Abstract
In December 2019, an outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection occurred in Wuhan, Hubei Province, China and spread across China and beyond. On February 12, 2020, WHO officially named the disease caused by the novel coronavirus as Coronavirus Disease 2019 (COVID-19). Since most COVID-19 infected patients were diagnosed with pneumonia and characteristic CT imaging patterns, radiological examinations have become vital in early diagnosis and assessment of disease course. To date, CT findings have been recommended as major evidence for clinical diagnosis of COVID-19 in Hubei, China. This review focuses on the etiology, epidemiology, and clinical symptoms of COVID-19, while highlighting the role of chest CT in prevention and disease control.
A full translation of this article in Chinese is available in the supplement. - 请见䃼充资料阅读文章中文版∘
Summary
Radiologists understanding of clinical and chest CT imaging features of coronavirus disease 2019 (COVID-19) will help to detect the infection early and assess the disease course.
Essentials
■ Coronavirus disease 2019 (COVID-19) presents with nonspecific clinical manifestations, so diagnosis depends on epidemiological factors including Wuhan exposure or close contact history.
■ Typical CT findings of COVID-19 include peripherally distributed multifocal ground-glass opacities (GGOs) with patchy consolidations and posterior part or lower lobe involvement predilection
■ Increasing numbers, extent, and density of GGOs on CT indicate disease progression.
■ Thin-slice chest CT plays a vital role in early detection, observation, and disease evaluation.
Introduction
An ongoing outbreak of pneumonia associated with a novel coronavirus, called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was reported in Wuhan, Hubei province, China (1-3) in December 2019. In the following weeks, infections spread across China and other countries around the world (4-6). The Chinese public health, clinical, and scientific communities took prompt response to allow for timely recognition of the new virus and shared the viral gene sequence to the world (2,7). On January 30, 2020, the World Health Organization (WHO) declared the outbreak a Public Health Emergency of International Concern (PHEIC) (8). On February 12, 2020, WHO named the disease caused by the novel coronavirus as Coronavirus Disease 2019 (COVID-19) (9). A group of international experts, with a range of specializations, has worked with Chinese counterparts to try to contain the outbreak (10).
At present, real-time reverse-transcription–polymerase-chain-reaction (RT-PCR) assay for COVID-19 has been developed and used in clinics. Although RT-PCR remains the reference standard to make a definitive diagnose of COVID-19 infection (11), the high false negative rate (12) and unavailability of RT-PCR assay in the early stage of the outbreak restricted prompt diagnosis of infected patients. Radiological examinations, especially thin slice chest CT, play an important role in fighting this infectious disease (13). Chest CT can identify the early phase lung infection (14-15) and prompt larger public health surveillance and response systems (16). Currently, chest CT findings have been recommended as major evidence for confirmed clinical diagnosis in Hubei, China. The addition of chest CT for diagnosis resulted in 14840 confirmed new cases (13332 clinically diagnosed cases) reported on February 13, 2020. Comprehensive and timely review of radiological role in fighting CIVID-19 remains urgent and mandatory.
Etiology
In preliminary report, complete viral genome analysis reveals that the virus shares 88% sequence identity to two bat-derived severe acute respiratory syndrome (SARS)-like coronaviruses, but more distant from severe acute respiratory syndrome coronavirus (SARS-CoV) (17). Hence, it was temporarily called 2019-novel coronavirus (2019-nCoV). Coronavirus is an enveloped and single-stranded ribonucleic acid named for its solar corona like appearance due to 9-12 nm-long surface spikes (18). There are four major structural proteins encoded by the coronaviral genome on the envelope, one of which is the spike (S) protein that binds to angiotensin-converting enzyme 2 (ACE2) receptor and mediates subsequent fusion between the envelope and host cell membranes to aid viral entry into the host cell (19,20). On February 11, 2020, the Coronavirus Study Group (CSG) of the International Committee on Taxonomy of Viruses finally designated it as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) based on phylogeny, taxonomy and established practice (21). Soon later, WHO named the disease caused by this coronavirus as Coronavirus Disease 2019 (COVID-19) (9). On the basis of current data, it seems that COVID-19 might be initially hosted by bats, and might have been transmitted to humans via pangolin (22) or other wild animals (17,23) sold at the Huanan seafood market but subsequent spread via human-to-human transmission.
Epidemiology
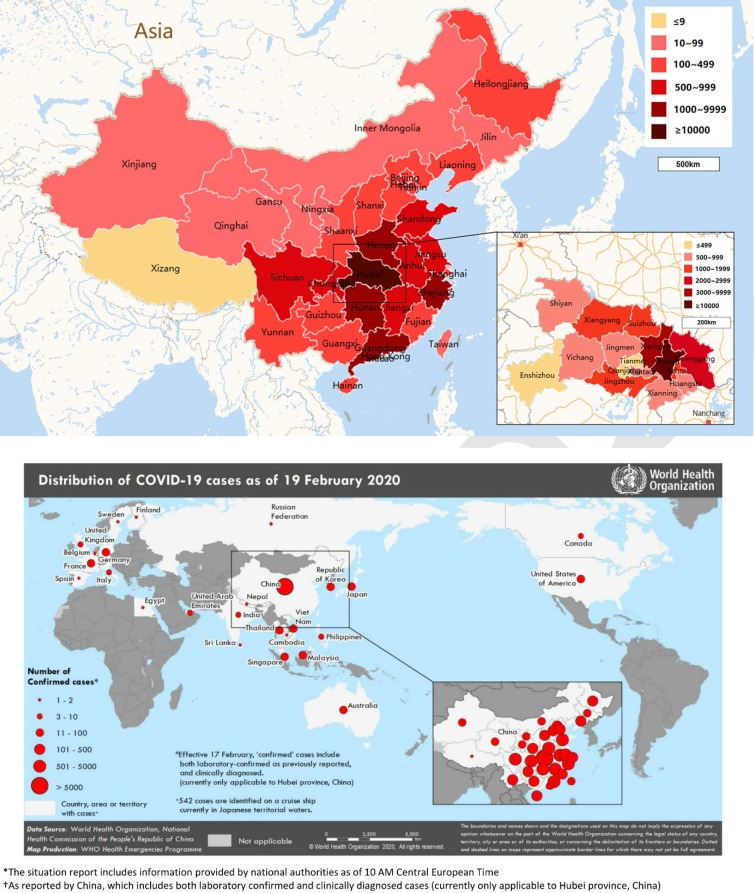
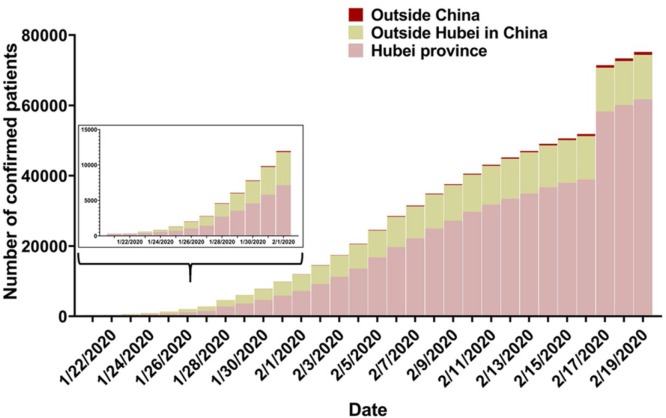
On December, 2019, the earliest symptom onset of confirmed patients appeared (24). At first, the morbidity remained low but reached a tipping point in the middle of January 2020. During the second half of this month, a remarkable increase of infected patients in affected cities occurred outside Hubei province because of the population movement before lunar Chinese New Year (25). Followed by an exponential growth until January 23, 2020, the outbreak spread to the other countries, attracting extensive attention around the world (Figure 1). Evidence of clusters of infected family members and medical workers confirmed the presence of human-to-human transmission (12) by droplets, contact and fomite (26-27). So far, there is no definite evidence for intrauterine infection (28). Current estimates are that COVID-19 has a median incubation period of 3 days (range 0 to 24 days), with potential asymptomatic transmission (26, 29). At the end of January 2020, WHO confirmed more than ten thousand cases infected with COVID-19 across China (30). On February 13, 2020, 13332 new clinically diagnosed cases were firstly reported from Hubei. Official reports included clinically diagnosed cases and laboratory-confirmed cases because chest CT findings are recommended as the major evidence for clinically confirmed cases by Diagnosis and Treatment Program of 2019 New Coronavirus Pneumonia (trial Fifth version) by National Health and Health Commission of China in 2020 (13). As of February 19, 2020, this rose to a total of 74280 confirmed cases in China and 924 confirmed cases in 24 countries outside China, and a total of 2009 deaths globally (10) (Figure 2). To control COVID-19, effective prevention and control measurements must include early detection, diagnosis, treatment, and quarantine to block human-to-human transmission as well as reducing secondary infections among close contacts and health care workers (10).
