Abstract
The current study assessed the efficacy of a brief video intervention (Prevention of Post-Rape Stress [PPRS]) delivered in the emergency department to recent sexual assault (SA) victims. PPRS was compared to treatment as usual (TAU) and an active control condition (Pleasant Imagery and Relaxation Instruction [PIRI]). Primary outcomes were posttraumatic stress disorder (PTSD) symptoms and perceived present control. Prior SA was examined as a moderator of treatment effects. Women (n = 233; aged 15 years and older; 59.70% identified as a racial or ethnic minority) who received a post-SA medical forensic exam participated in the study ( NCT01430624). Participants were randomized to watch the PPRS video (n = 77), the PIRI video (n = 77), or receive TAU (n = 79). Participants completed measures of PTSD symptoms and perceived present control 1.5-, 3-, and 6-months post-SA. An interaction between condition and prior SA was found on PTSD symptom frequency and on perceived present control. Among women with a prior SA, women in the PPRS versus TAU condition reported less frequent PTSD symptoms 6-months post-SA. Those in the PPRS condition had lower perceived present control than those in the TAU condition among those with no prior SA 3-months post-SA. However, at 6-months post-SA, among women with a prior SA, women in the PPRS reported higher perceived present control than those in TAU. These findings partially replicate a prior study in which PPRS was found to be beneficial in mitigating the development of PTSD symptoms, but only for women with a prior SA.
Keywords: sexual assault, PTSD, clinical trials, computer/Internet technology, secondary prevention
Sexual assault (SA), ranging from nonconsensual sexual contact to completed rape, is common in the United States with approximately 20% of women reporting attempted or completed rape in their lifetime (Smith et al., 2018). SA exposure is associated with greater risk of general mental health problems, with particularly strong relations with trauma-related symptoms and suicidality (Dworkin, Menon, Bystrynski, & Allen, 2017). Factors associated with lower risk of distress have also been identified, including perceived control over the recovery process (e.g., Ullman & Peter-Hagene, 2014). Although there are several evidence-based treatments for posttraumatic stress disorder (PTSD; e.g., Foa, Hembree, & Rothbaum, 2007; Resick, Monson, & Chard, 2016), efforts to prevent the onset or persistence of PTSD symptoms among recently sexually assaulted individuals have not received as much attention. This study assessed a video-based prevention program delivered immediately after a post-SA medical forensic exam visit on PTSD symptoms and perceived control.
Post-SA Medical Forensic Exam and Perceived Present Control
Although mental health sequalae after SA are well-documented, only 68.9% of emergency departments (EDs) that provide SA medical forensic exams have mental health counselors available for same day services (Patel et al., 2013), and there is no standard protocol for prevention of mental health symptoms post-SA. The SA medical forensic exam (SAMFE) includes provision of acute medical care, prevention for sexually transmitted infections, and forensic collection of information and samples that can aid in a police investigation. This exam takes place typically within 72–120 hr of the SA (Office on Violence Against Women, 2013) and allows for a unique opportunity to prevent post-SA mental health sequalae concurrently with prevention of sexually transmitted infections.
Natural recovery after SA is common; however, it is unclear what factors are associated with natural recovery versus the experience of ongoing PTSD symptoms. The temporal model of control distinguishes among various aspects of control, only some of which are adaptive following SA or other potentially traumatic events (Frazier, Berman, & Steward, 2001). Specifically, focusing on aspects of traumatic events that are currently uncontrollable such as the occurrence of the event (past control) or preventing the event from happening again (future control) are associated with poorer mental health in SA survivors (Frazier, 2003). By contrast, focusing on what is controllable in the present, including the recovery process (perceived present control), is associated with lower distress (e.g., Frazier, 2003; Walsh & Bruce, 2011). In a large sample of SA victims, perceived present control over recovery served as an indirect pathway from positive social reactions to assault disclosure and fewer PTSD symptoms (Ullman & Peter-Hagene, 2014). In addition, higher perceived present control in SA victims was associated with less problem drinking, more positive reactions to mental health professionals, and fewer suicide attempts (Peter-Hagene & Ullman, 2014; Ullman & Najdowski, 2009; Ullman & Peter-Hagene, 2014). Interventions that aim to increase present control reduce symptoms of anxiety, depression, and stress in college students (e.g., Hintz, Frazier, & Meredith, 2015), particularly among students with a history of interpersonal violence (e.g., Nguyen-Feng et al., 2016). Extending this work, this study examined an intervention targeting post-SA PTSD to determine whether there were increases in perceived present control in addition to reductions in post-SA mental health symptoms (PTSD).
Secondary Prevention for Post-SA Mental Health Symptoms After Recent SA
To date, only two acute post-SA mental health interventions have been empirically examined in ED settings. One acute secondary prevention program is a modified brief prolonged exposure (PE) treatment (Rothbaum et al., 2012), and the other is a brief post-rape video intervention (Prevention of Post-Rape Stress [PPRS]; Resnick, Acierno, Amstadter, Self-Brown, & Kilpatrick, 2007; Resnick, Acierno, Waldrop, et al., 2007). The modified brief PE treatment was adapted to ED settings and included three 1 hr weekly sessions conducted by a clinician trained in PE. Although the modified PE treatment has promising preliminary effects at mitigating the development of PTSD symptoms (Rothbaum et al., 2012), it requires significant resources, including clinicians trained in PE to be available within the ED, and repeated therapy visits by recent victims, a sample that experiences large barriers to health care visits post-SA (Darnell et al., 2015). Therefore, a video aimed at secondary prevention of mental health sequalae after a SA that can be delivered in a single session could have a broader impact on post-SA mental health. A video intervention has several additional benefits in that it can be standardized, requires no staff training, and requires only minimal additional resources within the ED for post-SA medical forensic exams. The PPRS video targets post-rape mental health concerns including PTSD and is available in standard (approximately 18 min that consists of both exam preparation and post-SA coping strategy modeling and instruction; Resnick, Acierno, Amstadter, et al., 2007; Resnick, Acierno, Waldrop, et al., 2007) and brief (approximately 9-min segment of coping strategies only; Miller, Cranston, Davis, Newman, & Resnick, 2015) formats.
The standard PPRS presented during the post-SA medical forensic exam was effective, compared to treatment as usual (TAU) which does not address mental health except for referrals or inpatient psychiatric hospitalization, at mitigating the development of PTSD symptoms among recent SA victims with a prior SA (Resnick, Acierno, Waldrop, et al., 2007). The brief PPRS was effective for mitigating the development of state anxiety post-SA and at a 2-month follow-up assessment compared to TAU, regardless of SA history (Miller et al., 2015). Women without a prior SA reported lower PTSD symptoms than women with a prior SA in the brief PPRS condition at 2-week follow-up but no interaction was found post-SA or at 2-month follow-up. PPRS has been compared to TAU in previous studies, but to our knowledge, no studies have examined the PPRS compared to an active comparison on mental health outcomes.
The only study comparing PPRS to an active comparison examined substance use outcomes (Walsh et al., 2017; 2019). The active comparison was a commercially available video that provided mindfulness skills including breathing skills, relaxation, and imagery (Pleasant Imagery and Relaxation Instruction [PIRI]). Although to our knowledge the PIRI video has not undergone scientific testing in relation to post-SA posttraumatic stress symptoms, the use of mindfulness skills can decrease anxiety (see Manzoni, Pagnini, Castelnuovo, & Molinari, 2008). PIRI, however, has been found to be associated with reductions in post-SA opioid misuse when provided during the SA medical forensic exam among women with a prior SA history (Gilmore et al., 2019). However, no research has examined if the PPRS is more effective than an active control, like the PIRI, at mitigating the development of posttraumatic stress symptoms.
