ABSTRACT
Scorpionism has a high incidence rate in Brazil. It is considered a serious public health problem mainly in tropical and subtropical regions around the world. The number of scorpion accidents have increased over the years and the highest frequencies have been reported mainly in the Brazilian Northeast region. Therefore, in this study we report a retrospective clinical and epidemiological analysis of scorpion stings from 2007 to 2017 in Alagoas State, Northeast Brazil, at a referral hospital for assistance and treatment of accidents by venomous animals. During the analyzed period, the referral hospital treated 27,988 cases, and an increase in the number of cases has taken place over the years. The highest frequency of scorpion stings was observed in females, and the age range most affected was from 20 to 29 years old. The most stung body site was the foot, followed by finger, toe or hand. Regarding the severity, most severe cases were reported in children up to 4 years old (69.4%) and 50% of the total cases treated with serotherapy corresponded to patients in this age range. Interestingly, it was also found that the occurrence of systemic manifestations and the severity of the cases were significantly associated with pediatric patients. In this way, this study highlights the scorpionism as an environmental public health problem in Alagoas State, Northeast Brazil, as well as the need to intensify the epidemiological surveillance and educational campaigns to prevent and control scorpion accidents throughout the year.
Keywords: Scorpionism, Scorpion stings, Tropical medicine, Epidemiology
INTRODUCTION
Scorpionism is a serious public health problem reaching high incidence rates and severity mainly in tropical and subtropical regions around the world1,2. In Brazil, scorpionism has a high incidence rate due to the wide distribution of scorpions in all the regions and ecosystems of the country3. The species of the genus Tityus, mainly Tityus serrulatus known as “yellow scorpion” due to its coloring, is considered the most dangerous scorpion and accounts for the highest number of accidents2,4.
Scorpion toxin is composed of a complex mixture of low molecular weight proteins that prolong depolarization of post-ganglionic nerve endings throughout the body, leading to a massive release of neurotransmitters, which trigger the predominance of systemic effects (adrenergic and/or cholinergic)5. Additionally, it is known that the mediators of the inflammatory response and toxicity on the cardiac fibers are involved in the genesis of the pulmonary edema due to the increase of permeability of the capillaries6.
Local pain is present in almost all the cases, with different levels of intensity and irradiation being reported as a pricking or burning sensation. Other local symptoms may be present, such as hyperemia, paresthesia, hyperesthesia, edema, sweating and piloerection2. Furthermore, systemic manifestations may occur and are more frequent in children, usually appearing hours after the accident1.
Scorpion envenomation cases may be classified as mild, moderate, or severe: 1) Mild cases have local signs, such as pain, erythema and local paraesthesia; 2) Moderate cases have sweating, nausea, occasional vomiting, tachycardia, agitation and mild arterial hypertension; 3) In severe cases, besides showing the signs and symptoms of mild and moderate cases, the patient also shows excessive sweating, profuse and incoercible vomiting, prostration, bradycardia, acute pulmonary edema and shock1,7,8. Moreover, complications such as acute pulmonary edema, shock or multiple organ failure are related to mortality7. The severity of clinical manifestations depends on the scorpion features (species, size and amount of venom injected) and victim factors (age, body weight and health status)1. The risk group for a poor prognosis includes mainly children under 5 years of age9 and the clinical outcome may be negatively influenced by the long period from the time of sting to the medical care1.
Epidemiology study of scorpionism in Brazil, from the years 2000 to 2012, reported 482,616 accidents and 728 deaths which shows an increase of 323% in the incidence rate between the first and last year of the study10. Comparing the Brazilian regions, the Northeast had the highest annual incidence and mortality rates. Alagoas State had the highest average annual incidence rate (105.9/100,000 inhabitants)10. However, although it is a serious public health problem, the epidemiology of scorpionism remains underreported1,2 and until the present moment, there is no study analyzing cases of scorpion accidents solely in Alagoas State. Therefore, in this study we report a retrospective analysis of the clinical and epidemiological profile of scorpion stings at the referral Hospital for Assistance and Treatment of accidents by venomous animals in Alagoas, Northeast of Brazil, in the period from 2007 to 2017.
MATERIAL AND METHODS
The Alagoas State is in Northeast Brazil with an area of 27,767 km2and comprises 102 municipalities11,12. These municipalities are grouped into three mesoregions (East, Agreste and Sertao)12. The East mesoregion covers the coast and the forest zone, where the capital Maceio is located11. On the coast and in the forest zone, the annual range of rainfall levels is between 1,300 to 1,600 mm and the maximum annual average air temperature in this region fluctuates between 30 and 31 °C11.
According to the 2010 Brazilian census, the resident population in Alagoas State is 3,120,494 inhabitants, composed of 48.5% men and 51.5% women12. Maceio is the State capital and most populous city, where 29.9% of the population resides12.
In this study, the scorpionism cases were analyzed at a Referral Hospital for the Assistance and Treatment of venomous animals’ accidents in Alagoas State, located in Maceio, and occurred from January 1, 2007 to December 31, 2017. The cases of accidents caused by venomous animals in Brazil are of compulsory notification thus being reported in notification forms and recorded in the SINAN (Sistema de Informacao de Agravos de Notificacao) database. Data were obtained from the TabWin version 3.6b software platform (Ministerio da Saude, Brasilia, DF, Brazil) from SINAN, a public domain database. It was based solely on secondary data, without access to the patients’ nominal data or anything else that could lead to identification; therefore, ensuring the confidentiality of the information collected. All the ethical and legal requirements were followed as specified by Resolution Nº 466/12 from the National Health Council (CNS) of Brazil.
The software Microsoft Excel 2010 was used to register collected data and the demographic information was obtained from the 2010 census of the Brazilian Institute of Geography and Statistics (IBGE)12.
The fields of the SINAN Notification Form (SNF) for accidents with venomous animals are available as Supplementary Material (1.5MB, pdf) . The variables analyzed in this study were: date of accident, gender (female or male), patient’s age, skin color/ethnicity (white, black, Asian, multiracial or indigenous), accident zone (urban, peri-urban or rural), occupation, education level (based on Brazilian law and guidelines), body site of the scorpion sting, severity classification (mild, moderate or severe), local manifestations, systemic manifestations, time between the sting and the medical care, and treatment with serotherapy.