Figure 1:
Countries, territories, or areas with confirmed cases of Coronavirus Disease 2019 (COVID-19). a: The geographic location of patients with confirmed COVID-19 in China, February 19, 2020. b: Countries, territories or areas with reported confirmed COVID-19, February 19, 2020. Note.—Data in Panel a is from World Health Organization, National Health Commission of the People’s Republic of China; Panel b is adapted from Ref. 10.
Figure 2a:
Tendency chart of confirmed cases, new cases, and deaths of Coronavirus Disease 2019 (COVID-19) a: The tendency chart of confirmed patients from Hubei to the areas outside Hubei in China and countries outside China. b: The tendency chart of new cases of confirmed patients and deaths in China. Note.—Data are from World Health Organization, National Health Commission of the People’s Republic of China. The patients were laboratory-confirmed cases before February, 17, 2020; and included clinically diagnosed cases then.
Figure 2b:
Tendency chart of confirmed cases, new cases, and deaths of Coronavirus Disease 2019 (COVID-19) a: The tendency chart of confirmed patients from Hubei to the areas outside Hubei in China and countries outside China. b: The tendency chart of new cases of confirmed patients and deaths in China. Note.—Data are from World Health Organization, National Health Commission of the People’s Republic of China. The patients were laboratory-confirmed cases before February, 17, 2020; and included clinically diagnosed cases then.
Clinical Symptom Spectrum
Understanding the clinical symptoms of COVID-19 is important, although the clinical symptoms are indicated nonspecific. Common symptoms include fever, cough and myalgia or fatigue. Patients may initially present with diarrhea and nausea a few days prior to fever, suggesting fever is dominant but not the premier symptom of infection. A small number of patients can have headache or hemoptysis (26,32) and even relatively asymptomatic (12). Affected older men with comorbidities are more likely to have respiratory failure due to severe alveolar damage (31). Disease onset may show rapid progression to organ dysfunction (e.g., shock, acute respiratory distress syndrome [ARDS], acute cardiac injury, and acute kidney injury) and even death in severe cases (1,32). Meanwhile, patients might show normal or lower white blood cell counts, lymphopenia, or thrombocytopenia, with extended activated thromboplastin time and increased C-reactive protein level (1,26,31-32). In short, a patient having fever and upper respiratory tract symptoms with lymphopenia or leukopenia should be suspected, especially for patients with Wuhan exposure or close contact history.
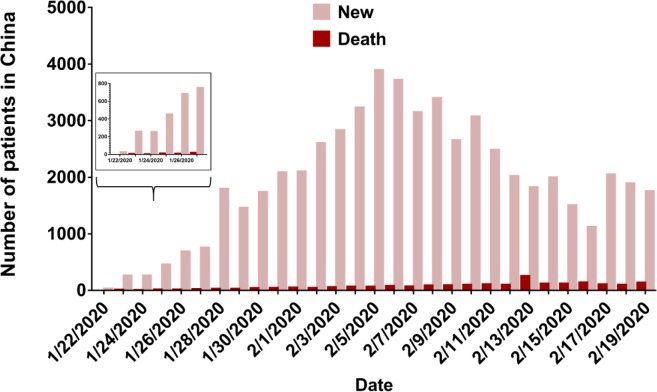
Diagnosis of COVID-19 Infection
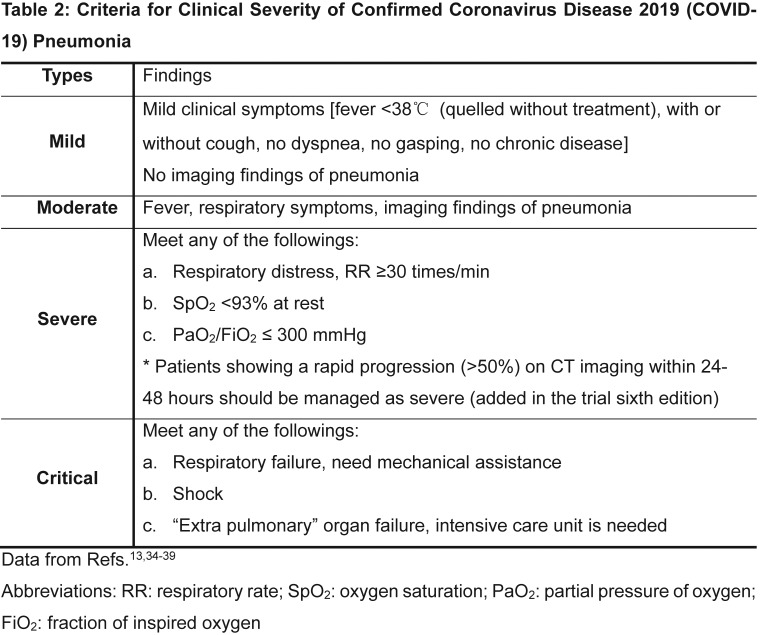
The first task for the clinical diagnostic workflow is to confirm Wuhan exposure history or close contact with people from Wuhan or confirmed patients during the past two weeks. However, the number of the patients with unknown exposure history is increasing due to the rapid and wide spread of the disease. The National Health Commission of China (33,34) formulated the Diagnosis and Treatment Program of 2019 New Coronavirus Pneumonia (trial sixth version) (Table 1) based on the recommendations of the World Health Organization (WHO) on severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) (35-37). A patient with one exposure history and two clinical conditions is considered as suspected case. If there is no clear exposure history, suspected patients should meet 3 clinical conditions (Table 1). Based on the fifth trial edition (13), chest CT findings of viral pneumonia are regarded as evidence of clinical diagnosis of COVID-19 infection. However, the WHO did not accept CT without RT-PCR confirmation until February, 17, 2020 (38) and the most recently published Diagnosis and Treatment Program of 2019 New Coronavirus Pneumonia (trial sixth version) has deleted the term of clinical diagnosis (34). The final etiology diagnosis of COVID-19 is necessary, which can be further confirmed by positive real-time RT-PCR assay for COVID-19 using respiratory or blood samples or by viral gene sequencing of respiratory or blood samples that are highly homologous with COVID-19. According to the clinical manifestations, confirmed patients are divided into mild, moderate, severe, and critical types (Table 2) (13,34, 39).
