Abstract
Anxiety disorders are among the most prevalent mental disorders, but the subcategory of specific phobias has not been well studied. Phobias involve both fear and avoidance. For people who have specific phobias, avoidance can reduce the constancy and severity of distress and impairment. However, these phobias are important because of their early onset and strong persistence over time. Studies indicate that the lifetime prevalence of specific phobias around the world ranges from 3% to 15%, with fears and phobias concerning heights and animals being the most common. The developmental course of phobias, which progress from fear to avoidance and then to diagnosis, suggests the possibility that interrupting the course of phobias could reduce their prevalence. Although specific phobias often begin in childhood, their incidence peaks during midlife and old age. Phobias persist for several years or even decades in 10–30% of cases, and are strongly predictive of onset of other anxiety, mood, and substance-use disorders. Their high comorbidity with other mental disorders, especially after onset of the phobia, suggests that early treatment of phobias could also alter the risk of other disorders. Exposure therapy remains the treatment of choice, although this approach might be less effective in the long term than previously believed. This Review discusses the literature regarding the prevalence, incidence, course, risk factors, and treatment of specific phobias, and presents epidemiological data from several population-based surveys.
Introduction
Anxiety disorders, which include generalised anxiety disorder, panic disorder, agoraphobia, social phobia, and specific (simple) phobias, are more prevalent in adults than are other mental disorders.1 In 1987, Marks2 reviewed the existing literature and conceptualised the study of anxiety, which led to a surge in research on the epidemiology and natural history of the subcategories of panic and agoraphobia,3–7 social phobia,8–16 and generalised anxiety disorder.17–20 However, less research has been done on the subcategory of specific phobias,21–23 which is the subject of this Review. As many people with specific phobias do not seek treatment, the epidemiological aspects of this Review concentrate on population-based data, focusing on the prevalence, incidence, and natural history of specific phobias. We also discuss research on risk factors (including genetic epidemiology) and treatment modalities for specific phobias. We systematically reviewed the epidemiological research literature on any specific phobia, and eight specific phobias were assessed on the basis of three separate population-based surveys. The aim of this Review is to introduce researchers and clinicians to this relatively under-developed field, to highlight the importance of specific phobias, and to provide some guidance regarding treatment options.
Diagnosis
The diagnosis of phobic reaction was described in two short paragraphs in the first edition of the American Psychiatric Association DSM in 1952,24 which stated that “the commonly observed forms of phobic reaction include fear of syphilis, dirt, closed places, high places, open places, animals, etc. The patient attempts to control his anxiety by avoiding the phobic object or situation.” Since then, types of phobia (including social phobias, agoraphobia, and specific phobias) have been more narrowly specified, and subtypes of specific phobias (including phobias related to blood, injections, and injury) have been expanded. The diagnosis of a specific phobia requires unreasonable fear associated with a specific object or situation, avoidance of the object or situation, persistence of the fear over time, and clinically significant distress or impairment associated with the fear, or avoidance.25 The definitions in the American and international classifications26 are similar, which is important for our discussion of worldwide results.
The requirement that the individual recognises their phobia as unreasonable indicates that the presence of insight is important, and suggests that the interview or self-report method of assessment by a clinician or survey interviewer (as used in much of the research discussed herein) is probably a valid method of diagnosis. Specific phobias can be diagnosed with only a few questions. For example, the first question about specific phobias from the revised third edition of the Diagnostic Interview Schedule,27 used in the Epidemiologic Catchment Area (ECA) study,28 asks about the fear itself and avoidance (eg, for blood and injection phobia, “have you ever had such an unreasonable fear of seeing blood; getting an injection; or going to the dentist that you tried to avoid it?”). The second question asks about persistence (eg, “did any of these fears continue for months or even years?”), and is followed by a series of questions about possible resulting distress or impairment, such as seeing a doctor, taking medication, or staying away from work.
Prevalence and incidence
Our literature search identified 25 population-based studies of the prevalence of specific phobias in adults, done between 1984 and 2016 in populations around the world (table 1). The median lifetime prevalence is 7·2% (IQR 4·0–10·4), and varies considerably among these reports, from 1·5% in Florence, Italy,41 and 2·6% in China50 to 14·4% in Oslo, Norway.39 Although some of this variation is likely to be due to the use of different assessment procedures, many structured survey assessment procedures are similar, deriving from the Diagnostic Interview Schedule53 (used in the ECA studies28), which evolved into the University of Michigan Composite International Diagnostic Interview,54 and then into the version used in the WHO World Mental Health Surveys.55 Differences in survey responses or age ranges of the samples could also explain the variation. However, large variations are also present in studies striving to use identical methods, such as the high rate for Baltimore in the ECA study (14·5% for male participants and 23·5% for female participants) as compared with the New Haven (3·8% and 8·5%) and St Louis (4·0% and 9·4%) ECA sites,56 and the large difference between two samples from different areas of Norway.39,42 These differences could provide guidance about as-yet-unknown risk factors, and suggest different causes that might be amenable to prevention or treatment. In east Asian populations, geographical variation is low, confined within the low lifetime prevalence in these regions: 2·6% in China, 3·4% in Japan, and 3·8% in Korea. There is no obvious trend in prevalence by calendar period. The 25 WHO World Mental Health Surveys also showed less variation than did other population-based studies, presumably because the WHO surveys all used the same instrument.57 However, low-income countries showed slightly lower prevalence in the WHO surveys, consistent with the pattern of results seen in the earlier individual studies. The large differences between populations suggest the importance of studying risk factors for specific phobias.