The linear regression analysis13 for the number of cases over the years was performed using R version 3.4.4 (R Core Team, Vienna, Austria). The Student’s t-test (unpaired samples)14 was performed to compare the number of cases between male and female groups. The Analysis of Variance (ANOVA) one-way15 with Tukey’s multiple comparisons test16 was used to establish whether there is a difference among the months by using the Graph-Pad Prism 6.00 (GraphPad Software, La Jolla, CA, USA).
The observed cases of demographic variables were compared to the frequencies from Alagoas’ population, obtained from the 2010 Brazilian census12, by applying the Pearson’s Chi-square Goodness-of-Fit test17 or Binomial Test18 by using the GraphPad Prism version 6 software, as detailed in the Supplementary Material (1.5MB, pdf) .
In order to evaluate the association between the occurrence of systemic clinical manifestations and the most frequent sociodemographic and clinical characteristics, the Pearson’s chi-square test for independence19 was performed using the IBM SPSS Statistics for Windows version 23.0 (IBM Corp., Armond, NY, USA). Some variables were not included because they did not meet the test assumption that no more than 20% of the expected counts are less than 5 and all individual expected counts are 1 or greater20 (Supplementary Material (1.5MB, pdf) ). The level of significance was p < 0.05.
RESULTS
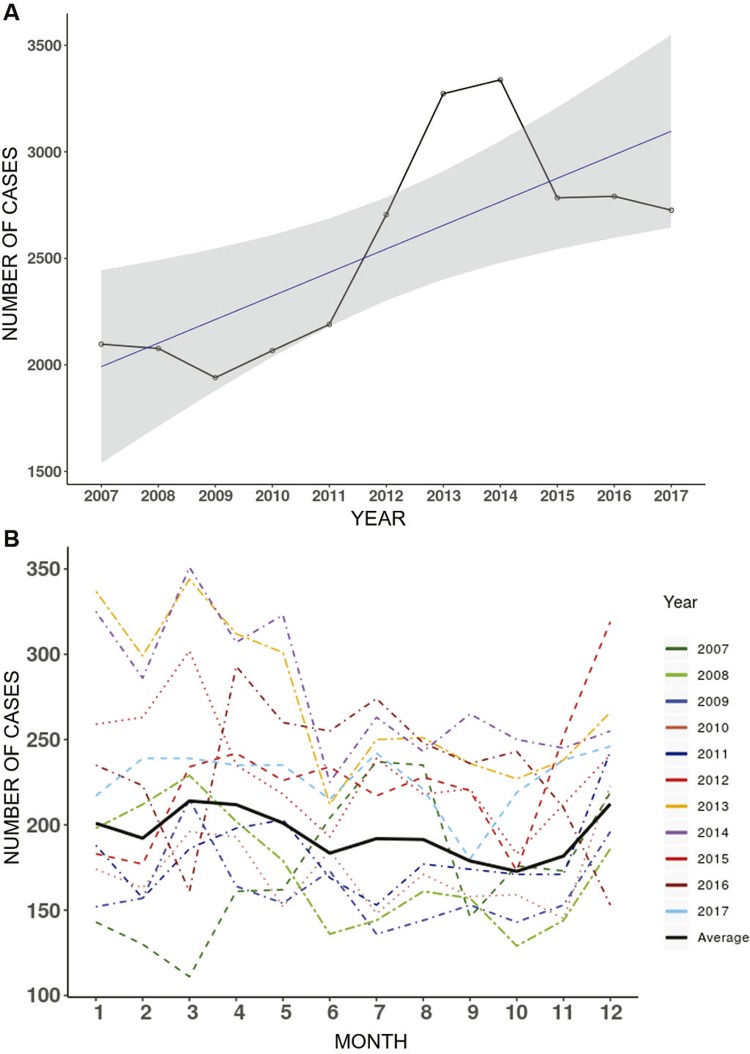
In this retrospective study, from 2007 to 2017, the Referral Hospital for the Assistance and Treatment of Accidents by Venomous Animals in Alagoas State, Brazil, attended 27,988 cases of scorpion stings. During this period, Alagoas State registered 63,762 cases in the SINAN database, with an average incidence rate of 177.4/100,000 inhabitants. Hence, the data collected at a referral hospital represents 44% of the total cases reported in the State. The analysis over the years showed an increase in the number of scorpion sting cases (β = 0.73; p <0.01) (Figure 1A). It is worth mentioning that cases of scorpionism occurred throughout the year and no significant difference among the months was observed in the analyzed period (p = 0.4977) (Figure 1B).
Figure 1. - Temporal distribution of scorpionism cases treated at the referral hospital for the assistance and treatment of accidents by venomous animals in Alagoas State, Northeast of Brazil, from 2007 to 2017. A) Absolute number of scorpionism cases per year (black line) analyzed by a linear regression model (blue line) (β = 0.73; p < 0.01); B) Absolute number of scorpionism cases distributed by month of the accident.
Of the total (n=27,988), the number of cases were higher in females compared to males (Female = 61.8% vs Male = 38.2%) and the average number of cases per year was significant between different genders (male = 972.5 ± 53.6 vs female = 1575.0 ± 97.4; mean ± SEM; p < 0.0001).
The highest frequency of sting cases occurred in the group of 20-29 years old (16.9 %), as shown in Table 1. Regarding the geographic distribution, the urban area presented the highest frequency of cases (n = 26,494; 94.7 %), while the number of cases in the peri-urban and rural areas accounted for less than 2% of all the cases (Table 1). In this study, the multiracial group was the most representative 88.8% of the cases (n = 24,858), followed by the white group (n = 1,426; 5.1%), the black group (n = 1,243; 4.4%), the indigenous group (n = 25; 0.1%) and the Asian group (n = 16; 0.1%) (Table 1). It is important to emphasize that the discrepancy between the distribution of scorpion sting cases considering demographic variables (gender, age range, skin color/ethnicity and accident zone) is significantly different (p < 0.0001) from the population frequencies of Alagoas State (Supplementary Material (1.5MB, pdf) ). Furthermore, considering the education level, the highest number of cases occurred in the group that completed high school (n= 5,859; 20.9%) (Table 1).