Table 1:
Case Definition for Surveillance of Coronavirus Disease 2019 (COVID-19) by Chinese Health Commission
Table 2:
Criteria for Clinical Severity of Confirmed Coronavirus Disease 2019 (COVID-19) Pneumonia
The Role of Radiology in Detection of COVID-19
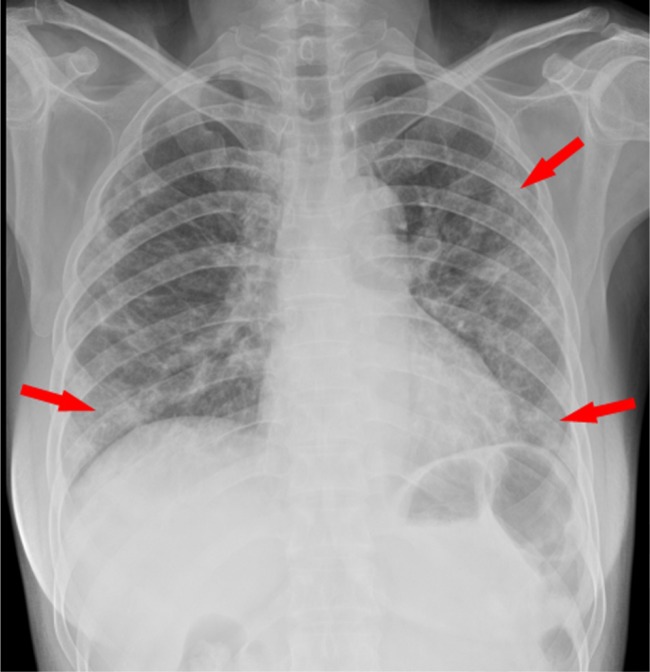
Radiological examinations are of great importance in the early detection and management of COVID-19. Because chest radiography is not sensitive for the detection of ground-glass opacity (GGO) and may demonstrate normal findings in early stage of infection (16), it was not recommended as the first-line imaging modality for COVID-19. However, bilateral multifocal consolidation (Figure 3) can be seen in severe patients, partially fused into massive consolidation with small pleural effusions and even presenting with “white lung” (11). Thin slice chest CT functions more effectively in early detection of COVID-19 pneumonia (12,16). The largest sample study to date showed that among 3665 confirmed cases, 95.5% (n=3498) patients were diagnosed as pneumonia (25). Pan et al (40) reviewed 21 confirmed patients who underwent repeated CT at approximately 4 day intervals and found that negative findings were revealed in four patients on early stage (0-4 days after onset of the initial symptom), but repeat chest CT showed lung abnormalities in all of these 4 patients.
Figure 3:
Chest radiography of confirmed Coronavirus Disease 2019 (COVID-19) pneumonia A 53-year-old female had fever and cough for 5 days. Multifocal patchy opacities can be seen in both lungs (arrows).
CT Imaging Findings
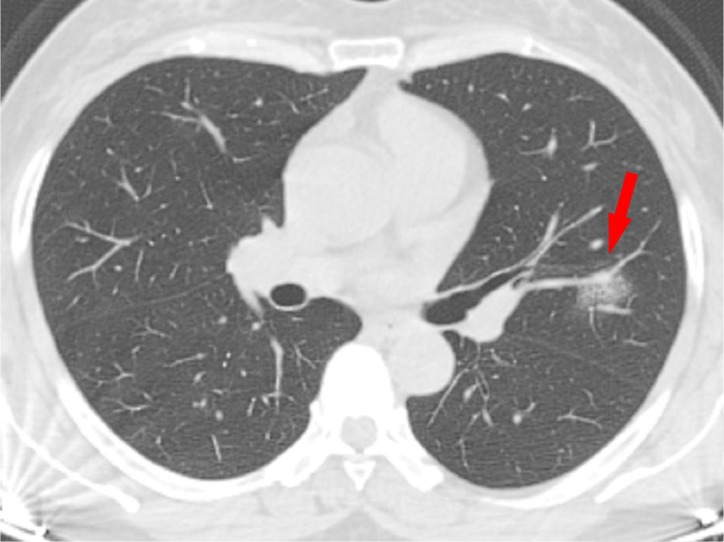
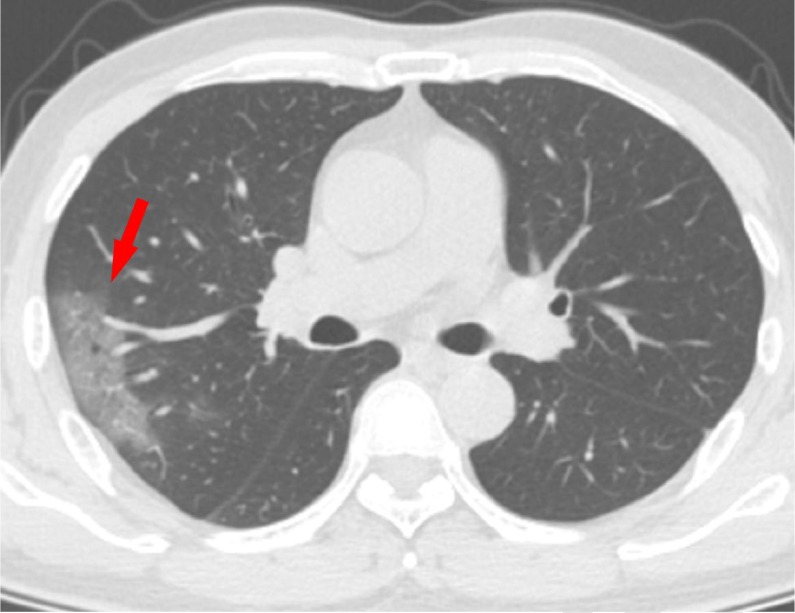
To date, only five case series studies (16,40-43) and some case reports (44-54) have investigated the chest CT imaging features of COVID-19 pneumonia. COVID-19 pneumonia has nonspecific and various chest CT imaging features. The typical chest CT findings include multifocal bilateral GGOs with patchy consolidations, prominent peripherally subpleural distribution and preferred posterior part or lower lobe predilection (Figures 4-9) (14,55-56). GGO is a hazy increase in attenuation that appears in a variety of interstitial and alveolar processes with preservation of the bronchial and vascular margins (57), while consolidation is an area of opacification obscuring the margins of vessels and airway walls (58). In patients with COVID-19 pneumonia, focal or multifocal pure GGO (Figures 4a, 5, 6b) and GGO with reticular and/or interlobular septal thickening as typical crazy-paving pattern (Figure 6a) were often observed, while pure consolidation (Figure 7) was relatively less common or absent (16,40-42). Pure GGO lesions (Figure 4a, 5, 9b) can be the early appearance of COVID-19 pneumonia. Chung et al. (41) found one patient with an initial normal chest CT that evolved into a new solitary, rounded peripheral GGO after three days. The reversed CT halo sign defined as a rounded area of ground glass surrounded by a complete or almost complete ring of consolidation can also be observed (16,49). Pleural effusion, lung cavitation, lymphadenopathy and calcification are rarely reported (40-44,49-50). Table 3 summarizes the characteristic chest CT imaging features of COVID-19 pneumonia.
Figure 4a:
CT findings of confirmed Coronavirus Disease 2019 (COVID-19) pneumonia Solitary rounded ground-glass opacity (GGO) pattern. A 51-year-old woman presenting without fever had close contact with patients with lab-confirmed COVID-19. a, Baseline axial unenhanced chest CT acquired 6 days before the first positive RT-PCR test showed a rounded GGO in the left lung upper lobe (arrow). b. Follow-up chest CT 4 days later showed the size increase of the lesion (arrow).
Figure 9a:

CT findings of confirmed Coronavirus Disease 2019 (COVID-19) pneumonia showing disease progression A 48-year-old woman presented with high fever (39.1 °C, 102.38℉) and Wuhan exposure history. a-b, On January 23, 2020, baseline axial unenhanced chest CT showed ground-glass opacity (GGO) with consolidation in lower lobe of right lung with typical air bronchogram (Panel a, arrow) and one pure GGO (Panel b, arrow) in the upper lobe of left lung. c-d, Three days later, follow-up axial unenhanced chest CT showed the disease progression, appearing as increased extent and consolidation (arrows) compared with baseline chest CT.
