Abstract
With emerging interest in the use of telemedicine, allergy-immunology should be at the forefront of adoption and implementation of these services. Patients report a greater desire for telemedicine services as well as satisfaction with video-based visits with their providers. Interim virtual visits can accommodate overscheduled clinics, reduce burdens of travel to distant sites, improve access to subspecialty care, and increase adherence during monitoring of chronic allergic conditions. The outpatient nature of allergy-immunology coupled with the ease of conducting many aspects of a routine visit via telemedicine makes the incorporation of telehealth training into fellowship programs highly desirable. The short-term closure of hospital-affiliated clinics, in particular, for vulnerable or immunodeficient patients, in the setting of a global pandemic demonstrates the timeliness of this topic.
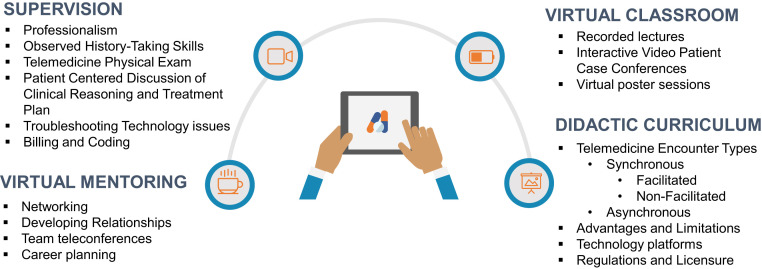
A framework for implementing telemedicine into the allergy-immunology curriculum, training faculty on appropriate supervision, providing elective clinical experience in the form of continuity clinics, and simulating telemedicine delivery is discussed. Proposed telemedicine competencies desired for the independent practice of telemedicine are suggested.
Key words: Telemedicine, Fellowship, Trainee, Education, Virtual Classroom, Mentoring
Abbreviations used: AAAAI, American Academy of Allergy, Asthma, and Immunology; ACGME, Accreditation Council for Graduate Medical Education
Telemedicine has recently been highlighted as a medium of health care delivery that can improve patient-physician interactions, access to care1 as well as increase patient adherence and cost savings. Telemedicine services have been shown to be effective for improvement in asthma care and quality of life.2 Publications and engagement with telehealth and telemedicine services in allergy-immunology have increased since 2015; however, the recent public health emergency has brought telemedicine usage into the forefront quicker than prior attempts to incorporate this technology into the practice environment. Importantly, institutions with allergy-immunology training programs have quickly implemented telemedicine programs to provide both continuity of care for existing patients and an opportunity for trainees in a changing educational environment. The outpatient nature of the specialty and the recent precipitous decline in allergy-immunology specific patient volume emphasizes the importance of considering virtual training and telemedicine as core aspects of preparing future allergist-immunologists for clinical practice.
Incorporation of Telemedicine into Fellowship Training Programs
Recently, 2 publications in The Journal of Allergy and Clinical Immunology: In Practice addressed incorporation of telemedicine into practice3 and triaging of patients to virtual visits.4 Another consideration in addition to practical concerns includes the use of this technology for continuity of training. Although there is a general desire to incorporate telemedicine training into medical school curricula,5 at present, the Accreditation Council for Graduate Medical Education (ACGME) does not mention this as a core program requirement.6 Telemedicine training is not mentioned in the Allergy Immunology Milestones 2.0 planned for July 2020; however, the systems-based practice, professionalism, and communication skill subparts are well poised for evaluation using supervised telemedicine. In light of the projected duration of the COVID-19 pandemic, ACGME-accredited programs should foresee the need to incorporate telemedicine into training, both in direct patient care and in the virtual classroom. A framework for the incorporation of teletraining into allergy-immunology training programs is shown in Figure 1 .
Figure 1.
A framework for incorporation of teletraining into allergy-immunology training programs.
Telemedicine didactic training content
As telemedicine has not yet been incorporated into mainstream medical school and residency education, trainees will need an initial didactic curriculum before embarking on their first telemedicine encounter.
Trainees should be educated in the underlying telemedicine technology to ensure that they are compliant with appropriate security and technology considerations. Trainees should be aware of various platforms for videoconferencing and telemedicine services7 as well as issues related to Health Insurance Portability and Accountability Act compliance, encryption of data during transmission, and the need for auditing in their technology platform. Desktop computers, laptops, and mobile devices such as tablets or smartphones may be used for telemedicine visits. The capabilities of these products and their applications with the different options and IT support should be discussed. The use of screenshots and video and/or audio recording should be strictly prohibited unless there is informed consent from the patient for teaching or research purposes.