Table 1. Distribution of scorpion sting cases at the referral hospital for the assistance and treatment of accidents by venomous animals in Alagoas State, Northeast of Brazil, from 2007 to 2017, according to the gender, age, accident zone, skin color/ethnicity and education level of patients.
| Sociodemographic characteristics | Gender | Total | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Female | Male | ||||||
|
| |||||||
| N | % | N | % | N | % | ||
| Age Range in years | < 1-year-old | 79 | 0.5 | 78 | 0.7 | 157 | 0.6 |
| 1- to 4 | 1,030 | 6.0 | 1,049 | 9.8 | 2,079 | 7.4 | |
| 5- to 9 | 1,216 | 7.0 | 1,183 | 11.1 | 2,399 | 8.6 | |
| 10- to 14 | 1,234 | 7.1 | 1,056 | 9.9 | 2,290 | 8.2 | |
| 15- to 19 | 1,377 | 8.0 | 980 | 9.2 | 2,357 | 8.4 | |
| 20- to 29 | 2,909 | 16.8 | 1,833 | 17.1 | 4,742 | 16.9 | |
| 30- to 39 | 2,682 | 15.5 | 1,474 | 13.8 | 4,156 | 14.8 | |
| 40- to 49 | 2,384 | 13.8 | 1,230 | 11.5 | 3,614 | 12.9 | |
| 50- to 59 | 2,017 | 11.7 | 865 | 8.1 | 2,882 | 10.3 | |
| 60- to 69 | 1,390 | 8.0 | 583 | 5.5 | 1,973 | 7.0 | |
| 70- to 79 | 717 | 4.1 | 269 | 2.5 | 986 | 3.5 | |
| > 80-years | 260 | 1.5 | 93 | 0.9 | 353 | 1.3 | |
|
| |||||||
| Accident zone | Urban | 16,420 | 94.9 | 10,074 | 94.2 | 26,494 | 94.7 |
| Peri-urban | 128 | 0.7 | 98 | 0.9 | 226 | 0.8 | |
| Rural | 138 | 0.8 | 125 | 1.2 | 263 | 0.9 | |
| Ignored/Omitted | 609 | 3.5 | 396 | 3.7 | 1,005 | 3.6 | |
|
| |||||||
| Skin color/Ethnicity | White | 921 | 5.3 | 505 | 4.7 | 1,426 | 5.1 |
| Black | 745 | 4.3 | 498 | 4.7 | 1,243 | 4.4 | |
| Asian | 10 | 0.1 | 6 | 0.1 | 16 | 0.1 | |
| Multiracial | 15,332 | 88.6 | 9,526 | 89.1 | 24,858 | 88.8 | |
| Indigenous | 15 | 0.1 | 10 | 0.1 | 25 | 0.1 | |
| Ignored/Omitted | 272 | 1.6 | 148 | 1.4 | 420 | 1.5 | |
|
| |||||||
| Educational level | Unlettered | 654 | 3.8 | 269 | 2.5 | 923 | 3.3 |
| Uncomplete primary school | 1,555 | 9.0 | 1,079 | 10.1 | 2,634 | 9.4 | |
| Complete primary school | 857 | 5.0 | 484 | 4.5 | 1,341 | 4.8 | |
| Uncomplete middle school | 2,571 | 14.9 | 1,740 | 16.3 | 4,311 | 15.4 | |
| Complete middle school | 1,448 | 8.4 | 858 | 8.0 | 2,306 | 8.2 | |
| Uncomplete high school | 970 | 5.6 | 563 | 5.3 | 1,533 | 5.5 | |
| Complete high school | 3,907 | 22.6 | 1,952 | 18.3 | 5,859 | 20.9 | |
| Uncomplete higher education | 465 | 2.7 | 319 | 3.0 | 784 | 2.8 | |
| Complete higher education | 1,135 | 6.6 | 513 | 4.8 | 1,648 | 5.9 | |
| Not applicable | 2,174 | 12.6 | 1,309 | 12.2 | 3,483 | 12.4 | |
| Ignored/Omitted | 1,559 | 9.0 | 1,607 | 15.0 | 3,166 | 11.3 | |
The professional occupation was recorded in 71.6% (n = 20,042) of the cases in the SNF. Of them, 32% were students, followed by housewives (21.5%) and retirees/pensioners (8.4%). Among the female victims, most of them were housewives (n = 4,263; 32.7%), followed by students (n = 3,425; 26.3%) and retirees/pensioners (n = 1,204; 9.3%). In the male group, most were students (n = 2,554; 36.4%), followed by retirees/pensioners (n = 479, 6.8%) and bricklayers (n = 307; 4.4%). However, it is worth mentioning that only 0.7% of all scorpion sting cases were reported as work-related accidents in the SNF.
Regarding the severity classification, 98.1% (n=27,469) of the cases were classified as mild, while just a few cases were classified as moderate (n=381; 1.4 %) or severe (n=98; 0.4%) (Table 2). Local (LM) and systemic (SM) manifestations were reported in 95.4% (n = 26,707) and 1.9% (n = 525) of the cases, respectively. The most frequent LM was local pain (98.3%) and the most frequent SM was vagal hyperactivity manifestations (60.6%), including nausea and vomiting. We observed an association between the occurrence of SM and the patient’s age (p <0.001), in most cases (61.2%) detected in patients up to 9 years of age. In addition, the association between age and severity was significant (p <0.001) (Supplementary Material (1.5MB, pdf) ), in which 59.3% of the moderate and 83.7% of the severe cases occurred in the group up to 9 years of age (Table 3). It is important to emphasize that in the group of children up to 4 years old, 69.4% were classified as severe cases, and from the total cases treated with serotherapy, 50% of them were in this age group (Table 4).
Table 2. - Distribution of clinical characteristics of scorpion sting cases at the referral hospital for the assistance and treatment of accidents by venomous animals in Alagoas State, Northeast of Brazil, from 2007 to 2017, according to the severity, sting location, local and systemic manifestations and serotherapy.