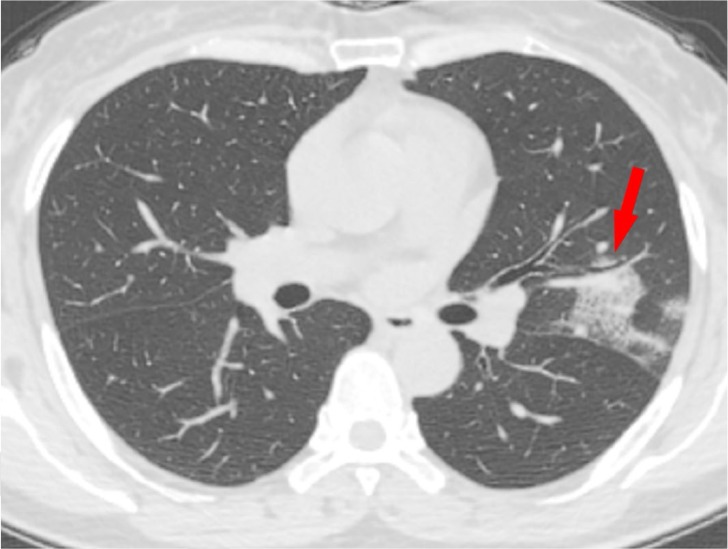
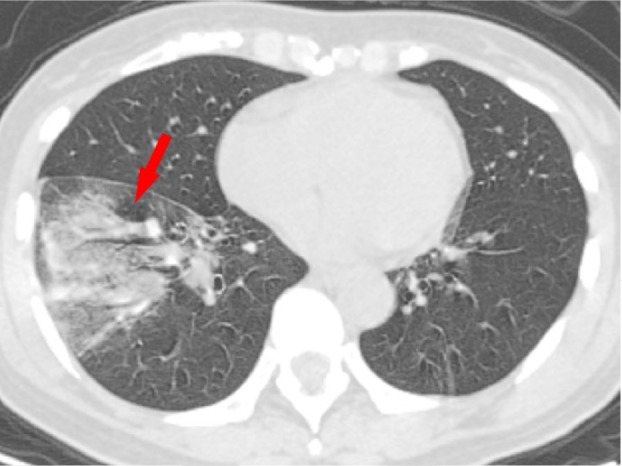
Figure 5:
CT findings of confirmed Coronavirus Disease 2019 (COVID-19) pneumonia Patchy GGO pattern. A 58-old-year man with close contact history presenting without fever. Axial unenhanced chest CT showed patchy pure GGO (arrow).
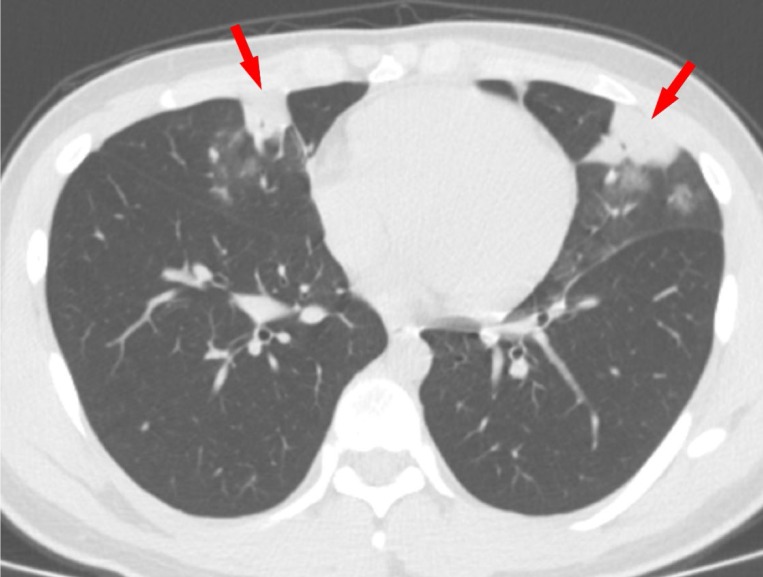
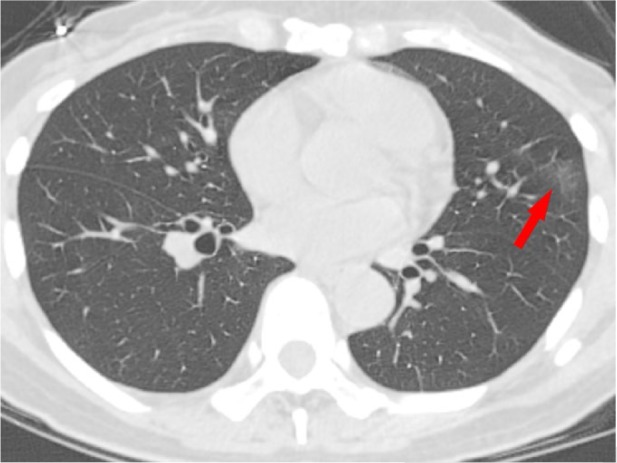
Figure 6b:
CT findings of confirmed Coronavirus Disease 2019 (COVID-19) pneumonia Crazy paving pattern. A 69-old-year woman presenting with fever, cough, and muscle soreness with Wuhan exposure history. a, Axial unenhanced chest CT acquired on January 26, 2020 showed patchy GGO with typical crazy paving pattern (arrow). b, Axial unenhanced chest CT acquired on January 31, 2020 showed multiple subpleural distributed GGOs (arrows).
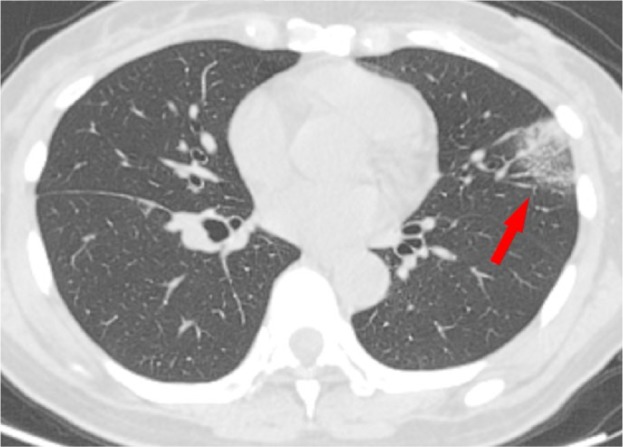
Figure 6a:
CT findings of confirmed Coronavirus Disease 2019 (COVID-19) pneumonia Crazy paving pattern. A 69-old-year woman presenting with fever, cough, and muscle soreness with Wuhan exposure history. a, Axial unenhanced chest CT acquired on January 26, 2020 showed patchy GGO with typical crazy paving pattern (arrow). b, Axial unenhanced chest CT acquired on January 31, 2020 showed multiple subpleural distributed GGOs (arrows).
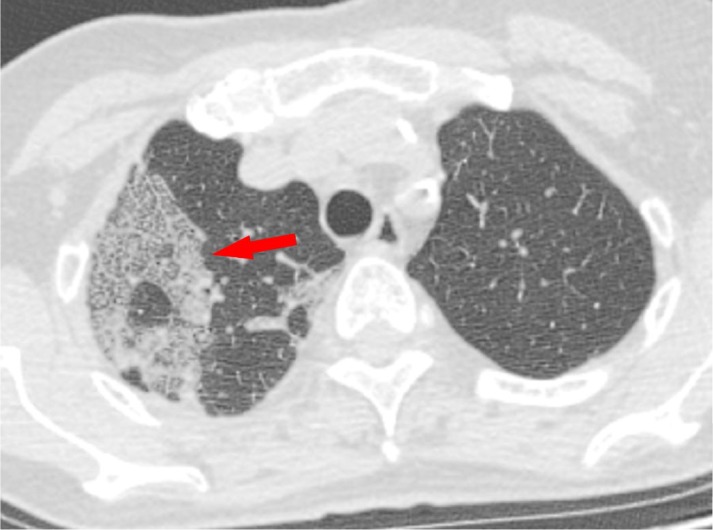
Figure 7:
CT findings of confirmed Coronavirus Disease 2019 (COVID-19) pneumonia Consolidation pattern. A 17-year-old male presented with fever (38.1°C, 100.58°F), cough for three days, and Wuhan exposure history. Axial unenhanced chest CT acquired on January 27, 2020 showed multiple pure consolidation lesions (arrows) in the middle lobe of right lung and upper lobe of left lung.
