Abstract
A potential link between mortality, D-dimer values and a prothrombotic syndrome has been reported in patients with COVID-19 infection. The National Institute for Public Health of the Netherlands asked a group of Radiology and Vascular Medicine experts to provide guidance for the imaging workup and treatment of these important complications. This report summarizes evidence for thromboembolic disease, potential diagnostic and preventive actions as well as recommendations for patients with COVID-19 infection.
Introduction
Background
Coronavirus disease 2019 (COVID-19) is spreading rapidly around the globe since its first outbreak in Wuhan, China. COVID-19 is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which spreads from human to human primarily via aerosols from coughing or sneezing, but also via contaminated surfaces (1). SARS-CoV-2 enters cells by endocytosis after binding to the transmembrane angiotensin converting enzyme-2 (ACE2) protein on cells in the lung, heart, blood vessels, kidney, and gastrointestinal tract (2). The diagnosis of COVID-19 is confirmed by a positive reverse transcriptase polymerase chain reaction (RT-PCR) from nose, throat, sputum or bronchoalveolar lavage. The sensitivity of this test is suboptimal (50-80%), probably due to sampling error, low viral loads as well as timing of the sample in the disease course (3, 4). In most COVID-19 patients, non-contrast chest CTscanning shows bilateral ground glass opacities with a peripheral and basal distribution. The sensitivity of CT-imaging, not specificity, may be higher than the standard nasopharyngeal swab RT-PCR (5).
Clinicians worldwide face this new severe infectious lung disease with no proven therapies. Based on recent reports that demonstrated a strong association between elevated D-dimer levels and poor prognosis, concerns have risen about thrombotic complications in patients with COVID-19.
The National Institute for Public Health of the Netherlands asked a group of Radiology and Vascular Medicine experts to provide guidance for the imaging workup and treatment of these important complications. We used a question answer format to provide an expert opinion on the imaging workup, prevention and treatment of possible thromboembolic complications in patients with COVID-19:
Evidence for embolic/ thromboembolic disease in COVID-19
Current literature on coagulation and thrombosis in COVID-19
Venous thromboembolism (VTE)
There are no publications on the prevalence or incidence of VTE (i.e. deep vein thrombosis (DVT) and/or pulmonary embolism (PE)) in patients with COVID-19. However, there are case reports on thromboembolic disease, stroke and myocarditis in patients with COVID-19 (6-9).
Disseminated intravascular coagulation (DIC)
One Chinese single-center retrospective cohort study (Tongji hospital) of 183 patients with confirmed COVID-19 evaluated DIC (5). According to the International Society on Thrombosis and Hemostasis definition of DIC, 15 of 21 non-survivors (71%) were classified as having overtDIC (≥5 points) any time during follow-up, whereas only 1 of 162 survivors (0.6%) met these criteria (P<0.001). The median time from admission to DIC was 4 days (range, 2-12 days).
Thrombosis
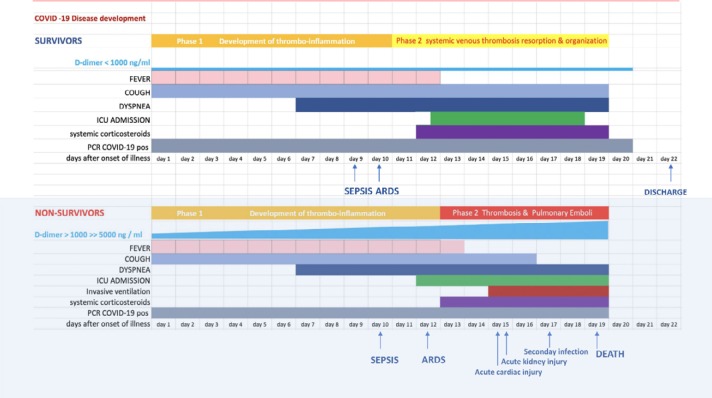
Recent observations suggest that respiratory failure in COVID-19 is not driven by the development of the acute respiratory distress syndrome (ARDS) alone (10), but that (microvascular) thrombotic processes may play a role as well. This may have important consequences for the diagnostic and therapeutic management of these patients. There is a strong association between D-dimer levels, disease progression and chest CT features suggesting venous thrombosis (11)(Figure 1) .