Current Study
The current study assessed the efficacy of a brief video intervention (PPRS) delivered during the SAMFE in terms of mitigating the development of post-SA PTSD and increasing perceived present control up to 6 months post-exam both over time and at each follow-up. Time points examined included 1.5-, 3-, and 6-months post-SA medical forensic exam. The first follow-up (1.5 months) was chosen to allow for ample time for participants to be able to meet criteria for PTSD within the follow-up procedures. The 3-month follow-up was included because among SA victims, those who do not meet criteria for PTSD 3-months after the SA had steady improvement in mental health symptoms over time, while those with PTSD at 3-months post-SA had a long-term PTSD diagnosis (Rothbaum, Foa, Riggs, Murdock, & Walsh, 1992). The 6-month assessment was used to assess the long-term maintenance of PTSD post-SA.
PPRS was compared to TAU and an active control condition (PIRI), given that relaxation can reduce anxiety (see Manzoni et al., 2008). PPRS was hypothesized to be more effective at mitigating the development of PTSD and increasing perceived present control compared to the TAU and PIRI conditions. Given that prior research (Resnick, Acierno, Waldrop, et al., 2007) has found prior SA history to moderate the effect of PPRS, moderation was examined. Covariates were examined including age, minority status, and whether the SA was drug or alcohol facilitated given the differential outcomes based on SA type (Zinzow et al., 2010). Changes in PTSD symptoms and perceived present control were examined both over time and at each time point.
Method
Participants
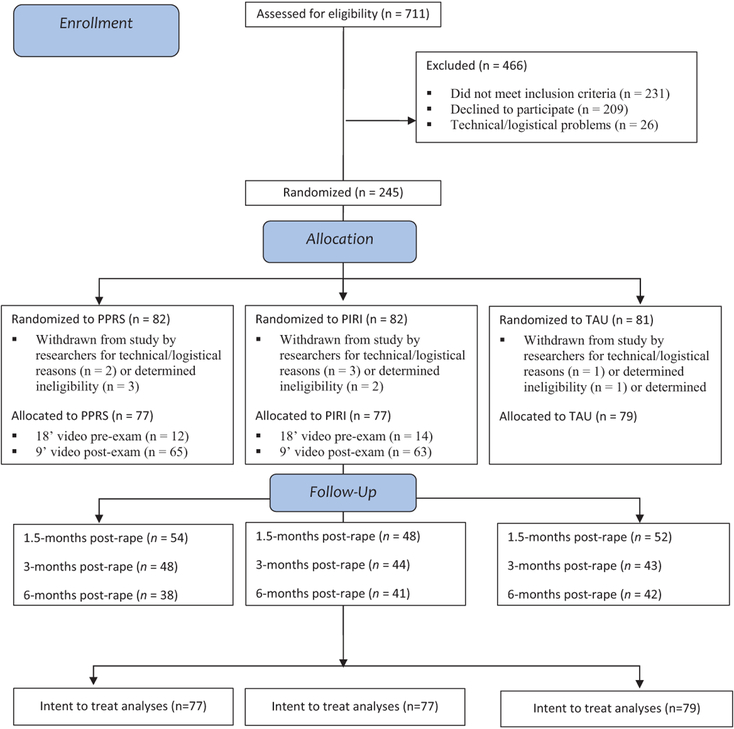
Girls and women aged 15 years or older who were recent victims of SA (rape, suspected rape, or attempted rape) and received a SAMFE within 7 days of assault at one of two medical centers in a Midwestern metropolitan area were assessed for eligibility by medical personnel (N = 711; see Figure 1 for CONSORT diagram). A total of 466 were excluded because they declined to participate (n = 209), did not meet inclusion criteria (n = 231), or because of technical/logistical problems (n = 26). Those that did not meet inclusion criteria (n = 231) were non-English speaking or were unable to consent due to serious injuries or medical issues, psychological distress (e.g., inability to answer questions or watch a video due to distress), or acute intoxication. Of the remaining 245, 233 completed the condition to which they were randomly assigned: PPRS (n = 77), PIRI (n = 77), and TAU (n = 79). A computerized random numbers generator assigned participants to each condition using a stratified blocked randomization procedure with variable block sizes of 9 or 12.
Figure 1.
CONSORT Diagram
Of the 233 participants, 154 (66%) completed one or more follow-up assessments at 1.5-, 3-, and 6-months post-SA (54 in PPRS, 48 in PIRI, 52 in TAU). Comparisons to non-completers indicated no differences on age or race except that those who participated were more likely to indicate more than one race than nonparticipants, 11.6% versus 1.7%, χ2 (1, N = 407) = 14.2, p < .0005. Treatment groups also did not differ in terms of age, minority status, marital status, education, household income, student status, or employment status.
Measures
Demographics.
Participants provided self-report data on their age, race/ethnicity, marital status, education, student/employment status, and household income.
Prior SA.
At the medical exam and at initial follow-up (T1), participants were asked whether, other than the incident that brought them to the hospital, anyone had ever used force or threat of force to have unwanted sexual contact with them. A “yes” response to either question was coded as 1.
Drug- or alcohol-facilitated rape.
To determine classification of drug- or alcohol-facilitated or incapacitated SA/rape (DAFR), women were asked about use of alcohol or drugs at the time of the assault, whether use was voluntary or whether the assailant(s) gave them drugs or tried to get them drunk, and whether they passed out due to substance use or were awake but too intoxicated to know what they were doing or to control their behavior. Those reporting either of the latter indicators of impairment due to substances were classified as DAFR. This was assessed at time 1 (1.5-months post-SA). Participants were also classified as experiencing DAFR if they indicated that they had passed out in their report to the ED.
PTSD symptoms.
PTSD symptoms were assessed at the 1.5-, 3-month, and 6-month follow-up using the Posttraumatic Diagnostic Scale (PDS; Foa, Cashman, Jaycox, & Perry, 1997) in reference to the Past 2 weeks consistent with previous publications (e.g., Resnick, Acierno, Waldrop, et al., 2007). Symptoms were assessed in response to the index SA for which participants sought a medical exam. The PDS assesses the frequency of symptoms using 17 items rated from 0 (not at all or only one time) to 3 (5 or more times a week/almost always); total scores range from 0 to 51. The recommended clinical cutoff score for the PDS is 20 (Foa et al., 1993; Foa, Zoellner, & Feeny, 2006). The PDS has shown acceptable internal consistency in past research (Foa et al., 1997) and in the current sample (α = .89–.92). Consistent with the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5; American Psychiatric Association, 2013) guidelines, pre-intervention PTSD was not assessed because exams occurred within 7 days of a SA.
Perceived present control.
Perceived present control was measured at the 1.5-, 3-, and 6-month follow-up with the eight-item perceived present control sub-scale of the Perceived Control over Stressful Events Scale (Frazier et al., 2012; Frazier et al., 2011). This scale assesses perceptions of control over aspects of stressors and traumas that are more controllable in the present (vs. focusing on past or future control). Participants rated items on a 1 (strongly disagree) to 4 (strongly agree) scale with regard to the SA over the past week (e.g., “I have control over how I think about the assault”). Acceptable internal consistency has been established for this scale (Frazier et al., 2011) and was demonstrated in the current sample (α = .79–.87).