Figure 9b:
CT findings of confirmed Coronavirus Disease 2019 (COVID-19) pneumonia showing disease progression A 48-year-old woman presented with high fever (39.1 °C, 102.38℉) and Wuhan exposure history. a-b, On January 23, 2020, baseline axial unenhanced chest CT showed ground-glass opacity (GGO) with consolidation in lower lobe of right lung with typical air bronchogram (Panel a, arrow) and one pure GGO (Panel b, arrow) in the upper lobe of left lung. c-d, Three days later, follow-up axial unenhanced chest CT showed the disease progression, appearing as increased extent and consolidation (arrows) compared with baseline chest CT.
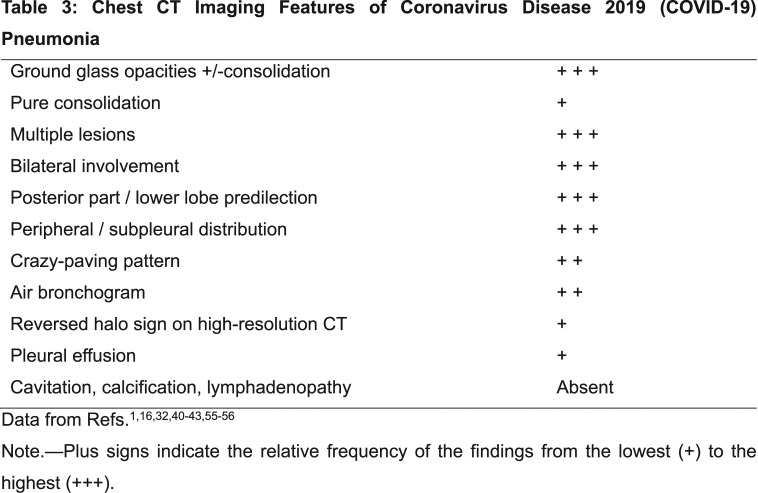
Table 3:
Chest CT Imaging Features of Coronavirus Disease 2019 (COVID-19) Pneumonia
Figure 4b:
CT findings of confirmed Coronavirus Disease 2019 (COVID-19) pneumonia Solitary rounded ground-glass opacity (GGO) pattern. A 51-year-old woman presenting without fever had close contact with patients with lab-confirmed COVID-19. a, Baseline axial unenhanced chest CT acquired 6 days before the first positive RT-PCR test showed a rounded GGO in the left lung upper lobe (arrow). b. Follow-up chest CT 4 days later showed the size increase of the lesion (arrow).
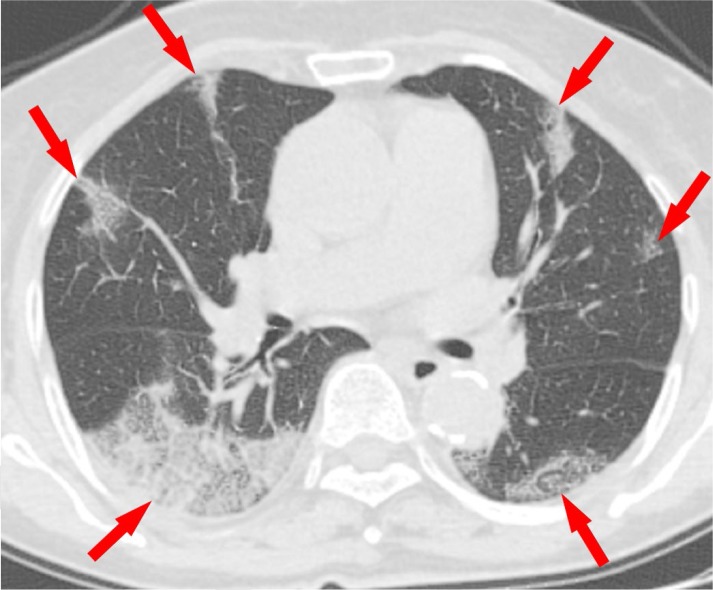
Figure 8a:
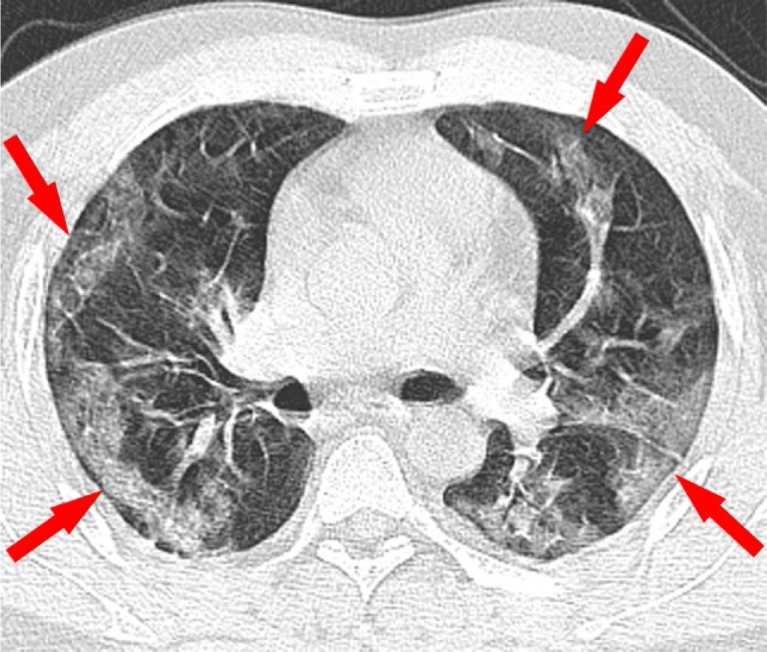
CT findings of severe type confirmed Coronavirus Disease 2019 (COVID-19) pneumonia A 43-year-old man presented with no fever and Wuhan exposure history. Axial unenhanced chest CT was acquired on the same day as reverse-transcription–polymerase-chain-reaction. a-b. Two thin slice axial unenhanced chest CT images showed diffusely subpleural distributed ground-glass opacities (arrows). Images provided by courtesy of Dr. Wei Chen, Department of Radiology, The Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University, Zhejiang, China.
Figure 8b:
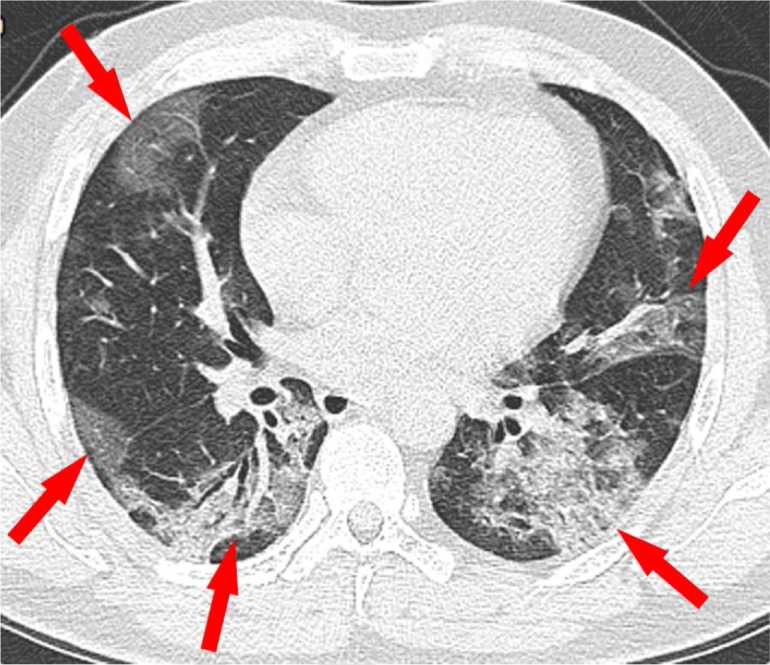
CT findings of severe type confirmed Coronavirus Disease 2019 (COVID-19) pneumonia A 43-year-old man presented with no fever and Wuhan exposure history. Axial unenhanced chest CT was acquired on the same day as reverse-transcription–polymerase-chain-reaction. a-b. Two thin slice axial unenhanced chest CT images showed diffusely subpleural distributed ground-glass opacities (arrows). Images provided by courtesy of Dr. Wei Chen, Department of Radiology, The Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University, Zhejiang, China.
