Abstract
Background.
Transgender women (TW) in Puerto Rico (PR) face social stigmatization. Physicians’ transgender stigma can have detrimental consequences for TW’s health.
Purpose.
The objective of this study was to document physicians’ knowledge, competencies, and attitudes towards TW in PR and study their associations with stigma towards TW.
Methods.
We implemented an exploratory sequential mixed-methods study. We used in-depth interviews (n=30) and self-administered questionnaire (n=255).
Results.
Qualitative results illustrated lack of recognition of the needs of TW; they also evidenced the impact of stigmatizing attitudes on clinical decisions. Quantitative results showed that more willingness and knowledge to provide health services to TW were negatively associated with stigma. Participants who reported history of training in working with TW presented significantly less stigma than participants who had not received such training.
Conclusion.
In order to provide stigma-free services for TW in PR, specialized training regarding the particular needs of this population is needed.
Keywords: Transgender, trans women, stigma, physicians, Puerto Rico
Transgender is used as an umbrella term to describe people whose assigned sex at birth is not fully aligned with their current gender identity.1 Due to social stigma, transgender people are placed in vulnerable situations in their everyday lives, resulting in high risks for health problems, high under- and unemployment, poverty, and, of particular relevance to this article, reduced access to health care services.2–8 Specifically, transwomen (TW; male-to-female transgender people who often feminize their bodies through hormone therapy or surgery) continue to be disproportionately affected by health disparities that persist across multiple health outcomes.3,6,9,10 Complicating the situation is that health surveillance systems in the United States (U.S.) rarely monitor transgender individuals as such,2 and lack of information and training about trans-specific health care among physicians is common.11
In this article we present data from a study conducted in Puerto Rico (PR) that aimed to explore four areas related to the provision of care to TW among a sample of physicians through a mixed-methods approach: 1) knowledge of transgender health; 2) competencies in treating TW; 3) willingness to provide services to this population; and 4) stigma-related attitudes toward TW We utilized a multilevel (i.e., structural, interpersonal, individual) social determinants of health approach,12 focusing on the potential negative effects of transgender stigma on TW in the context of access to health care. Social determinants are the conditions in the environments in which people are born, live, work, and age that affect a wide range of health, functioning, quality of life outcomes, and risks.13 They include access and quality of medical care.14 Addressing social determinants of health is extremely important for improving the health of marginalized populations, such as TW, and reducing disparities in health and health care.
Health disparities among TW.
Approximately .6% of the U.S. population identifies as transgender.15 This segment of the population faces significant health disadvantages (i.e., they are disparately and negatively affected by health conditions relative to the overall U.S. population) in several areas,16 including HIV, substance use, and mental health conditions. For example, in the U.S. (including PR), TW are one of the groups most affected by HIV and are 49 times more likely to be living with this condition than the general population.17 The prevalence of HIV among TW is equal to or greater than its prevalence among other highly affected populations such as men who have sex with men.3,17 In the U.S., between 20% and 30% of TW abuse substances, compared with 9% of the general population.18 Community surveys with TW have found high levels of alcohol and marijuana use (50% and 38%, respectively) and high prevalence of sex under the influence of drugs and alcohol.19 In PR, 14.7% of the general population reports engaging in substance abuse.20 In contrast, data from previous research with TW on the Island show that more than half of participants (56%) reported having used alcohol, marijuana, or cocaine during the last month.21 Transgender populations have been shown to have a higher prevalence of mental health conditions and suicidality than individuals who are not transgender.22 Among the general population in the U.S., 18.5% experience mental health conditions in a given year.23 In comparison, studies with TW have documented higher rates of depression (35%–44%), anxiety (28%), and overall psychological distress (40%).6,24
Due to these health disparities, TW will require enhanced medical and mental health care. Health care providers must be aware of the implications of the health concerns borne disproportionately by this population and the larger social and structural barriers that may affect access to care, including stigma.5,21,25 Stigma and discrimination manifested in the delivery of health care could affect TW’s trust and ability to access appropriate care.16
Transgender stigma as a social determinant of health.