Figure 1:
A schematic representation of the pathophysiological disease development of COVID-19, based on the results of the Wuhan population in the context of plasma D-dimer values, clinical and imaging characteristics (Clinical findings reconstructed from reference Zhou et al).
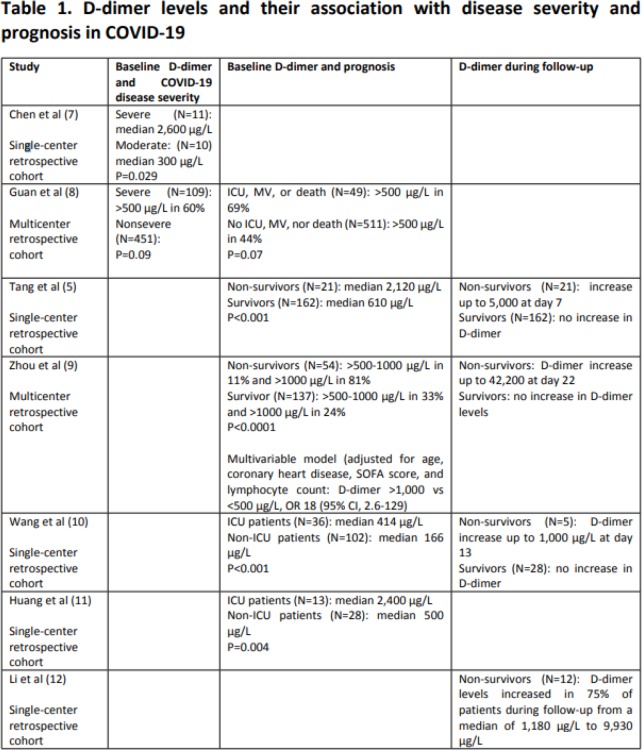
D-dimer
D-dimer is a degradation product of cross-linked fibrin and reflects blood clot formation and its subsequent fibrinolysis. Testing uses an enzyme-linked immunoabsorbent assay (ELISA) or microlatex agglutination assay (12). D-dimer has a very high sensitivity for thrombotic disease, but its specificity is poor. Various studies in patients with COVID-19 have consistently shown a very strong association between increased D-dimer levels and severe disease/poor prognosis (Table 1) (7, 11, 13-17).
Table 1.
D-dimer levels and their association with disease severity and prognosis in COVID-19
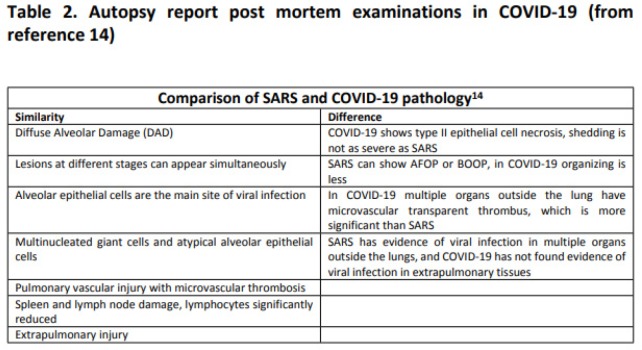
Pathology findings
Diffuse alveolar damage (DAD) is common autopsy finding in COVID-19 patients (18, 19). One series (19) describes the pulmonary histopathology in SARS1 (N=44) and SARS2 (COVID-19) (N=4) patients (Table 2) with both infections showing DAD, pulmonary microvascular thrombosis and necrosis in mediastinal lymph nodes and the spleen. However, only COVID-19 patients showed small vessel thrombosis in multiple organs.
Table 2.
Autopsy report post mortem examinations in COVID-19(from reference 14)
A recent report suggest that SARS2 (COVID-19) facilitates endotheliitis, which could explain the systemic impaired microcirculatory function in different vascular beds (20)(20).
Coagulation and COVID-19
The coagulation system can be activated by a variety of different viruses, including HIV, Dengue virus, and Ebola virus (21, 22). During the relatively recent outbreak of SARS-CoV in 2003, which was associated with even higher morbidity and mortality than COVID-19, vascular endothelial damage in both small- and mid-sized pulmonary vessels was noted together with DIC, DVT and PE resulting in pulmonary infarction (23-26). A case report of an autopsy described thrombosis in multiple organs in a patient with proven SARS-CoV infection (27). Given the similarity between SARS-CoV and SARS-CoV-2, similar thrombotic complications are likely to be present in patients with COVID-19. Whether the coagulation cascade is directly activated by the virus or whether this is the result of local or systemic inflammation is not completely understood.