Figure 9c:
CT findings of confirmed Coronavirus Disease 2019 (COVID-19) pneumonia showing disease progression A 48-year-old woman presented with high fever (39.1 °C, 102.38℉) and Wuhan exposure history. a-b, On January 23, 2020, baseline axial unenhanced chest CT showed ground-glass opacity (GGO) with consolidation in lower lobe of right lung with typical air bronchogram (Panel a, arrow) and one pure GGO (Panel b, arrow) in the upper lobe of left lung. c-d, Three days later, follow-up axial unenhanced chest CT showed the disease progression, appearing as increased extent and consolidation (arrows) compared with baseline chest CT.
Figure 9d:
CT findings of confirmed Coronavirus Disease 2019 (COVID-19) pneumonia showing disease progression A 48-year-old woman presented with high fever (39.1 °C, 102.38℉) and Wuhan exposure history. a-b, On January 23, 2020, baseline axial unenhanced chest CT showed ground-glass opacity (GGO) with consolidation in lower lobe of right lung with typical air bronchogram (Panel a, arrow) and one pure GGO (Panel b, arrow) in the upper lobe of left lung. c-d, Three days later, follow-up axial unenhanced chest CT showed the disease progression, appearing as increased extent and consolidation (arrows) compared with baseline chest CT.
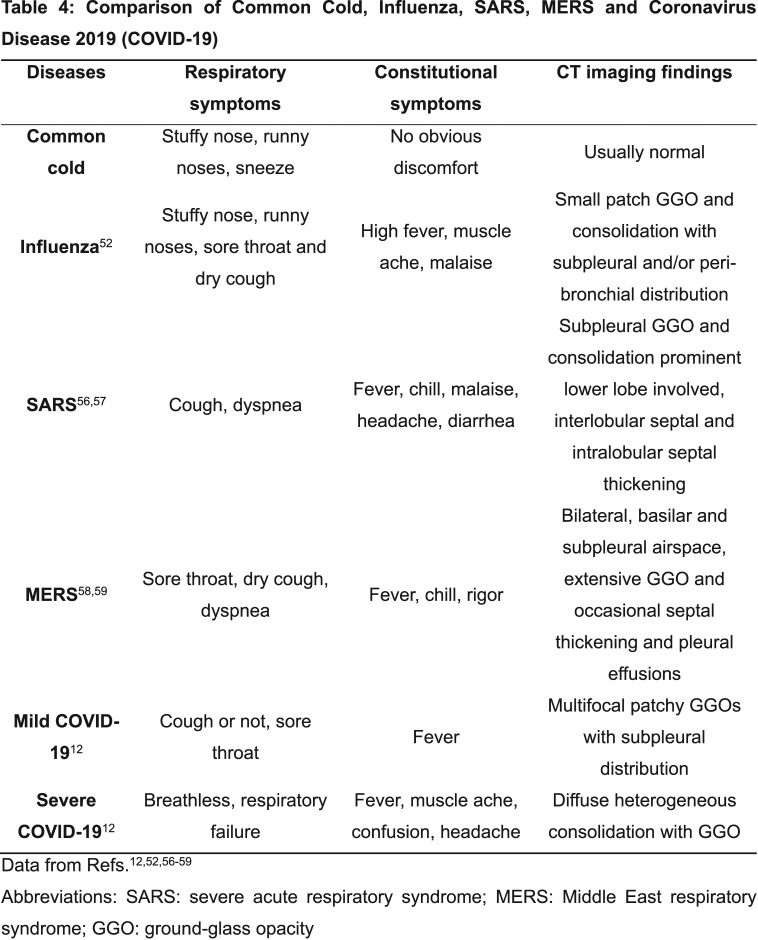
Other diseases mimic COVID-19 pneumonia and should be differentiated, including community-acquired pneumonia such as streptococcus pneumonia, mycoplasma and chlamydia related pneumonia, and other coronavirus infections. Differential diagnosis is very important to early quarantine suspected patients with fever and reduce cross infection. Table 4 shows typical clinical and imaging findings of COVID-19 mimics such as common cold, influenza, and other coronaviruses diseases including SARS and MERS (11,59-63). Wuhan exposure history or close contact with confirmed or suspected patients is an essential clue for the diagnosis. However, for patients with unknown epidemiological history, typical clinical and imaging appearance can indicate suspected COVID-19; RT-PCR test should be performed in these patients. In summary, the diagnosis of COVID-19 should combine epidemiological history, clinical and imaging manifestations, and RT-PCR test (the reference standard).
Table 4:
Comparison of Common Cold, Influenza, SARS, MERS and Coronavirus Disease 2019 (COVID-19)
The Value of Radiology in Prevention and Control of COVID-19
Although chest CT findings are nonspecific for COVID-19 detection, CT findings have been recommended as major evidence of clinical diagnosis in Hubei province by the National Health and Health Commission of China (13). RT-PCR positive for COVID-19 remains the reference standard (11), but RT-PCR results can be affected by sampling errors and low virus load (64-66). Previous SARS studies (67-69) showed that RT-PCR lacked sensitivity during the first five days of the disease. Current reports show that chest CT may demonstrate pneumonia but multiple RT-PCR tests of nasopharyngeal or throat swabs test negative (12,53,70-71), and Fang et al. (72) compared the detection rate of initial chest CT and RT-PCR and reported a higher detection rate for initial CT (50/51[98%]) than first RT-PCR (36/51[71%]) patients (P<0.001). Xie et al. found that of 167 patients evaluated, 3% (5/167) patients had initially negative RT-PCR but positive chest CT and both RT-PCR and CT were concordant for COVID19 in 92.8% (n=155/167) patients (70). Furthermore, RT-PCR results must be checked by the Centers for Disease Control and Prevention (CDC) in the early stage of an outbreak, taking a longer time to confirm the final diagnosis (25). Thin slice chest CT is easy to perform, fast, and detects early COVID-19 pneumonia with high sensitivity, providing valuable information for further diagnosis, while aiding prevention and control of COVID-19.
CT can also assess the disease severity of COVID-19 to guide clinical management. Clinical observations showed (1) that intensive care unit (ICU) patients on admission often presented with bilateral multiple lobular and subsegmental consolidation, while non-ICU patients presented with bilateral GGOs and subsegmental consolidation. In severe patients, CT can demonstrate diffuse heterogeneous consolidation with GGOs in bilateral lungs with air bronchial sign and bronchiectasis (Figure 9), presenting as “white lung” when most lung lobes are affected (15). Patients also may present with thickening of interlobar septa and bilateral pleura with a small pleural effusion (11,56).
Additionally, CT surveils disease time course of COVID-19. Chung et al. (41) found that 7 of 8 patients showed marked progression presenting as increasing number, extent, and density of GGOs (Figures 4, 9). Pan et al (40) reviewed 21 confirmed and recovered patients who underwent repeated CT at approximately 4-day intervals and summarized four stages of the disease: early, progressive, peak, and absorption. They found that GGOs will rapidly grow, demonstrating consolidation and crazy-paving pattern as the disease progresses. The lesions will absorb without crazy-paving pattern on absorption stage, suggesting crazy-paving pattern as another index to evaluate the disease course. The study by Song et al (42) concluded that greater consolidation indicated disease progression. Some case reports showed that smaller size, extent, and absorption of these lesions indicate the improvement (32,42,51-53).
