Letter:
The COVID-19 pandemic will certainly become a defining moment of the decade and possibly the century. Globally, we have been forced to adapt to a new normal that involves “social distancing,” “shelter-in-place” orders, citizens required to wear personal protective equipment in public, and navigating an economic shutdown. At the time of writing, the United States has surpassed 1 million confirmed cases of COVID-19, and 50,000 deaths in the period of only 2 months.1 The concept of “social distancing” is not new and has been shown to be an effective means to control the spread of highly contagious respiratory pathogens in the past.2 To advance this goal, medical students in the United States have been recommended by the Association of American Medical Colleges to not report for clinical clerkships since mid-March of this year.3 Recent work by Lewis et al.4 summarized how resident neurosurgical education has evolved to meet the needs of residents unable to attend face-to-face meetings. It details a network of virtual conferences, online education resources, and telemedicine visits that allow self-disciplined residents the ability to continue distance learning.4 However, no work to date has examined how undergraduate medical education can adapt to provide continuity of learning for medical students and continue recruitment of students into the field of neurosurgery.
To address this, the Department of Neurosurgery at Emory University School of Medicine has rapidly created a 1-week virtual clerkship that integrates didactics, case discussions, and telemedicine. In this letter, we wish to share our method for developing and delivering this curriculum to the Class of 2022 at our institution, as well as early lessons learned from the first iteration of this course.
Background
At our institution, the Class of 2022 had just begun their core clerkships (what most would call an “M3” student or a “third-year medical student”) in March 2020. Before these students had even reached 2 weeks of clinical coursework, their rotations were suspended without a plan on how to continue facilitating their medical educations. It is imperative that their education continue remotely to ensure an on-time graduation. Furthermore, there is still uncertainty as to when students may be allowed back into clinical settings, a decision that rests on individual schools, as well as local, state, and national governments. A delay in the completion of medical training for an entire class of students would have unforeseen and severe implications in the stability of our nation's medical schools and residency programs.
Virtual learning has been proven as a useful adjuvant to clinical education, and it has been used as a component of medical training during preclinical years.5 , 6 In fact, the use of teleconferences as a component of a surgical clerkship has been shown to increase the opportunity for student learning, and provide a medium to facilitate discussion of clinical cases.7 Others have used techniques, such as virtual reality, live streaming rounds from the hospital, and virtual patients, as a means to remotely educate students and develop their clinical skills.8, 9, 10, 11, 12, 13 During the COVID-19 pandemic, there has been a push to create a temporary fully virtual curriculum for trainees of all levels. Within our field of neurosurgery, the Congress of Neurological Surgeons has provided virtual learning in the form of online grand rounds and virtual visiting professors that provide 2–3 hours per week of didactics from faculty around the country.14 Despite all of these efforts, however, the gaps left in the standard third-year medical student clinical curriculum remains unfilled. Crucially, no medical school has yet reported a virtual class for third-year medical students within the field of neurosurgery that incorporates telemedicine.
Creation and Implementation
Our overarching goals in designing our curriculum were to expose students to neurosurgical topics building off of prior knowledge; introduce them to neurosurgical faculty and residents, as well as students interested in neurosurgery to learn from their experiences; facilitate interactions with neurosurgical patients through telemedicine clinics; and build synthesis and presentation skills. This meant recapitulating the didactic, clinical, and surgical experience via a teleconferencing tool.