| Clinical Characteristics | Gender | Total | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Female | Male | ||||||
|
| |||||||
| N | % | N | % | N | % | ||
| Severity | Mild | 16,998 | 98.3 | 10,471 | 97.9 | 27,469 | 98.1 |
| Moderate | 225 | 1.3 | 156 | 1.5 | 381 | 1.4 | |
| Severe | 54 | 0.3 | 44 | 0.4 | 98 | 0.4 | |
| Ignored/omitted | 18 | 0.1 | 22 | 0.2 | 40 | 0.1 | |
|
| |||||||
| Sting location | Head | 151 | 0.9 | 139 | 1.3 | 290 | 1.0 |
| Arm | 491 | 2.8 | 348 | 3.3 | 839 | 3.0 | |
| Forearm | 336 | 1.9 | 289 | 2.7 | 625 | 2.2 | |
| Hand | 1,715 | 9.9 | 1,197 | 11.2 | 2,912 | 10.4 | |
| Finger | 3,105 | 18.0 | 2,079 | 19.4 | 5,184 | 18.5 | |
| Torso | 753 | 4.4 | 598 | 5.6 | 1,351 | 4.8 | |
| Leg | 614 | 3.6 | 440 | 4.1 | 1,054 | 3.8 | |
| Thigh | 490 | 2.8 | 423 | 4.0 | 913 | 3.3 | |
| Foot | 5,373 | 31.1 | 2,717 | 25.4 | 8,090 | 28.9 | |
| Toe | 2,690 | 15.6 | 1,399 | 13.1 | 4,089 | 14.6 | |
| Ignored/Omitted | 1,577 | 9.1 | 1,064 | 10.0 | 2,641 | 9.4 | |
|
| |||||||
| Local manifestations | Yes | 16,592 | 95.9 | 10,115 | 94.6 | 26,707 | 95.4 |
| No | 537 | 3.1 | 446 | 4.2 | 983 | 3.5 | |
| Ignored/omitted | 166 | 1.0 | 132 | 1.2 | 298 | 1.1 | |
|
| |||||||
| Systemic manifestations | Yes | 327 | 1.9 | 198 | 1.9 | 525 | 1.9 |
| No | 16,828 | 97.3 | 10,404 | 97.3 | 27,232 | 97.3 | |
| Ignored/omitted | 140 | 0.8 | 91 | 0.9 | 231 | 0.8 | |
|
| |||||||
| Serotherapy | Yes | 272 | 1.6 | 186 | 1.7 | 458 | 1.6 |
| No | 16,999 | 98.3 | 10,480 | 98.0 | 27,479 | 98.2 | |
| Ignored/omitted | 24 | 0.1 | 27 | 0.3 | 51 | 0.2 | |
Table 3. Distribution of scorpion sting cases according to the severity considering the age range, sting location, the time between the sting and the medical care after the incident and serotherapy reported at the referral hospital for the assistance and treatment of accidents by venomous animals in Alagoas State, Northeast of Brazil, from 2007 to 2017.
| Severity | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Mild | Moderate | Severe | Ignored/omitted | Total | |||||||
|
| |||||||||||
| N | % | N | % | N | % | N | % | N | % | ||
| Age Range (years) | < 1-year-old | 126 | 0.5 | 21 | 5.5 | 10 | 10.2 | 0 | 0.0 | 157 | 0.6 |
| 1- to 4 | 1,877 | 6.8 | 140 | 36.7 | 58 | 59.2 | 4 | 10.0 | 2,079 | 7.4 | |
| 5- to 9 | 2,318 | 8.4 | 65 | 17.1 | 14 | 14.3 | 2 | 5.0 | 2,399 | 8.6 | |
| 10- to 14 | 2,269 | 8.3 | 15 | 3.9 | 0 | 0.0 | 6 | 15.0 | 2,290 | 8.2 | |
| 15- to 19 | 2,341 | 8.5 | 12 | 3.1 | 1 | 1.0 | 3 | 7.5 | 2,357 | 8.4 | |
| 20- to 29 | 4,706 | 17.1 | 27 | 7.1 | 1 | 1.0 | 8 | 20.0 | 4,742 | 16.9 | |
| 30- to 39 | 4,122 | 15.0 | 25 | 6.6 | 4 | 4.1 | 5 | 12.5 | 4,156 | 14.8 | |
| 40- to 49 | 3,587 | 13.1 | 17 | 4.5 | 6 | 6.1 | 4 | 10.0 | 3,614 | 12.9 | |
| 50- to 59 | 2,847 | 10.4 | 29 | 7.6 | 0 | 0.0 | 6 | 15.0 | 2,882 | 10.3 | |
| 60- to 69 | 1,955 | 7.1 | 15 | 3.9 | 1 | 1.0 | 2 | 5.0 | 1,973 | 7.0 | |
| 70- to 79 | 972 | 3.5 | 13 | 3.4 | 1 | 1.0 | 0 | 0.0 | 986 | 3.5 | |
| > 80-years | 349 | 1.3 | 2 | 0.5 | 2 | 2.0 | 0 | 0.0 | 353 | 1.3 | |
|
| |||||||||||
| Sting Location | Head | 282 | 1.0 | 5 | 1.3 | 2 | 2.0 | 1 | 2.5 | 290 | 1.0 |
| Arm | 824 | 3.0 | 11 | 2.9 | 3 | 3.1 | 1 | 2.5 | 839 | 3.0 | |
| Forearm | 615 | 2.2 | 9 | 2.4 | 1 | 1.0 | 0 | 0.0 | 625 | 2.2 | |
| Hand | 2,849 | 10.4 | 46 | 12.1 | 13 | 13.3 | 4 | 10.0 | 2,912 | 10.4 | |
| Finger | 5,106 | 18.6 | 62 | 16.3 | 9 | 9.2 | 7 | 17.5 | 5,184 | 18.5 | |
| Torso | 1,340 | 4.9 | 6 | 1.6 | 3 | 3.1 | 2 | 5.0 | 1,351 | 4.8 | |
| Leg | 1,045 | 3.8 | 6 | 1.6 | 2 | 2.0 | 1 | 2.5 | 1,054 | 3.8 | |
| Thigh | 898 | 3.3 | 13 | 3.4 | 2 | 2.0 | 0 | 0.0 | 913 | 3.3 | |
| Foot | 7,923 | 28.8 | 126 | 33.1 | 27 | 27.6 | 14 | 35.0 | 8,090 | 28.9 | |
| Toe | 4,014 | 14.6 | 59 | 15.5 | 13 | 13.3 | 3 | 7.5 | 4,089 | 14.6 | |
| Ignored/omitted | 2,573 | 9.4 | 38 | 10.0 | 23 | 23.5 | 7 | 17.5 | 2,641 | 9.4 | |
|
| |||||||||||
| Time between the sting and the medical care | < 1 hour | 15,604 | 56.8 | 166 | 43.6 | 39 | 39.8 | 22 | 55.0 | 15,831 | 56.6 |
| 1 to 3 hours | 5,022 | 18.3 | 91 | 23.9 | 33 | 33.7 | 5 | 12.5 | 5,151 | 18.4 | |
| 3 to 6 hours | 1,515 | 5.5 | 32 | 8.4 | 11 | 11.2 | 2 | 5.0 | 1,560 | 5.6 | |
| 6 to 12 hours | 1,130 | 4.1 | 16 | 4.2 | 4 | 4.1 | 2 | 5.0 | 1,152 | 4.1 | |
| 12 to 24 hours | 759 | 2.8 | 23 | 6.0 | 2 | 2.0 | 1 | 2.5 | 785 | 2.8 | |
| > 24 hours | 298 | 1.1 | 11 | 2.9 | 1 | 1.0 | 0 | 0.0 | 310 | 1.1 | |
| Ignored/omitted | 3,141 | 11.4 | 42 | 11.0 | 8 | 8.2 | 8 | 20.0 | 3,199 | 11.4 | |
|
| |||||||||||
| Serotherapy | Yes | 69 | 0.3 | 299 | 78.5 | 88 | 89.8 | 2 | 5.00 | 458 | 1.6 |
| No | 27,365 | 99.6 | 81 | 21.3 | 9 | 9.2 | 24 | 60.0 | 27,479 | 98.2 | |
| Ignored/omitted | 35 | 0.1 | 1 | 0.3 | 1 | 1.0 | 14 | 35.0 | 51 | 0.2 | |
Table 4. - Distribution of serotherapy administrated to the cases after the scorpion sting according to patients’ age at the referral hospital for the assistance and treatment of accidents by venomous animals in Alagoas State, Northeast of Brazil, from 2007 to 2017.