Trainees will require education on patient privacy, particularly if they are engaging in telemedicine encounters from their homes. The trainee should ensure that they are the only person working from the device and that the device has proper protection, such as a screen protector to prevent content from being viewed by a passer-by. The telemedicine visits should be conducted in a private room. Listening devices, such as the Amazon Echo or Google Home, should be removed or turned off, and the trainees should wear headphones if conducting the visit from home as there is a risk of the patient being overheard. In addition, the trainees should be educated on how to initiate privacy discussions regarding their own and the patient's environment. Trainees should be educated concerning the need for end-to-end encryption of all data and messages that are transmitted.
Studies have shown that there is a lack of understanding of the laws governing telemedicine amongst trainees.8 In response to the COVID-19 pandemic, regulatory bodies have relaxed previous requirements for a pre-existing patient-physician relationship for engaging in telemedicine services.9 Individual states have temporarily relaxed state requirements for licensure, both for telemedicine and direct practice.10 Changes to telemedicine enacted by the Centers for Medicare and Medicaid Services during the COVID-19 Public Health Emergency as of May 6, 2020, are shown in Table I ; however, rules and waivers continue to evolve in a changing practice environment. An understanding of contemporary rules and regulatory requirements, as well as the ability to locate key resources to track evolving federal and state rules and regulations for training fellows in operational considerations, is important. Some key resources are shown in Table II . As laws that govern interstate medical licensing evolve, new opportunities will arise to provide additional training opportunities and experiences for trainees.
Table I.
Regulatory changes to telemedicine during the COVID-19 public health emergency enacted by the Centers for Medicare and Medicaid Services (CMS)
| Telehealth services defined under the Social Security Act Sec. 1834(m) | Waiver under the Telehealth Services During Certain Emergency Periods Act of 202011 | |
|---|---|---|
| State licensing requirements | In 49 states and the District of Columbia, providers can only treat patients in states where they are licensed | The Department of Health and Human Services (HHS) has waived certain federal licensing requirements, providers must adhere to state licensing regulations |
| Many states have announced waivers of licensure requirements via interstate reciprocity | ||
| Geographic area | The patient must be present at an originating site located in either a rural health professional shortage area or county outside a metropolitan statistical area | Geographic requirements have been waived so beneficiaries in both urban and rural areas can use telemedicine |
| Originating site | Physician/practitioner offices, hospitals, critical access hospitals, rural health clinics, federally qualified health centers, renal dialysis facilities, skilled nursing facilities, mental health centers, homes of beneficiaries with end-stage renal disease, mobile stroke units | All originating site requirements have been waived by CMS |
| Patient's homes have been deemed an eligible originating site | ||
| Hospitals can bill an originating site fee even though patients are at home | ||
| Distant site practitioners | Physicians, physician assistants, nurse practitioners, nurse-midwives, clinical nurse specialists, certified registered nurse anesthetists, clinical psychologists, clinical social workers, registered dieticians | No change |
| Modality | Interactive audio and video telecommunications system that permits 2-way, real-time communication | HHS will exercise discretion in enforcement of HIPAA violations and penalties against health care professionals who serve patients in good faith through non-HIPAA compliant technologies such as Skype or FaceTime |
| Audio-only consults are permitted | ||
| Providers do not need to list home address on Medicare enrollment while continuing to bill from their enrolled location | ||
| Pre-existing relationship | Per CMS, providers could only see patients with whom they had an established relationship (claims history in the prior 3 y) | The Coronavirus Aid, Relief, and Economic Security Act (enacted on March 27, 2020) eliminated the requirement for a pre-existing established relationship |
HIPAA, Health Insurance Portability and Accountability Act.
Table II.
Key resources for training fellows on telemedicine rules, regulations, reimbursement, and practice
| Resource | Description | Reference |
|---|---|---|
| Federation of State Medical Boards Telemedicine (FSMB) | FSMB's site promoting best practices, policies, advocacy, and other resources for key issues related to telemedicine policy | 12 |
| American Telehealth Association (COVID-19 Microsite) | Nonprofit association focused on transforming health care through adoption of telemedicine | 13 |
| Centers for Medicare and Medicaid Services (CMS) | CMS description of covered telehealth codes; State Medicaid, CHIP and CMS factsheets, and toolkits | 11,14, 15, 16 |
| Center for Connected Health Policy | A nonprofit organization that tracks telehealth policy regulations and changes to state regulations | 17 |
| American Academy of Allergy Asthma & Immunology | Resources for clinicians on allergy-immunology relevant changes to telemedicine | 18 |
| American Medical Association (AMA) | AMA quick guide to telemedicine in practice | 19 |
The initial didactic curriculum should ensure that trainees are able to recognize the different types of telemedicine encounters available, synchronous and asynchronous, with the advantages and limitations of each.
