Abstract
To date, no country has reached a natural COVID-19 epidemic peak and observed peaks essentially reflect the effectiveness of ‘lockdown’ measures. The major challenge is finding a responsible way out of ‘lockdown’, given that SARS- CoV-2 is now an established global pathogen. Acknowledging limitations in our knowledge regarding the sufficiency and durability of immune responses following natural SARS Cov-2 infection, we discuss three pathways to ‘community protection’. Uncontrolled epidemic spread (route 1; R0 > 2) has been associated with overwhelmed health care systems and high death rates, especially in the vulnerable. Controlled epidemic spread (route 2; effective R0 1–2) can be achieved with limited or strict control of social mixing; strict control will be necessary to ensure that only low-risk individuals become infected, without spill-over to vulnerable groups during their period of infectiousness. It has been demonstrated that local epidemic elimination (route 3; effective R0 < 1) can be achieved through prolonged ‘lock down’, supplemented by early active case finding with quarantine of close contacts to ensure rapid termination of transmission chains within the community. Although universal availability of a safe and effective vaccine remains the preferred ‘exit strategy’, this may be hard to achieve and alternative options must be considered with careful consideration of all adverse outcomes – including health, social and economic consequences.
Keywords: COVID-19, SARS Cov-2, Community protection, Herd immunity, Controlled infection
The COVID-19 pandemic represents many of the characteristics previously identified in emerging infectious disease ‘nightmare scenarios’, including the ‘silent man’ phenomenon (Hill-Cawthorne et al., 2019). Stringent social/physical distancing measures have successfully flattened the COVID-19 epidemic curve in countries like Australia, New Zealand, Iceland, China and South Korea. However, while these stringent measures (also referred to as ‘lockdown’) have been highly successful in preventing catastrophic epidemic escalation, they impose major social and economic costs on society.
The challenge for countries with highly effective public health systems that are able to establish epidemic control is “How to find a responsible way out of lockdown”. Mathematical models consistently predict rapid epidemic rebound following relaxation of lockdown measures - in the absence of herd immunity and as long as the SARS CoV-2 virus circulates within the country (Ferguson et al., 2020, Kissler et al., 2020). The height of the predicted rebound peak is partly determined by the success of the initial lockdown measures, with a higher peak if the initial lockdown measures were very successful and prevented the accrual of substantial herd immunity (Ferguson et al., 2020). However, the overriding determinant of the height of the rebound peak, as with the height of the initial peak, will be the effectiveness of the social/physical distancing measures that remain in place. We now know that effective epidemic containment is possible, even in the absence of herd immunity. This provides scope for experimentation, with the assurance that containment can be re-established as required.
Critically, no country has as yet reached a natural epidemic peak. The peaks that we observe essentially reflect the effectiveness of lockdown measures – they do not necessarily indicate that the worst is past. Even countries with high disease and death rates, like Italy, are not yet close to their natural epidemic peak. In fact, at the end of April, it was estimated that less than 5% of the Italian population had been infected (based on the assumption that 10 people were infected for every one of the ∼200 000 cases formally reported), meaning that more than 95% of the population remained vulnerable to infection and able to facilitate epidemic rebound.
Given that SARS- CoV-2 is now a global pathogen, the reality is that it will likely be around ‘forever’ with possible seasonal variation as observed with the other beta coronaviruses. Beta coronaviruses known to infect man include SARS- CoV-1, which was successfully eradicated, and MERS that causes severe disease with case fatality rates in excess of 10% (Su et al., 2016). It also includes CoV-OC43 and HCoV-HKU1 that are associated with mild upper respiratory tract infections, typically associated with autumn/wintertime colds in temperate regions (Killerby et al., 2018, Neher et al., 2020).