Stigma is considered one of the social conditions that shapes population health.26 Stigmatization is a multilevel process that shapes structural, interpersonal, and/or individual determinants of health.27 In the case of TW, for instance, stigmatization might be manifested in: the denial of medical insurance coverage for gender-affirming medical interventions (a structural determinant); the risk of physical and psychological violence when gender non-conformity becomes apparent in social or intimate interactions (an interpersonal determinant); or shame and avoidance of routine health care facilities due to internalized stereotypes and negative experiences with medical providers (an individual determinant).
Research has begun to document the impact of stigma manifestations on the health of the transgender population across the lifespan.28 These manifestations may be explicit (i.e., deliberate, easy to identify)29 or tacit (i.e., less intentional, harder to identify). Stigma has been associated with mental, physical, and sexual violence,8 depression, anxiety, and somatization,6 hormone and silicone injection without medical supervision,5 reproductive health care avoidance,30 HIV risk behaviors,31 substandard substance use treatment,32 increased suicide attempts,33 and mental health treatment disparities.34 These studies provide evidence that stigma is a social determinant of health28 that can influence well-being through the production of inequities and stress.26,35
Stigma among health professionals.
Previous research has shown that many health professionals hold negative attitudes towards socially stigmatized populations.36,37 However, the attitudes of health professionals toward the transgender population have not been specifically examined, particularly from the providers’ perspective. Despite evidence suggesting that transgender people experience stigma in health care settings7,8,32,38 and that lack of knowledge and skills can potentially result in stigmatizing encounters (for example, the use of inappropriate language30,39,40), research on transgender stigma among health professionals is very limited41 and has relied almost exclusively on patients’ perceptions of care,1,41,42 while the perspectives of physicians have largely been overlooked.
Recent literature has stressed the need to address stigmatization at multiple levels to reduce health disparities among the transgender population. Our previous, formative research with TW in PR showed that, while interacting with health care providers in clinical scenarios, they experienced high levels of transgender stigma accompanied by lack of overall knowledge about transgender health and competencies to interact with them.5,10,25,43,44 Taking this into consideration, our specific aims reflect four areas related to the provision of care (i.e., physicians’ knowledge on transgender health, competencies in treating TW, willingness to provide services to this population, and stigma-related attitudes toward TW). We defined knowledge of transgender health as having accurate information about the specific health-related needs of this population. Competencies in treating TW are related to having the skills to interact and provide health care to TW. We defined willingness to provide services to TW as a positive disposition to provide trans-sensitive health care to this population. Finally, stigma-related attitudes towards TW refer to negative beliefs towards the population.
We investigated these areas both qualitatively and quantitatively. In the quantitative component, we included measures of social desirability, previous training, religiosity, and the importance of religion, as previous research indicated that these variables may affect social stigma.45–49 We hypothesized that willingness to provide services to TW, knowledge of TW health, previous training in transgender health, and competencies to provide services to TW would be negatively associated with stigma, whereas religiosity and the importance of religion would be positively associated with stigma. Finally, we hypothesized that social desirability would be negatively associated with stigma.
Methods
To achieve the above objectives, we implemented an exploratory sequential mixed-methods study. In the qualitative phase (Phase 1), we conducted semi-structured in-depth interviews with a small sample of physicians (n=30) to explore stigmatizing attitudes among them in a rich way. We also gathered information in this qualitative phase to develop the items for the quantitative survey that was administered in Phase 2. This survey was given to a larger sample of participants (n=255) in order to identify the relationships among the stigmatization of TW (i.e., attitudes or behaviors toward them) and physicians’ knowledge, competencies, and willingness to treat TW.
Participants and procedures.