Synchronous
Synchronous visits are real-time video conferences between the physician, trainee, and the patient in a medical consultation similar to the in-person setting. As these can be either facilitated or nonfacilitated visits, trainees must be adept in both types of encounters and which is preferred for particular circumstances. Telephone visits, without video capabilities, can be used if the patient does not have access to video equipment; however, this may provide greater limitations on the telehealth visit.
Nonfacilitated visits
Nonfacilitated visits occur between the physician, patient, and trainee directly in real time. History taking and discussion of the patient's assessment and treatment plan should mirror a traditional, in-clinic appointment. As there are no specialized health care personnel with the patient at home, the physical examination is more limited; however, trainees can be instructed on aspects of the allergy-immunology physical examination that can be assessed by telemedicine20 with the patient's cooperation using resources created by the American Academy of Allergy, Asthma, and Immunology (AAAAI). For example, patients can be instructed on how to take their own vital signs using home thermometers and blood pressure cuffs as well as directed on positioning for a video examination of their oropharynx or skin. There are limitations to a physical examination by telemedicine, particularly in the ability to visualize the nasal cavity and auscultate the lungs, of which trainees need to be aware. Future considerations for select patients may include procurement of low-cost home-monitoring equipment, digital stethoscopes, spirometry tools, or mobile health apps that may assist in chronic disease management. For most patients, using existing cameras on mobile devices for routine physical examinations will likely be sufficient.
In addition, trainees will need direction on how to convey empathy and foster the therapeutic alliance between physicians and patients in the digital medium. Trainees may find that telemedicine lends itself to multitasking more than in-person visits as the electronic medical record is directly available to review medical records and write orders efficiently. Similar to in-person etiquette, attempts to reduce distraction for clear communication are needed. The trainees should indicate when they are placing orders or reviewing the chart so that patients feel assured that the physician's attention is directed toward their care.
Nonfacilitated visits may be best suited for in situations where a full physical examination is not necessary for appropriate patient management. Discussion of laboratory results, review of asthma medication adherence, or triage of acute issues would be examples of appropriate nonfacilitated visits. Trainees need to be instructed on instances when a patient should be evaluated in-person whether during an initial visit or for follow-up purposes.
Facilitated visits
Facilitated visits occur at a site distant to the allergist, but with the assistance of a health care professional. In these visits, the patient travels to a nearby clinical space and has a remote visit with the allergist, whereas a facilitator, often a registered nurse or other practitioner who may have obtained a telehealth facilitator certificate, performs the physical examination. Specialized equipment, such as a digital otoscope or stethoscope, transmits physical examination information to the telemedicine physician in real time for a more extensive examination than is possible with nonfacilitated visits. Trainees will need to learn how to direct a physical examination in a facilitated visit as well as troubleshoot technical issues with the equipment in real time. Trainees will need to develop a relationship with the facilitator as an integral member of the care team. Facilitated visits can be used for new patient visits, which require a full physical examination, or follow-up visits.
Asynchronous
The use of asynchronous telemedicine technology via store and forward or remote patient monitoring can be useful in both training and patient care.21
Store and forward
Store and forward telemedicine involves electronic storage of medical information obtained from a patient or medical service for forwarding to a health care provider or used between health care professionals for interpretation.
Store and forward telemedicine can be used to train fellows on dermatologic conditions. For consultation regarding skin rashes or lesions, the patient can take a photograph of the area of concern and send it to the allergy-immunology fellow for evaluation. Similar to telemedicine training for dermatology residents,22 allergy-immunology trainees can initially independently evaluate the skin condition to create a differential diagnosis and treatment plan based on the appearance and then confer with the attending physician, or even a consulting dermatologist, for further education in the management of skin conditions. Spirometry performed by mobile device apps can also be transmitted to physicians before telemedicine appointments. Trainees can learn how to coach patients through an in-home spirometry as well as give direction on how to perform a bronchodilator response remotely. Subsequently, fellows can review their interpretation of the spirometry with their attending for diagnostic verification and consolidation of clinical reasoning in the virtual encounter as they would in-person.