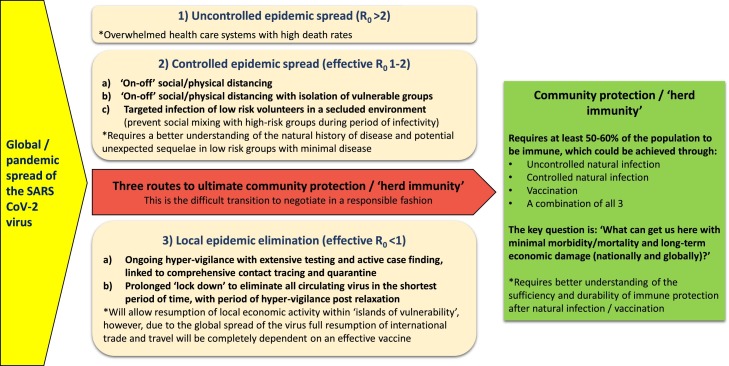
Although we need to learn more about the immunity induced by natural SARS Cov-2 infection, experience with other coronavirus infections has shown that protective immunity can develop and usually offers some cross-protection against other beta-coronaviruses (Kissler et al., 2020, Huang et al., 2020), but will likely wane over time. However, recurrent infection with the same virus is rare and even if it does occur it is associated with milder symptoms and reduced viral excretion (Huang et al., 2020). Thus, in future the world might see seasonal disease spikes affecting those with absent or waning immunity, but we should not observe repeated pandemic outbreaks once herd immunity has been established. Figure 1 presents an overview of identified pathways to herd immunity, which should provide reasonable community protection.
Figure 1.
Three potential routes to ultimate community protection.
Pathways to herd immunity
Route 1 (Uncontrolled epidemic spread - R0 >2)
Given the infectiousness and high virulence (especially among older people) of SARS- CoV-2, the experience to date demonstrates that with uncontrolled epidemic spread health care systems are overwhelmed and death rates are high. Despite initial delays in recognising the scale of the threat, most resource rich countries have been able to contain exponential epidemic growth by implementing strict social/physical distancing. However, this is far more challenging in poor countries where effective social/physical distancing is near impossible to enforce and sustain for an extended period of time. These countries may be partially protected by their younger age demographic, since young people tend to develop mild disease.
A more feasible option may be to try and limit mortality by preventing ‘epidemic overshoot’, i.e. the number of additional people infected when a rapidly spreading epidemic enters a completely naïve population, compared with when it reaches a natural plateau as herd immunity accumulates in time. A targeted strategy of short term lockdown once ‘near herd immunity levels’ have been reached (infection of around 40–50% of the population) could save many lives, without the excessive socioeconomic disruption caused by prolonged lockdown measures. Other practical interventions to consider include targeted social distancing that focuses on the highest risk groups and particular hot spot areas, strict attention to hand hygiene and universal wearing of face masks in an attempt to reduce the effective R0. It should be noted that there is little evidence that cloth masks protect the wearer (Offeddu et al., 2017, MacIntyre et al., 2013), but the aim would be to limit droplet (and possibly aerosol) production at source. In settings where social/physical distancing is highly problematic universal mask wearing might reduce overall environmental contamination and epidemic spread, especially from minimally symptomatic COVID-19 cases that unwittingly transmit the infection.
Route 2 (Controlled epidemic spread – effective R0 1-2)
This route presents two broad options for controlled epidemic spread - those with limited control of social mixing (presented by 2a and 2b) and those with strict control of social mixing to ensure that only the lowest risk groups become infected (presented by 2c) with complete isolation from vulnerable groups during their period of infectiousness.
Modelled outcomes of routes 2a and 2b demonstrated an inability to limit excessive mortality, given that social mixing inevitably allows spread to vulnerable groups (Ferguson et al., 2020). Sweden provides a case in point, where limited social distancing has been successful in reducing exponential epidemic growth with some accrual of herd immunity, but the price has been high with many deaths in vulnerable groups. Given limited intensive care unit (ICU) capacity even in well-resourced settings, the effective R0 needs to be very close to 1 (<1.2) in order to prevent health system overload. An effective R0 of around 1 would draw the epidemic out over 3–5 years or more. This implies that social distancing measures will have to stay in place for a long period of time (being ramped up and down as the situation demands), while international travel will pose an ongoing risk of disease importation and subsequent epidemic spread in the absence of herd immunity.