Intervention Conditions
PPRS.
This video entitled Steps to Recovery included a female narrator providing information to prevent future emotional problems and substance abuse, such as instructions for implementation of self-directed exposure exercises, methods to recognize and terminate inappropriate avoidance, and strategies to engage in activities that specifically did not involve substance use and to avoid situations or cues that have been triggers for use. Participants either received a shorter video (9 min; 82% of participants) or a longer (18 min video; 18% of participants). The longer video included information about what to expect during a SAMFE and was shown in the beginning of the study. However, due to the needs of the ED setting and to not disrupt clinical flow, the video was moved to after the SAMFE; therefore, information about what to expect during a SAMFE was removed, resulting in the shorter video. Prior to the video, participants were provided with the following information about the video: “The video was developed to help women and girls learn some effective ways to deal with problems that sometimes happen after a SA.”
PIRI.
This video included a female narrator providing instructions in diaphragmatic breathing, use of words such as relax paired with exhalation, instructions regarding muscle relaxation, and pleasant nature-related imagery and sounds. The original commercial product entitled Relax©, David Garrigus Productions, was edited for content and length. Similar to PPRS, there were short (9 min; 82% of participants) and long (18 min; 18% of participants) versions of the video. Prior to watching the video, participants were provided with the following information about the video: “The video was developed to help women and girls learn relaxation skills to deal with problems that sometimes happen after a SA.”
TAU.
TAU involved completion of an SAMFE performed by an SA Nurse Examiner. This includes a physical exam as well as information about local resources. All participants received TAU; however, TAU refers to the TAU-only condition.
Procedures
Procedures were approved by two university and two affiliated hospital Institutional Review Boards and are listed on clinicaltrials.gov ( NCT01430624). Participants provided written informed consent at the time of the SAMFE, which included access to medical records and self-report information. Videos and other procedures were administered in a private room within the hospital. On average, participants in both the PPRS and PIRI conditions indicated that they were able to pay attention to the video (M = 3.19 and 3.07 out of 4, respectively). Participants completed three structured telephone follow-up interviews targeted at 1.5-, 3-, and 6-months post-SA conducted by Counseling Psychology doctoral students and the assessors were blind to the treatment condition of the participants (for more information regarding procedures, see Walsh et al., 2017. Nurses noted whether the video intervention conditions were delivered as intended and in cases in which there were technical difficulties that prevented showing a video as assigned or other procedural problems the participant was withdrawn from the study.
Data Analytic Plan
Descriptive statistics were calculated using the intent to treat sample. Unconditional and conditional latent growth curve models (LGCMs) were estimated separately for PTSD symptoms and perceived present control. A nonsignificant chi-square, comparative fit index (CFI) >.90, Root Mean Square Error of Approximation (RMSEA) <.08, and Standardized Root Mean Square Residual (SRMR) <.05 were indicative of acceptable model fit (Bentler, 1995; Browne & Cudeck, 1993). Regression models were used to predict reported frequency of PTSD symptoms and perceived present control at 1.5-, 3-, and 6-months post-SA.1 At each time point, PTSD symptom frequency and perceived present control were predicted simultaneously to allow for correlated residuals between outcomes measured at the same time. Predictors for the LGCMs and regression models by time point included two dummy coded variables reflecting the contrast between the PPRS (0) and PIRI (1) conditions and the PPRS (0) and TAU (1) conditions, minority status, age, prior SA, and whether the index rape was DAFR and interactions between the dummy coded intervention conditions and prior SA. All main effects (intervention conditions, demographics, prior SA, and DAFR) were entered simultaneously on a single step and then interactions between intervention condition and prior SA were added on the next step. Missing outcome data were not associated with any baseline demographic characteristics, study condition, or other variables. Thus, they were considered to be missing at random (MAR) and handled via robust maximum likelihood (MLR) estimation with robust standard errors. All analyses were conducted in Mplus v8.
Results
Descriptive statistics are presented in Table 1. LGCM results are presented in Table 2. The fit of the unconditional, χ2 (df = 1) = 11.70 p = .0006; CFI =.93; RMSEA = .26; SRMR = .04, conditional main effect, χ2 (df = 7) = 19.71, p = .006; CFI =.94; RMSEA = .09; SRMR = .03, and conditional interaction, χ2 (df = 9) = 19.24, p = .02; CFI =.95; RMSEA = .07; SRMR = .02, models for PTSD were mostly acceptable and suggested that on average, PTSD symptoms declined over follow-up. Women with prior SA and those who self-identified as ethnic minority had more severe PTSD at intercept. No main effects or interactions were significant predictors of PTSD slope.
Table 1.
Descriptive Statistics of Study Variables.
| M (SD) | % (n) | Range | |
|---|---|---|---|
| Prior SA | — | 61.69% (95) | |
| Age | 27.43 (9.70) | 15–56 | |
| Ethnic/racial minority status | — | 59.70% (139) | |
| DAFR | — | 60.40% (93) | |
| PTSD symptoms | |||
| 1.5 months post assault | 26.64 (11.24) | 0–49 | |
| 3 months post assault | 22.76 (12.07) | 0–49 | |
| 6 months post assault | 20.19 (12.55) | 0–47 | |
| Perceived present control | |||
| 1.5 months post assault | 22.92 (4.93) | 9–32 | |
| 3 months post assault | 23.66 (5.64) | 8–32 | |
| 6 months post assault | 24.70 (5.69) | 9–32 | |
Note. Prior SA = prior sexual assault; DAFR = drug- or alcohol-facilitated rape; PTSD = posttraumatic stress disorder.
Table 2.
Latent Growth Curve Model Estimates.