Remote patient monitoring
Remote patient monitoring captures and records patient physiologic data outside of the clinic or hospital setting. These data are transmitted to health care providers for review, diagnosis, and clinical management. A clinical trial of remote patient monitoring of asthma demonstrated improved asthma control and lung function with the use of remote peak flow and symptom monitoring.23 Sensors that attach to the patient's inhalers can serve as monitoring for asthma medication adherence. Trainees should be educated on the interpretation of remote patient monitoring data and how to incorporate it into their patient care and education. Telemedicine training of fellows will require continual adaptation to involve emerging technologies such as mHealth applications and digital therapeutics.
Electronic consultations and messages
Electronic consultations (e-consults) make use of communication within the electronic health record to provide recommendations from a specialist to a patient's primary care doctor or other treating specialist. E-consults can be used efficiently, particularly for historical adverse drug reactions and immunodeficiency consultations, in an expedited manner streamlining timely access to necessary care from specialists.24 Trainees should be educated on performing e-consults for ordering testing in advance of a visit, planning skin testing, or oral challenge testing in a subsequent visit, second opinions, and appropriately guiding a referring provider on interim management before evaluation in a telemedicine or in-person allergy-immunology visit. Trainees should be given the opportunity to respond to e-consults, initially with substantial attending oversight and then with growing independence. As e-consults can reduce unnecessary overutilization of health care services, trainees should be well versed in how to incorporate these encounters into their future practice.
Electronic messages from patients can also serve as training tools for common allergy-immunology questions. Patient queries can give trainees the opportunity to carefully consider responses to key practice questions and review the evidence-base for decision making without the immediacy required during a scheduled visit. Practice with electronic message management during fellowship training can aid trainees in efficient time management for their future clinical practice.
Supervision of telemedicine visits
The COVID-19 pandemic has brought telemedicine and telehealth services to the forefront of health care.4 Many practices are struggling to adapt to these changes, and training programs face the challenge of educating trainees in a virtual environment and creating instructional modules to train supervisors in the use of telemedicine and telehealth systems. The AAAAI and the American College of Allergy, Asthma, and Immunology have shared resources and guides for practices to assist them through this transition period.18 It is beneficial for attendings to familiarize themselves with telemedicine tools so they can better instruct their trainees on how to use them.
Whether in-person or via telemedicine, the history and physical examination remain the core of the patient visit. Telemedicine offers the unique opportunity to supervise trainees from the medical student to the fellow level. Most trainees will not have their own telemedicine account and will rely on their supervising attending's access to the telemedicine platform. The attending physician or clinic staff can schedule the appointment and inquire if the patient (and the parent and/or guardian, if appropriate) would be agreeable to having a trainee join their session in advance, or seek permission for the trainee to participate in the telemedicine visit at the start of the visit with the trainee on a group video chat. Once consent has been obtained, the encounter can proceed.
Although the appointment format may appear different, the same etiquette rules govern each encounter. Trainees are expected to wear appropriate attire and maintain the same level of professionalism throughout the meeting as they would for an in-person visit. Each encounter must begin with introductions and consent, from either the patient or parent and/or guardian in the case of a child who has not reached the age of consent, to continue with the appointment should be obtained. For pediatric patient, discussion of optimal camera positioning with both the child and adult may be necessary. Throughout the visit, eye contact should be maintained with the patient and their parents and/or guardians when appropriate. The interview should be conducted in the same manner as an in-person encounter. The AAAAI has published resources on how to conduct a professional telemedicine visit that can be used by trainees.25
During their first few sessions, the trainees may benefit from observing the attendings while they conduct the interview and physical examination, but may be able to initiate and lead subsequent patient encounters. Although the patient is not physically present, a physical examination can and should be performed. There is a lot of information that can be obtained from observing the patient, such as his or her general appearance, orientation, respiratory effort, movement, and affect. Parents can be taught to perform specific portions of the examination, such as the abdominal examination, on their children. Certain elements, such as rashes, can be determined on a case by case basis depending on the quality of the equipment used to conduct the examination. If necessary, a trainee can state “deferred” or “recommend in-office evaluation.”