| Age Range (years) | Serotherapy | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Yes | No | Ignored/omitted | Total | |||||
|
|
|
|
|
|||||
| N | % | N | % | N | % | N | % | |
| < 1 | 30 | 6.6 | 127 | 0.5 | 0 | 0.0 | 157 | 0.6 |
| 1- to 4 | 199 | 43.4 | 1,876 | 6.8 | 4 | 7.8 | 2,079 | 7.4 |
| 5- to 9 | 83 | 18.1 | 2,314 | 8.4 | 2 | 3.9 | 2,399 | 8.6 |
| 10- to 14 | 10 | 2.2 | 2,278 | 8.3 | 2 | 3.9 | 2,290 | 8.2 |
| 15- to 19 | 12 | 2.6 | 2,338 | 8.5 | 7 | 13.7 | 2,357 | 8.4 |
| 20- to 29 | 23 | 5.0 | 4,706 | 17.1 | 13 | 25.5 | 4,742 | 16.9 |
| 30- to 39 | 24 | 5.2 | 4,124 | 15.0 | 8 | 15.7 | 4,156 | 14.8 |
| 40- to 49 | 18 | 3.9 | 3,593 | 13.1 | 3 | 5.9 | 3,614 | 12.9 |
| 50- to 59 | 28 | 6.1 | 2,846 | 10.4 | 8 | 15.7 | 2,882 | 10.3 |
| 60- to 69 | 16 | 3.5 | 1,954 | 7.1 | 3 | 5.9 | 1,973 | 7.0 |
| 70- to 79 | 11 | 2.4 | 975 | 3.5 | 0 | 0.0 | 986 | 3.5 |
| > 80 | 4 | 0.9 | 348 | 1.3 | 1 | 2.0 | 353 | 1.3 |
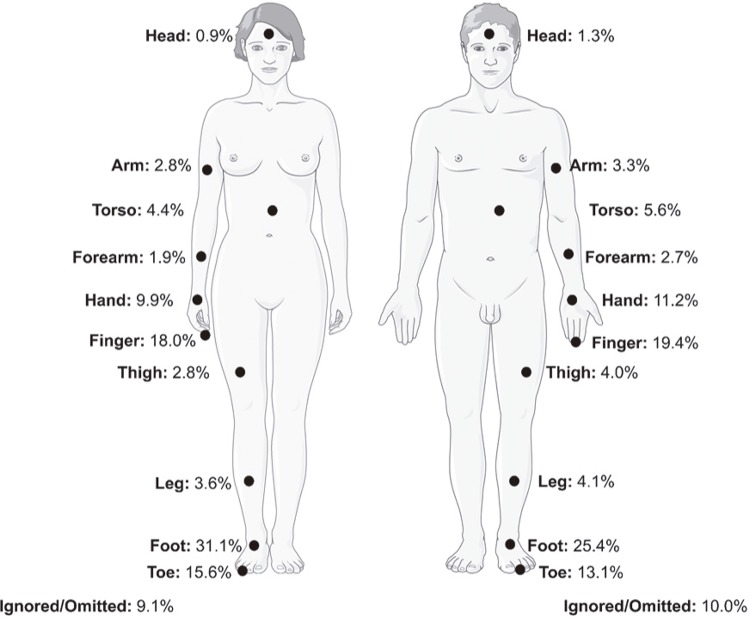
The analysis comparing the body sites of scorpion stings revealed a higher frequency in the foot (28.9%), followed by the finger (18.5%), the toe (14.6%) and the hand (10.4%) (Table 3). In addition, the frequency distribution of the stung body site was very similar for both male and female groups (Figure 2). Considering the case severity, the most common body sites were the foot, finger, and toe in the mild and moderate cases. However, in the severe cases, the most commonly stung site was also the foot (27.6%), followed by both the hand and toe with the same frequencies (both at 13.3%) (Table 3).
Figure 2. Frequency distribution of body sites of scorpion stings cases treated at the referral hospital for the assistance and treatment of accidents by venomous animals in Alagoas State, Northeast of Brazil, from 2007 to 2017.
Considering the time between the scorpion sting and the medical care assistance, 56.6% of all the cases were treated at the hospital within the first hour after the accident (Table 3), and an association was detected between the occurrence of systemic manifestations (SM) and the time elapsed until medical care (p <0.001) (Supplementary Material (1.5MB, pdf) ). In addition, SM were not observed in 64.2% of the cases which were treated up to one hour after the accident, therefore suggesting that a faster medical assistance after a scorpion sting contributes to a better prognosis.
The serotherapy was administered to 1.6% of all the cases, of which, 78.5% of the moderate cases and 89.8% of the severe cases were treated with anti-scorpion venom serum (Table 3).
DISCUSSION
Scorpion envenomation is one of the most serious health challenges in tropical and subtropical regions, and epidemiological research can identify factors attributed to scorpion stings which guide public health policies. In light of these, over the years, our study has shown an increase in the number of cases of scorpion stings treated at a referral hospital for the treatment of accidents by venomous animals in Alagoas State.