Table 1:
Lifetime prevalence of specific phobia in adults according to study and population
| Survey | Sample size | Age range, years | Lifetime prevalence (%) | |||
|---|---|---|---|---|---|---|
| Male participants | Female participants | Total | ||||
| USA and Canada | ||||||
| Bland et al, 198829 | Edmonton | 3258 | ≥18 | 4·6% | 9·8% | 7·2% |
| Eaton et al, 199130 | ECA | 14436 | ≥18 | 7·8% | 14·4% | 11·2% |
| Magee et al, 199631 | NCS | 8098 | 15–54 | 6.7% | 15·7% | 11·3% |
| Kessler et al, 200532 | NCS·R | 9282 | ≥18 | 8·9% | 15·8% | 12·5% |
| Stinson et al, 200723 | NESARC | 43093 | 18–98 | 6·2% | 12·4% | 9·4% |
| Latino populations | ||||||
| Canino et al, 198733 | Puerto Rico | 1551 | 17–64 | 7·6% | 9·6% | 8·6% |
| Vega et al, 199834 | MAPSS | 3012 | 18–59 | 6·2% | 8·8% | 7·4% |
| Vicente et al, 200635 | Chile | 2978 | ≥15 | 4·0% | 14·8% | 9·8% |
| Medina·Mora et al, 200736 | MNCS | 5826 | 18–65 | 7·0% | ||
| Viana and Andrade, 201237 | SPMMHS | 5037 | ≥18 | 7·9% | 16·5% | |
| Europe | ||||||
| Bijl et al, 199838 | NEMESIS | 7076 | 18–64 | 6·6% | 13·6% | 10·1% |
| Kringlen et al, 200139 | Oslo | 2066 | 18–65 | 8·0% | 19·5% | 14·4% |
| Alonso et al, 200440 | ESEMeD | 21 425 | ≥18 | 4·9% | 10·3% | 7·7% |
| Faravelli et al, 200441 | Italy | 2500 | ≥14 | 0·8% | 2·1% | 1·5% |
| Kringlen et al, 200642 | Rural Norway | 1080 | 18–65 | 2.4% | 10·6% | 6·5% |
| de Graaf et al, 201243 | NEMESIS2 | 6646 | 18–64 | 5·5% | 10·3% | 7·9% |
| Kiejna et al, 201544 | Poland | 10 081 | 18–64 | 2·2% | 4·6% | 3·4% |
| Middle East and Africa | ||||||
| Gureje et al, 200645 | Nigeria | 4984 | ≥18 | 5·4% | ||
| Karam et al, 200846 | Lebanon | 2857 | ≥18 | 4·0% | 10·2% | 7·1% |
| Alhasnawi et al, 200947 | Iraq MHS | 4332 | ≥18 | 4·2% | ||
| Asia | ||||||
| Chen et al, 199348 | Hong Kong | 7229 | 18·64 | 0·96% | 3·16% | |
| Oakley Browne et al, 200649 | NZ MHS | 12 992 | ≥16 | 7·3% | 14·1% | 10·8% |
| Lee et al, 200750 | China | 5201 | 18·70 | 2·6% | ||
| Cho et al, 201051 | Korea ECA·R | 6510 | 18·64 | 2·1% | 5·5% | 3·8% |
| Ishikawa et al, 201652 | Japan | 2130 | ≥20 | 3·4% | ||
| Overall* | ||||||
| Median (IQR) | 5·8% (2·4–7·6) | 6.7% (9·2–14·6) | 7·2% (4·0–10·4) | |||
| World MHS26 | ||||||
| 6 low·income and low·middle·income countries | 31 773 | ≥18 | 5·7% | |||
| 6 upper·middle·income countries | 24 612 | ≥18 | 8·0% | |||
| 13 high·income countries | 68 517 | ≥18 | 8·1% | |||
ECA=Epidemiologic Catchment Area. NCS=National Comorbidity Survey. NCS-R=National Comorbidity Survey Replication. NESARC=National Epidemiologic Survey of Alcohol and Related Conditions. MAPSS=Mexican American Prevalence and Services Survey. MNCS=Mexican National Comorbidity Survey. SPMMHS=São Paulo Megacity Mental Health Survey Sample. NEMESIS=Netherlands Mental Health Survey and Incidence Study. ESEMeD=European Study of the Epidemiology of Mental Disorders. MHS=Mental Health Survey. ECA-R=Epidemiologic Catchment Area Replication.
Including all studies in table except World MHS.
In all studies included in this Review, the lifetime prevalence of specific phobias was higher in female participants than in male participants. The greatest differences were observed in Chile, rural Norway, and Hong Kong, where prevalence in female participants was more than three times as high as in male participants, and the smallest differences were seen in two Latino populations: Mexicans in southern California34 and Puerto Ricans (table 1).33 The higher prevalence in women was consistent with a Darwinian interpretation58 (ie, that the process of selection favours groups in which the female members of the species were most avoidant of danger, especially during child-rearing years).59 However, there was no obvious explanation for the variation in male:female ratios around the world.
The first occurrence of a specific phobia can happen at any time throughout the lifespan, as shown by data from the Baltimore ECA follow-up,60 a cohort study designed to explore the life-course structure of mental disorders (figure). This study interviewed individuals selected probabilistically from the household-residing population in eastern Baltimore in 1981, with follow-up interviews of the same respondents in 1982, 1993–96, and 2004–05.60 When asked about the first occurrence of a phobia, many participants responded that they had experienced the phobia since they were a child or since they could remember, or similar, resulting in peaks in incidence at or below 5 years of age (figure). These findings are consistent with those of the Early Developmental Stages of Psychopathology study in Germany (in which almost all of the sample of 3021 adolescents reported onset of specific phobia in childhood or adolescence),62 the National Comorbidity Survey (NCS; in which the median age of onset in 8098 adults was 15 years),31 and the World Mental Health Surveys (completed in 22 countries with a total sample size of 124 902, in which the median age of onset was 8 years).57 The incidence of new specific phobias in girls during childhood was much higher than in boys, and gently declined thereafter until the beginning of adulthood (about 20 years of age), after which it rose until about age 30 years for women (figure). The peak incidence in women occurred during the years of reproduction and child rearing, possibly reflecting an evolutionary advantage. Men and women had an additional peak in incidence during old age that was much stronger for women, reaching nearly 1% per year. This pattern might reflect the new occurrence of physical conditions63 or adverse life events (such as the unexpected death of a loved one)64 during those years.
Figure: Incidence of specific phobia by age of first onset.
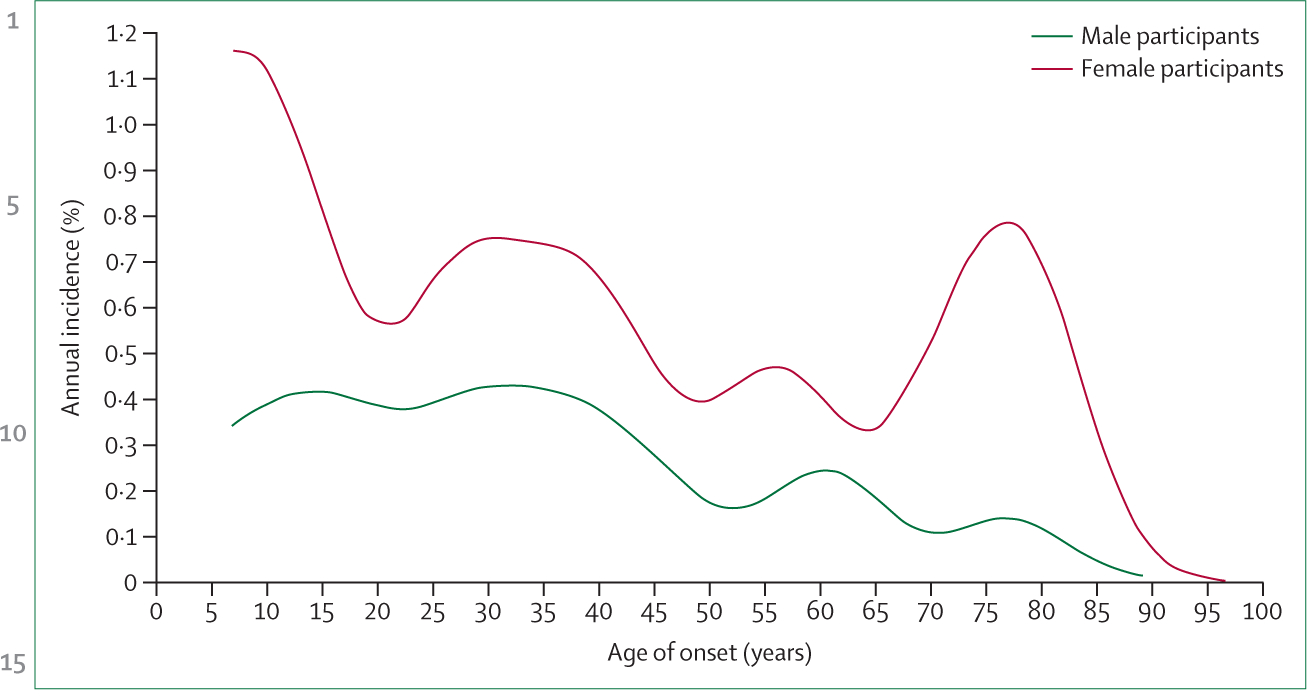
Data are from the Baltimore Epidemiologic Catchment Area follow-up study61 of 1920 respondents followed up from 1981 through 1993 (adapted from Public Mental Health [Oxford University Press] with permission). Kernel smoothing was applied, averaging incidence over a 5-year window to reduce variation.
