, myocardial ischaemia, gastrointestinal disturbances, agitation, cerebral oedema, hyperkalaemia and hypokalaemia, hyponatraemia, hypocalcaemia, respiratory alkalosis, lactic acidosis and rhabdomyolysis.3
Case presentation
A 26-year-old, 86.3 kg woman presented to the emergency department following an ingestion of two heaped teaspoons of powdered caffeine (20 g), or 231 mg/kg, 3 hours prior to hospital attendance. She denied alcohol consumption, illicit drugs or smoking. She had a history of depression and panic disorder, for which she took fluoxetine and propranolol. The patient also takes the combined contraceptive pill.
In the emergency department, the patient initially reported palpitations, sweating, anxiety and dyspnoea but denied any other symptoms. Observations on triage showed a heart rate of 109 beats/min, blood pressure 116/67 mm Hg, respiratory rate 17 breaths/min, saturations 99% in room air and a temperature of 35.5°C. Glasgow Coma Scale on presentation was 14/15, but decreased while in the emergency department and the patient became increasingly agitated and tachypnoeic. The patient vomited a small amount of gastric contents.
Physical and neurological examination revealed a regular tachycardia, hypotension and hyperventilation, but were otherwise unremarkable. The patient also vomited a small amount of gastric contents.
Investigations
Initial ECG showed a polymorphic ventricular tachycardia.
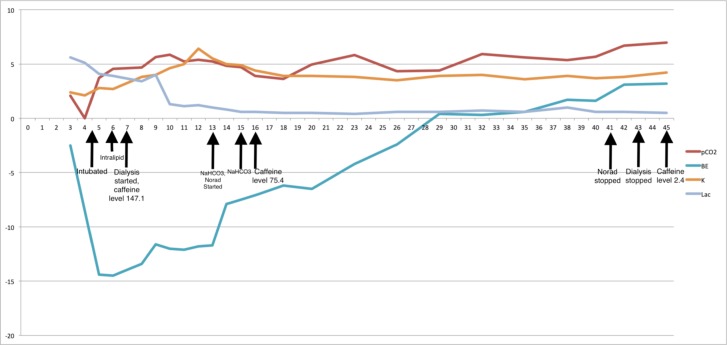
Initial arterial blood gas taken on room air showed a metabolic acidosis with respiratory alkalosis; pH was 7.60, pCO2 2.06 kPa, pO2 25.36 kPa, bicarbonate 22.1 mmol/L, base excess −2.5 mmol/L, potassium 2.4 mmol/L, lactate 5.6 mmol/L. Serial arterial blood gases were measured during the patient’s treatment (figure 1).
Figure 1.
The pCO2, base excess, potassium and lactate levels, with important interventions indicated by arrows.
Laboratory findings showed a leucocytosis (white cell count 19.9×109 cells/L), but other blood tests were unremarkable.
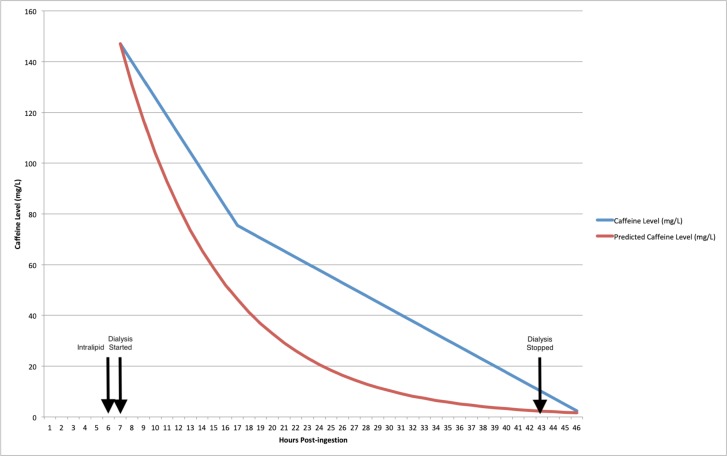
The first caffeine level (147.1 mg/L) was measured 7 hours after the ingestion and following the administration of intralipid, but before haemodialysis was initiated. Caffeine levels were measured intermittently, and the results are displayed against a first order elimination curve assuming a half-life of 6 hours (figure 2). Approximately one half-life and an administration of intralipid had passed before the first caffeine level was measured, so peak caffeine concentrations were likely significantly higher.
Figure 2.
Serial serum caffeine levels were measured. The results are displayed against the known elimination of caffeine (assuming a half-life of 6 hours), with intralipid and dialysis indicated by arrows. Peak caffeine concentration was 147.1 mg/L.