Conclusion
In conclusion, characteristic chest CT imaging features and Wuhan exposure or close contact history, highly suggest COVID-19 pneumonia, although RT-PCR remains the reference standard. Typical CT features of COVID-19 pneumonia include multifocal bilateral GGOs with patchy consolidations, prominent peripherally subpleural distribution, and preferred posterior part or lower lobe predilection. Thin slice chest CT can help prompt diagnosis, guide clinical decision making, and monitor disease progression, playing a critical role in the early prevention and control of COVID-19. Special attention should be paid to the role of radiologists in fighting this new infectious disease.
APPENDIX
Conflicts of interest: All authors have no conflicts of interest to disclose.
Drs Zu and Jiang had equal contributions to this work.
Supported by The National Key Research and Development Program of China (2017YFC0113400 for L.J.Z.).
Abbreviations:
- ARDS
- acute respiratory distress syndrome
- COVID-19
- Coronavirus Disease 19
- GGO
- ground-glass opacity
- MERS
- Middle East respiratory syndrome
- RT-PCR
- reverse-transcription–polymerase-chain-reaction
- SARS
- severe acute respiratory syndrome
- SARS-CoV-2
- severe acute respiratory syndrome coronavirus 2
References
- 1.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020 Jan 24. pii: S0140-6736(20)30183-5. doi: 10.1016/S0140-6736(20)30183-5. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020 Jan 24. doi: 10.1056/NEJMoa2001017. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-Infected pneumonia. N Engl J Med 2020 Jan 29. doi:10.1056/NEJMoa2001316. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Phan LT, Nguyen TV, Luong QC, et al. Importation and human-to-human transmission of a novel coronavirus in vietnam. NEJM. January 28, 2020. doi: 10.1056/NEJMc2001272. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020 Jan 31. doi: 10.1056/NEJMoa2001191. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Giovanetti M, Benvenuto D, Angeletti S, Ciccozzi M. The first two cases of 2019-nCoV in Italy: where they come from? J Med Virol. 2020 Feb 5. doi: 10.1002/jmv.25699. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020 Feb 3. doi: 10.1038/s41586-020-2008-3. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization . Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). 2020. at https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov). Published January 31, 2020.
- 9.World Health Organization . WHO Director-General's remarks at the media briefing on 2019-nCoV on 11 February 2020. 2020. at https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020. Published February 11, 2020.
- 10.World Health Organization . Coronavirus Disease 2019(COVID-19): situation report—30. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200219-sitrep-30-covid-19.pdf?sfvrsn=6e50645_2. Published February 20, 2020. Accessed February 20, 2020
- 11.Chinese Society of Radiology . Radiological diagnosis of new coronavirus infected pneumonitis: Expert recommendation from the Chinese Society of Radiology (First edition). Chin J Radiol, 2020,54(00): E001-E001. DOI: 10.3760/cma.j.issn.1005-1201.2020.0001. [Google Scholar]
- 12.Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020 Jan 24. pii:S0140-6736(20)30154-9. doi: 10.1016/S0140-6736(20)30154-9. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.General Office of National Health Committee . Office of state administration of traditional Chinese medicine. Notice on the issuance of a programme for the diagnosis and treatment of novel coronavirus (2019-nCoV) infected pneumonia (trial fifth edition) (2020-02-26)[EB/OL]. http://bgs.satcm.gov.cn/zhengcewenjian/2020-02-06/12847.html
- 14.Kanne JP. Chest CT findings in 2019 novel coronavirus (2019-nCoV) infections from Wuhan, China: key points for the radiologist. Radiology. 2020 Feb 4:200241. doi:10.1148/radiol.2020200241. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pan Y, Guan H. Imaging changes in patients with 2019-nCov. Eur Radiol. 2020 Feb 6. doi:10.1007/s00330-020-06713-z. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ng M, Lee EYP, Yang J, et al. Imaging profile of the COVID-19 infection: Radiologic findings and literature review. Radiology: Cardiothoracic Imaging 2020;2(1):e200034. doi:10.1148/ryct.2020200034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020 Jan 30:S0140-6736(20)30251-8. doi: 10.1016/S0140-6736(20)30251-8. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang Q, Wang YH, Ma JC, et al. Description of the first strain of 2019-nCoV, C-Tan-nCoV Wuhan Strain — National Pathogen Resource Center, China, 2020. 2020. at http://weekly.chinacdc.cn/en/article/id/e3a460f1-661b-4180-b562-ecd8e9502082. [PMC free article] [PubMed]
- 19.Kirchdoerfer RN, Cottrell CA, Wang N, et al. Pre-fusion structure of a human coronavirus spike protein. Nature. 2016; 531(7592):118–121. doi: 10.1038/nature17200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu X, Chen P, Wang J, et al. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci China Life Sci. 2020 Jan 21. doi: 10.1007/s11427-020-1637-5. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gorbalenya AE, Baker SC, Baric RS, et al. Severe acute respiratory syndrome-related coronavirus: the species and its viruses – a statement of the coronavirus study group. bioRxiv preprint first posted online February 11, 2020. 2020:2020.2002.2007.937862. doi:10.1101/2020.02.07.937862. Accessed February 12, 2020.
- 22.Lam TTY, Shum MHH, Zhu HC, et al. Identification of 2019-nCoV related coronaviruses in Malayan pangolins in southern China. bioRxiv preprint first posted online February 18, 2020. 2020:2020.2002.2013.945485. doi: 10.1101/2020.02.13.945485. Accessed February 20, 2020.
- 23.Zhang L, Shen FM, Chen F, Lin Z. Origin and evolution of the 2019 novel coronavirus. Clin Infect Dis. 2020 Feb 3:ciaa112. doi: 10.1093/cid/ciaa112. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu Han health committee . Notice on the issuance of unexplained viral pneumonia [EB/OL]. 2020. http://wjw.wuhan.gov.cn/front/web/showDetail/2020010309017.] Published January 3, 2020. Accessed February 8, 2020.
- 25.Yang Y, Lu Q, Liu M, et al. Epidemiological and clinical features of the 2019 novel coronavirus outbreak in China. 10.1101/2020.02.10.20021675. Accessed February 13, 2020. [DOI]
- 26.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of 2019 novel coronavirus infection in China. 10.1101/2020.02.06.20020974. Accessed February 13, 2020. [DOI]
- 27.Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020 Feb 3. doi: 10.1038/s41586-020-2012-7. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen HJ, Guo JJ, Wang C, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. The Lancet. doi:10.1016/s0140-6736(20)30360-3. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 29.Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. NEngl J Med. 2020 Jan 30. doi:10.1056/NEJMc2001468. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Health Organization . Novel coronavirus(2019-nCoV): situation report—12. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200201-sitrep-12-ncov.pdf?sfvrsn=273c5d35_2. Published February 1, 2020. Accessed February 10,2020.
- 31.Chen N, Zhou M, Dong X,et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020Jan 30. pii: S0140-6736(20)30211-7. doi: 10.1016/S0140-6736(20)30211-7. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 32.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020 Feb 7. doi:10.1001/jama.2020.1585. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization . Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected. 2019. At https://www.who.int/csr/disease/coronavirus_infections/InterimGuidance_ClinicalManagement_NovelCoronavirus_11Feb13u.pdf?ua=1&ua=1. Accessed February 11, 2020.
- 34.General Office of National Health Committee . Office of State Administration of Traditional Chinese Medicine. Notice on the issuance of a program for the diagnosis and treatment of novel coronavirus (2019-nCoV) infected pneumonia (trial sixth edition) (2020-02-19) [EB/OL]. http://yzs.satcm.gov.cn/zhengcewenjian/2020-02-19/13221.html]
- 35.World Health Organization . WHO guidelines for the global surveillance of severe acute respiratory syndrome (SARS). 2004. at https://www.who.int/csr/resources/publications/WHO_CDS_CSR_ARO_2004_1.pdf?ua=1. Published January, 2004. Updated October, 2004.