High plasma levels of proinflammatory cytokines (interleukin-2, interleukin-7, granulocyte colony-stimulating factor, IP10, MCP1, MIP1A and tumor necrosis factor-α) have been observed in COVID-19 patients admitted to intensive care units. This is consistent with a “cytokine storm” with the secondary development of a hemophagocytic lymphohistiocytosis (28, 29). While many pro-inflammatory cytokines trigger the coagulation system, Zhou and colleagues (11) showed that the increase in IL-6 was discrepant with the elevations in D-dimer; IL-6 levels appeared to increase only 13 days after disease onset, whereas D-dimer levels were already 10-fold increased by that time. This observation suggests that the very high D-dimer levels observed in COVID-19 patients are not only secondary to systemic inflammation, but also reflect true thrombotic disease, possibly induced by cellular activation that is triggered by the virus.
What diagnostic and preventive actions should be initiated?
Role of antithrombotic therapy
Notably, a Chinese single-center retrospective cohort study (Tonghi hospital) of 449 consecutive patients classified as having severe COVID-19 indicates that prophylactic doses of heparins might be associated with improved survival (20%) in patients with evidence of sepsis induced coagulopathy (SIC)/DIC) (30). Severe COVID-19 was defined as either a respiratory rate ≥30/min, arterial oxygen saturation ≤93% at rest, or PaO2/FiO2 ≤300 mmHg. Exclusion criteria included bleeding diathesis, hospital stay <7 days and lack of information of coagulation parameters and medications. Of the 449 patients, 99 (22%) received heparin for 7 days or longer (LMWH in 94 patients, usually enoxaparin 40-60 mg/day, and UFH in 5). Heparin was associated with lower 28-day mortality among the 97 patients with a SIC score ≥4, (40% vs 64%; OR, 0.37 [95% CI, 0.15-0.90]; P=0.029), but not among the 352 patients with a SIC score <4 (29% vs 23%; P=0.42).
Chest CT
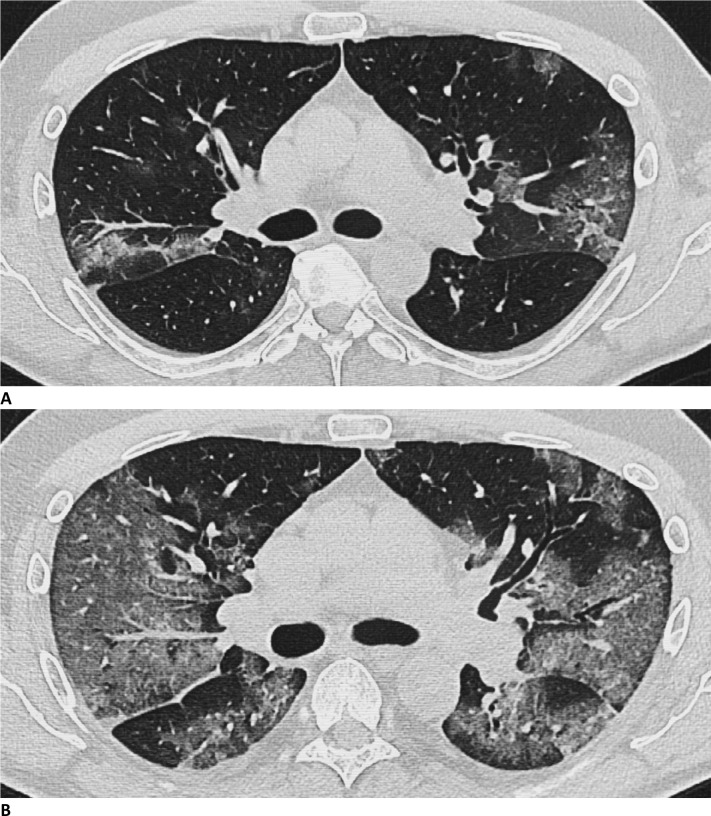
Several proposals have been made to enable standardized reporting, such as CO-RADS by the Dutch Radiological Society (31) and a consensus statement from the USA (32). Typical characteristics and time course of lung changes on chest CT were recently described (33). The CT severity score on initial scans is based on the amount of lung tissue (% lung parenchyma) that is involved at presentation (34). The common chest CT features have recently been enumerated from 1014 patients (5). Ground glass opacities (GGO) were found in all patients (100%) . The uniformity of GGOs in this disease was confirmed in 158 consecutive patients from Italy (35).