One of the more challenging aspects of supervising a telemedicine visit is to promote clinical reasoning, elicit a differential diagnosis, and discuss the care plan while in front of the patient. In a conventional encounter, the trainee would conduct the history and physical examination, and then leave the room to discuss the case with his or her attending. Some telemedicine platforms allow providers to place their patients in waiting rooms, which can be done while the case is discussed with the trainee. Alternatively, the encounter can be closed, and the patient can be called back once the plan is formulated. A preferred method that would enhance the learning process is to permit the trainee to summarize and formulate his or her plan with the patient still in the visit. The attending can either agree or explain why an alternative plan might be more appropriate. Faculty can use this opportunity to detail their clinical reasoning to the patient to enhance the understanding of the treatment plan. Faculty consistently report evaluation fatigue; however, telemedicine is appropriate for direct “bedside rounds” and performance evaluation by nature of the technology.
At the end of each encounter, the trainee should recap the visit by verifying the patient's pharmacy, review the treatment plan, discuss any follow-up, and perform education as needed. Proper telemedicine etiquette would be to invite the patient to end the visit first to ensure that the trainee has finished discussing the patient's concerns. Once the visit is concluded, the trainee can complete the documentation within the guidelines of his or her health care system. Although the core elements of a patient's note do not change, many health care systems have their own modifications to acknowledge that the visit was conducted through telemedicine. In particular, the trainee should document the modality of telemedicine that was employed, who was present during the visit, the location of the patient and the physician, any technical interruptions, and the attending physician should document his or her presence and supervision during key portions of the encounter. The same responsibilities as he or she has for in-person visits apply to these encounters, including following up on laboratory results and diagnostic studies and contacting any primary care/specialty offices. The same billing and coding requirements that apply to traditional in-office visits apply to telemedicine, with the exception of state-specific modifiers.
A case review should be conducted after each visit for training purposes. The teaching standards and scope of practice should be consistent with existing in-person sessions. In addition, patients can provide near real-time feedback after the visits with a brief survey or comments. Digital patient feedback may be reviewed with trainees to provide additional training on practice-based learning and professionalism. Before incorporating trainees into the clinic, it would be advisable to perform training simulations so that they can understand the benefits, limitations, and scope of telemedicine and telehealth visits. Adequate supervision can easily be maintained as trainees are directly observed while conducting their telemedicine visits. It is the duty of the supervising attending to provide feedback to trainees so that they can learn from each encounter. Trainees should become proficient in telemedicine core competencies, as detailed in Table III .
Table III.
Proposed allergy-immunology telemedicine core competencies
| Competency domain | Allergy and immunology telemedicine related competencies | Examples |
|---|---|---|
| Medical knowledge | Recognizes limitations of telemedicine | Recognizes types of visits, examination, counseling, and treatment that can occur via telemedicine |
| Patient care | Elicits appropriate history and remote targeted physical examination | Demonstrates the ability to instruct patients on performing a remote physical examination |
| Performs an allergy home visit | Assesses allergic environment, medications, and inhaler/device technique | |
| Practice-based learning and improvement | Evaluates gaps in performance while conducting visits for telemedicine; seeks feedback and simulated patients for improvement | Modifies telemedicine practice based on feedback from simulated and supervised patient encounters |
| Interpersonal communication skills | Communicates effectively with the patient and other participants on the telemedicine visits | Engages family members (guardians, other caregivers) via telemedicine; communicates with home health infusion services for biologic treatments |
| Professionalism | Conducts web presence in a professional manner | Ensures that lighting, appearance, and surroundings are appropriate |
| Ensures that appropriate type of telemedicine encounter is used; assures that all aspects of encounter are captured and documented | Obtains consent, timely record keeping, assuring appointment times, and virtual waiting rooms are appropriately monitored | |
| Systems-based practice | Advocates for appropriate use of telemedicine | Assures that appropriate patients are selected for use of telemedicine services |
| Understands licensing, billing, and legal considerations while using telemedicine | Analyzes barriers to telemedicine implementation |
Limitations of training using telemedicine
It is important to understand the limitations and barriers of telemedicine that apply to both trainees and their patients. Many new trainees feel unprepared to use telemedicine effectively.8 There are portions of the physical examination that cannot be performed virtually, and the patient may still have to travel to obtain labs and other diagnostic studies. Consideration should be given to the socioeconomic status and the resources patients have, such as internet service, video and audio equipment, and language or visual difficulties3 as these may be barriers to utilization. Patients may be distrustful of telemedicine, and some patients may have difficulty in adopting telemedicine services.26 Some barriers can be overcome by educating patients about the benefits and safety of telemedicine, and by providing them with step by step instructions on how to access it. As rules and regulations surrounding the delivery of telemedicine services change, the cost barriers to accessing telemedicine are likely to be reduced. Many hospital systems already have telephone interpreter or facilitator services to assist in language translation. These services can be incorporated into a patient visit and used to accommodate the hearing and visually impaired. Trainees should be educated on how to accommodate these requests and seek guidance from their attending physician.