In a previous study conducted with SINAN data encompassing all Brazilian States in the years 2000 to 2012, Alagoas presented the highest annual average incidence rate10. When comparing with the period analyzed in our study, the rate increased more than 60%, raising alarm to this public health problem. The literature points out that during the hottest and rainiest periods of the year there are the highest incidences of scorpion stings in Brazil21. However, we did not observe a significant difference in the number of cases of scorpion stings among the months in the analyzed period in Alagoas. This result can be explained by the slight temperature variations mainly in Maceio and the forest zone regions of Alagoas State11, which should have allowed the same level of scorpion activity throughout the year. In the same way, previous studies performed in the Northeast region of Brazil had also failed to detect significant differences in the number of cases over the months22,23.
The highest frequency of scorpion stings was observed in females compared to the male group of patients. These data corroborate results of other studies carried out in the Northeast region of Brazil22,24-26. This exposure relationship can be explained by the longer period of time that women usually stay in the home environment, compared to men, as previously reported27. The home environment is a shelter for scorpion feeding and proliferation, due to the abundant presence of synanthropic opportunistic arthropods which constitute its diet28. On the other hand, it is important to note that studies carried out in the Brazilian North, South and Southeast regions detected a higher incidence rate of scorpion stings in males, related to the exposure in the workplace29,30. Another fact that may explain the disparity among genders is probably the higher propensity to seek medical care by women. In this way, aspects of gender identity reinforced by cultural standards can influence those seeking medical treatment, therefore, resulting in the self-neglected care needed to maintain the quality of health31,32.
The patient’s occupation highlights the home environment as a risky place for scorpion stings because most of the patients were students, housewives and retired/pensioners. However, it is important to emphasize that, while the SNF provides a field for reporting occupational accidents, a field detailing the patient’s activity at the time of the accident could better clarify and establish a more accurate relationship between exposure to risks.
The largest number of cases occurred in adult patients, corroborating other previous studies that highlighted this economically active population as the most susceptible to scorpion stings10,22,24,25. Moreover, the majority of the cases in this study occurred in urban areas, as previously reported in different regions of Brazil10,22,24,25. In this way, socio-demographics factors such as urbanization, high-density population, low-income population, poor housing conditions and lack of sanitation are determining factors for the increase in the number of cases of scorpionism3,30. In addition, the high density of the scorpion population can be justified by both, adaptations to the urban environment and the rapid spread of the scorpion species by parthenogenesis reproduction33.
Several body sites can be targeted by scorpions. In the present study, the majority of scorpion stings occurred on the lower limbs followed by upper limbs as reported in some studies24,34. Moreover, the foot was the most affected body site corresponding to 28.9 % of all cases. In contrast, other studies carried out in other locations around Brazil, have detected the upper limbs as the most affected anatomical sites22,30,35,36. It is important to emphasize that the extremities of the body are generally the most affected sites and are usually associated with routine activities such as wearing shoes without careful observation36.
The elapsed time between the sting and early medical treatment is a crucial factor that greatly influences the prognosis of scorpion accidents7, as our study revealed that approximately 75% of all the patients received medical treatment up to 3 hours after the accident, in accordance with other previous studies22-24,26,29. In addition, in pediatric patients, a known risk group for scorpionism9,37, it was shown that prompt medical care may result in a better prognosis and therefore in mild cases38. The observation that the majority of cases with moderate or severe cases was detected in the age group up to 9 years old highlights the need for additional care with pediatric patients. Moreover, the frequencies of moderate and severe cases observed in this age group were higher than those previously reported39,40. The severity of scorpion envenomation depends on several factors such as the anatomical location of the bite, age, weight, and health status of the victim1. In pediatric patients, both the lowest blood volume and the lowest total body volume contributed to the excessive concentration of scorpion venom in the plasma, favoring the manifestation of severe symptoms and consequently, a higher risk of death5,41.
The treatment with serotherapy is indicated only in moderate and severe cases7, and in consonance with this indication, we observed that the antitoxin sera was administered to 1.6 % of the total cases; which is a result similar to the frequency reported by another epidemiological study in Brazil36.
In Brazil, accidents with venomous animals require a mandatory report, filling all the fields in the SNF, according to the Ministry of Health42. It is important to emphasize that certain data such as the education level, the occupational employment, sting location and time elapsed between the accident and the medical care were sometimes ignored and unfilled which undermines the epidemiological analysis. This lack of information has also been reported for other diseases with mandatory reporting43-45. Therefore, the awareness among healthcare professionals of the importance of completing the SNF ensures the integrity of the collected and reported data.
The SINAN data has the purpose of identifying priority areas, monitoring and evaluation46. Our study highlights the urgent necessity of public policies that promote monitoring and treatment, but mainly control strategies. In this sense, actions to prevent proliferation, through monitoring, control, management, and environmental education46 should be implemented by the State. For monitoring, it is necessary to use indicators that clarify the level and intensity of home infestations, which can be carried out by community health agents and/or endemic agents46. Some species of scorpions are adapted to human environments and play an important role in the ecological balance47. Therefore, the eradication of these species is neither possible nor viable.
The control and population management of the species is based on the removal of scorpions and the modification of environmental conditions, disfavoring the occurrence, permanence, and proliferation of these animals46. The actions of health managers must embrace efforts in urban cleaning, sanitation, public works, and environmental education, while incorporating control measures into the daily life of the population46.
In summary, this study reported scorpionism as a serious public health problem in previous years in Alagoas State, Northeast Brazil, with an enormous number of cases occurring from 2007 to 2017. The clinical and epidemiological factors of scorpionism raised in this endemic area can collaborate to health surveillance of scorpion accidents, mainly in tropical and subtropical regions throughout the world. The results have also highlighted the need to establish and/or intensify prevention and education campaigns to avoid scorpion stings that may result in the reduction of its morbidity.
ACKNOWLEDGMENTS
We would like to thank the support of Teaching Assistance Management at Hospital Escola Dr. Helvio Auto, Maceio, Alagoas, Brazil for allowing and approving the data collection for this study. The authors also acknowledge the website https://smart.servier.com used to generate the manuscript Figure 2.
ETHICAL APPROVAL
All the data were based only on secondary data, without access the patients’ nominal data or anything else that could identify and following the ethical and legal requirements as requested by Resolution Nº 466/12 from the National Health Council (CNS), Brazil. The data collection for this study was authorized by Teaching Assistance Management at Hospital Escola Dr. Hélvio Auto, Maceió, Alagoas, Brazil.