| Intercept | Slope | |||
|---|---|---|---|---|
| B (SE) | β (SE) | B (SE) | β (SE) | |
| PTSD Symptoms Unconditional Model | ||||
| Estimate | 26.79 (.94)*** | 2.45 (.19)*** | −1.55 (.23)*** | −.66 (.13)*** |
| Variance | 119.36 (16.27)*** | 1.0 | 5.50 (1.59)*** | 1.0 |
| PTSD Symptoms Conditional Main Effects Model | ||||
| PIRI versus PPRS | −1.61 (2.05) | −0.07 (0.09) | 0.73 (0.55) | 0.15 (0.12) |
| TAU versus PPRS | 1.30 (2.03) | 0.06 (0.09) | 0.45 (0.54) | 0.09 (0.11) |
| Age | 0.16 (0.10) | 0.14 (0.09) | 0.02 (0.02) | 0.09 (0.09) |
| Prior SA | 4.34 (1.77)** | 0.20 (0.08)** | 0.00 (0.47) | 0.00 (0.10) |
| Minority status | 4.38 (1.75)** | 0.20 (0.08)** | −0.35 (0.45) | −0.08 (0.10) |
| DAFR | 1.10 (1.80) | 0.05 (0.08) | −0.57 (0.44) | −0.12 (0.09) |
| PTSD Symptoms Conditional Interaction Model | ||||
| PIRI versus PPRS × prior SA | 1.06 (4.11) | 0.04 (0.14) | −0.29 (1.06) | −0.05 (0.17) |
| TAU versus PPRS × prior SA | 3.95 (4.15) | 0.14 (0.14) | 0.98 (1.09) | 0.16 (0.18) |
| Perceived Present Control Unconditional Model | ||||
| Unconditional model | 22.97 (0.40)*** | 5.08 (0.45)*** | 0.39 (0.10)*** | 0.35 (0.09)*** |
| Variance | 20.47 (3.40)*** | 1.0 | 1.27 (0.31)*** | 1.0 |
| Perceived Present Control Conditional Main Effects Model | ||||
| PIRI versus PPRS | 0.18 (0.94) | 0.02 (0.10) | 0.21 (0.25) | 0.09 (0.11) |
| TAU versus PPRS | −0.07 (0.88) | −0.01 (0.09) | −0.43 (0.25)+ | −0.18 (0.20)+ |
| Age | −0.09 (0.04)* | −0.19 (0.09)* | −0.002 (0.01) | −0.01 (0.10) |
| Prior SA | −0.26 (0.81) | −0.03 (0.09) | −0.14 (0.22) | −0.06 (0.10) |
| Minority status | −2.56 (0.78)*** | −0.28 (0.08)*** | 0.06 (0.21) | 0.03 (0.09) |
| DAFR | 0.19 (0.79) | 0.02 (0.09) | 0.18 (0.22) | 0.08 (0.10) |
| Perceived Present Control Conditional Interaction Model | ||||
| PIRI versus PPRS × prior SA | −1.72 (1.79) | −0.14 (0.15) | 0.64 (0.50) | 0.21 (0.17) |
| TAU versus PPRS × prior SA | −1.80 (1.74) | −0.15 (0.14) | −0.60 (0.51) | −0.20 (0.17) |
Note. N = 233. B = unstandardized estimate; SE = standard error; β = standardized estimate; PTSD = posttraumatic stress disorder; prior SA = prior sexual assault (1 = prior SA, 0 = no prior SA); PIRI = Pleasant Imagery and Relaxation Instruction (coded as 1); PPRS = Prevention of Post-Rape Stress (coded as 0); TAU = Treatment as Usual (coded as 1); DAFR = Drug- or Alcohol-Facilitated Rape; minority status (minority coded as 1, non-minority coded as 0). All conditional interaction models included the main effects in addition to the interaction terms; estimates for the main effects available upon request.
p <.10.
p < .05.
p < .01.
p < .001.
The fit of the unconditional, χ2 (df = 1) = .69, p = .004; CFI =1.00; RMSEA = .001; SRMR = .01, conditional main effect, χ2 (df = 16) = 25.01, p = .07; CFI =.95; RMSEA = .05; SRMR = .04, and conditional interaction, χ2 (df = 20) = 27.73, p = .12; CFI =.96; RMSEA = .04; SRMR = .04, models for perceived present control were good and suggested that on average, perceived present control increased over follow-up. Older and minority women had lower levels of perceived present control at intercept and there was a trend for women in the TAU condition to show more of a decline in perceived present control over follow-up relative to PPRS. Intervention conditions did not interact with prior SA to predict perceived present control slope or intercept.
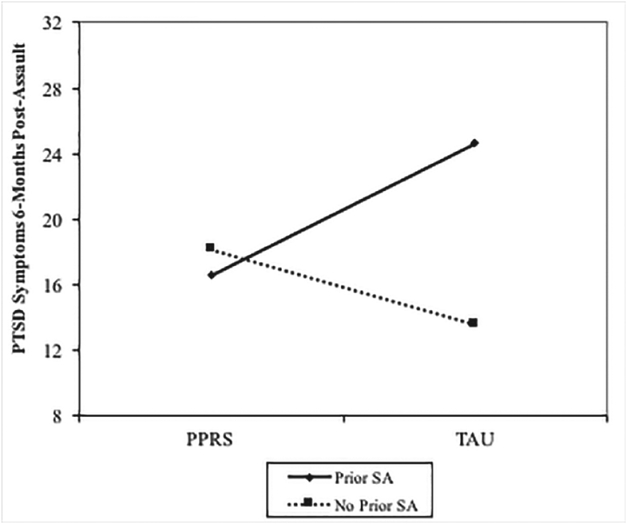
Interaction models for PTSD and perceived present control at each time point are presented in Table 3. There were no main effect differences on PTSD or perceived present control based on condition at any time point. For PTSD symptom frequency at 6 months post-SA, the TAU versus PPRS comparison interacted with SA history, B = 9.45, SE = 5.51, p = .048. Among women with prior SA, those in the PPRS condition had less severe PTSD symptoms than those in the TAU condition 6-months post-SA, B = 10.79, SE = 3.98, p = .009 (see Figure 2). In contrast, there was no difference in PTSD symptom severity in the PPRS condition compared to the TAU condition among women with no prior SA, B = −3.70, SE = 4.29, p = .393.
Table 3.
Predictors of PTSD Symptom Frequency and Perceived Present Control.
| Total PTSD symptoms | 1.5 months post assault | 3 months post assault | 6 months post assault | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B (SE) | CR | 95% CI | B (SE) | CR | 95% CI | B (SE) | CR | 95% CI | |
| R2 = .11; f2 = .12 | R2 = .16; f2 = .19 | R2 = .12; f2 = .14 | |||||||
| Prior SA | 2.43 (2.76) | 0.88 | −2.12 to 6.97 | 3.70 (3.09) | 1.20 | −1.38 to 8.78 | 0.76 (4.15) | 0.18 | −6.06 to 7.58 |
| PIRI versus PPRS | −2.31 (2.99) | −0.77 | −7.24 to 2.61 | −1.82 (3.88) | −0.47 | −8.20 to 4.55 | 2.10 (4.31) | 0.49 | −4.99 to 9.18 |
| TAU versus PPRS | −0.77 (3.19) | −0.24 | −6.02 to 4.47 | −4.92 (3.10) | −1.59 | −10.03 to 0.18 | −1.47 (4.14) | −0.35 | −8.28 to 5.35 |
| Age | 0.15 (0.10) | 1.58 | −0.01 to 0.31 | 0.12 (0.10) | 1.20 | −0.05 to 0.29 | 0.24 (0.11) | 2.18 | 0.06 to 0.43* |
| Minority status | 4.28 (1.75) | 2.45 | 1.40 to 7.15* | 4.03 (1.98) | 2.03 | 0.77 to 7.28 | 2.88 (2.07) | 1.39 | −0.54 to 6.29 |
| DAFR | 1.09 (1.80) | 0.61 | −1.87 to 4.05 | −1.80 (1.99) | −0.91 | −5.07 to 1.46 | −1.22 (2.28) | −0.53 | −4.96 to 2.53 |
| PIRI versus PPRS × prior SA | 1.20 (4.11) | 0.29 | −5.56 to 7.96 | 0.92 (4.94) | 0.19 | −7.21 to 9.05 | −0.11 (5.55) | −0.02 | −9.24 to 9.01 |
| TAU versus PPRS × prior SA | 3.88 (4.23) | 0.92 | −3.07 to 10.84 | 7.80 (4.45) | 1.75 | 0.48 to 15.12 | 9.45 (5.51) | 1.96 | 0.38 to 18.52* |
| Perceived present control | R2 = .10; f2 = .11 | R2 = .12; f2 = .14 | R2 = .19; f2 = .23 | ||||||
| Prior SA | 0.60 (1.12) | 0.53 | −1.60 to 2.80 | 1.87 (1.55) | 1.20 | −1.17 to 4.91 | 0.46 (1.86) | 0.24 | −3.21 to 4.09 |
| PIRI versus PPRS | 0.96 (1.36) | 0.70 | −1.71 to 3.62 | 2.81 (1.91) | 1.47 | −0.94 to 6.55 | 0.40 (1.93) | 0.21 | −3.38 to 4.19 |