Fears of specific objects or situations are widespread in the population. For example, more than 70% of people in the USA report having one or more unreasonable fears.23 The prevalence of these fears is much higher than that of the consequent diagnoses (table 2), which require the presence of avoidance and impairment related to the fear. In publicly available datasets from the USA (the National Epidemiologic Survey of Alcohol and Related Conditions [NESARC]23 and the NCS31) and from the Netherlands Mental Health Survey and Incidence Study (NEMESIS)38—all of which included large probabilistic samples representing national populations and used structured, diagnostically oriented interviews—fears of animals and heights are the two most prevalent fears in all three samples, and the order of prevalence of the different specific fears is relatively constant, with the exception that fear of blood is less prevalent in NESARC than in the other two studies (table 2). The conditional probabilities of meeting the diagnostic criteria for specific phobias given the presence of the fear are similar across all seven fears and across all three samples (about 25–30%). The lifetime prevalence estimates of particular specific phobias (about 2–6%; table 2, rightmost columns) are of the same order of magnitude as many other, more broadly defined, psychiatric diagnoses. The baseline prevalence estimates for specific phobias in the Baltimore ECA (table 3, left column) are higher than the estimates from the NESARC, NCS, and NEMESIS studies (table 2), suggesting Baltimore to be an outlier with particularly high prevalence (as also shown in table 1). Since phobias are, by definition, distressing or impairing, their effective prevention or treatment could have a non-trivial effect on the mental health of the population. For blood or injection phobia, prevention could also provide a physical health benefit, because people with this phobia presumably avoid contact with doctors who engage in preventive measures across the general health spectrum. Although there are a range of universal prevention programmes for early psychopathology in general, few of them have been examined specifically with respect to simple phobias.66,67
Table 2:
Lifetime prevalence of specific fears, phobia given specific fears, and specific phobias
| Prevalence of fear (%) in total sample* | Prevalence of specific phobia (%) in participants with specific fear† | Prevalence of specific phobia (%) in total sample‡ | |||||||
|---|---|---|---|---|---|---|---|---|---|
| NESARC (n=43093) | NCS (n=8098) | NEMESIS (n=7076) | NESARC (n=43093) | NCS (n=8098) | NEMESIS (n=7076) | NESARC (n=43093) | NCS (n=8098) | NEMESIS (n=7076) | |
| Animals | 19·7% | 22·2% | 12·6% | 24·0% | 25·8% | 26·5% | 4·7% | 5·7% | 3·3% |
| Heights | 18·7% | 20·4% | 19·1% | 24·2% | 26·2% | 25·5% | 4·5% | 5·3% | 4·9% |
| Flying | 11·4% | 13·2% | 6·9% | 25·6% | 26·9% | 36·6% | 2·9% | 3·5% | 2·5% |
| Closed spaces | 11·1% | 11·9% | 9·5% | 28·9% | 35·1% | 35·0% | 3·2% | 4·2% | 3·3% |
| Water | 9·5% | 9·4% | 7·1% | 25·7% | 35·8% | 30·4% | 2·4% | 3·4% | 2·2% |
| Storms | 7·6% | 8·7% | 7·0% | 25·7% | 33·1% | 31·3% | 1·9% | 2·9% | 2·2% |
| Blood | 7·4% | 13·9% | 9·5% | 28·6% | 32·8% | 33·3% | 2·1% | 4·5% | 3·2% |
NESARC=National Epidemiologic Survey of Alcohol and Related Conditions (using the Alcohol Use Disorder and Associated Disabilities Interview Schedule).23 NCS=National Comorbidity Survey (using the Composite International Diagnostic Interview).31 NEMESIS=Netherlands Mental Health Survey and Incidence Study (using the Composite International Diagnostic Interview).38
Lifetime prevalence of specific fears in the total sample.
Lifetime prevalence of specific phobia diagnosis among people with a specific fear of the same stimulus.
Lifetime prevalence of specific phobia diagnosis with a particular fear in the total sample.
Table 3:
12-month prevalence and persistence of specific phobias in adults in three longitudinal studies
| ECA65 | NCS31 | NESARC23 | |||||
|---|---|---|---|---|---|---|---|
| Baseline prevalence | Persistence at 1 year | Persistence at 12 years | Baseline prevalence | Persistence at 10 years | Baseline prevalence | Persistence at 3 years | |
| Animals | 8·6% (04) | 12% | 14% | 4·9% (0·3) | 25% | 3·7% (0·2) | 15% |
| Heights | 6·9% (0·4) | 20% | 11% | 4·3% (0·4) | 38% | 3·4% (0·1) | 17% |
| Storms* | 3·9% (0·3) | 14% | 8% | 2·4% (0·3) | 25% | 1·5% (0·1) | 14% |
| Water* | 4·0% (0·3) | 17% | 6% | 2·8% (0·3) | 25% | 1·9% (0·1) | 11% |
| Flying† | 3·0% (0·3) | 12% | 6% | 2·9% (0·3) | 37% | 2·3% (0·1) | 16% |
| Crowds | 1·9% (0·2) | 9% | 28% | ·· | ·· | 1·2% (0·1) | 19% |
| Closed spaces | 2·5% (0·2) | 6% | ·· | 3·5% (0·4) | 34% | 2·4% (01) | 17% |
| Blood‡ | ·· | ·· | ·· | 3·6% (0·3) | 28% | 1·6% (0·1) | 15% |
| Dentist‡ | ·· | ·· | ·· | ·· | ·· | 0·5% (0·1) | 14% |
| Hospital‡ | ·· | ·· | ·· | ·· | ·· | 1·8% (0·1) | 12% |
Baseline prevalence (in 12 months preceding initial interview) is shown as % (SE). Persistence is defined as occurrence in the 12-month period preceding the follow-up interview among patients who met the criteria for the disorder in the 12 months preceding the baseline interview. ECA=Epidemiologic Catchment Area. NCS=National Comorbidity Survey. NESARC=National Epidemiologic Survey of Alcohol and Related Conditions.
NCS assessed fear of storms and water together at 10-year follow-up.
ECA assessed fear of flying together with other forms of public transportation at baseline and 1 year.
NCS assessed fear of blood and injections together with fear of dentists, doctors, and hospitals.