The typical CT pattern of COVID-19 pneumonia in Rome, Italy was characterized by the consistent presence of peripheral ground glass opacities associated with multi-lobar and posterior involvement, bilateral distribution, and subsegmental vessel enlargement (Figure 2). Vessel enlargement was described in the vicinity of areas with GGO, which is compatible with thrombo-inflammatory processes (35-40). Subsegmental vascular enlargement (more than 3 mm diameter) in areas of lung opacity was observed in 89% of patients with confirmed COVID19 pneumonia. All the CT’s were done without contrast. Although in situ thrombosis is certainly a possibility, these findings could be due to hyperemia and increased blood flow (Figure 2) (35)
Figure 2:
Chest CT images in 51-year-old male patient presenting with progressive symptoms of cough and fever, proven COVID-19. (A) Day 7 after onset of symptoms: CT demonstrates bilateral ground glass opacities (GGOs) and early vascular enlargement. (B) Day 10: Rapid progression of GGOs with vascular thickening and interstitial pulmonary edema. (Figure courtesy of Department of Radiology, Haaglanden Medical Centre, The Hague, the Netherlands.)
A recent retrospective study in 1008 patients, in which 25 patients underwent CT pulmonary angiography, demonstrated acute PE in 10 patients (40%), which were mainly located in subsegmental vessels (7). All patients were treated with anticoagulant therapy, and three demonstrated partial or complete resolution at follow-up CT pulmonary angiography, while two patients died (7).
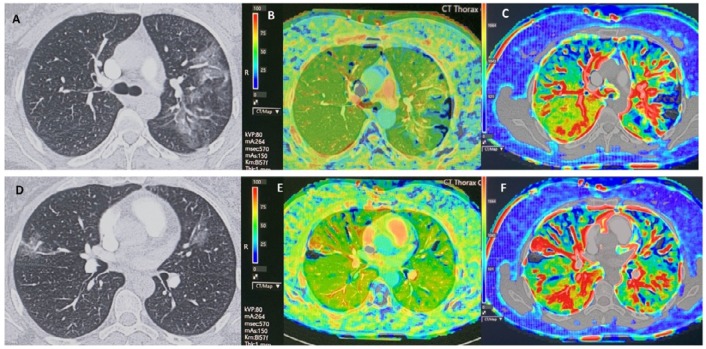
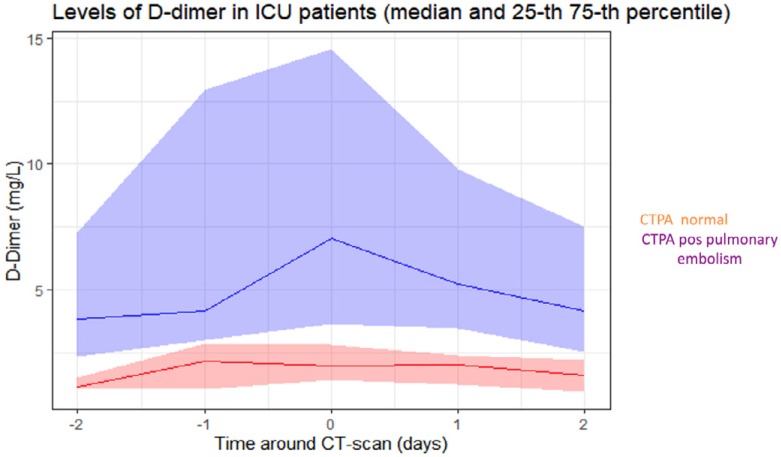
Pulmonary thrombo-inflammatory processes, systemic-thrombosis and PE are currently poorly evaluated on chest CT examinations when iodinated intravenous contrast is not given (41). Figure 3 demonstrates CT perfusion findings in early phase of the disease with multiple bilateral perfusion deficits due to microvascular obstruction. In the later stages of the illness, there are currently few clinical CT investigations with intravenous contrast in patients who become respiratory insufficient. In late phases of disease, it has been challenging to diagnose thromboembolic disease or complications. Importantly, this is a phase where plasma D-dimer may become extremely elevated in those with thrombo-inflammatory underlying pathophysiology (Figure 4) (13).