Telemedicine or in-person visits may be used to establish care. In-person visits may be preferable if a physical examination or procedure is necessary to render a correct diagnosis, such as examination of the nasal cavity for polyps or spirometry for a new diagnosis of asthma. Fellows must be trained to identify situations that require an in-person evaluation even if the patient would prefer a telemedicine visit. For example, specific IgE testing for allergic conditions could be performed either in anticipation of, or after a telemedicine encounter, and can be reviewed virtually, whereas allergy skin testing may be needed for certain conditions such as penicillin allergy. In contrast, pulmonary function tests, exhaled nitric oxide, and patch testing can only be performed during in-person clinic visits. Discussions about food and drug allergy may be appropriate for a telemedicine visit, but skin testing and oral or graded-dose challenges must be performed in a setting with an attending physician personally supervising the procedure due to the risk of anaphylaxis. Facilitated telemedicine visits with a non-physician health care professional would not be appropriate for procedures that carry a risk of anaphylaxis. Although it would not be appropriate for trainees to supervise nurse practitioners or physician assistants directly, trainees could participate in facilitated interactions whereby the attending allergy-immunology specialist is overseeing a low-risk procedure with a nurse practitioner or physician assistant for education purposes.27 Situations that would not be appropriate for continued monitoring via telemedicine include new or worsening symptoms despite initial treatment. Evaluation of certain allergic conditions such as assessment of nasal polyps, rhinoscopy, and evaluation of tympanic membranes is not possible via telemedicine. Other scenarios where the physical examination may change the course of disease management such as a detailed skin or genital examination in the setting of primary immunodeficiency, pulmonary examination, or evaluation of new lymphadenopathy or hepatosplenomegaly in hypereosinophilic syndromes would be better suited for an in-person visit.
Training in telemedicine can confer a significant educational benefit to allergy-immunology fellows. Before their initial telemedicine encounter with patients, they should be given the opportunity to practice with standardized patients to gain familiarity with telemedicine and to build confidence in their skills. Simulated standardized telemedicine encounters at the end of the training, even as a graduation requirement, give program faculty the opportunity to observe and assess how well a trainee can make appropriate treatment decisions in real time as a factor in readiness for independent practice. As telemedicine visits are likely to be a component of ongoing allergy-immunology clinical practice, we would offer our trainees a significant advantage in training them in the proper execution of both direct-to-consumer and facilitated visits as well as the use of asynchronous telemedicine technology during their fellowship.
Virtual classroom
Until recently, the majority of didactics in allergy-immunology programs employed in-person, content-based learning for didactic lessons for trainees. Advancements in adult learning methods have blossomed with approaches such as the flipped classroom, which blends online instruction, traditional homework, and experiential learning, where students learn through reflections on their experiences.28 , 29 Virtual learning approaches are on the rise in the allergy-immunology community with recorded lectures, webinars, podcasts, and other national resources. Despite these offerings, implementation of virtual learning experiences into allergy-immunology fellowship programs has been slow as most graduate medical education programs continue to employ “community of practice” models in a small or large group classroom-type setting. In March 2020, the emergence of the COVID-19 pandemic caused a sudden need to shift training to the virtual classroom. In-training examinations were moved to remote monitored examinations, and programs reported moving didactics such as journal clubs to virtual classrooms.30 Enduring e-learning instructional content can be created that can be widely shared. One can imagine the virtual classroom toppling institutional silos and bringing greater access to unique training opportunities across the nation. Examples include the American College of Allergy, Asthma & Immunology/Conferences On-Line Allergy lectures31 shared on YouTube and regional videocast conferences in the DC-Maryland-Virginia area for complex immunodeficiency cases seen in Primary Immunodeficiency Clinic as models for collaborative educational endeavors. The move to virtual education may facilitate increased interaction, draw on unique strengths of individual training programs, and can create a nationwide community of allergy-immunology learners.