Clinical course
Specific phobias are not transient disorders, as shown by data from the ECA, NCS, and NESARC studies (table 3). Persistence, reflecting the chronicity of the disorder, is measured by the percentage of patients with a past-year history of the disorder at the baseline interview who report an occurrence of the disorder within the 12 months preceding the follow-up interview. In the ECA sample, 6–20% of specific phobias were persistent at 1 year, and 6–28% at 12 years; in the NCS sample, persistence at 10 years ranged from 25% to 38%; and in the NESARC sample, persistence at 3 years ranged from 12% to 19% (table 3). A similar estimate of persistence, 17·5% for any specific phobia, was observed after 8 years of follow-up in the Mexican Adolescent Mental Health Survey,68 while persistence in the NCS sample after 10 years was greater, at about 25%. In all three samples shown in table 3, one of the most persistent phobias was that of heights. This degree of persistence is similar to that of other common, non-psychotic mental disorders.61
Specific phobias are strong predictors of other anxiety disorders and of mood and substance-use disorders (table 4). In the NESARC study,23 anxiety disorders were the most strongly predicted, as might be expected, with odds ratios (ORs) ranging from 5·60 to 7·41 (95% CIs 4·95–8·40), without much change after adjustment for sociodemographic factors (5·12 to 7·18 [4·50–8·11]). Even after adjustment for other common mental disorders, the ORs for any anxiety disorder were high (3·84 [3·46–4·27]; table 4). Mood disorders were also strongly predicted (4·05 [3·69–4·46]), and the OR remained high after adjusting for closely related mood disorders (eg, the ORs for specific phobias predicting major depressive disorder were 1·99 [1·80–2·20] after adjusting for the earlier occurrence of dysthymia and mania). The ORs for substance-use disorders were lower than those of anxiety disorders, but still non-trivial and statistically significant (1·83 [1·67–2·00]).23 High cooccurrence of specific phobias and other mental disorders was also observed across the World Mental Health Survey samples, in which 61% of lifetime cases of specific phobia had at least one other mental disorder.57 These data suggest that the incidence of other common mental disorders could potentially be reduced by effective treatment of specific phobias.69,70
Table 4:
Lifetime specific phobia as a predictor of lifetime mood, anxiety, and substance disorders (National Epidemiologic Survey of Alcohol and Related Conditions [n=43 093])23
| Unadjusted OR (95% CI) | OR adjusted for sociodemographic factors (95% CI)* | OR adjusted for sociodemographic and psychiatric factors (95% CI)† | |
|---|---|---|---|
| Mood disorders | 4·05 (3·69–4·46) | 3·70 (3·36–4·09) | 2·03 (1·84–2·25) |
| Major depression | 4·08 (3·72–4·46) | 3·68 (3·34–4·04) | 1·99 (1·80–2·20) |
| Dysthymia | 3·69 (3·24–4·19) | 3·40 (2·99–3·87) | 1·51 (1·32–1·74) |
| Mania or hypomania | 3·66 (3·27–4·10) | 3·65 (3·23–4·12) | 1·84 (1·62–2·09) |
| Anxiety disorders | 6·27 (5·66–6·94) | 5·89 (5·32–6·52) | 3·84 (3·46–4·27) |
| Panic disorder | 5·60 (4·95–6·33) | 5·12 (4·50–5·82) | 3·05 (2·67–3·48) |
| Social phobia | 7·41 (6·54–8·40) | 7·18 (6·36–8·11) | 4·68 (4·12–5·32) |
| Generalised anxiety disorder | 6·22 (5·47–7·07) | 5·79 (5·08–6·60) | 3·09 (2·71–3·53) |
| Substance use disorders | 2·18 (2·00–2·37) | 2·63 (2·41–2·87) | 1·83 (1·67–2·00) |
| Alcohol use disorder | 1·79 (1·64–1·96) | 2·30 (2·09–2·54) | 1·62 (1·46–1·79) |
| Nicotine dependence | 2·59 (2·37–2·83) | 2·74 (2·51–3·00) | 1·83 (1·66–2·03) |
| Drug use disorder | 2·20 (1·96–2·46) | 2·54 (2·24–2·87) | 1·52 (1·35–1·72) |
All associations are significant at p<0·001.
Adjusted for age, sex, education, and urbanicity.
Adjusted for age, sex, education, urbanicity, and selected lifetime mental disorders (mood, anxiety, and substance-use disorders).
Risk factors
Risk factors for specific phobias have not been well studied. Most potentially pertinent studies group the anxiety disorders into one category in their presentation of even the most rudimentary risk factors. The most important demographic risk factor for specific phobias seems to be female sex (table 1). We identified five studies in which the prevalence of specific phobias could be compared between rural and urban populations,23,39,42,34,33 and found very little difference between the two groups, except in Norway, where the prevalence was 14% in the urban population and 7% in the rural population.39,42
We estimated the association between the prevalence of specific fears and education, marital status, and residence in the NESARC sample, which was the only study to have this amount of detail for specific phobias of animals, heights, storms, and closed spaces (table 5).23 Lower educational attainment was associated with higher prevalence of any specific phobia (40% in people with less than high school education vs 29% in college graduates), as was formerly married status (38% in people who were separated or divorced, and 42% in widowed people, vs 35% in married people). The difference in prevalence between rural and urban areas was trivial, which is surprising given that exposures to fear stimuli presumably differ between those areas, with more exposure to animals in rural areas and heights in urban areas.
Table 5:
Lifetime prevalence of specific phobias by three demographic characteristics (National Epidemiologic Study of Alcohol and Related Conditions [n=43 093])23
| Any specific phobia | Animals | Heights | Storms | Closed places | |
|---|---|---|---|---|---|
| Educational level | |||||
| Less than high school | 40% (1·0) | 24% (0·8) | 23% (0·6) | 14% (07) | 13% (0·6) |
| High school graduate | 37% (0·7) | 21% (0·6) | 20% (0·5) | 9% (0·3) | 11% (0·4) |
| Some college | 35% (0·7) | 19% (0·5) | 18% (0·5) | 6% (0·3) | 11% (0·4) |
| College graduate | 29% (0·7) | 15% (0·6) | 15% (0·5) | 4% (0.2) | 9% (0·4) |
| Marital status | |||||
| Never married | 33% (0·8) | 19% (0·6) | 17% (0.6) | 6% (0·4) | 9% (0·4) |
| Married | 35% (0·6) | 19% (0·4) | 18% (0·4) | 7% (0.3) | 11% (0·3) |
| Separated or divorced | 38% (0·8) | 22% (07) | 21% (0·6) | 9% (0·5) | 13% (0·5) |
| Widowed | 42% (1·1) | 25% (0·9) | 22% (0·8) | 14% (0·6) | 14% (0·6) |
| Residence | |||||
| Rural | 38% (0.9) | 21% (0·8) | 21% (0·5) | 9% (0·4) | 12% (0·5) |
| Suburban | 34% (0·8) | 18% (0·5) | 18% (0·5) | 7% (0.3) | 11% (0·3) |
| City | 35% (0·9) | 21% (0·6) | 19% (0·6) | 8% (0·4) | 11% (0·4) |
Data are % (SE)
Data from the World Mental Health Surveys also indicate a higher prevalence of any specific phobia in people with lower educational attainment.57 Lower educational attainment is an indicator of lower socioeconomic status in general, which is presumably associated with less control over the social and physical environment, especially in conditions of stress. Consistent with data from the USA, World Mental Health Survey data indicate a higher prevalence of any specific phobia among formerly married people (relative odds 1·3 in high-income countries and 1·1 in low-income or middle-income countries).57 These data suggest that marital status as a risk factor for specific phobias might vary by geographical region, or according to other environmental characteristics. It seems reasonable that having a marital partner would alleviate fears somewhat in offering a protective element (ie, a spouse) to the environment; it is also possible that formerly married people are more likely to be depressed, which might be a risk factor for simple phobias.
Although genetic risk factors for specific phobias have been studied for at least three decades,71 many of the existing studies involve overlapping samples.72 Phobias are more likely to occur in people whose family members have phobias. Twin studies suggest that within-family resemblance is due to shared environmental factors in childhood,73–75 whereas genetic factors influence familial resemblance in adulthood.76 A meta-analysis of ten independent twin studies of specific phobias reported a mean heritability of about 30% for the three subtypes of phobias studied (animal, situational, and blood-illness).72 Genetic epidemiological methods are also useful to elucidate how phobias relate to personality traits and other psychiatric disorders. Multivariate structural equation modelling of twin data suggests that genetic factors that influence animal and situational phobias are distinguishable from those that influence major depressive disorder, generalised anxiety disorder, panic disorder, agoraphobia, and social phobia.77 Specific phobias also appear to be less genetically correlated with neuroticism and extraversion than are other anxiety and depressive disorders, including social phobia and agoraphobia.78,79
Treatment
Only about a tenth to a quarter of people with specific phobias eventually receive treatment,30,57 possibly because avoidance can reduce stress and impairment. Predictors for receiving treatment include having more severe impairment, having particular phobias (eg, people with phobias of flying, closed spaces, or heights are more likely to seek treatment), and having a greater number of phobias.57 To our knowledge, no studies have addressed the comparative effectiveness of different treatment options. Therefore, we discuss the evidence regarding the effectiveness of treatments relative to non-treatment control conditions, with a preference for published systematic reviews and meta-analyses.