Figure 3:
This proof of concept demonstrates CT perfusion findings in phase 1 in a 43-year old female patient proven COVID-19 with multiple ground glass opacities, with plasma Ddimer < 500 ng/ml and without pulmonary embolism on CT pulmonary angiography. There are multiple bilateral perfusion deficits due to microvascular obstruction, with increased blood flow in or adjacent to areas of ground glass opacities. The blood flow is slightly increased in the right lower lobe. Scan parameters: Conventional Dynamic Perfusion CT, Somatom Drive, Siemens; Scan volume 8,4 cm (aorta arch – left atrium); 1 mm recon; Dual input lung perfusion 4D, Vitrea, Vital, Canon; pulmonary flow: ml/min./100 ml; arterial flow: ml/min./100 ml; perfusion Index: % Baseline chest CT findings in selected slices (A, D), with perfusion index (B,E) and pulmonary arterial flow (C, F) in corresponding slices. (Figure courtesy of Department of Radiology, Haaglanden Medical Centre, The Hague, the Netherlands.)
Figure 4:
Plasma D-dimer course in 43 consecutive patients with COVID-19, admitted to the intensive care unit. PE was diagnosed with CTPA in 35 patients. (Figure courtesy of Dr Diederik Gommers, Erasmus University Medical Centre, Rotterdam, the Netherlands).
We conclude that careful attention needs to be paid to the initial diagnosis, prevention and treatment of the prothrombotic and thrombotic state that can occur in a substantial percentage of COVID-19 patients.
Summary Recommendations: Diagnostic and Therapeutic Management as proposed for Dutch Healthcare
Prophylactic-dose low-molecular-weight heparin should be initiated in all patients with (suspected) COVID-19 admitted to the hospital, irrespective of risk scores (e.g. Padua score).
A baseline (non-contrast) chest CT should be considered in all patients with suspected COVID-19 who have an indication for hospital admission (Dutch Healthcare).
In patients with suspected COVID-19 as well as a high clinical suspicion for PE (e.g. based on hemoptysis, unexplained tachycardia, or signs/symptoms of DVT, acute deterioration upon moving patient), CT pulmonary angiography should be considered if the D-dimer level is elevated. The D-dimer threshold used should follow locally used algorithms, i.e. ≥500 mg/L, age-adjusted threshold, or ≥1,000 mg/L when no YEARS criteria are present. If PE is confirmed, therapeutic anticoagulation is indicated.
-
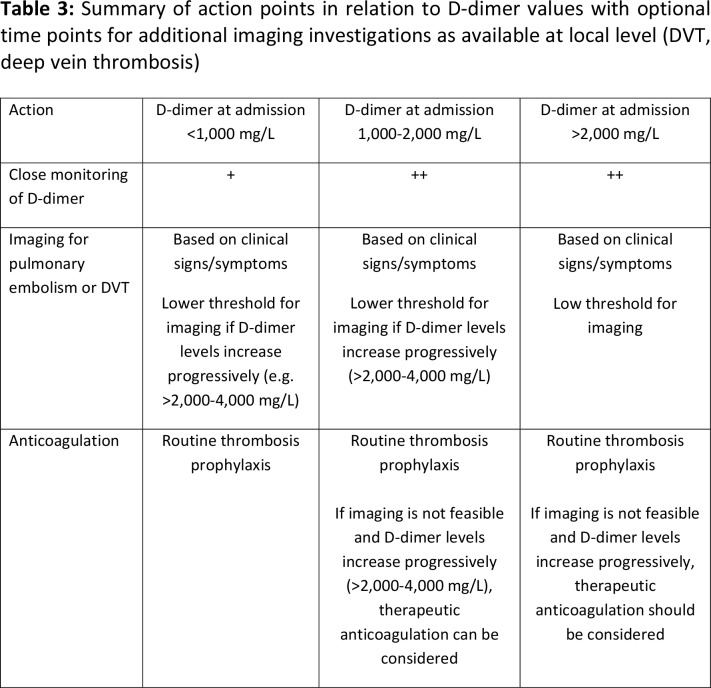
In patients with COVID-19 admitted to the hospital, routine D-dimer testing on admission and serially during hospital stay should be considered for prognostic stratification with additional imaging as available at local level (Table 3).
a. In patients with a D-dimer <1,000 µg/L on admission and no significant increase during follow-up, prophylactic anticoagulation should be continued.