FUNDING
JTS has a PhD scholarship from the Fundação de Amparo à Pesquisa do Estado de Alagoas (FAPEAL).
REFERENCES
- 1.Santos MS, Silva CG, Neto BS, Grangeiro CR, Júnior, Lopes VH, Teixeira AG, Júnior, et al. Clinical and epidemiological aspects of scorpionism in the world: a systematic review. Wilderness Environ Med. 2016;27:504–518. doi: 10.1016/j.wem.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 2.Chippaux JP, Goyffon M. Epidemiology of scorpionism: a global appraisal. Acta Trop. 2008;107:71–79. doi: 10.1016/j.actatropica.2008.05.021. [DOI] [PubMed] [Google Scholar]
- 3.Reckziegel GC, Pinto VL., Junior Análise do escorpionismo no Brasil no período de 2000 a 2010. Rev Pan-Amaz Saude. 2014;5:67–68. [Google Scholar]
- 4.Pucca MB, Oliveira FN, Schwartz EF, Arantes EC, Lira-da-Silva RM. Scorpionism and dangerous species of Brazil. In: Gopalakrishnakone P, editor, editor. Toxinology. Dordrecht: Springer Netherlands; 2014. pp. 1–24. [Google Scholar]
- 5.Isbister GK, Bawaskar HS. Scorpion envenomation. N Engl J Med. 2014;371:457–463. doi: 10.1056/NEJMra1401108. [DOI] [PubMed] [Google Scholar]
- 6.Amaral CF, Rezende NA. Both cardiogenic and non-cardiogenic factors are involved in the pathogenesis of pulmonary oedema after scorpion envenoming. Toxicon. 1997;35:997–998. doi: 10.1016/s0041-0101(96)00206-1. [DOI] [PubMed] [Google Scholar]
- 7.Brasil. Ministério da Saúde. Fundação Nacional de Saúde . Manual de diagnóstico e tratamento de acidentes por animais peçonhentos. 2ª. Brasília: Ministério da Saúde; 2001. [cited 2020 Apr 14]. https://www.icict.fiocruz.br/sites/www.icict.fiocruz.br/files/Manual-de-Diagnostico-e-Tratamento-de-Acidentes-por-Animais-Pe--onhentos.pdf. [Google Scholar]
- 8.Brasil. Ministério da Saúde. Sistema de Informação de Agravos de Notificação Ficha de investigação: acidentes por animais peçonhentos. [cited 2020 Apr 14]. http://portalsinan.saude.gov.br/images/documentos/Agravos/AAP/Animais_Peconhentos_v5.pdf.
- 9.Bouaziz M, Bahloul M, Kallel H, Samet M, Ksibi H, Dammak H, et al. Epidemiological, clinical characteristics and outcome of severe scorpion envenomation in South Tunisia: Multivariate analysis of 951 cases. Toxicon. 2008;52:918–926. doi: 10.1016/j.toxicon.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 10.Reckziegel GC, Pinto VL., Jr Scorpionism in Brazil in the years 2000 to 2012. 46J Venom Anim Toxins Incl Trop Dis. 2014;20 doi: 10.1186/1678-9199-20-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barros AH, Araújo JC, Filho, Silva AB, Santiago GA. Climatologia do Estado de Alagoas. Recife: Embrapa; 2012. [Google Scholar]
- 12.Instituto Brasileiro de Geografia e Estatística . Censo demográfico 2010 : características da população e dos domicílios : resultados do universo. Rio de Janeiro: IBGE; 2010. [Google Scholar]
- 13.Zou KH, Tuncali K, Silverman SG. Correlation and simple linear regression. Radiology. 2003;227:617–622. doi: 10.1148/radiol.2273011499. [DOI] [PubMed] [Google Scholar]
- 14.Kim TK. T test as a parametric statistic. Korean J Anesthesiol. 2015;68:540–546. doi: 10.4097/kjae.2015.68.6.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kao LS, Green CE. Analysis of variance: is there a difference in means and what does it mean? J Surg Res. 2008;144:158–170. doi: 10.1016/j.jss.2007.02.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McHugh ML. Biochem Med. Vol. 21. Zagreb: 2011. Multiple comparison analysis testing in ANOVA; pp. 203–209. [DOI] [PubMed] [Google Scholar]
- 17.Buckalew LW, Pearson WH. Determination of critical observed frequencies in chi square. Bull Psychon Soc. 1981;18:289–290. [Google Scholar]
- 18.Fraas JW, Newman I. A binomial test of model fit. Struct Equ Modeling. 1994;1:268–273. [Google Scholar]
- 19.McHugh ML. Biochem Med. Vol. 23. Zagreb: 2013. The chi-square test of independence; pp. 143–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yates D, Moore D, McCabe G. The practice of statistics. New York: WH Freeman & Company; 1999. [Google Scholar]
- 21.Brazil TK, Porto TJ. Os escorpiões. Salvador: EDUFBA; 2010. [Google Scholar]
- 22.Furtado SS, Belmino JF, Diniz AG, Leite RS. Epidemiology of scorpion envenomation in the State of Ceará, Northeastern Brazil. 15Rev Inst Med Trop Sao Paulo. 2016;58 doi: 10.1590/S1678-9946201658015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lira-da-Silva RM, Amorim AM, Carvalho FM, Brazil Acidentes por escorpião na cidade do Salvador, Bahia, Brasil TK. Gaz Med Bahia. 2009;79(Supl 1):43–49. [PubMed] [Google Scholar]
- 24.Araújo KA, Tavares AV, Marques MR, Vieira AA, Leite RS. Epidemiological study of scorpion stings in the Rio Grande do Norte State, Northeastern Brazil. e58Rev Inst Med Trop Sao Paulo. 2017;59 doi: 10.1590/S1678-9946201759058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mesquita FN, Nunes MA, Santana VR, Machado JM, Neto, Almeida KB, Lima SO. Acidentes escorpiônicos no estado do Sergipe - Brasil. Rev Fac Cienc Med Sorocaba. 2015;17:15–20. [Google Scholar]
- 26.Almeida TS, Fook SM, França FO, Monteiro TM, Silva EL, Gomes LC, et al. Spatial distribution of scorpions according to the socioeconomic conditions in Campina Grande, State of Paraíba, Brazil. Rev Soc Bras Med Trop. 2016;49:477–485. doi: 10.1590/0037-8682-0128-2016. [DOI] [PubMed] [Google Scholar]