Exposure therapy is the current treatment of choice for specific phobias.80,81 The standard form of exposure therapy involves in-vivo or imaging approaches to phobic stimuli or situations. Virtual-reality exposure therapy was first introduced more than two decades ago to treat fear of heights82 and remains a viable treatment option for other specific phobias.83 Three decades ago, Öst pioneered a one-session treatment approach for specific phobias, with an average duration of approximately 2 h.84,85 Subsequent studies by Öst and colleagues suggested that a single 3-h session of massed exposure therapy is as effective as multiple sessions (total 6 h) of more gradual exposure therapy for the treatment of phobias of flying,86 blood and injections,87 and claustrophobia.88 The results of a 2008 meta-analysis indicate that multiple sessions might be somewhat more effective than the single-session approach, as measured by questionnaire-based functional outcomes at follow-up,81 and careful consideration is needed when choosing the appropriate number and duration of sessions for patients;89 however, the massed single-session approach could be considered a viable option for suitable patients.
Early studies of exposure therapies for specific phobias90 were criticised for their various methodological limitations, including selection biases, the use of small, unrepresentative samples, and compromised control conditions. Although exposure therapy is much more widely studied and accepted now than it was in the early 1970s, systematic reviews suggest that the evidence base could still be improved.80,81 Additionally, although the available evidence indicates moderately high short-term efficacy of psychological treatments for specific phobias,80 most studies have only followed up patients for short durations. The assessment of long-term effectiveness is particularly important because treated phobias in patients (and extinguished fear responses in other animals) are susceptible to relapse.91–96 One of the notable risk factors for relapse is context change, in which the individual reencounters the phobic stimulus or situation outside of the context in which extinction originally occurred.93,96 Accordingly, studies have sought to extinguish conditioned responses to fear or phobic stimuli in multiple contexts, finding this approach to be comparatively more effective than extinction in a single context.95–98
Pharmacotherapy is not a common treatment choice for specific phobias. However, within the past decade, studies have investigated pharmacological augmentation of exposure therapy in attempts to improve treatment outcomes. In one approach, clinicians administer the antibiotic D-cycloserine, which is thought to facilitate fear extinction learning through its role as an N-methyl D-aspartate receptor agonist.99,100 The results of the first published, double-blind, randomised trial in humans indicated that oral administration of D-cycloserine (50 mg or 500 mg) before virtual-reality exposure therapy for phobia of heights was associated with substantially greater improvement than was placebo.100 Results from a systematic review of placebo-controlled studies suggest that pre-exposure D-cycloserine administration (50 mg, 250 mg, or 500 mg) is associated with a small exposure augmentation benefit in patients with anxiety, obsessive-compulsive, or post-traumatic stress disorders (compared with pretreatment, d=–0·25 at post-treatment, d=0·19 at follow-up).101 In another approach, clinicians administer glucocorticoids—which appear to have a role in fear extinction processing—before exposure therapy. In two randomised trials, participants in the treatment group were orally administered 20 mg cortisol 1 h before virtual-reality exposure therapy for fear of heights102 or in-vivo exposure therapy for fear of spiders.103 Both studies found that cortisol administration enhanced the efficacy of treatment relative to placebo-controlled exposure therapy.
Conclusion
Although specific phobias have a high prevalence, a low percentage of affected people seek treatment. Specific phobias begin early in life and persist over years or decades, and are associated with increased risk of various other mental disorders. The prevalence, incidence, course, and comorbidities of specific phobias are similar across the different subtypes, with the possible exception that fear of heights is more prevalent and more persistent than other subtypes. The consistent associations with some risk factors, such as female sex, education, and formerly married status, suggest the possible existence of causal pathways that could be altered to produce beneficial effects.
Future studies should more thoroughly examine barriers to treatment for specific phobias, and more high-quality studies assessing longer-term outcomes in patients treated with different forms of exposure therapy (eg, massed single-session vs more gradual multiple-session exposure, or single-context vs multiple-context exposure) are needed. The potential benefits of pharmacological augmentation of exposure also warrant further study. There is insufficient research regarding how the onset of related phobias is affected by the initial exposure to the feared object or situation, or the context of the exposure (such as the presence of social support or stress, and the magnitude of the exposure itself). Furthermore, little is known about the possibility of crossover from one type of specific phobia to another. Future research could illuminate these possibilities.
Search strategy and selection criteria.
We searched PubMed on Oct 11, 2017, combining MeSH and open terms for phobias (“phobia*”[tw]) and epidemiology (“Epidemiologic Studies”[MeSH:NoExp] OR “Observational Study”[Publication Type] OR “Observational Study as Topic”[MeSH] OR “Cohort Studies”[MeSH] OR “epidemiologic study”[tw] OR “epidemiologic studies”[tw] OR “follow up”[tw] OR “longitudinal”[tw] OR “prospective*”[tw] OR “observational study”[tw] OR “observational studies”[tw]). The search was limited to studies in English and yielded 1536 records, which we assessed for their relevance to the prevalence, incidence, course, risk factors, or consequences of phobias. Citations included in reviews that did not meet the inclusion criteria were searched to identify relevant articles that the original search might have failed to capture.
Acknowledgments
WWE’s work is funded in part by a National Institute on Aging grant (U01AG052445).
Footnotes
Declaration of interests
We declare no competing interests.