| TAU versus PPRS | 0.71 (1.33) | 0.53 | −1.90 to 3.32 | 3.11 (1.58) | 1.97 | 0.02 to 6.20* | 1.06 (1.97) | 0.54 | −2.81 to 4.92 |
| Age | −0.09 (0.04) | −2.16 | −0.18 to −0.01* | −0.04 (0.05) | −0.78 | −0.14 to 0.06 | −0.08 (0.06) | −1.40 | −0.19 to 0.03 |
| Minority status | −2.48 (0.78) | −3.20 | −4.00 to −0.96* | −2.61 (0.94) | −2.77 | −4.46 to −0.76* | −2.06 (0.94) | −2.19 | −3.91 to −0.23* |
| DAFR | 0.32 (0.80) | 0.40 | −1.24 to 1.88 | 0.98 (0.93) | 1.06 | −0.84 to 2.79 | 0.97 (1.00) | 0.97 | −0.99 to 2.92 |
| PIRI versus PPRS × prior SA | −1.34 (1.82) | −0.74 | −4.89 to 2.22 | −2.23 (2.40) | −0.93 | −6.93 to 2.46 | 0.84 (2.39) | 0.35 | −3.83 to 5.52 |
| TAU versus PPRS × prior SA | −1.39 (1.77) | −0.79 | −4.85 to 2.07 | −4.81 (2.12) | −2.27 | −8.96 to −0.65* | −5.47 (2.44) | −2.24 | −10.23 to −0.67* |
Note. N = 233. CR = critical ratio; CI = confidence interval; PTSD = posttraumatic stress disorder; prior SA = prior sexual assault (1 = prior SA, 0 = no prior SA); PIRI = Pleasant Imagery and Relaxation Instruction (coded as 1); PPRS = Prevention of Post-Rape Stress (coded as 0); TAU = Treatment as Usual (coded as 1); DAFR = Drug- or Alcohol-Facilitated Rape; minority status (minority coded as 1, non-minority coded as 0).
p < .05.
p < .01.
p < .001.
Figure 2. Interaction between treatment condition and prior SA history on PTSD symptoms.
Note. The difference between PPRS (Prevention of Post-Rape Stress) and TAU (treatment as usual) is only significantly different for those with a prior SA (sexual assault) history (t = 8.07, p = .02) and not for those with no prior SA (t = −2.99, p = .48).
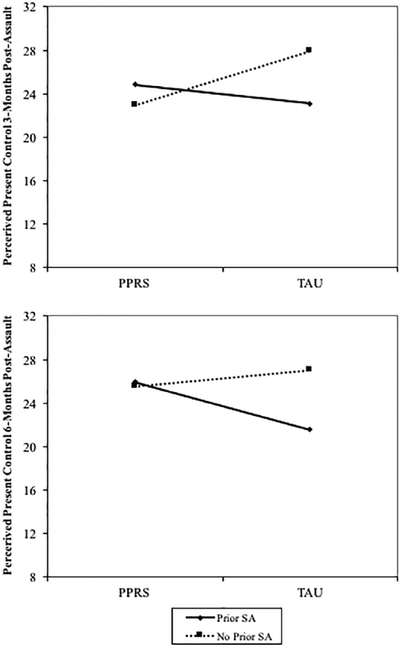
For perceived present control, interactions between the TAU versus PPRS comparison and prior SA were significant at 3 months, B = −4.81, SE = 2.12, p = .023 and 6 months post-SA, B = −5.45, SE = 2.44, p = .025 (see Figure 3). At 3 months post-SA, the difference between the TAU and PPRS conditions was not significantly different for women with prior SA, B = −1.70, SE =1.45, p = .242; those with no prior SA reported more perceived present control in the TAU than in the PPRS condition, B = 3.11, SE = 1.58, p = .049. At 6 months post-SA, among women with prior SA, those in the PPRS condition had higher perceived present control than those in the TAU condition, B = −4.40, SE = 1.43, p = .002. There was no difference in perceived present control in the PPRS condition compared to the TAU condition among women with no prior SA, B = 1.06, SE = 1.97, p = .592. The PIRI versus PPRS comparison did not interact with SA history to predict either outcome at any time point. Finally, there were no significant interactions between the TAU-PIRI comparison and prior SA on either outcome.
Figure 3. Interactions between treatment condition and prior SA history on perceived present control.
Note. At 3 months, the difference between Prevention of Post-Rape Stress (PPRS) and treatment as usual (TAU) is not different for those with a prior sexual assault (SA) history (t = −1.70, p = .24) but is significantly different for those without prior SA (t = 3.11, p < .05). At 6 months, the difference between PPRS and TAU is only significantly different for those with a prior SA history (t = −4.40, p < .01) and not for those with no prior SA (t = 1.05, p = .59).
Discussion
These findings add to the emerging literature aimed at preventing PTSD by assessing the effects of a scalable technology-based intervention on PTSD and perceived present control, a coping-related variable strongly associated with better outcomes among women who have experienced SA (e.g., Frazier, 2003; Ullman & Peter-Hagene, 2014). This study examined a difficult-to-reach sample of participants who experienced a recent SA. Although we did not reach our recruitment goals, the findings partially supported our hypotheses. There was no support for main effects of the PPRS video on PTSD symptoms compared to TAU. There were also no significant differences between PPRS and PIRI; therefore, the PPRS video does not appear to be more effective than a relaxation control condition. However, among women with prior SA, those receiving PPRS had less frequent PTSD symptoms and higher perceived present control 6-months post-SA compared to those receiving TAU. These findings had a medium effect size (Cohen, 1988), suggesting there may be some clinically significant differences in PTSD symptoms as well as perceived present control among those with prior SA who also received the video. These findings are important in that the development of PTSD symptoms can be long-standing across one’s life and associated with significant morbidity (Johnson, Zlotnick, & Perez, 2008). Therefore, mitigating the development of PTSD symptoms among those with prior SA can prevent the onset of chronic symptoms that are associated with disability and impairment. This finding is consistent with previous literature suggesting that technology-based interventions are particularly useful for women with more severe SA histories (Gilmore, Lewis, & George, 2015; Resnick, Acierno, Waldrop, et al., 2007). It is possible that women with prior SA may attend to, and learn from, coping skills presented in the PPRS video more than those without such histories because the relevance of this material is more apparent. More work is needed to understand why the PPRS is effective for women with prior SA. Among those with prior SA, the PPRS may be a low-resource and expedient method to reduce PTSD symptoms and increase perceived present control. There were no significant findings regarding PTSD symptoms and perceived present control over time based on condition. There were significant changes over time based on prior SA, age, and race/ethnicity. Taken together, these findings suggest that video-based interventions can be effective within the ED among recently victimized individuals at certain time points post-SA, especially those with prior SA.