b. In patients with a D-dimer <1,000 µg/L on admission but a significant increase during hospital stay to levels above 2,000-4,000 µg/L, imaging for DVT or PE should be considered, in particular when signs suggestive of clinically-relevant hypercoagulability such as venous congestion/thrombosis are present on chest CT, clotting of extracorporeal circuits, or when patients deteriorate clinically (e.g. refractory hypoxemia or unexplained new-onset tachycardia or hypotension). When imaging is not feasible, therapeutic-dose low-molecularweight heparin without imaging can be considered when the risk of bleeding is acceptable.
c. For patients with D-dimer values between 1,000 and 2,000 µg/L, there is no clear-cut guidance other than institution of prophylactic anticoagulation. These patients may suffer from venous thromboembolism, and where possible this should be excluded. Close monitoring of D-dimer in combination with clinical findings should lead to further decision making along the lines of low vs strongly increased D-dimer levels.
d. In patients with a strongly increased D-dimer on admission (e.g. 2,000-4,000 µg/L), caution is warranted. D-dimer testing should be repeated within 24-48 hours to detect further increases in which case imaging for DVT or PE should be considered as outlined above.
Table 3:
Summary of action points in relation to D-dimer values with optional time points for additional imaging investigations as available at local level (DVT, deep vein thrombosis)
References
- 1.van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, Lloyd-Smith JO, de Wit E, Munster VJ. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 2020;382:15641567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang Q, Zhang Y, Wu L, Niu S, Song C, Zhang Z, Lu G, Qiao C, Hu Y, Yuen KY, Wang Q, Zhou H, Yan J, Qi J. Structural and functional basis of SARS-CoV-2 entry by using human ACE2. Cell 2020; 10.1016/j.cell.2020.03.045. Published April 9, 2020. Accessed April 19, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, Tan W. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA 2020; doi: 10.1001/jama.2020.3786. Published March 11, 2020. Accessed April 8, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xu H, Yan L, Qiu CM, Jiao B, Chen Y, Tan X, Chen Z, Ai L, Xiao Y, Luo A, Li S. Analysis and Prediction of False Negative Results for SARS-CoV-2 Detection with Pharyngeal Swab Specimen in COVID-19 Patients: A Retrospective Study. MedRxiv 2020; 10.1101/2020.03.26.20043042. Published March 30, 2020. Accessed April 8, 2020. [DOI] [Google Scholar]
- 5.Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology 2020;200642. doi: 10.1148/radiol.2020200642. Published February 26, 2020. Accessed April 10, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Danzi GB, Loffi M, Galeazzi G, Gherbesi E. Acute pulmonary embolism and COVID-19 pneumonia: a random association? Eur Heart J 2020; doi: 10.1093/eurheartj/ehaa254. Published March 30, 2020. Accessed April 11, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen J, Wang X, Zhang S, Liu B, Wu X, Wang Y, Wang X, Yang M, Sun J, Xie Y. Findings of acute pulmonary embolism in COVID-19 patients. The SFAR website. https://sfar.org/thelancet-infectious-diseases-findings-of-acute-pulmonary-embolism-in-covid-19-patients/ Published March 19,2020. Assessed April 8, 2020. [Google Scholar]
- 8.Bonow RO, Fonarow GC, O’Gara PT, Yancy CW. Association of coronavirus disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardiol 2020; doi: 10.1001/jamacardio.2020.1105. Published March 27, 2020. Accessed March 28, 2020. [DOI] [PubMed] [Google Scholar]