A potential approach to assist the development of herd immunity in the absence of an effective vaccine, would be to specifically target infection at the lowest risk groups, as in route 2c. A remarkable and consistent observation during the pandemic has been that healthy young people very rarely develop severe disease (Ludvigsson, 2020). In fact, a high proportion of those infected report only minimal symptoms and may even be completely asymptomatic. However, it should be acknowledged that significant morbidity and even mortality has been documented in rare instances and that long term sequelae of infection remains unknown.
The infection of healthy young volunteers (without any pre-existing co-morbidity or risk factor) in a secure environment (without any social mixing outside that environment during the period of infectivity) could help to build herd immunity with minimal morbidity or mortality. Potential benefits of facilitating natural infection in a safe and responsible manner include:
-
1)
immune individuals will be able to ‘get on with their life’ without the need for ongoing social restrictions and without putting the safety of vulnerable people at risk
-
2)
increasing numbers of immune individuals will build community protection. Given that SARS CoV-2 has an estimated R0 of 2.4 (although this may be variable in different conditions) (Ferguson et al., 2020), around 60% of the population will require immunity to limit transmission and protect vulnerable groups in the absence of any other measures. However, as a complementary measure it could support limited social distancing measures and will be additive to the immunity resulting from uncontrolled natural infection and that afforded by any future vaccine, which would prioritise vulnerable populations.
Such an approach would be highly controversial, with multiple ethical hurdles to be overcome in the context of a novel disease about which many questions remain unanswered. Careful consideration should be given to unrecognised or delayed sequelae of COVID-19 and this should be specifically studied in young people who have developed mild disease. Better characterisation of the sufficiency and durability of immune responses following mild COVID-19 disease is essential, as is careful exploration of potential antibody dependent enhancement (ADE) of disease during re-infection. ADE has not been observed in any of the other beta coronaviruses, but SARS CoV-2 is an unpredictable novel virus. The acceptability and safety of voluntary natural infection of low risk groups requires better data and preferably better treatment before it is even contemplated. If the infection of large numbers of volunteers is not considered safe or feasible, then the infection of smaller numbers of volunteers could still be useful in assisting urgent drug and vaccine development (Eyal et al., 2020) and there is growing support for this concept (Callaway, 2020) – provisionally also from the World Health Organisation (WHO, 2020).
Route 3 (Local epidemic elimination – effective R0 <1)
If R0 is sustained below 1 the epidemic will be unable to sustain itself, leading to eventual local elimination. This can be achieved through early active case finding with widespread testing, linked to strict quarantine of close contacts to prevent secondary cases and ensure rapid termination of transmission chains within the community. This also has ethical issues and privacy concerns, but the broad consensus is that it can be done in a fashion that still respects the liberties that underpin Western democratic societies (Hart et al., 2020). Alternatively, elimination can be achieved if very stringent lockdown measures terminate all transmission for a sufficient period of time to eliminate any remaining viral reservoirs. Patients who remain potentially infectious need to be kept in strict isolation, given indications that some people may excrete the virus for weeks, although it has not been verified that this is indeed live virus that can be transmitted (Atkinson and Petersen, 2020).
If local elimination is successful then life can essentially return to ‘normal’, except that contact with the outside world needs to be carefully considered, since rapid epidemic escalation could occur whenever the infection re-enters the country. Given that SARS CoV-2 is now an established global pathogen, this ‘solution’ will create ‘islands of vulnerability’ that traps countries in protective self-imposed isolation - in the absence of an effective vaccine.
We hoped to provide a coherent overview of pathway options to address the ‘wicked problems’ posed by COVID-19. At a national level, policies and actions need to be guided by what the end goal is. To date this has not been clearly articulated and short term targets, such as ‘bending the curve’ have been used to motivate action and define success. The longer-term exit strategy needs to consider and balance not only the health outcomes, but also the social and economic consequences of any course of action. Given the caveats around establishing natural herd immunity in the absence of better data on the safety and immunogenicity of natural SARS CoV-2 infection, every effort should be made to find a safe and effective vaccine in the shortest possible time frame. Although competition drives invention and efficiency, we are faced with a global problem that requires global solutions and excessive rivalry may hamper a coordinated global effort that will provide community protection to all, irrespective of their nationality or ability to pay.