A total of 342 physicians were invited by phone or email to participate in the study and 80% (N=285) agreed. They were not compensated financially for their participation in the study. All procedures were implemented in Spanish. For Phase 1, 30 participants were recruited via purposive sampling to ensure the inclusion of both HIV-care providers (n=12, 40%) and physicians from other specialty areas (n=18, 60%) (See Table 1 for a detailed description). The study’s project coordinator (PC) and two research assistants (RAs) gathered physicians’ contact information through the Internet and contacted their offices. Physicians from governmental, community-based, and private health care settings were included. The inclusion criteria were: 1) licensed as a physician in PR and 2) engaged in direct service delivery. The RAs explained to physicians the nature of the study and scheduled the interview if the individual agreed to participate. Almost all interviews were carried out at physicians’ offices. The principal investigators (PIs) and the PC conducted the interviews. Once the consent form was reviewed and signed by participants, they completed a paper-and-pencil, self-administered Demographic Data Questionnaire (DDQ). Subsequently, they participated in an in-depth interview that was audio-recorded and later transcribed for qualitative coding and analysis. The average interview lasted 55 minutes. Physicians who participated in Phase 1 were between the ages of 27 and 72 years (mean age: 54 years) (see Table 1). More than half were males (56.7%) and most self-dentified as heterosexual (83.3%). Most participants were living with a partner (80%). Seventy percent reported being religious, with different levels of participation in religious activities (Table 1). More than 80% had an annual income greater than $70,000. Most (83.3%) reported not having formal training in transgender health. Almost two-thirds (63.3%) reported having provided services to TW.
Table 1.
SOCIO-DEMOGRAPHIC DATA OF INTERVIEWS AND QUESTIONNAIRES (N=255)
| Interviews |
Questionnaires |
|||
|---|---|---|---|---|
| Variable | N | % | N | % |
| Age range | ||||
| 26–40 | 6 | 23.3 | 68 | 27.0 |
| 41–50 | 2 | 6.7 | 53 | 21.0 |
| 51–60 | 9 | 30.0 | 89 | 35.3 |
| >60 | 12 | 40.0 | 42 | 12.6 |
| Gender | ||||
| Male | 17 | 56.7 | 124 | 48.6 |
| Female | 13 | 43.3 | 129 | 50.6 |
| Sexual Orientation | ||||
| Heterosexual | 25 | 83.3 | 229 | 90.5 |
| Homosexual/Lesbian | 5 | 16.7 | 20 | 7.9 |
| Bisexual | 0 | 0 | 4 | 1.6 |
| Marital Status | ||||
| Married | 16 | 53.3 | 135 | 57.2 |
| Single | 1 | 3.3 | 40 | 16.9 |
| Divorce | 2 | 10.0 | 22 | 9.3 |
| Widow | 2 | 26.7 | 6 | 2.5 |
| Living with partner (not legally married) | 8 | 26.7 | 27 | 11.4 |
| Religion | ||||
| Catholic | 18 | 60.0 | 151 | 63.4 |
| Protestant | 3 | 10.0 | 29 | 12.2 |
| Santero | 1 | 3.3 | 1 | .4 |
| None | 1 | 23.3 | 39 | 16.4 |
| Other | 1 | 3.3 | 18 | 7.6 |
| Importance of religion | ||||
| Not important | 3 | 10.0 | 33 | 14.1 |
| Of minor importance | 7 | 23.3 | 55 | 23.3 |
| Important | 13 | 43.3 | 72 | 2.1 |
| Very Important | 7 | 23.3 | 74 | 41.1 |
| Participation on religious activities | ||||