Virtual methods can easily recapitulate standard teaching methods such as presenting virtual patient cases, simulation-based learning, and conducting case conferences via videoconference. Trainees can even stand in front of a “virtual poster” via technology platforms with screen-sharing ability to present their research. Available technology allows for new avenues of collaboration such as the use of team-based applications for collaborative writing assignments, curriculum development, and clinical trial or grant writing exercises.
Finally, virtual communication can enhance team mentoring for allergy-immunology trainees. The traditional, single mentee to single mentor pairing is slowly being replaced by team-mentoring approaches that give trainees greater access to a more diverse mentoring experience. A move to the virtual environment may facilitate greater networking opportunities via social media networks or facilitative networking across institutions via videoconferencing initiated by program directors to meet trainee career objectives.
Conclusions
Telemedicine represents an unprecedented opportunity to teach and evaluate the clinical skills of trainees. At the beginning of their fellowship, trainees should participate in simulation telemedicine cases to introduce the technology, stereotypic allergy-immunology case scenarios and to model appropriate virtual etiquette. At the completion of their training, supervising faculty can use telemedicine encounters to directly assess trainees' clinical reasoning, professionalism, and communication skills and assure a more precise assessment of the core competencies with direct observation using telemedicine.
Footnotes
This study was funded in part by Division of Intramural Research (DIR), National Institute of Allergy and Infectious Diseases, National Institutes of Health.
Conflicts of interest: The authors declare that they have no conflicts of interest.
References
- 1.Elliott T., Shih J., Dinakar C., Portnoy J., Fineman S. American college of allergy, asthma & immunology position paper on the use of telemedicine for allergists. Ann Allergy Asthma Immunol. 2017;119:512–517. doi: 10.1016/j.anai.2017.09.052. [DOI] [PubMed] [Google Scholar]
- 2.Chongmelaxme B., Lee S., Dhippayom T., Saokaew S., Chaiyakunapruk N., Dilokthornsakul P. The effects of telemedicine on asthma control and patients’ quality of life in adults: a systematic review and meta-analysis. J Allergy Clin Immunol Pract. 2019;7:199–216.e11. doi: 10.1016/j.jaip.2018.07.015. [DOI] [PubMed] [Google Scholar]
- 3.Portnoy J., Waller M., Elliott T. Telemedicine in the era of COVID-19. J Allergy Clin Immunol Pract. 2020;8:1489–1491. doi: 10.1016/j.jaip.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shaker M.S., Oppenheimer J., Grayson M., Stukus D., Hartog N., Hsieh E.W.Y. COVID-19: pandemic contingency planning for the allergy and immunology clinic. J Allergy Clin Immunol Pract. 2020;8:1477–1488.e5. doi: 10.1016/j.jaip.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Triola M.M., Friedman E., Cimino C., Geyer E.M., Wiederhorn J., Mainiero C. Health information technology and the medical school curriculum. Am J Manag Care. 2010;16(Suppl HIT):SP54–S56. [PubMed] [Google Scholar]
- 6.Accreditation Council for Graduate Medical Education ACGME program requirements for graduate medical education in allergy and immunology. 2020. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/020_AllergyImmunology_2020.pdf?ver=2020-02-25-140036-943 Available from:
- 7.Baker J., Stanley A. Telemedicine technology: a review of services, equipment, and other aspects. Curr Allergy Asthma Rep. 2018;18:60. doi: 10.1007/s11882-018-0814-6. [DOI] [PubMed] [Google Scholar]
- 8.Waseh S., Dicker A.P. Telemedicine training in undergraduate medical education: mixed-methods review. JMIR Med Educ. 2019;5:e12515. doi: 10.2196/12515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Center for Medicare and Medicaid Services CMS.gov Newsroom. Additional background: sweeping regulatory changes to help U.S. healthcare system address COVID-19 patient surge. 2020. https://www.cms.gov/newsroom/fact-sheets/additional-backgroundsweeping-regulatory-changes-help-us-healthcare-system-address-covid-19-patient Available from:
- 10.New York State Education Department COVID-19 pandemic and professional practice. 2020. http://www.op.nysed.gov/COVID-19_EO.html Available from:
- 11.Centers for Medicare & Medicaid Services Medicare telemedicine health care provider fact sheet. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet Available from:
- 12.Federation of State Medical Boards Telemedicine key issues and policy. https://www.fsmb.org/advocacy/telemedicine/ Available from:
- 13.American Telemedicine Association COVID-19. https://www.americantelemed.org/covid-19/ Available from:
- 14.Centers for Medicare & Medicaid Services List of telehealth services. https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes Available from:
- 15.Centers for Medicare & Medicaid Services, Medicare Learning Network Telehealth services. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/TelehealthSrvcsfctsht.pdf Available from:
- 16.Centers for Medicare & Medicaid Services State medicaid & CHIP telehealth toolkit: policy considerations for states expanding use of telehealth: COVID-19 version. https://www.medicaid.gov/medicaid/benefits/downloads/medicaid-chip-telehealth-toolkit.pdf Available from:
- 17.Center for Connected Health Policy. Search telehealth resources. https://www.cchpca.org/resources/search-telehealth-resources Available from:
- 18.American Academy of Allergy Asthma & Immunology Utilize telemedicine. 2020. https://education.aaaai.org/resources-for-a-i-clinicians/telemedicine_covid-19 Available from:
- 19.American Medical Association AMA quick guide to telemedicine in practice. https://www.ama-assn.org/practice-management/digital/ama-quick-guide-telemedicine-practice Available from:
- 20.Elliot T., 4AI4YOU How to conduct a physical exam via telemedicine [video]. YouTube. 2020. https://www.youtube.com/watch?v=4hRObfNyDvc&feature=youtu.be Available from:
- 21.Chan D.S., Callahan C.W., Sheets S.J., Moreno C.N., Malone F.J. An internet-based store-and-forward video home telehealth system for improving asthma outcomes in children. Am J Health Syst Pharm. 2003;60:1976–1981. doi: 10.1093/ajhp/60.19.1976. [DOI] [PubMed] [Google Scholar]
- 22.Boyers L.N., Schultz A., Baceviciene R., Blaney S., Marvi N., Dellavalle R.P. Teledermatology as an educational tool for teaching dermatology to residents and medical students. Telemed J E Health. 2015;21:312–314. doi: 10.1089/tmj.2014.0101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rasmussen L.M., Phanareth K., Nolte H., Backer V. Internet-based monitoring of asthma: a long-term, randomized clinical study of 300 asthmatic subjects. J Allergy Clin Immunol. 2005;115:1137–1142. doi: 10.1016/j.jaci.2005.03.030. [DOI] [PubMed] [Google Scholar]
- 24.Phadke N.A., Wolfson A.R., Mancini C., Fu X., Goldstein S.A., Ngo J. Electronic consultations in allergy/immunology. J Allergy Clin Immunol Pract. 2019;7:2594–2602. doi: 10.1016/j.jaip.2019.05.039. [DOI] [PubMed] [Google Scholar]
- 25.Elliot T., 4AI4YOU How to conduct a professional telemedicine visit using good webside manner [video]. YouTube. 2020. https://www.youtube.com/watch?v=8bMFL56Zflc Available from:
- 26.Almathami H.K.Y., Win K.T., Vlahu-Gjorgievska E. Barriers and facilitators that influence telemedicine-based, real-time, online consultation at patients’ homes: systematic literature review. J Med Internet Res. 2020;22:e16407. doi: 10.2196/16407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Staicu M.L., Holly A.M., Conn K.M., Ramsey A. The use of telemedicine for penicillin allergy skin testing. J Allergy Clin Immunol Pract. 2018;6:2033–2040. doi: 10.1016/j.jaip.2018.04.038. [DOI] [PubMed] [Google Scholar]
- 28.Eaton M. The flipped classroom. Clin Teach. 2017;14:301–302. doi: 10.1111/tct.12685. [DOI] [PubMed] [Google Scholar]
- 29.Yardley S., Teunissen P.W., Dornan T. Experiential learning: transforming theory into practice. Med Teach. 2012;34:161–164. doi: 10.3109/0142159X.2012.643264. [DOI] [PubMed] [Google Scholar]
- 30.Codispoti C.D., Bandi S., Moy J., Mahdavinia M. Running a virtual allergy division and training program in the time of COVID-19 pandemic. J Allergy Clin Immunol. 2020;145:1357–1359. doi: 10.1016/j.jaci.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dowling P.J., Kader R., Portnoy J.M. COLA (conferences on-line allergy) at 10 years—evolution of an online fellowship curriculum. J Allergy Clin Immunol Pract. 2019;7:2568–2573. doi: 10.1016/j.jaip.2019.06.025. [DOI] [PubMed] [Google Scholar]