A recent text by Thomas et al.15 titled “Curriculum Development for Medical Education” outlines 6 main pillars for creating and delivering a medical curriculum: 1) problem identification; 2) needs assessment of targeted learners; 3) goals and specific measurable objectives; 4) educational strategies; 5) implementation; and 6) evaluation and feedback. In our case, the problem was clear: the neurosurgical clerkship and subinternships were put on hold. To continue to deliver clinical and didactic sessions to students we used Zoom, Inc. (San Jose, California, USA), a teleconferencing tool that has already been used by our department for streaming conferences, and offered HIPAA/PIPEDA (Health Insurance Portability and Accountability Act, 1996/Personal Information Protection and Electronic Document Act) enabled plans for telemedicine clinics.16
Assessing the needs of medical students was done using a 3-fold technique. First, we queried common practice question test banks and review books used for USMLE Step 2 CK (United States Medical Licensure Examination Step 2 Clinical Knowledge) preparation, ensuring that we had a focused series of topics that were appropriate for medical students preparing for board examinations. However, we wanted to go beyond delivering a board review series. To that end, we referred to a recent supplement published in Operative Neurosurgery, titled “Essential Neurosurgery for Medical Students.” Supported by the Congress of Neurological Surgeons and Society of Neurological Surgeons, this series contains a “basic fund of [neurosurgical] knowledge all physicians should have, regardless of their chosen specialty.”17 The chapters served as scaffolds around which we constructed our lecture sessions, and allowed an introduction to a wider breadth of topics in neurosurgery. Finally, we selected a series of competencies deemed essential for clinical success, as determined by our medical school executive curriculum committee.18
Many of our learners were undecided about a specialty and would likely have questions about training and working as a neurosurgeon. Previous work by Zuckerman et al.19 showed formal exposure to faculty neurosurgeons in medical school through a structured curriculum that changed perceptions about a neurosurgeon's quality of life, both in training and beyond. We hoped that access to neurosurgeons in our elective would similarly increase interest in and understanding of the field. To accomplish this, we encouraged residents, fellows, and faculty to discuss their decision for choosing a career in neurosurgery, what their training was like, and describe their work-life over the course of their careers.
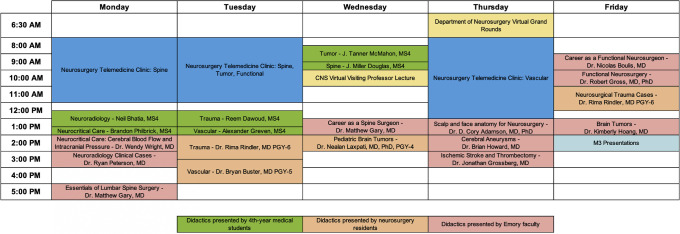
With our collected resources, we developed a series of learning objectives tied to medical student competencies (Table 1 ). Over the course of 1 week, senior medical students, residents, fellows, and faculty delivered didactic lectures via Zoom. These lectures covered principles of general neurosurgical and subspecialty topics, including neuroradiology, neurocritical care, trauma, vascular, tumor, spine, and functional. In total, there were 23 hours of didactics spread over 21 sessions (Figure 1 ). Trainee and faculty expertise guided students through curated surgical video content of select neurosurgical procedures. These were interspersed with telemedicine sessions, in which students joined faculty members virtually to observe and participate in clinic visits adding to a cumulative of 12 hours of clinic time. Participation in these visits required prior completion of online telehealth training modules to ensure HIPAA compliance. At the end of the week, students were asked to deliver a short presentation on a topic or patient of interest, which served as their assessment along with attendance and participation in all sessions. This included attendance of virtual grand rounds.14
Table 1.
Neurosurgery Elective Course Objectives
| To provide an introduction and basic clinical experience in neurosurgery. |
| Students will use critical thinking skills to develop a framework for defining, localizing, diagnosing, and managing common neurosurgical pathology. |
| Students will familiarize themselves with radiographic presentations of neuroanatomy and common neurosurgical pathology. |
| Students will become acquainted with emerging and innovative research and technologies in neurosurgery. |
| Students will demonstrate their understanding of common neurosurgical topics in the form of 15-minute presentations and receive feedback. |
| Students will become acquainted with surgeons and surgical practice. |
Figure 1.
One week virtual neurosurgery clerkship schedule.
Feedback
At the time of writing this letter, it is unclear when students across the nation will be able to reenter the clinical environment. Thus this course will be offered several more times within the coming months to students in the Class of 2022. Because the turnaround time from conception to the first lecture was 3 weeks, it was crucial to solicit feedback from the medical students to improve future iterations. To that end, students were asked to fill out pre- and posttests and feedback surveys that facilitated assessment of fund of knowledge improvements, changes in student perceptions of the neurosurgical field, and suggestions for curriculum refinement.