Findings indicating reduced PTSD symptom frequency only among women with prior SA were partially consistent with prior findings (Resnick, Acierno, Waldrop, et al., 2007). Results of that study indicated less frequent PTSD symptoms among those with prior SA at 1.5-months post-SA rather than at 6-months post-SA as reported in this study. Thus, while the time frame differed, the previous study (Resnick, Acierno, Waldrop, et al., 2007) indicated that the PPRS was effective at mitigating the development of PTSD symptoms among women with prior SA.
The findings for perceived present control differ by follow-up period. Three months post-SA, there was a main effect for treatment condition, such that those in the TAU reported more perceived present control compared to those in the PPRS condition. Among those with no prior SA, women reported more perceived present control in the TAU than the PPRS condition. This finding was not anticipated, as it would be expected that providing the PPRS would have either no effect or a positive effect on perceived present control for women who experienced SA. Although only speculative, it is possible that individuals who have not experienced a prior SA believe initially that they have the skills to get through the aftermath of SA on their own. Therefore, it is possible that they may have disregarded the information in the video at first, but if they were still experiencing PTSD symptoms 3 months after the SA, they may have become disheartened and realized they may need to use skills to cope with the SA even 3 months later. This study was not adequately powered to examine a three-way interaction between PTSD, treatment condition, and prior SA history on perceived present control; however, it may be that the maintenance of PTSD symptoms may impact one’s perceived present control at each time point. Although surprising, the 3-month finding was consistent with previous findings (Resnick, Acierno, Waldrop, et al., 2007) where women with no prior SA had relatively higher frequency of PTSD symptoms in the PPRS condition, though not significant, compared to TAU 1.5-months post-SA. This pattern was not maintained at 6-months post-SA. The overall pattern suggests prior SA is associated with more frequent PTSD symptoms and lower perceived present control but the PPRS video mitigated the effect of prior SA, making those with prior SA have similar symptom patterns to those with no prior SA. Despite prior SA experiences, and consistent with previously reported findings (Resnick, Acierno, Waldrop et al., 2007), the average PTSD symptom score at 6-month follow-up was below the suggested clinical cut-off score. Therefore, although many individuals are doing well with regard to PTSD symptom frequency 6-months post-SA, the PPRS can be helpful in mitigating the development of symptoms among those with a prior SA history.
Finally, the majority of the sample identified as a racial/ethnic minority (59.7%) and this group was at particular risk for more severe PTSD symptoms as well as less perceived present control. In relation to PTSD symptoms, women who identified as racial/ethnic minorities had more severe PTSD symptoms at the 1.5-month follow-up period compared to their White counterparts, although this difference was not maintained at the 3- or 6-month follow-ups. In relation to perceived present control, women who identified as racial/ethnic minorities had less perceived present control at each time point than their White counterparts. More work is needed to understand why this difference was found. Previous work on perceived present control has largely focused on college samples that are predominately White (e.g., Coudray, Palmer, & Frazier, 2019; Nguyen-Feng, Baker, Merians, & Frazier, 2017); therefore, it is possible that there are pre-SA racial/ethnic differences in this construct that have not yet been established in the literature. Certainly, racial/ethnic minorities experience disparities in access to health care (for a review, see Fiscella & Sanders, 2016) in addition to experiences of discrimination which may contribute to perceived present control. Future work is needed to elucidate the unique factors contributing to the maintenance of post-SA mental health symptoms among racial/ethnic minorities and ensure that prevention programs tailor to these unique factors.
Strengths, Limitations, and Future Directions
Strengths of this study include accessing a difficult-to-reach population immediately post-SA and allowing ED providers to implement an intervention at the time of the SAMFE. A notable strength was an active control comparison as well as the examination of perceived present control rather than mental health symptoms alone. Although the PPRS did not differ from PIRI, the PPRS differed significantly from TAU among those with prior SA histories 6-months after SA in regard to PTSD and perceived present control and the PIRI did not differ from TAU. There were several limitations to the study. Participants were provided with different information based on their assigned condition. Most (82%) participants received a brief version of the videos post-exam compared to the full video before the exam. It is possible that there were unforeseen, and therefore, not assessed, differences between video types in outcomes. Future work should include a thorough pilot stage that would allow for clinical flow problems to be detected prior to beginning the randomized clinical trial and would allow for one version of the video rather than needing to change due to clinical flow disruptions in the middle of the trial. Prior SA and DAFR were assessed using one-item measures due to time limitations. Future research should include the same instructions for each video, test the same version of the videos for every participant, and include a more comprehensive assessment of prior SA and DAFR. Furthermore, we did not assess for sexual and gender minority status and we excluded individuals who did not speak English. Lesbian, gay, bisexual, transgender, queer, intersex and asexual and/or ally (LGBTQIA+) communities as well as those who do not speak English may be at particular risk for SA, have less access to medical care, and experience discrimination at higher levels than other populations, and therefore, it would be important for future work to test the effectiveness of prevention efforts among these populations. Finally, the sample size was small and many participants were lost to follow-up. The study had to discontinue prior to recruiting the entire sample needed for adequate power (projected N = 566) due to years spent recruiting; therefore, the sample may not be adequately powered to detect all significant findings. Future work should include national recruitment to ensure adequate sample size for this specialized, at-risk population. Many of the participants that were enrolled in the study were lost to follow-up, and although the analyses accounted for these individuals, it is possible that those who were lost to follow-up differed in severity than those who completed all follow-up assessments.
Implications for Practice and Policy
Currently, the standard practice of an SAMFE does provide individuals who recently experienced an SA with preventive medications for sexually transmitted infections, but no prevention is provided for post-SA mental health sequelae. The findings from this study, combined with the extant literature on post-SA mental health, suggest a need for prevention to be embedded within the SAMFE. However, there are limited resources to accomplish this task. This study provides an examination of the PPRS as a preventive tool to reduce post-SA PTSD symptoms and increase perceived control for those with a prior SA history. It is unclear if prior histories of traumatic event exposure including those with interpersonal violence histories would similarly benefit from the PPRS. Although the PPRS was only effective among those with a prior SA, this group may have elevated risk for mental health sequelae, so this finding is promising and suggests that prevention given during the SAMFE is possible and effective for some subgroups. Nonetheless, more work is needed to determine what universal prevention strategy can be utilized for individuals who recently experienced SA.
Conclusion
The PPRS did not significantly alter symptom trajectory post-SA, and there were no main effects on PTSD or perceived present control. However, the PPRS was effective at mitigating the development of PTSD symptoms and increasing perceived present control 6-months post-SA among women with prior SA. Therefore, universal use of the PPRS may not be warranted; however, these initial findings are promising. Future work should determine what components would be beneficial to add to PPRS to increase its effectiveness for individuals with no prior SA. This research adds to the literature using technology-based interventions in ED settings, which can have broader implications for individuals receiving care within an ED setting.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Data collection and manuscript preparation were supported by grants from the National Institute on Drug Abuse (NIDA; R01DA023099 to Dr. Resnick and K23DA042935 to Dr. Gilmore).
Author Biographies
Amanda K. Gilmore, PhD, is an assistant professor in the Department of Health Policy & Behavioral Sciences and the Mark Chaffin Center of Healthy Development in the School of Public Health at Georgia State University. Her research focuses on prevention of alcohol use and sexual assault, as well as secondary prevention of substance use and mental health symptoms after sexual assault.