Treatment
Initial management was with fluid and electrolyte replacement, but the patient remained alkalotic, hypokalaemic and in ventricular tachycardia. She was therefore admitted to the intensive care unit for central vascular access, haemodialysis, electrolyte replacement, cardiac monitoring and invasive ventilation. The patient was sedated with midazolam and fentanyl, and paralysed with rocuronium. Fifty grams of activated charcoal was administered, as well as intravenous intralipid.
Following the above treatment, and with haemodialysis ongoing, the patient’s ECG briefly reverted to sinus rhythm before returning to ventricular tachycardia. Serial arterial blood gases demonstrated rapid acid–base and electrolyte shifts, and the patient became acidotic and hyperkalaemic (see above). This responded to 2× boluses of 100 mL of 1.4% sodium bicarbonate. Administration of 20 mmol of magnesium caused the cardiac rhythm to revert to sinus tachycardia, and the patient then remained in sinus rhythm. Despite this, the patient remained hypotensive, and so norepinephrine was initiated.
The day after the overdose, she remained intubated, ventilated, sedated and on dialysis with cardiac monitoring. The rocuronium was discontinued. On the second day, sedation and haemofiltration were stopped and she was extubated uneventfully. Renal indices and acid-–base status remained within normal limits following the discontinuation of haemofiltration, and there were no further witnessed arrhythmias on cardiac monitoring.
Outcome and follow-up
The patient was monitored on the intensive care unit for 7 further days; she had one episode of tachypnoea and desaturation thought to be secondary to aspiration pneumonia, but this resolved and she was discharged with ongoing psychiatric support but no further medical follow-up.
The last follow-up was roughly a month after discharge, when the patient visited the intensive care unit to thank the team that took care of her. She reported feeling well in herself, was well-supported by her family and had been engaging well with psychiatric care.
Discussion
The varied effects of caffeine overdose can be explained by the broad range of receptors targeted by caffeine. Caffeine acts as an adenosine receptor antagonist and, at toxic concentrations, inhibits phosphodiesterase enzymes and promotes intracellular calcium release. Other important effects include catecholamine release, and the activation of Na/K ATPase channels.3
Adenosine receptors are widespread throughout the body, and their antagonism causes central nervous system (CNS) stimulation as well as positive ionotropic and chronotropic effects.7 This is consistent with the agitation exhibited by the patient, as well as the ventricular tachycardia that responded to the ion channel-stabilising effects of magnesium.
The antagonism of phosphodiesterase enzymes explains the hypotension requiring norepinephrine even after sinus rhythm was restored, while catecholamine release and Na/K ATPase activation can account for the metabolic disturbances which likely exacerbated the patient’s malignant arrhythmias. Excessive catecholamine release causes lipolysis and glycogenolysis leading to pyruvate production and, if pyruvate is not aerobically metabolised, lactataemia and a metabolic acidosis.8
The majority of caffeine metabolites are renally cleared, while a further 2%–3% of ingested caffeine is excreted unaltered in the urine.9 Caffeine shows low (10%–35%) protein binding, has a small volume of distribution and is extensively filtered at the renal glomerulus, but 98% of filtered caffeine is then reabsorbed in the renal tubule.10 Haemodialysis, therefore, could potentially have a significant impact on the elimination of caffeine from the poisoned patient, and it has been employed in previous cases of caffeine overdose.11 The moderately lipophilic nature of caffeine suggests a role for the administration of intralipid in the removal of caffeine.12 13
Female sex, obesity and the use of the contraceptive pill significantly slow caffeine elimination.14–16 Ninety-five per cent of caffeine metabolism occurs in the liver via the enzyme CYP1A2 of the cytochrome p450 family of enzymes which are inhibited by the use of the contraceptive pill, while women are known to exhibit reduced CYP450 activity.10 With this in mind, the patient is likely to have cleared the caffeine from her bloodstream slower than the general population, which is consistent with the measured caffeine levels showing a mean half-life of 6.5 hours despite the use of intralipid and dialysis.
Patient’s perspective.
I found out about caffeine overdoses from an article in Daily Mail Australia about a teenager who had died after taking two teaspoons of caffeine powder. I went online and bought 1 kg of powdered caffeine for £29.99 with next day delivery. My family and I are shocked that you can buy such a dangerous amount of caffeine so easily and cheaply.
Learning points.
Physiological, cardiovascular and metabolic disturbances in caffeine overdose may develop simultaneously and present a moving target for clinicians supporting a patient’s physiology.
Patients are often agitated and tachypnoeic, develop unstable arrhythmias, acid–base and electrolyte disturbances.
Caffeine overdoses over 5 g, as well as those presenting with metabolic derangements or unstable arrhythmias should be managed in an intensive care setting.
No guidelines exist on the management of caffeine overdose, but this and other case reports suggest that intralipid and haemodialysis appear to be an effective treatment for caffeine toxicity.