Initial positive feedback of our curriculum included appreciation of fundamental concept review, exposure to emerging technologies and research, the quality of student engagement over the video conferencing software, and opportunities to interface with faculty in a small group setting (Table 2). Points for improvement included creating a defined role for medical students in the telemedicine experience, additional early neuroanatomy review in a clinical context, stricter timing for the delivered lectures, and additional surgical video content.
Table 2.
Summary of Feedback Received after First Week of Neurosurgery Elective
| Points of Positive Feedback | Points of Negative Feedback |
|---|---|
|
|
GCS, Glasgow Coma Scale.
Conclusions
“He who studies medicine without books sails an uncharted sea, but he who studies medicine without patients does not go to sea at all.” As Dr. William Osler most famously stated, a virtual neurosurgery elective will never take the place of seeing and touching the patient, as well as being present in the operating room. However, the current pandemic will assuredly see an end, and the lessons learned may inform changes to clinical educational well beyond the era of social distancing. Furthermore, if there were to be a resurgence of the current pandemic in the coming months or a different crisis in the coming years, this curriculum may be relied on to quickly transition to a virtual learning environment with minimal disruptions. It is anticipated that many industries will opt to incorporate video conferencing, remote learning, and other techniques into standard practice going forward. Similarly, it is possible that medical training will be forever changed based on the experiences of these few months. The benefits of in-person versus online didactic lectures have been arenas of debate long before this pandemic and may be pushed to a conclusion.20 , 21 The convenience provided by virtual conferencing may save transit time for countless faculty, students, and residents, and the ability for students to join faculty via telemedicine clinic may enable more consistent interaction between the 2. Already at our institution, we are exploring the possibility of beginning a longitudinal, once-weekly virtual neurosurgery lecture series for interested students to partake in outside of the established medical school curriculum. Although countless doors have temporarily been shut because of the COVID-19 pandemic, it is clear that unforeseen new ones have been opened.
CRediT authorship contribution statement
Reem A. Dawoud: Conceptualization, Methodology, Writing - original draft. Brandon Philbrick: Conceptualization, Methodology, Writing - original draft. J. Tanner McMahon: Conceptualization, Methodology, Writing - original draft. J. Miller Douglas: Conceptualization, Methodology, Writing - original draft. Neil Bhatia: Methodology. Razan Faraj: Methodology. Alex Greven: Methodology. Bryan Buster: Methodology, Writing - review & editing. Rima S. Rindler: Methodology, Writing - review & editing. Nealen G. Laxpati: Methodology. Matthew F. Gary: Conceptualization, Methodology, Writing - review & editing.
Acknowledgments
The authors acknowledge the efforts of Dr. Cory Adamson, M.D., Ph.D., Dr. Wendy Wright, M.D., Dr. Ryan Peterson, M.D., Dr. Kimberly Hoang, M.D., Dr. Brian Howard, M.D., Dr. Jonathan Grossberg, M.D., Dr. Nicholas Boulis, M.D., Dr. Kunal Gupta, M.D., Ph.D., and Dr. Robert Gross, M.D., Ph.D.
Footnotes
Reem A. Dawoud and Brandon Philbrick contributed equally to this work.
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Centers for Disease Control and Prevention Cases in U.S. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html Available at: Published April 26, 2020.