Kate Walsh, PhD, is an assistant professor (tenure-track) at Ferkauf Graduate School of Psychology at Yeshiva University. She is interested in the prevention of sexual assault and the treatment of common sequelae of sexual assault.
Patricia Frazier, PhD, is a distinguished McKnight University professor in the Department of Psychology at the University of Minnesota. Her research interests include using technology to develop innovative interventions for trauma survivors.
Liza Meredith, PhD, is an assistant contract professor at University of Minnesota. She teaches and coordinates Introduction of Psychology at the university.
Linda E. Ledray, PhD, founded one of the first Sexual Assault Nurse Examiner (SANE) programs at Hennepin County Medical Center in Minneapolis, MN, in 1977 and she was the program director until 2009. This model was based on both process and outcome research and is a model for hundreds of programs throughout the US and a number of foreign countries. Dr. Ledray is a retired Army Colonel and continues to work as a consultant for RTI in Raleigh, NC, on the Sexual Assault Kit Initiative funded by BJA.
Joanne L. Davis, PhD, is a professor of Psychology at The University of Tulsa, Director of Clinical Training, Director of the Trauma Research: Assessment, Prevention, and Treatment Center, and Co-Director of The University of Tulsa Institute of Trauma, Adversity, and Injustice. Dr. Davis’ research focuses on the treatment of nightmares and sleep problems in trauma-exposed individuals as well as on prevention efforts to impact the prevalence and impact of interpersonal trauma. She is the developer of a cognitive behavioral treatment targeting nightmares and sleep problems, Exposure, Relaxation, and Rescripting Therapy, and has conducted research to evaluate its efficacy for the past 18 years. She is a trainer for the Army Medical Education Division for treatment approaches for insomnia and nightmares.
Ron Acierno, PhD, is a professor and vice chair of Veterans Affairs in the Department of Psychiatry and Behavioral Sciences. He also serves as the Executive Director of the UTHealth Trauma and Resilience Center (TRC). Dr. Acierno has two related but distinct research foci: epidemiological studies of elder mistreatment and treatment outcome studies, focusing on victims of trauma, disaster, combat or loss. He has served as Principal Investigator on grants from NIA, NIMH, NIJ, the Department of Defense, The Department of Veterans Affairs, the South Carolina Department of Public Safety, the Archstone Foundation, and the Retirement Research Foundation. Thus, Dr. Acierno mixes epidemiological research with treatment outcome research, and keeps close to the clinical world as a clinician-administrator for treatment programs serving both civilian and military traumatized populations. Dr. Acierno has also been recognized for his personal investment in the mentoring of others, with over 20 current faculty researchers across the country having worked alongside him in his lab over the years. Dr. Acierno has over 150 published articles and 30 book chapters, and has served on the Editorial Boards of several journals.
Ken Ruggiero, PhD, is professor and SmartState endowed chair at the Medical University of South Carolina, where he serves as Director of the Technology Applications Center for Healthful Lifestyles and the Trauma Resilience and Recovery Program. His work centers on improving access and quality of mental health care to vulnerable and underserved populations, particularly children and adults who have been affected by traumatic events such as disasters, serious injury, child abuse, and occupational incidents. This includes research on self-help apps for disaster victims and technology-enhanced treatments for survivors of traumatic injury. He also works with community agencies to help mental health providers improve quality of care with children.
Dean G. Kilpatrick’s, PhD, primary research interests include measuring the prevalence of rape, other violent crimes and other types of potentially traumatic events, as well as assessing PTSD and other mental health impacts of such events. Dr. Kilpatrick and colleagues have conducted numerous studies on these topics, using national household probability samples of adults and adolescents. This research has been funded by the Centers for Disease Control and Prevention, NIMH, NIDA, NICHD, National Institute of Justice, and the VA. He also is Director of a large recently established National Mass Violence and Victimization Center that is designed to study and improve the nation’s capacity to respond to victims and survivors of mass violence incidents.
Anna E. Jaffe, PhD, is a postdoctoral fellow in the Department of Psychiatry and Behavioral Sciences at the University of Washington. Her research focuses broadly on the occurrence and effects of interpersonal violence. She is particularly interested in the prevention and treatment of sexual assault, recovery following alcohol-involved sexual assault, and associations between PTSD and alcohol use problems.
Heidi S. Resnick, PhD, was a professor emerita at the National Crime Victims Research and Treatment Center within the Department of Psychiatry at the Medical University of South Carolina. Dr. Resnick led or served as a co-investigator on federally funded research investigating prevalence and risk factors for PTSD and other adaptations following exposure to traumatic events, with an emphasis on sexual assault. She and colleagues conducted research to develop and evaluate secondary prevention approaches that might reduce PTSD or other difficulties following exposure to traumatic events. She was an exemplary mentor and researcher and her work moved the field forward by addressing the acute needs of individuals after a sexual assault.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Initial analyses revealed that changes in perceived present control did not mediate changes in PTSD symptoms; therefore, PTSD and perceived present control were both examined as outcomes.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Bentler PM (1995). EQS structural equations program manual. Encino, CA: Multivariate Software. [Google Scholar]
- Browne MW, & Cudeck R (1993). Alternative ways of assessing model fit. In Bollen KA & Long JS (Eds.), Testing structural equation models (pp. 136–162). Newbury Park, CA: SAGE. [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Erlbaum. [Google Scholar]
- Coudray C, Palmer R, & Frazier P (2019). Moderators of the efficacy of a web-based stress management intervention for college students. Journal of Counseling Psychology. 10.1037/cou0000340 [DOI] [PubMed] [Google Scholar]
- Darnell D, Peterson R, Berliner L, Stewart T, Russo J, Whiteside L, & Zatzick D (2015). Factors associated with follow-up attendance among rape victims in acute medical care. Psychiatry, 78, 89–101. doi: 10.1080/00332747.2015.1015901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dworkin ER, Menon SV, Bystrynski J, & Allen NE (2017). Sexual assault victimization and psychopathology: A review and meta-analysis. Clinical Psychology Review, 56, 65–81. doi: 10.1016/j.cpr.2017.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiscella K, & Sanders MR (2016). Racial and ethnic disparities in the quality of health care. Annual Review of Public Health, 37, 375–394. [DOI] [PubMed] [Google Scholar]
- Foa EB, Cashman L, Jaycox L, & Perry K (1997). The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment, 9, 445–451. doi: 10.1037/1040-3590.9.4.445 [DOI] [Google Scholar]
- Foa EB, Hembree EA, & Rothbaum BO (2007). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences. New York, NY: Oxford University Press. [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, & Rothbaum BO (1993). Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress, 6, 459–473. doi: 10.1037/1040-3590.9.4.445 [DOI] [Google Scholar]