The use of magnesium appeared to resolve the ventricular tachycardia, which may be lifesaving in caffeine-poisoned patients with unstable arrhythmias. Other reports have demonstrated the use of propranolol or esmolol in caffeine-induced ventricular dysrhythmias.3 17
Footnotes
Contributors: RH managed the patient, conceived the case report, collected and analysed patient data, and authored the report. SJT managed the patient, collected and analysed patient data, and authored the report. TC managed the patient, collected patient data and provided editorial support for the manuscript. AA managed the patient, collected patient data and provided editorial support for the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Frary CD, Johnson RK, Wang MQ. Food sources and intakes of caffeine in the diets of persons in the United States. J Am Diet Assoc 2005;105:110–3. 10.1016/j.jada.2004.10.027 [DOI] [PubMed] [Google Scholar]
- 2.Blanchard J, Sawers SJ. The absolute bioavailability of caffeine in man. Eur J Clin Pharmacol 1983;24:93–8. 10.1007/BF00613933 [DOI] [PubMed] [Google Scholar]
- 3.Willson C. The clinical toxicology of caffeine: a review and case study. Toxicol Rep 2018;5:1140–52. 10.1016/j.toxrep.2018.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kerrigan S, Lindsey T. Fatal caffeine overdose: two case reports. Forensic Sci Int 2005;153:67–9. 10.1016/j.forsciint.2005.04.016 [DOI] [PubMed] [Google Scholar]
- 5.Banerjee P, Ali Z, Levine B, et al. Fatal caffeine intoxication: a series of eight cases from 1999 to 2009. J Forensic Sci 2014;59:865–8. 10.1111/1556-4029.12387 [DOI] [PubMed] [Google Scholar]
- 6.Cappelletti S, Piacentino D, Fineschi V, et al. Caffeine-Related deaths: manner of deaths and categories at risk. Nutrients 2018;10:611. 10.3390/nu10050611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sheth S, Brito R, Mukherjea D, et al. Adenosine receptors: expression, function and regulation. Int J Mol Sci 2014;15:2024–52. 10.3390/ijms15022024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sepkowitz KA. Energy drinks and caffeine-related adverse effects. JAMA 2013;309:243. 10.1001/jama.2012.173526 [DOI] [PubMed] [Google Scholar]
- 9.Alsabri SG, Mari WO, Younes S, et al. Kinetic and dynamic description of caffeine. J Caffeine Adenosine Res 2018;8:3–9. 10.1089/caff.2017.0011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arnaud MJ. Pharmacokinetics and metabolism of natural methylxanthines in animal and man. Handb Exp Pharmacol 2011;200:33–91. 10.1007/978-3-642-13443-2_3 [DOI] [PubMed] [Google Scholar]
- 11.Ishigaki S, Fukasawa H, Kinoshita-Katahashi N, et al. Caffeine intoxication successfully treated by hemoperfusion and hemodialysis. Intern Med 2014;53:2745–7. 10.2169/internalmedicine.53.2882 [DOI] [PubMed] [Google Scholar]
- 12.Fabrizio C, Desiderio M, Coyne RF. Electrocardiogram abnormalities of caffeine overdose. Circ Arrhythm Electrophysiol 2016;9. 10.1161/CIRCEP.115.003088 [DOI] [PubMed] [Google Scholar]
- 13.Muraro L, Longo L, Geraldini F, et al. Intralipid in acute caffeine intoxication: a case report. J Anesth 2016;30:895–9. 10.1007/s00540-016-2198-x [DOI] [PubMed] [Google Scholar]
- 14.Nehlig A. Interindividual differences in caffeine metabolism and factors driving caffeine consumption. Pharmacol Rev 2018;70:384–411. 10.1124/pr.117.014407 [DOI] [PubMed] [Google Scholar]
- 15.Kamimori GH, Somani SM, Knowlton RG, et al. The effects of obesity and exercise on the pharmacokinetics of caffeine in lean and obese volunteers. Eur J Clin Pharmacol 1987;31:595–600. 10.1007/BF00606637 [DOI] [PubMed] [Google Scholar]
- 16.Abernethy DR, Todd EL. Impairment of caffeine clearance by chronic use of low-dose oestrogen-containing oral contraceptives. Eur J Clin Pharmacol 1985;28:425–8. 10.1007/BF00544361 [DOI] [PubMed] [Google Scholar]
- 17.Andrade A, Sousa C, Pedro M, et al. Dangerous mistake: an accidental caffeine overdose. BMJ Case Rep 2018;2018. 10.1136/bcr-2018-224185. [Epub ahead of print: 08 Jun 2018]. [DOI] [PMC free article] [PubMed] [Google Scholar]