To the Editor: The effect of the Covid-19 pandemic on medical care for conditions other than Covid-19 has been difficult to quantify.1 Any decrease in care for patients with acute conditions such as ischemic stroke may be consequential because timely treatment may decrease the incidence of disability.2-4
We used the numbers of patients in a commercial neuroimaging database associated with the RAPID software platform (iSchemaView) as a surrogate for the quantity of care that hospitals provided to patients with acute ischemic stroke. This software system is typically used to select patients who may benefit from endovascular thrombectomy by identifying occlusions of major brain arteries or regions of the brain with potentially reversible ischemia that have not become infarcted.5 Imaging data with demographic information are uploaded in real time to a data repository. The vendor of RAPID was not involved in the analysis or interpretation of the data or the writing of this letter. The first author serves on the medical advisory board of the vendor, and the last author is a consultant to the vendor. No confidentiality agreements related to this analysis are in place between the authors and this company.
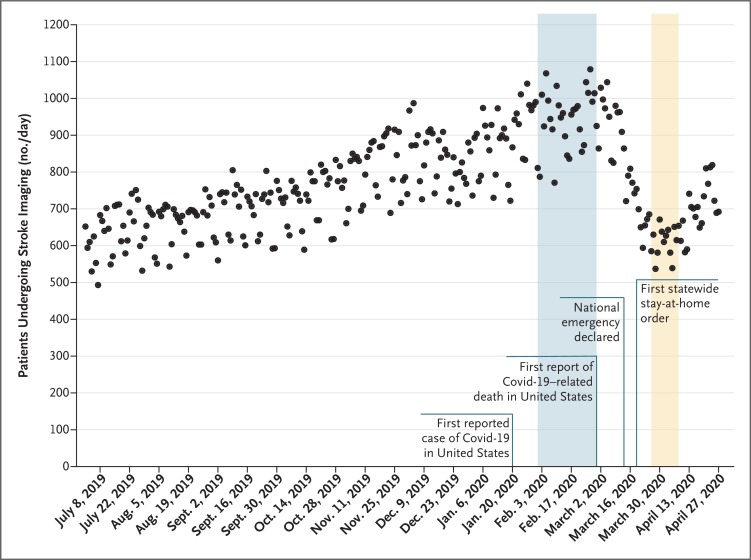
We had access to data on 231,753 patients who underwent imaging processed with RAPID software in 856 hospitals in the United States from July 1, 2019 through April 27, 2020. The daily counts of unique patients who underwent imaging decreased in March 2020 (Figure 1). We therefore chose to compare the mean daily counts per hospital of patients in the RAPID system in an ostensibly prepandemic 29-day epoch from February 1, 2020, through February 29, 2020, with the mean daily counts per hospital of patients in a 14-day epoch during the early pandemic, from March 26, 2020, through April 8, 2020. During the prepandemic epoch, the numbers of patients per hospital who underwent imaging were similar to the baseline numbers immediately before the prepandemic epoch. The nadir of the daily counts after the first case of Covid-19 was reported in the United States occurred during the 14-day epoch. The number of patients who underwent imaging decreased by 39%, from 1.18 patients per day per hospital in the prepandemic epoch to 0.72 patients per day per hospital in the early-pandemic epoch (see Figs. S1 and S2 in the Supplementary Appendix, available with the full text of this letter at NEJM.org). An apparent increase in the number of patients who underwent imaging after the early-pandemic epoch warrants further investigation.
Figure 1. Daily Counts of Unique Patients Who Underwent Neuroimaging for Stroke in the United States, July 2019 through April 2020.
All the neuroimaging tests were processed with RAPID software. Each dot represents a daily count of patients. Shaded regions correspond to the prepandemic (blue) and early-pandemic (yellow) epochs. The increase in the number of patients who underwent imaging from July 2019 to March 2020 reflects an increase in the number of hospitals that were using RAPID software.
The decrease in the use of stroke imaging from the prepandemic epoch to the early-pandemic epoch was seen across all age, sex, and stroke severity subgroups (Table S1); this suggests a decrease in the number of evaluations both in patients with severe strokes and in nonelderly patients who may have been at low risk for Covid-19 complications. Decreases in the numbers of patients who underwent stroke imaging were seen in most states and across a range of hospital volumes (Fig. S3 and Table S2). These decreases suggest that differences in regional incidences of Covid-19 were not the primary cause of decreased use of stroke imaging.
Our analysis has limitations. We used a surrogate for the amount of care provided, and the database, which pertains predominantly to patients who were under consideration for endovascular thrombectomy at designated stroke centers, may not reflect the care provided at other hospitals. We found that the collateral effect of Covid-19 was a decrease of approximately 39% in the numbers of patients who received evaluations for acute stroke between two recent epochs in U.S. hospitals.
Supplementary Appendix
Disclosure Forms
This letter was published on May 8, 2020, at NEJM.org.
Footnotes
Disclosure forms provided by the authors are available with the full text of this letter at NEJM.org.
References
- 1.Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol 2020. April 9 (Epub ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016;387:1723-1731. [DOI] [PubMed] [Google Scholar]
- 3.Nogueira RG, Jadhav AP, Haussen DC, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 2018;378:11-21. [DOI] [PubMed] [Google Scholar]
- 4.Albers GW, Marks MP, Kemp S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 2018;378:708-718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heit JJ, Sussman ES, Wintermark M. Perfusion computed tomography in acute ischemic stroke. Radiol Clin North Am 2019;57:1109-1116. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.