- Foa EB, Zoellner LA, & Feeny NC (2006). An evaluation of three brief programs for facilitating recovery after assault. Journal of Traumatic Stress, 19, 29–43. doi: 10.1002/jts.20096 [DOI] [PubMed] [Google Scholar]
- Frazier P (2003). Perceived control and distress following sexual assault: A longitudinal test of a new model. Journal of Personality and Social Psychology, 84, 1257–1269. doi: 10.1037/0022-3514.84.6.1257 [DOI] [PubMed] [Google Scholar]
- Frazier P, Anders S, Shallcross S, Keenan N, Perera S, Howard K, & Hintz S (2012). Further development of the temporal model of control. Journal of Counseling Psychology, 59, 623–630. doi: 10.1037/a0029702 [DOI] [PubMed] [Google Scholar]
- Frazier P, Berman M, & Steward J (2001). Perceived control and posttraumatic stress: A temporal model. Applied and Preventive Psychology, 10, 207–223. doi: 10.1016/S0962-1849(01)80015-9 [DOI] [Google Scholar]
- Frazier P, Keenan N, Anders S, Perera S, Shallcross S, & Hintz S (2011). Perceived past, present, and future control and adjustment to stressful life events. Journal of Personality and Social Psychology, 100, 749–765. doi: 10.1037/a0022405 [DOI] [PubMed] [Google Scholar]
- Gilmore AK, Lewis MA, & George WH (2015). A randomized controlled trial targeting alcohol use and sexual assault risk among college women at high risk for victimization. Behaviour Research and Therapy, 74, 38–49. doi: 10.1016/j.brat.2015.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmore AK, Walsh K, Frazier P, Ledray L, Acierno R, Ruggiero KJ, Kilpatrick DG, & Resnick HS (2019). Prescription opioid misuse after a recent sexual assault: A randomized clinical trial of a video intervention. American Journal on Addictions, 28, 376–381. DOI: 10.1111/ajad.12922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hintz S, Frazier PA, & Meredith L (2015). Evaluating an online stress management intervention for college students. Journal of Counseling Psychology, 62, 137–147. doi: 10.1037/cou0000014 [DOI] [PubMed] [Google Scholar]
- Johnson DM, Zlotnick C, & Perez S (2008). The relative contribution of abuse severity and PTSD severity on the psychiatric and social morbidity of battered women in shelters. Behavior Therapy, 39, 232–241. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Ruggiero KJ, Conoscenti LM, & McCauley J (2007). Drug-facilitated, incapacitated, and forcible rape: A national study. Charleston: National Crime Victims Research & Treatment Center, Medical University of South Carolina. [Google Scholar]
- Manzoni GM, Pagnini F, Castelnuovo G, & Molinari E (2008). Relaxation training for anxiety: A ten-years systematic review with meta-analysis. BMC Psychiatry, 8, 41–53. doi: 10.11.86/1471-244X-8-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller KE, Cranston CC, Davis JL, Newman E, & Resnick H (2015). Psychological outcomes after a sexual assault video intervention: A randomized trial. Journal of Forensic Nursing, 11, 129–136. doi: 10.1097/jfn.0000000000000080 [DOI] [PubMed] [Google Scholar]
- Nguyen-Feng VN, Baker MR, Merians AN, & Frazier PA (2017). Sexual victimization, childhood emotional abuse, and distress: Daily coping and perceived control as mediators. Journal of Counseling Psychology, 64, 672–683. [DOI] [PubMed] [Google Scholar]
- Nguyen-Feng VN, Frazier PA, Greer CS, Meredith L, Howard KG, & Paulsen JA (2016). Testing the efficacy of three web-based interventions for reducing distress among interpersonal violence survivors. Translational Issues in Psychological Science, 4, 439–448. doi: 10.1037/tps0000099 [DOI] [Google Scholar]
- Office on Violence Against Women. (2013). National protocol for sexual assault medical forensic examinations. Washington, DC: U.S. Department of Justice. [Google Scholar]
- Patel A, Roston A, Tilmon S, Stern L, Roston A, Patel D, & Keith L (2013). Assessing the extent of provision of comprehensive medical care management for female sexual assault patients in US hospital emergency departments. International Journal of Gynecology & Obstetrics, 123, 24–28. [DOI] [PubMed] [Google Scholar]
- Peter-Hagene LC, & Ullman SE (2014). Social reactions to sexual assault disclosure and problem drinking: Mediating effects of perceived control and PTSD. Journal of Interpersonal Violence, 29, 1418–1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Monson CM, & Chard KM (2016). Cognitive processing therapy for PTSD: A comprehensive manual. New York, NY: Guilford Press. [Google Scholar]
- Resnick HS, Acierno R, Amstadter AB, Self-Brown S, & Kilpatrick DG (2007). An acute post-sexual assault intervention to prevent drug abuse: Updated findings. Addictive Behaviors, 32, 2032–2045. doi: 10.1016/j.addbeh.2007.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick HS, Acierno R, Waldrop AE, King L, King D, Danielson C, … Kilpatrick D (2007). Randomized controlled evaluation of an early intervention to prevent post-rape psychopathology. Behaviour Research and Therapy, 45, 2432–2447. doi: 10.1037/e322352004-162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbaum BO, Foa EB, Riggs DS, Murdock T, & Walsh W (1992). A prospective examination of post-traumatic stress disorder in rape victims. Journal of Traumatic Stress, 5, 455–475. [Google Scholar]
- Rothbaum BO, Kearns MC, Price M, Malcoun E, Davis M, Ressler KJ, … Houry D (2012). Early intervention may prevent the development of posttraumatic stress disorder: A randomized pilot civilian study with modified prolonged exposure. Biological Psychiatry, 72, 957–963. doi: 10.1016/j.bio-psych.2012.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith SG, Zhang X, Basile KC, Merrick MT, Wang J, Kresnow M, & Chen J (2018). The National Intimate Partner and Sexual Violence Survey (NISVS): 2015 Data brief - updated release. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. Retrieved from: https://www.cdc.gov/violenceprevention/pdf/2015data-brief508.pdf [Google Scholar]
- Ullman SE, & Najdowski CJ (2009). Correlates of serious suicidal ideation and attempts in female adult sexual assault survivors. Suicide and Life-Threatening Behavior, 39, 47–57. doi: 10.1521/suli.2009.39.1.47 [DOI] [PubMed] [Google Scholar]
- Ullman SE, & Peter-Hagene L (2014). Social reactions to sexual assault disclosure, coping, perceived control, and PTSD symptoms in sexual assault victims. Journal of Community Psychology, 42, 495–508. doi: 10.1002/jcop.21624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh RM, & Bruce SE (2011). The relationships between perceived levels of control, psychological distress, and legal system variables in a sample of sexual assault survivors. Violence Against Women, 17, 603–618. doi: 10.1177/1077801211407427 [DOI] [PubMed] [Google Scholar]
- Walsh K, Gilmore AK, Frazier P, Ledray L, Acierno R, Ruggiero KJ, Kilpatrick DG, & Resnick HS (2017). A randomized clinical trial examining the effect of video-based prevention of alcohol and marijuana use among recent sexual assault victims. Alcoholism: Clinical and Experimental Research, 41, 2163–2172. DOI: 10.1111/acer.13505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh K, Gilmore A, Schumacher J, Coffey S, Frazier P, Ledray L, Acierno R, Ruggiero K, Kilpatrick DG, & Resnick HS (2019). Post-sexual assault cigarette smoking: Findings from a randomized clinical trial of a video-based intervention. Addictive Behaviors, 100, 106–121. doi: 10.1016/j.addbeh.2019.106121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinzow HM, Resnick HS, McCauley JL, Amstadter AB, Ruggiero KJ, & Kilpatrick DG (2010). The role of rape tactics in risk for posttraumatic stress disorder and major depression: Results from a national sample of college women. Depression and Anxiety, 27, 708–715. doi: 10.1002/da.20719 [DOI] [PubMed] [Google Scholar]