- 2.Fong M.W., Gao H., Wong J.Y. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings—social distancing measures. Emerg Infect Dis. 2020;26:976–984. doi: 10.3201/eid2605.190995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whelan A., Prescott J., Young G., Catanese V., McKinney R. 2020. Guidance on medical students’ participation in direct patient contact activities.https://www.aamc.org/news-insights/press-releases/covid-19-updated-guidance-medical-students-roles-direct-patient-care Available at: Accessed April 28, 2020. [Google Scholar]
- 4.Lewis C.T., Zeineddine H.A., Esquenazi Y. Challenges of neurosurgery education during the coronavirus disease 2019 (COVID-19) pandemic: a U.S. perspective. https://doi.org/10.1016/j.wneu.2020.04.179 [e-pub ahead of print]. World Neurosurg. accessed April 28, 2020. [DOI] [PMC free article] [PubMed]
- 5.Almarzooq Z., Lopes M., Kochar A. Virtual learning during the COVID-19 pandemic: a disruptive technology in graduate medical education. https://doi.org/10.1016/j.jacc.2020.04.015 [e-pub ahead of print]. J Am Coll Cardiol. accessed April 28, 2020. [DOI] [PMC free article] [PubMed]
- 6.Gilmartin-Thomas J.F.M., Duncan G. Educating students about dementia with virtual learning experiences. Am J Health Syst Pharm. 2017;74:956–957. doi: 10.2146/ajhp170094. [DOI] [PubMed] [Google Scholar]
- 7.Mcintyre T.P., Monahan T.S., Villegas L., Doyle J., Jones D.B. Teleconferencing surgery enhances effective communication and enriches medical education. Surg Laparosc Endosc Percutan Tech. 2008;18:45–48. doi: 10.1097/SLE.0b013e31815746a8. [DOI] [PubMed] [Google Scholar]
- 8.Konakondla S., Fong R., Schirmer C.M. Simulation training in neurosurgery: advances in education and practice. Adv Med Educ Pract. 2017;8:465–473. doi: 10.2147/AMEP.S113565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kirkman M.A., Ahmed M., Albert A.F., Wilson M.H., Nandi D., Sevdalis N. The use of simulation in neurosurgical education and training. J Neurosurg. 2014;121:228–246. doi: 10.3171/2014.5.JNS131766. [DOI] [PubMed] [Google Scholar]
- 10.Breining G. Future or fad? Virtual reality in medical education. Association of American Medical Colleges. August 2018. https://www.aamc.org/news-insights/future-or-fad-virtual-reality-medical-education Available at:
- 11.Alaraj A., Lemole M., Finkle J. Virtual reality training in neurosurgery: review of current status and future applications. Surg Neurol Int. 2011;2:52. doi: 10.4103/2152-7806.80117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shao X., Yuan Q., Qian D. Virtual reality technology for teaching neurosurgery of skull base tumor. BMC Med Ed. 2020;20:3. doi: 10.1186/s12909-019-1911-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weiner S. No classrooms, no clinics: medical education during a pandemic. Association of American Medical Colleges. April 2020. https://www.aamc.org/news-insights/no-classrooms-no-clinics-medical-education-during-pandemic Available at:
- 14.Congress of Neurological Surgeons Online Grand rounds Complimentary online education. https://www.cns.org/onlineed Available at:
- 15.Thomas P., Kern D., Hughes M., Chen B. Curriculum Development for Medical Education: A Six-Step Approach. Johns Hopkins University Press. 2016. Overview: a six-step approach to curriculum development; pp. 4–7.https://jhu.pure.elsevier.com/en/publications/curriculum-development-for-medical-education-a-six-step-approach Available at: Accessed April 28, 2020. [Google Scholar]
- 16.Zoom for Healthcare. Zoom. https://zoom.us/healthcare Available at:
- 17.Barrow D.L., Bendok B.R. Essential neurosurgery for medical students. Oper Neurosurg. 2019;17(suppl 2):S1–S255. doi: 10.1093/ons/opz071. [DOI] [PubMed] [Google Scholar]
- 18.Emory University School of Medicine Graduation requirements for the MD degree. https://med.emory.edu/education/programs/md/student-handbook/academics/graduation-requirements.html Available at:
- 19.Zuckerman S.L., Mistry A.M., Hanif R. Neurosurgery elective for preclinical medical students: early exposure and changing attitudes. World Neurosurg. 2016;86:120–126. doi: 10.1016/j.wneu.2015.08.081. [DOI] [PubMed] [Google Scholar]
- 20.Gupta A., Saks N.S. Exploring medical student decisions regarding attending live lectures and using recorded lectures. Med Teach. 2013;35:767–771. doi: 10.3109/0142159X.2013.801940. [DOI] [PubMed] [Google Scholar]
- 21.Kauffman C.A., Derazin M., Asmar A., Kibble J.D. Relationship between classroom attendance and examination performance in a second-year medical pathophysiology class. Adv Physiol Educ. 2018;42:593–598. doi: 10.1152/advan.00123.2018. [DOI] [PubMed] [Google Scholar]