References
- 1.Eaton WW, Martins SS, Nestadt G, Bienvenu OJ, Clarke D, Alexandre P. The burden of mental disorders. Epidemiol Rev 2008; 30: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marks IM. Fears, phobias, and rituals: Panic, anxiety and their disorders. New York: Oxford University Press, 1987. [Google Scholar]
- 3.Eaton WW, Kessler RC, Wittchen HU, Magee WJ. Panic and panic disorder in the United States. Am J Psychiatry 1994; 151: 413–20. [DOI] [PubMed] [Google Scholar]
- 4.Goodwin RD. The prevalence of panic attacks in the United States: 1980 to 1995. J Clin Epidemiol 2003; 56: 914–16. [DOI] [PubMed] [Google Scholar]
- 5.Grant BF, Hasin DS, Stinson FS, et al. The epidemiology of DSM-IV panic disorder and agoraphobia in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry 2006; 67: 363–74. [DOI] [PubMed] [Google Scholar]
- 6.Kessler RC, Chiu WT, Jin R, Ruscio AM, Shear K, Walters EE. The epidemiology of panic attacks, panic disorder, and agoraphobia in the National Comorbidity Survey replication. Arch Gen Psychiatry 2006; 63: 415–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weissman MM. The epidemiology of panic disorder and agoraphobia In: Frances A, Hales R, eds. American Psychiatric Association review of psychiatry. Washington, DC: American Psychiatric Press, 1988: 54–66. [Google Scholar]
- 8.Stein MB, Torgrud LJ, Walker JR. Social phobia symptoms, subtypes, and severity: findings from a community survey. Arch Gen Psychiatry 2000; 57: 1046–52. [DOI] [PubMed] [Google Scholar]
- 9.Heimberg RG, Stein MB, Hiripi E, Kessler RC. Trends in the prevalence of social phobia in the United States: a synthetic cohort analysis of changes over four decades. Eur Psychiatry 2000; 15: 29–37. [DOI] [PubMed] [Google Scholar]
- 10.Lépine JP, Lellouch J. Classification and epidemiology of social phobia. Eur Arch Psychiatry Clin Neurosci 1995; 244: 290–96. [DOI] [PubMed] [Google Scholar]
- 11.Miloyan B, Bulley A, Pachana NA, Byrne GJ. Social phobia symptoms across the adult lifespan. J Affect Disord 2014; 168: 86–90. [DOI] [PubMed] [Google Scholar]
- 12.Neufeld KJ, Swartz KL, Bienvenu OJ, Eaton WW, Cai G. Incidence of DIS/DSM-IV social phobia in adults. Acta Psychiatr Scand 1999; 100: 186–92. [DOI] [PubMed] [Google Scholar]
- 13.Ruscio AM, Brown TA, Chiu WT, Sareen J, Stein MB, Kessler RC. Social fears and social phobia in the USA: results from the National Comorbidity Survey Replication. Psychol Med 2008; 38: 15–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schneier FR, Johnson J, Hornig CD, Leibowitz JR, Weissman MM. Social phobia. Comorbidity and morbidity in an epidemiologic sample. Arch Gen Psychiatry 1992; 49: 282–88. [DOI] [PubMed] [Google Scholar]
- 15.Wells JC, Tien AY, Garrison R, Eaton WW. Risk factors for the incidence of social phobia as determined by the Diagnostic Interview Schedule according to DSM-III in a population-based study. Acta Psychiatr Scand 1994; 90: 84–90. [DOI] [PubMed] [Google Scholar]
- 16.Wittchen HU, Fehm L. Epidemiology and natural course of social fears and social phobia. Acta Psychiatr Scand Suppl 2003: 4–18. [DOI] [PubMed] [Google Scholar]
- 17.Bienvenu OJ, Nestadt G, Eaton WW. Characterizing generalized anxiety: temporal and symptomatic thresholds. J Nerv Ment Dis 1998; 186: 51–56. [DOI] [PubMed] [Google Scholar]
- 18.Blazer DG, Hughes D, George LK, Swartz M, Boyar J. Generalized anxiety disorders In: Robins LN, Regier DA, eds. Psychiatric disorders in America. New York: The Free Press, 1991: 180–203. [Google Scholar]
- 19.Grant BF, Hasin DS, Stinson FS, et al. Prevalence, correlates, co-morbidity, and comparative disability of DSM-IV generalized anxiety disorder in the USA: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med 2005; 35: 1747–59. [DOI] [PubMed] [Google Scholar]
- 20.Wittchen HU, Zhao S, Kessler RC, Eaton WW. DSM-III-R generalized anxiety disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51: 355–64. [DOI] [PubMed] [Google Scholar]
- 21.Curtis GC, Magee WJ, Eaton WW, Wittchen HU, Kessler RC. Specific fears and phobias. Epidemiology and classification. Br J Psychiatry 1998; 173: 212–17. [PubMed] [Google Scholar]
- 22.Fredrikson M, Annas P, Fischer H, Wik G. Gender and age differences in the prevalence of specific fears and phobias. Behav Res Ther 1996; 34: 33–39. [DOI] [PubMed] [Google Scholar]
- 23.Stinson FS, Dawson DA, Patricia Chou S, et al. The epidemiology of DSM-IV specific phobia in the USA: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med 2007; 37: 1047–59. [DOI] [PubMed] [Google Scholar]
- 24.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Washington, DC: American Psychiatric Association, 1952. [Google Scholar]
- 25.American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5th edn Arlington, Virginia: American Psychiatric Association, 2013. [Google Scholar]
- 26.WHO. The ICD-10 classification of mental and behavioural disorders - diagnostic criteria for research. Geneva: World Health Organization, 1993. [Google Scholar]
- 27.Robins L, Helzer J, Cottler L, Goldring E. NIMH Diagnostic Interview Schedule: version iii revised (DIS-III-R). St Louis: Washington University, 1989. [Google Scholar]
- 28.Eaton WW, Regier DA, Locke BZ, Taube CA. The Epidemiologic Catchment Area program of the National Institute of Mental Health. Public Health Rep 1981; 96: 319–25. [PMC free article] [PubMed] [Google Scholar]
- 29.Bland RC, Orn H, Newman SC. Lifetime prevalence of psychiatric disorders in Edmonton. Acta Psychiatr Scand Suppl 1988; 338: 24–32. [DOI] [PubMed] [Google Scholar]
- 30.Eaton WW, Dryman A, Weissman MM. Panic and phobia In: Robins LN, Regier DA, ed. Psychiatric disorders in America: the Epidemiologic Catchment Area study. New York:The Free Press, 1991: 155–79. [Google Scholar]
- 31.Magee WJ, Eaton WW, Wittchen HU, McGonagle K, Kessler R. Agoraphobia, simple phobia, and social phobia in the National Comorbidity Survey. Arch Gen Psychiatry 1996; 53: 159–68. [DOI] [PubMed] [Google Scholar]
- 32.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005; 62: 593–602. [DOI] [PubMed] [Google Scholar]
- 33.Canino GJ, Bird HR, Shrout PE, et al. The prevalence of specific psychiatric disorders in Puerto Rico. Arch Gen Psychiatry 1987; 44: 727–35. [DOI] [PubMed] [Google Scholar]
- 34.Vega WA, Kolody B, Aguilar-Gaxiola S, Alderete E, Catalano R, Caraveo-Anduaga J. Lifetime prevalence of DSM-III-R psychiatric disorders among urban and rural Mexican Americans in California. Arch Gen Psychiatry 1998; 55: 771–78. [DOI] [PubMed] [Google Scholar]
- 35.Vicente B, Kohn R, Rioseco P, Saldivia S, Levav I, Torres S. Lifetime and 12-month prevalence of DSM-III-R disorders in the Chile psychiatric prevalence study. Am J Psychiatry 2006;163: 1362–70. [DOI] [PubMed] [Google Scholar]
- 36.Medina-Mora ME, Borges G, Benjet C, Lara C, Berglund P. Psychiatric disorders in Mexico: lifetime prevalence in a nationally representative sample. Br J Psychiatry 2007; 190: 521–28. [DOI] [PubMed] [Google Scholar]
- 37.Viana MC, Andrade LH. Lifetime prevalence, age and gender distribution and age-of-onset of psychiatric disorders in theSao Paulo Metropolitan Area, Brazil: results from the Sao Paulo Megacity Mental Health Survey. Rev Bras Psiquiatr 2012; 34: 249–60. [DOI] [PubMed] [Google Scholar]