- 9.Zhang Y, Xiao M, Zhang S, Xia P, Cao W, Jiang W, Chen H, Ding X, Zhao H, Zhang H, Wang C, Zhao J, Sun X, Tian R, Wu W, Wu D, Ma J, Chen Y, Zhang D, Xie J, Yan X, Zhou X, Liu Z, Wang J, Du B, Qin Y, Gao P, Qin X, Xu Y, Zhang W, Li T, Zhang F, Zhao Y, Li Y, Zhang S. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med 2020; doi: 10.1056/NEJMc2007575. Published April 8, 2020. Accessed April 10, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Magro C, Mulvey JJ, Berlin D, Nuovo G, Salvatore S, Harp J, Baxter-Stoltzfus A, Laurence J. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. Transl Res 2020; doi: 10.1016/j.trsl.2020.04.007. Published April 15, 2020. Accessed April 18, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054-1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Riley RS, Gilbert AR, Dalton JB, Pai S, McPherson RA. Widely used types and clinical applications of D-dimer assay. Lab Med 2016;47:90-102. doi: 10.1093/labmed/lmw001. [DOI] [PubMed] [Google Scholar]
- 13.Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, Liu L, Shan H, Lei C, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; doi: 10.1056/NEJMoa2002032. Published February 28, 2020. Accessed March 6, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA 2020; doi: 10.1001/jama.2020.1585. Published February 7, 2020. Accessed March 3, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 10.1016/S0140-6736(20)30183-5. Published January 24, 2020. Accessed March 6, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li X, Wang L, Yan S, Yang F, Xiang L, Zhu J, Shen B, Gong Z. Clinical characteristics of 25 death cases with COVID-19: a retrospective review of medical records in a single medical center, Wuhan, China. Int J Infect Dis 2020; doi: 10.1016/j.ijid.2020.03.053. Published April 3, 2020. Accessed April 6, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 2020;18:844-847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu Q, Wang R, Qu G, Wang Y, Liu P, Zhu Y, Fei G, Ren L, Zhou Y, Liu L. Gross examination report of a COVID-19 death autopsy. Fa Yi Xue Za Zhi 2020;36:21-23. doi: 10.12116/j.issn.10045619.2020.01.005. [DOI] [PubMed] [Google Scholar]
- 19.Zhang T, Sun L, Feng RE. Comparison of clinical and pathological features between severe acute respiratory syndrome and coronavirus disease 2019. Zhonghua Jie He He Hu Xi Za Zhi 2020;43:E040. doi: 10.3760/cma.j.cn112147-20200311-00312. [DOI] [PubMed] [Google Scholar]
- 20.Varga Z: Endothelial cell infection and endotheliitis in COVID-19. The Lancet’s website. https://www.thelancet.com/lancet/article/s0140-6736(20)30937-5. Published April 17, 2020. Assessed April 19,2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Antoniak S, Mackman N. Multiple roles of the coagulation protease cascade during virus infection. Blood 2014;123:2605-13. doi: 10.1182/blood-2013-09-526277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Antoniak S. The coagulation system in host defense. Res Pract Thromb Haemost 2018;2:549-557. doi: 10.1002/rth2.12109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee N, Hui D, Wu A, Chan P, Cameron P, Joynt GM, Ahuja A, Yung MY, Leung C, To KF, Lui SF, Szeto CC, Chung S, Sung JJ. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med 2003;348:1986-94. doi: 10.1056/NEJMoa030685 [DOI] [PubMed] [Google Scholar]
- 24.Chong PY, Chui P, Ling AE, Franks TJ, Tai DY, Leo YS, Kaw GJ, Wansaicheong G, Chan KP, Ean Oon LL, Teo ES, Tan KB, Nakajima N, Sata T, Travis WD. Analysis of deaths during the severe acute respiratory syndrome (SARS) epidemic in Singapore: challenges in determining a SARS diagnosis. Arch Pathol Lab Med 2004;128:195-204. [DOI] [PubMed] [Google Scholar]
- 25.Hwang DM, Chamberlain DW, Poutanen SM, Low DE, Asa SL, Butany J. Pulmonary pathology of severe acute respiratory syndrome in Toronto. Mod Pathol 2005;18:1-10. doi: 10.1038/modpathol.3800247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wong RS, Wu A, To KF, Lee N, Lam CW, Wong CK, Chan PK, Ng MH, Yu LM, Hui DS, Tam JS, Cheng G, Sung JJ. Haematological manifestations in patients with severe acute respiratory syndrome: retrospective analysis. BMJ 2003;326:1358-1362. doi: 10.1136/bmj.326.7403.1358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xiang-hua Y, Le-min W, Ai-bin L, Zhu G, Riquan L, Xu-you Z, Wei-wei R, Ye-nan W. Severe acute respiratory syndrome and venous thromboembolism in multiple organs. Am J Respir Crit Care Med 2010;182:436-7. doi: 10.1164/ajrccm.182.3.436. [DOI] [PubMed] [Google Scholar]