- 36.World Health Organization . Middle East respiratory syndrome case definition for reporting to WHO. 2017. https://www.who.int/csr/disease/coronavirus_infections/mers-interim–case-definition.pdf?ua=1.
- 37.Azhar EI,El-Kafrawy SA, Farraj SA, et al. Evidence for camel-to-human transmission of MERS coronavirus. N Engl J Med 2014; 370(26): 2499-505. [DOI] [PubMed] [Google Scholar]
- 38.World Health Organization . Coronavirus Disease 2019(COVID-19): situation report—28. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200217-sitrep-28-covid-19.pdf?sfvrsn=a19cf2ad_2. Published February 18, 2020. Accessed February 20, 2020
- 39.World Health Organization . Home care for patients with suspected novel coronavirus (nCoV) infection presenting with mild symptoms and management of contacts [EB/OL]. https://www.who.int/publications-detail/home-care-for-patients-with-suspected-novel-coronavirus-(ncov)-infection-presenting-with-mild-symptoms-and-management-of-contacts. Published January 20, 2020. Accessed February 11, 2020
- 40.Pan F, Ye T, Sun P, et al. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology 2020:200370. doi:10.1148/radiol.2020200370. Published February 1, 2020. Accessed February 13, 2020. [DOI] [PMC free article] [PubMed]
- 41.Chung M, Bernheim A, Mei X, et al. CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology. 2020 Feb 4:200230. doi:10.1148/radiol.2020200230. [Epub ahead ofprint] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Song F, Shi N, Shan F, et al. Emerging coronavirus 2019-nCoV pneumonia. Radiology 2020:200274. doi: 10.1148/radiol.2020200274 [Google Scholar]
- 43.Pan Y, Guan H, Zhou S,et al. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. European Radiology 2020. doi: 10.1007/s00330-020-06731-x. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liu T, Huang P, Liu H, et al. Spectrum of chest CT findings in a familial cluster of COVID-19 infection. Radiology: Cardiothoracic Imaging 2020;2(1):e200025. doi:10.1148/ryct.2020200025. Published February 1, 2020. Accessed February 13, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liu P, Tan XZ. 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology 2020:200257. doi: 10.1148/radiol.2020200257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lin X, GongZ, Xiao Z, Xiong J, Fan B, Liu J. Novel coronavirus pneumonia outbreakin2019: computed tomographicfindings in twocases. Korean J Radiol 2020;21. doi: 10.3348/kjr.2020.0078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lei J, Li J, Li X, Qi X. CT imaging of the 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology 2020:200236. doi: 10.1148/radiol.2020200236 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fang Y, Zhang H, Xu Y, Xie J, Pang P, Ji W. CT manifestations of two cases of 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology 2020:200280. doi: 10.1148/radiol.2020200280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kong W, Agarwal PP. Chest imaging appearance of COVID-19 infection. Radiology: Cardiothoracic Imaging. 2020;2(1):e200028. doi: 10.1148/ryct.2020200028. Published February 1, 2020. Accessed February 13, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li X, Zeng X, Liu B, Yu Y. COVID-19 infection presenting with CT halo sign. Radiology: Cardiothoracic Imaging 2020;2(1):e200026. doi: 10.1148/ryct.2020200026. Published February 1, 2020. Accessed February 13, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shi H, Han X, Zheng C. Evolution of CT manifestations in a patient recovered from 2019 novel coronavirus (2019-nCoV) pneumonia in Wuhan, China. Radiology 2020:200269. doi: 10.1148/radiol.2020200269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Duan YN, Qin J. Pre- and posttreatment chest CT findings: 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology 2020:200323. doi: 10.1148/radiol.2020200323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wu Y, Xie Yl, Wang X. Longitudinal CT findings in COVID-19 pneumonia: Case presenting organizing pneumonia pattern. Radiology: Cardiothoracic Imaging 2020;2(1):e200031. doi: 10.1148/ryct.2020200031. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Qian L, Yu J, Shi H. Severe acute respiratory disease in a Huanan seafood market worker: Images of an early casualty. Radiology: Cardiothoracic Imaging 2020;2(1):e200033. doi: 10.1148/ryct.2020200033. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kim H. Outbreak of novel coronavirus (COVID-19): What is the role of radiologists? Eur Radiol 2020. doi: 10.1007/s00330-020-06748-2. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lee KS. Pneumonia associated with 2019 novel coronavirus: can computed tomographic findings help predict the prognosis of the disease? Korean J Radiol 2020;21. 10.3348/kjr.2020.0096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Franquet T. Imaging of pulmonary viral pneumonia. Radiology 2011; 260(1): 18-39. doi: 10.1148/radiol.11092149. [DOI] [PubMed] [Google Scholar]
- 58.Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology 2008; 246(3):697-722. doi:10.1148/radiol.2462070712 [DOI] [PubMed] [Google Scholar]
- 59.Malainou C. Herold S. Influenza. Internist (Berl) 2019; 60(11):1127-1135. doi:10.1007/s00108-019-00670-6 [DOI] [PubMed] [Google Scholar]
- 60.De Wit E, Van Doremalen N, Falzarano D, Munster VJ. SARS and MERS: recent insights into emerging coronaviruses. Nat Rev Microbiol 2016;14(8):523-34. doi: 10.1038/nrmicro.2016.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hui DSC. Severe acute respiratory syndrome: historical, epidemiologic, and clinical features. Infect Dis Clin North Am 2019; 33(4):869-889. doi:10.1016/j.idc.2019.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chan JF, Lau SK, To KK, Cheng VC, Woo PC, Yuen KY. Middle East respiratory syndrome coronavirus: another zoonotic betacoronavirus causing SARS-like Disease. Clin Microbiol Rev 2015; 28(2): 465-522. doi: 10.1128/CMR.00102-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chan JF, Li KS, To KK, Cheng VC, Chen H, Yuen KY. Is the discovery of the novel human betacoronavirus 2c EMC/2012 (HCoV-EMC) the beginning of another SARS-like pandemic? J Infect 2012; 65(6):477-489. doi:10.1016/j.jinf.2012.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Peiris JS, Chu CM, Cheng VC, et al. Clinical progression and viral load in a community outbreak of coronavirus-associated SARS pneumonia: a prospective study. Lancet 2003;361(9371):1767-1772. doi: 10.1016/s0140-6736(03)13412-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hui DSC. Severe acute respiratory syndrome: historical, epidemiologic, and clinical features. Infect Dis Clin North Am 2019; 33(4):869-889. doi:10.1016/j.idc.2019.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.World Health Organization . Guidance on regulations for the transport of infectious substances 2019–2020. 2019. At https://www.who.int/ihr/publications/WHO-WHE-CPI-2019.20/en/.
- 67.Poon LL, Chan KH, Wong OK, et al. Early diagnosis of SARS coronavirus infection by real time RT-PCR. J Clin Virol 2003; 28(3):233-238. doi: 10.1016/j.jcv.2003.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ng EK, Hui DS, Chan KC, et al. Quantitative analysis and prognostic implication of SARS coronavirus RNA in the plasma and serum of patients with severe acute respiratory syndrome. Clin Chem 2003;49(12):1976-1980. doi:10.1373/clinchem.2003.024125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ng EK, Ng PC, Hon KL, et al. Serial analysis of the plasma concentration of SARS coronavirus RNA in pediatric patients with severe acute respiratory syndrome. Clin Chem 2003; 49(12):2085-2088. doi:10.1373/clinchem.2003.024588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Xie X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J. Chest CT for typical 2019-nCoV pneumonia: relationship to negative RT-PCR testing. Radiology 2020:200343. doi: 10.1148/radiol.2020200343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Huang P, Liu T, Huang L, et al. Use of chest CT in combination with negative RT-PCR assay for the 2019 novel coronavirus but high clinical suspicion. Radiology 2020:200330. doi: 10.1148/radiol.2020200330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P, Ji W. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology 2020:200432. doi: 10.1148/radiol.2020200432. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.