- 38.Bijl RV, Ravelli A, van Zessen G. Prevalence of psychiatric disorder in the general population: results of The Netherlands Mental Health Survey and Incidence Study (NEMESIS). Soc Psychiatry Psychiatr Epidemiol 1998; 33: 587–95. [DOI] [PubMed] [Google Scholar]
- 39.Kringlen E, Torgersen S, Cramer V. A Norwegian psychiatric epidemiological study. Am J Psychiatry 2001; 158: 1091–98. [DOI] [PubMed] [Google Scholar]
- 40.Alonso J, Angermeyer MC, Bernert S, et al. Prevalence of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl 2004: 21–7. [DOI] [PubMed] [Google Scholar]
- 41.Faravelli C, Abrardi L, Bartolozzi D, et al. The Sesto Fiorentino study: background, methods and preliminary results. Lifetime prevalence of psychiatric disorders in an Italian community sample using clinical interviewers. Psychother Psychosom 2004; 73: 216–25. [DOI] [PubMed] [Google Scholar]
- 42.Kringlen E, Torgersen S, Cramer V. Mental illness in a rural area: a Norwegian psychiatric epidemiological study. Soc Psychiatry Psychiatr Epidemiol 2006; 41: 713–19. [DOI] [PubMed] [Google Scholar]
- 43.de Graaf R, Ten Have M, van Gool C, van Dorsselaer S. Prevalence of mental disorders, and trends from 1996 to 2009. Results from NEMESIS-2. Tijdschr Psychiatr 2012; 54: 27–38 (in Dutch). [PubMed] [Google Scholar]
- 44.Kiejna A, Piotrowski P, Adamowski T, et al. The prevalence of common mental disorders in the population of adult Poles by sex and age structure - an EZOP Poland study. Psychiatr Pol 2015;49: 15–27 (in Polish). [DOI] [PubMed] [Google Scholar]
- 45.Gureje O, Lasebikan VO, Kola L, Makanjuola VA. Lifetime and 12-month prevalence of mental disorders in the Nigerian Survey of Mental Health and Well-Being. Br J Psychiatry 2006; 188: 465–71. [DOI] [PubMed] [Google Scholar]
- 46.Karam EG, Mneimneh ZN, Karam AN, et al. Mental disorders and war in Lebanon In: Kessler RC, Ustun TB, eds. The WHO World Mental Health Surveys: global perspectives on the epidemiology of mental disorders. New York: Cambridge University Press,2008: 265–78. [Google Scholar]
- 47.Alhasnawi S, Sadik S, Rasheed M, et al. The prevalence and correlates of DSM-IV disorders in the Iraq Mental Health Survey (IMHS). World Psychiatry 2009; 8: 97–109. [PMC free article] [PubMed] [Google Scholar]
- 48.Chen CN, Wong J, Lee N, Chan-Ho MW, Lau JT, Fung M. The Shatin community mental health survey in Hong Kong. II. Major findings. Arch Gen Psychiatry 1993; 50: 125–33. [DOI] [PubMed] [Google Scholar]
- 49.Oakley Browne MA, Wells JE, Scott KM, McGee MA. Lifetime prevalence and projected lifetime risk of DSM-IV disorders in Te Rau Hinengaro: the New Zealand Mental Health Survey. Aust NZ J Psychiatry 2006; 40: 865–74. [DOI] [PubMed] [Google Scholar]
- 50.Lee S, Tsang A, Zhang MY, et al. Lifetime prevalence and inter-cohort variation in DSM-IV disorders in metropolitan China. Psychol Med 2007; 37: 61–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cho MJ, Kim JK, Jeon HJ, et al. Lifetime and 12-month prevalence of DSM-IV psychiatric disorders among Korean adults. J Nerv Ment Dis 2007; 195: 203–10. [DOI] [PubMed] [Google Scholar]
- 52.Ishikawa H, Kawakami N, Kessler RC. Lifetime and 12-month prevalence, severity and unmet need for treatment of common mental disorders in Japan: results from the final dataset of World Mental Health Japan Survey. Epidemiol Psychiatr Sci 2016;25: 217–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Robins LN, Helzer JE, Croughan J, Ratcliff KS. National Institute of Mental Health Diagnostic Interview Schedule. Its history, characteristics, and validity. Arch Gen Psychiatry 1981; 38: 381–89. [DOI] [PubMed] [Google Scholar]
- 54.Wittchen HU, Zhao S, Abelson JM, Abelson JL, Kessler RC. Reliability and procedural validity of UM-CIDI DSM-III-R phobic disorders. Psychol Med 1996; 26: 1169–77. [DOI] [PubMed] [Google Scholar]
- 55.Kessler RC, Ustün TB. The World Mental Health (WMH) Survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res 2004; 13: 93–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Robins LN, Helzer JE, Weissman MM, et al. Lifetime prevalence of specific psychiatric disorders in three sites. Arch Gen Psychiatry 1984; 41: 949–58. [DOI] [PubMed] [Google Scholar]
- 57.Wardenaar KJ, Lim CCW, Al-Hamzawi AO, Alonso J. The cross-national epidemiology of specific phobia in the World Mental Health Surveys. Psychol Med 2017; 47: 1744–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McGuire M, Troisi A. Darwinian psychiatry. New York: Oxford University Press, 1998. [Google Scholar]
- 59.Bracha HS, Bienvenu OJ, Eaton WW. Testing the paleolithic-human-warfare hypothesis of blood-injection phobia in the Baltimore ECA follow-up study—towards a more etiologically-based conceptualization for DSM-V. J Affect Disord 2007; 97: 1–4. [DOI] [PubMed] [Google Scholar]
- 60.Eaton WW, Kalaydjian A, Scharfstein DO, Mezuk B, Ding Y. Prevalence and incidence of depressive disorder: the Baltimore ECA follow-up, 1981–2004. Acta Psychiatr Scand 2007; 116: 182–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Eaton WW, Alexandre PI, Kessler RC, et al. The population dynamics of mental disorders In: Eaton WW, and the Faculty, Students and Fellows of the Department of Mental Health, eds. Public Mental Health. New York: Oxford University Press, 2012: 125–50. [Google Scholar]
- 62.Beesdo K, Pine DS, Lieb R, Wittchen HU. Incidence and risk patterns of anxiety and depressive disorders and categorization of generalized anxiety disorder. Arch Gen Psychiatry 2010; 67: 47–57. [DOI] [PubMed] [Google Scholar]
- 63.El-Gabalawy R, Mackenzie CS, Shooshtari S, Sareen J. Comorbid physical health conditions and anxiety disorders:a population-based exploration of prevalence and health outcomes among older adults. Gen Hosp Psychiatry 2011; 33: 556–64. [DOI] [PubMed] [Google Scholar]
- 64.Keyes KM, Pratt C, Galea S, McLaughlin KA, Koenen KC, Shear MK. The burden of loss: unexpected death of a loved one and psychiatric disorders across the life course in a national study. Am J Psychiatry 2014; 171: 864–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Eaton WW, Anthony JC, Gallo J, et al. Natural history of Diagnostic Interview Schedule/DSM-IV major depression. The Baltimore Epidemiologic Catchment Area follow-up. Arch Gen Psychiatry 1997; 54: 993–99. [DOI] [PubMed] [Google Scholar]
- 66.Trumpf J, Margraf J, Vriends N, Meyer AH, Becker ES. Predictors of specific phobia in young women: a prospective community study. J Anxiety Disord 2010; 24: 87–93. [DOI] [PubMed] [Google Scholar]
- 67.Mendelson T, Pas ET, Leis JA, Bradshaw CP, Rebok GW, Mandell W. The logic and practice of the prevention of mental disorders In: Eaton WW (ed). Public mental health. New York: Oxford University Press, 2012: 459–509. [Google Scholar]
- 68.Albor YC, Benjet C, Méndez E, Medina-Mora ME. Persistence of specific phobia from adolescence to early adulthood: longitudinal follow-up of the Mexican Adolescent Mental Health Survey. J Clin Psychiatry 2017; 78: 340–46. [DOI] [PubMed] [Google Scholar]