- 28.Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, Wang T, Zhang X, Chen H, Yu HJ. Clinical and immunologic features in severe and moderate forms of Coronavirus Disease 2019. J Clin Invest. 2020; doi: 10.1172/JCI137244. Published April 13, 2020. Assessed April 15,2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mehta P, Mcauley D, Brown M, Sanchez E, Tattersall R, Manson J, HLH Across Speciality Collaboration, UK . Correspondence COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet 2020;395:1033-1034. doi: 10.1016/S0140-6736(20)30628-0. Published March 16, 2020. Assessed April 11,2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost 2020; doi: 10.1111/jth.14817. Published March 27,2020. Assessed April 9,2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nederlandse Vereniging voor Radiologie . Handreiking Standaardverslag CT-thorax COVID inclusief CO-RADS en CT score. The Nederlandse Vereniging voor Radiologie website. https://www.radiologen.nl/secties/netwerk-covid-19/documenten/handreikingstandaardverslag-ct-thorax-covid-inclusief-co-rads. Published April 10, 2020. Assessed April 19,2020. [Google Scholar]
- 32.Simpson S, Kay FU, Abbara S, Bhalla S, Chung JH, Chung M, Henry TS, Kanne JP, Kligerman S, Ko JP, Litt H. Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. Radiol Cardiothorac Imaging 2020; 10.1148/ryct.2020200152. Published March 25, 2020. Assessed April 10, 2020. [DOI] [PMC free article] [PubMed]
- 33.Pan F, Ye T, Sun P, Gui S, Liang B, Li L, Zheng D, Wang J, Hesketh RL, Yang L, Zheng C. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology 2020;200370. doi: 10.1148/radiol.2020200370. Published Febrary 13, 2020. Assessed April 14,2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wu J, Wu X, Zeng W, Guo D, Fang Z, Chen L, Huang H, Li CJIr. Chest CT Findings in Patients With Coronavirus Disease 2019 and Its Relationship With Clinical Features. Invest Radiol 2020;55:257-261. doi: 10.1097/RLI.0000000000000670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Caruso D, Zerunian M, Polici M, Pucciarelli F, Polidori T, Rucci C, Guido G, Bracci B, de Dominicis C, Laghi A. Chest CT Features of COVID-19 in Rome, Italy. Radiology 2020;201237. doi: 10.1148/radiol.2020201237. Published April 3, 2020. Assessed April 17, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Frazier AA, Franks TJ, Mohammed T-LH, Ozbudak IH, Galvin JR. Pulmonary veno-occlusive disease and pulmonary capillary hemangiomatosis. Radiographics 2007;27:867-882. doi: 10.1148/rg.273065194. [DOI] [PubMed] [Google Scholar]
- 37.Chung MP, Yi CA, Lee HY, Han J, Lee KS. Imaging of pulmonary vasculitis. Radiology 2010;255:322-341. doi: 10.1148/radiol.10090105. [DOI] [PubMed] [Google Scholar]
- 38.Albarello F, Pianura E, Di Stefano F, Cristofaro M, Petrone A, Marchioni L, Palazzolo C, Schininà V, Nicastri E, Petrosillo N, Campioni P, Eskild P, Zumla A, Ippolito G; COVID 19 INMI Study Group . 2019-novel Coronavirus severe adult respiratory distress syndrome in two cases in Italy: An uncommon radiological presentation. Int J Infect Dis 2020;93:192-197. doi: 10.1016/j.ijid.2020.02.043. Published Febrary 26, 2020. Assessed April 15, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bai HX, Hsieh B, Xiong Z, Halsey K, Choi JW, Tran TML, Pan I, Shi L-B, Wang D-C, Mei J, Jiang XL, Zeng QH, Egglin TK, Hu PF, Agarwal S, Xie F, Li S, Healey T, Atalay MK, Liao WH. Performance of radiologists in differentiating COVID-19 from viral pneumonia on chest CT. Radiology 2020:200823.doi: 10.1148/radiol.2020200823. Published March 10, 2020. Assessed April 12, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ye Z, Zhang Y, Wang Y, Huang Z, Song B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur Radiol 2020. doi: 10.1007/s00330-020-068010. Published March 19, 2020. Assessed April 11, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Klok F, Kruip M, van der Meer N, Arbous M, Gommers D, Kant K, Kaptein F, van Paassen J, Stals M, Huisman MV, Endeman H. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 2020. 10.1016/j.thromres.2020.04.013. Published April 10,2020. Assessed April 19, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]