Conflict of interest
No conflict of interest to declare.
Funding source
None.
Ethical approval
Approval was not required.
References
- Atkinson B., Petersen E. SARS-CoV-2 shedding and infectivity. Lancet. 2020;395:1339–1340. doi: 10.1016/S0140-6736(20)30868-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaway E. Hundreds of people volunteer to be infected with coronavirus. Nature. 2020;(April) doi: 10.1038/d41586-020-01179-x. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- Eyal N., Lipsitch M., Smith P.G. Human challenge studies to accelerate coronavirus vaccine licensure. J Infect Dis. 2020;(March) doi: 10.1093/infdis/jiaa152. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson N.M., Laydon D., Nedjati-Gilani G., Imai N., Ainslie K., Baguelin M. 2020. Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand, Imperial College COVID-19 Response Team, London.https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-NPI-modelling-16-03-2020.pdf [Google Scholar]
- Hart V., Siddarth D., Cantrell B., Tretikov L., Eckersley P., Langford J. 2020. Outpacing the virus: digital response to containing the spread of COVID-19 while mitigating privacy risks. 5th White Paper Harvard Edmond J. Safra Cetner for Ethics.https://ethics.harvard.edu/outpacing-virus [Google Scholar]
- Hill-Cawthorne G.A., Negin J., Capon T., Gilbert G.L., Nind L., Nunn M. Advancing planetary health in Australia – focus on emerging infections and antimicrobial resistance. BMJ Glob Health. 2019;4(2) doi: 10.1136/bmjgh-2018-001283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang A.T., Garcia-Carreras B., Hitchings M.D.T., Yang B., Katzelnick L.C., Rattigan S.M. A systematic review of antibody mediated immunity to coronaviruses: antibody kinetics, correlates of protection, and association of antibody responses with severity of disease. medRxiv preprint. 2020 doi: 10.1101/2020.04.14.20065771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killerby M.E., Biggs H.M., Haynes A., Dahl R.M., Mustaquim D., Gerber S.I. Human coronavirus circulation in the United States 2014-2017. J Clin Virol. 2018;101:52–56. doi: 10.1016/j.jcv.2018.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kissler S.M., Tedijanto C., Goldstein E., Grad Y.H., Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020;(April) doi: 10.1126/science.abb5793. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludvigsson J.F. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109:1088–1095. doi: 10.1111/apa.15270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacIntyre C.R., Wang Q., Seale H., Yang P., Shi W., Gao Z. A randomized clinical trial of three options for N95 respirators and medical masks in health workers. Am J Respir Crit Care Med. 2013;187:960–966. doi: 10.1164/rccm.201207-1164OC. [DOI] [PubMed] [Google Scholar]
- Neher R.A., Dyrdak R., Druelle V., Hodcroft E.B., Albert J. Potential impact of seasonal forcing on a SARS-CoV-2 pandemic. Swiss Med Wkly. 2020;150 doi: 10.4414/smw.2020.20224. eCollection 2020 March 9. [DOI] [PubMed] [Google Scholar]
- Offeddu V., Yung C.F., Low M.S.F., Tam C.C. Effectiveness of masks and respirators against respiratory infections in healthcare workers: a systematic review and meta-analysis. Clin Infect Dis. 2017;65:1934–1942. doi: 10.1093/cid/cix681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su S., Wong G., Shi W., Liu J., ACK, Zhou J. Epidemiology, genetic recombination and pathogenesis of coronaviruses. Trends Microbiol. 2016;24:490–502. doi: 10.1016/j.tim.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organisation (WHO) 2020. Key criteria for the ethical acceptability of COVID-19 human challenge studies - WHO Working Group for Guidance on Human Challenge Studies in COVID-19.https://www.who.int/ethics/publications/key-criteria-ethical-acceptability-of-covid-19-human-challenge/en/ [Google Scholar]