- 69.Lieb R, Miché M, Gloster AT, Beesdo-Baum K, Meyer AH, Wittchen HU. Impact of specific phobia on the risk of onset of mental disorders: a 10-year prospective-longitudinal community study of adolescents and young adults. Depress Anxiety 2016; 33: 667–75. [DOI] [PubMed] [Google Scholar]
- 70.Trumpf J, Margraf J, Vriends N, Meyer AH, Becker ES. Specific phobia predicts psychopathology in young women. Soc Psychiatry Psychiatr Epidemiol 2010; 45: 1161–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Loken EK, Hettema JM, Aggen SH, Kendler KS. The structure of genetic and environmental risk factors for fears and phobias. Psychol Med 2014; 44: 2375–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Van Houtem CM, Laine ML, Boomsma DI, Ligthart L, van Wijk AJ, De Jongh A. A review and meta-analysis of the heritability of specific phobia subtypes and corresponding fears. J Anxiety Disord 2013;27: 379–88. [DOI] [PubMed] [Google Scholar]
- 73.Eley TC, Rijsdijk FV, Perrin S, O’Connor TG, Bolton D. A multivariate genetic analysis of specific phobia, separation anxiety and social phobia in early childhood. J Abnorm Child Psychol 2008; 36: 839–48. [DOI] [PubMed] [Google Scholar]
- 74.Lichtenstein P, Annas P. Heritability and prevalence of specific fears and phobias in childhood. J Child Psychol Psychiatry 2000; 41: 927–37. [PubMed] [Google Scholar]
- 75.Sundet JM, Skre I, Okkenhaug JJ, Tambs K. Genetic and environmental causes of the interrelationships between self-reported fears. A study of a non-clinical sample of Norwegian identical twins and their families. Scand J Psychol 2003; 44: 97–106. [DOI] [PubMed] [Google Scholar]
- 76.Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry 2003; 60: 929–37. [DOI] [PubMed] [Google Scholar]
- 77.Hettema JM, Prescott CA, Myers JM, Neale MC, Kendler KS. The structure of genetic and environmental risk factors for anxiety disorders in men and women. Arch Gen Psychiatry 2005; 62: 182–89. [DOI] [PubMed] [Google Scholar]
- 78.Hettema JM, Neale MC, Myers JM, Prescott CA, Kendler KS. A population-based twin study of the relationship between neuroticism and internalizing disorders. Am J Psychiatry 2006; 163: 857–64. [DOI] [PubMed] [Google Scholar]
- 79.Bienvenu OJ, Hettema JM, Neale MC, Prescott CA, Kendler KS. Low extraversion and high neuroticism as indices of genetic and environmental risk for social phobia, agoraphobia, and animal phobia. Am J Psychiatry 2007; 164: 1714–21. [DOI] [PubMed] [Google Scholar]
- 80.Choy Y, Fyer AJ, Lipsitz JD. Treatment of specific phobia in adults. Clin Psychol Rev 2007; 27: 266–86. [DOI] [PubMed] [Google Scholar]
- 81.Wolitzky-Taylor KB, Horowitz JD, Powers MB, Telch MJ. Psychological approaches in the treatment of specific phobias: a meta-analysis. Clin Psychol Rev 2008; 28: 1021–37. [DOI] [PubMed] [Google Scholar]
- 82.Rothbaum BO, Hodges LF, Kooper R, Opdyke D, Williford JS, North M. Effectiveness of computer-generated (virtual reality) graded exposure in the treatment of acrophobia. Am J Psychiatry 1995; 152: 626–28. [DOI] [PubMed] [Google Scholar]
- 83.Arroll B, Wallace HB, Mount V, Humm SP, Kingsford DW. A systematic review and meta-analysis of treatments for acrophobia. Med J Aust 2017; 206: 263–67. [DOI] [PubMed] [Google Scholar]
- 84.Öst LG. One-session treatments for a case of multiple simple phobias. Scand J Behav Ther 1987; 16: 175–84. [Google Scholar]
- 85.Öst LG. One-session treatment for specific phobias. Behav Res Ther 1989; 27: 1–7. [DOI] [PubMed] [Google Scholar]
- 86.Öst LG, Brandberg M, Alm T. One versus five sessions of exposure in the treatment of flying phobia. Behav Res Ther 1997; 35: 987–96. [DOI] [PubMed] [Google Scholar]
- 87.Öst LG, Hellström K, Kåver A. One versus five sessions of exposure in the treatment of injection phobia. Behav Ther 1992; 23: 263–81. [Google Scholar]
- 88.Öst LG, Alm T, Brandberg M, Breitholtz E. One vs five sessions of exposure and five sessions of cognitive therapy in the treatment of claustrophobia. Behav Res Ther 2001; 39: 167–83. [DOI] [PubMed] [Google Scholar]
- 89.Abramowitz JS. The practice of exposure therapy: relevance of cognitive-behavioral theory and extinction theory. Behav Ther 2013; 44: 548–58. [DOI] [PubMed] [Google Scholar]
- 90.Watson JP, Gaind R, Marks IM. Prolonged exposure: a rapid treatment for phobias. BMJ 1971; 1: 13–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bouton ME. Context, ambiguity, and unlearning: sources of relapse after behavioral extinction. Biol Psychiatry 2002; 52: 976–86. [DOI] [PubMed] [Google Scholar]
- 92.Lipsitz JD, Mannuzza S, Klein DF, Ross DC, Fyer AJ. Specific phobia 10–16 years after treatment. Depress Anxiety 1999; 10: 105–11. [PubMed] [Google Scholar]
- 93.Rodriguez BI, Craske MG, Mineka S, Hladek D. Context-specificity of relapse: effects of therapist and environmental context on return of fear. Behav Res Ther 1999; 37: 845–62. [DOI] [PubMed] [Google Scholar]
- 94.Vervliet B, Craske MG, Hermans D. Fear extinction and relapse: state of the art. Annu Rev Clin Psychol 2013; 9: 215–48. [DOI] [PubMed] [Google Scholar]
- 95.Bandarian-Balooch S, Neumann DL, Boschen MJ. Exposure treatment in multiple contexts attenuates return of fear via renewal in high spider fearful individuals.J Behav Ther Exp Psychiatry 2015; 47: 138–44. [DOI] [PubMed] [Google Scholar]
- 96.Dunsmoor JE, Ahs F, Zielinski DJ, LaBar KS. Extinction in multiple virtual reality contexts diminishes fear reinstatement in humans. Neurobiol Learning Mem 2014; 113: 157–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Shiban Y, Pauli P, Mühlberger A. Effect of multiple context exposure on renewal in spider phobia. Behav Res Ther 2013; 51: 68–74. [DOI] [PubMed] [Google Scholar]
- 98.Shiban Y, Schelhorn I, Pauli P, Mühlberger A. Effect of combined multiple contexts and multiple stimuli exposure in spider phobia: a randomized clinical trial in virtual reality. Behav Res Ther 2015; 71: 45–53. [DOI] [PubMed] [Google Scholar]
- 99.Davis M Role of NMDA receptors and MAP kinase in the amygdala in extinction of fear: clinical implications for exposure therapy. Eur J Neurosci 2002; 16: 395–98. [DOI] [PubMed] [Google Scholar]
- 100.Ressler KJ, Rothbaum BO, Tannenbaum L, et al. Cognitive enhancers as adjuncts to psychotherapy: use of D-cycloserine in phobic individuals to facilitate extinction of fear. Arch Gen Psychiatry 2004; 61: 1136–44. [DOI] [PubMed] [Google Scholar]
- 101.Mataix-Cols D, Fernández de la Cruz L, Monzani B, et al. D-cycloserine augmentation of exposure-based cognitive behavior therapy for anxiety, obsessive-compulsive, and posttraumatic stress disorders: a systematic review and meta-analysis of individual participant data. JAMA Psychiatry 2017; 74: 501–10. [DOI] [PubMed] [Google Scholar]
- 102.de Quervain DJ, Bentz D, Michael T, et al. Glucocorticoids enhance extinction-based psychotherapy. Proc Natl Acad Sci USA 2011;108: 6621–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Soravia LM, Heinrichs M, Winzeler L, et al. Glucocorticoids enhance in vivo exposure-based therapy of spider phobia. Depress Anxiety 2014; 31: 429–35. [DOI] [PubMed] [Google Scholar]