- 27.Barbosa AL. Tendências nas horas dedicadas ao trabalho e lazer: uma análise da alocação do tempo no Brasil. Rio de Janeiro: IPRA; 2018. [Google Scholar]
- 28.Lourenço WR. What do we know about some of the most conspicuous scorpion species of the genus Tityus? A historical approach. 20J Venom Anim Toxins Incl Trop Dis. 2015;21 doi: 10.1186/s40409-015-0016-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Costa CL, Fé NF, Sampaio I, Tadei WP. A profile of scorpionism, including the species of scorpions involved, in the State of Amazonas, Brazil. Rev Soc Bras Med Trop. 2016;49:376–379. doi: 10.1590/0037-8682-0377-2015. [DOI] [PubMed] [Google Scholar]
- 30.Nunes CS, Bevilacqua PD, Jardim CC. Aspectos demográficos e espaciais dos acidentes escorpiônicos no Distrito Sanitário Noroeste, Município de Belo Horizonte, Minas Gerais, 1993 a 1996. Cad Saude Publica. 2000;16:213–223. doi: 10.1590/s0102-311x2000000100022. [DOI] [PubMed] [Google Scholar]
- 31.Levorato CD, Mello LM, Silva AS, Nunes AA. Fatores associados à procura por serviços de saúde numa perspectiva relacional de gênero. Cien Saude Coletiva. 2014;19:1263–1274. doi: 10.1590/1413-81232014194.01242013. [DOI] [PubMed] [Google Scholar]
- 32.Gomes R, Nascimento EF, Araújo FC. Por que os homens buscam menos os serviços de saúde do que as mulheres ? As explicações de homens com baixa escolaridade e homens com ensino superior. Cad Saude Publica. 2007;23:565–574. doi: 10.1590/s0102-311x2007000300015. [DOI] [PubMed] [Google Scholar]
- 33.Lourenço WR, Cuellar O. Scorpions, scorpionism, life history strategies and pathernogenesis. J Venom Anim Toxins. 1995;1:51–62. [Google Scholar]
- 34.Zanella DP, Valadão AF, Arêdes CA, Campos GC, Cordeiro ND, Spencer PJ. Escorpionismo no Vale do Aço, Minas Gerais. Braz J Surg Clin Res. 2018;23:60–66. [Google Scholar]
- 35.Soares MR, Azevedo CS, De Maria M. Escorpionismo em Belo Horizonte, MG: um estudo retrospectivo. Rev Soc Bras Med Trop. 2002;35:359–363. doi: 10.1590/s0037-86822002000400013. [DOI] [PubMed] [Google Scholar]
- 36.Barbosa AD, Magalhães DF, Silva JA, Silva MX, Cardoso MF, Meneses JN, et al. Caracterização dos acidentes escorpiônicos em Belo Horizonte, Minas Gerais, Brasil, 2005 a 2009. Cad Saude Publica. 2012;28:1785–1789. doi: 10.1590/s0102-311x2012000900016. [DOI] [PubMed] [Google Scholar]
- 37.Bahloul M, Chabchoub I, Chaari A, Chtara K, Kallel H, Dammak H, et al. Scorpion envenomation among children: Clinical manifestations and outcome (analysis of 685 cases) Am J Trop Med Hyg. 2010;83:1084–1092. doi: 10.4269/ajtmh.2010.10-0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Santos JM, Croesy GS, Marinho LF. Perfil epidemiológico dos acidentes escorpiônicos em crianças, no estado da Bahia, de 2007 a 2010. Rev Enferm Contemp. 2012;1:118–129. [Google Scholar]
- 39.Bosnak M, Ece A, Yolbas I, Bosnak V, Kaplan M, Gurkan F. Scorpion sting envenomation in children in southeast Turkey. Wilderness Environ Med. 2009;20:118–124. doi: 10.1580/07-WEME-OR-098RR3.1. [DOI] [PubMed] [Google Scholar]
- 40.Khatony A, Abdi A, Fatahpour T, Towhidi F. The epidemiology of scorpion stings in tropical areas of Kermanshah province , Iran , during 2008 and 2009. 45J Venom Anim Toxins Incl Trop Dis. 2015;21 doi: 10.1186/s40409-015-0045-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.D’Suze G, Moncada S, González C, Sevcik C, Aguilar V, Alagón A. Relationship between plasmatic levels of various cytokines, tumour necrosis factor, enzymes, glucose and venom concentration following Tityus scorpion sting. Toxicon. 2003;41:367–375. doi: 10.1016/s0041-0101(02)00331-8. [DOI] [PubMed] [Google Scholar]
- 42.Brasil. Ministério da Saúde. Gabinete do Ministro Portaria N° 204, de 17 de fevereiro de 2016. Define a Lista Nacional de Notificação Compulsória de doenças, agravos e eventos de saúde pública nos serviços de saúde públicos e privados em todo o território nacional, nos termos do anexo, e dá outras providências. [cited 2020 Apr 14]. https://portalarquivos2.saude.gov.br/images/pdf/2018/abril/25/Portaria-n---2014-de-17--Fevereiro-2016.pdf.
- 43.Pinheiro RS, Andrade VL, Oliveira GP. Subnotificação da tuberculose no Sistema de Informação de Agravos de Notificação (SINAN): abandono primário de bacilíferos e captação de casos em outras fontes de informação usando linkage probabilístico. Cad Saude Publica. 2012;28:1559–1568. doi: 10.1590/s0102-311x2012000800014. [DOI] [PubMed] [Google Scholar]
- 44.Lafetá KR, Martelli H, Júnior, Silveira MF, Paranaíba LM. Maternal and congenital syphilis, underreported and difficult to control. Rev Bras Epidemiol. 2016;19:63–74. doi: 10.1590/1980-5497201600010006. [DOI] [PubMed] [Google Scholar]
- 45.Lacerda KM, Fernandes RC, Nobre LC. Acidentes de trabalho fatais em Salvador, BA: descrevendo o evento subnotificado e sua relação com a violência urbana. Rev Bras Saude Ocup. 2014;39:63–74. [Google Scholar]
- 46.Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Vigilância Epidemiológica . Manual de controle de escorpiões. Brasília: Ministério da Saúde; 2009. [Google Scholar]
- 47.Lourenço WR. Scorpions and life-history strategies: from evolutionary dynamics toward the scorpionism problem. 19J Venom Anim Toxins Incl Trop Dis. 2018;24 doi: 10.1186/s40409-018-0160-0. [DOI] [PMC free article] [PubMed] [Google Scholar]