| I don’t participate | 9 | 30.0 | 86 | 36.4 |
| Weekly | 9 | 30.0 | 48 | 20.3 |
| Sometimes during the month | 4 | 13.3 | 5 | 2.1 |
| Sometime during the year | 8 | 26.7 | 97 | 41.1 |
| Annual income | ||||
| Less than $50,000 | 0 | 0 | 23 | 9.7 |
| From $50,001 to $60,000 | 1 | 3.3 | 10 | 4.2 |
| From $60,001 to $70,000 | 3 | 10.0 | 12 | 5.0 |
| More than $70,000 | 25 | 83.3 | 191 | 81.1 |
| Medical Specialty | ||||
| Allergy and immunology | 0 | 0 | 1 | .3 |
| Anesthesiology | 1 | 3.3 | 4 | 1.3 |
| Dermatology | 0 | 0 | 2 | .6 |
| Emergency Medicine | 2 | 6.7 | 2 | .6 |
| Endocrinology | 0 | 0 | 2 | .6 |
| Family medicine | 0 | 0 | 17 | 6 |
| Gastroenterology | 0 | 0 | 2 | .6 |
| General Medicine | 2 | 6.7 | 82 | 25.9 |
| Gynecology/obstetrics | 0 | 0 | 25 | 7.9 |
| HIV Specialist | 12 | 40.0 | 7 | 2.2 |
| Internal Medicine | 5 | 16.7 | 22 | 6.9 |
| Neurology | 0 | 0 | 6 | 1.9 |
| Odontology | 1 | 3.3 | 2 | .6 |
| Ophthalmology | 0 | 0 | 2 | .6 |
| Orthopedic | 0 | 0 | 2 | .6 |
| Pediatric | 3 | 10.0 | 21 | 6.6 |
| Physiatrist | 0 | 0 | 4 | 1.2 |
| Plastic Surgery | 1 | 3.3 | 18 | 5.7 |
| Psychiatry | 2 | 6.7 | 0 | 0 |
| Surgery | 0 | 0 | 9 | 2.8 |
| Urology | 1 | 3.3 | 1 | .3 |
| Organization | ||||
| Government | 18 | 60.0 | 59 | 17.6 |
| Community | 1 | 3.3 | 14 | 4.2 |
| Private | 11 | 36.7 | 200 | 60.5 |
| Years of experience | ||||
| 1–10 | 13 | 44.8 | 70 | 30.6 |
| 11–20 | 6 | 19.8 | 52 | 22.9 |
| 21–30 | 6 | 19.8 | 59 | 24.8 |
| 31–40 | 4 | 13.3 | 38 | 15.2 |
| >40 | 8 | 3.2 | ||
| Provision of health services to transgender women | ||||
| Yes | 19 | 63.3 | 109 | 46.6 |
| No | 7 | 23.3 | 29 | 12.4 |
| I don’t know | 1 | 3.3 | 26 | 11.1 |
| We don’t ask | 3 | 10.0 | 70 | 29.9 |
| Formal training on transgender health | ||||
| Yes | 4 | 13.8 | 43 | 18.5 |
| No | 25 | 83.3 | 190 | 81.5 |
For Phase 2, 255 physicians from a broad range of specialty areas (20 in total) (see Table 1) were recruited through convenience sampling. The inclusion criteria for this phase were the same ones used in Phase 1. As a result of a collaboration agreement, the Puerto Rico College of Physicians and Surgeons50 provided us with an island-wide list of practicing physicians. The RAs contacted physicians by phone or email and invited them to access the consent form, the DDQ, and the self-administered survey through a secure website. In addition, the PC and RAs attended two medical conferences that were held in the San Juan metropolitan area and recruited additional physicians to participate in the quantitative phase of the study. At these conferences, physicians were given a tablet with the informed consent information, the DDQ, and the survey. The average time needed to complete the survey was 30 minutes. Participants had a mean age of 49 years. They were balanced in terms of gender and most of them identified themselves as heterosexual (90.6%). More than half (56.5%) reported being married and three-fourths (75%) reported being religious, with different levels of participation in religious activities. Participants had the same income level as those who engaged in Phase 1. Eighty-two percent reported not having formal training in transgender health. Almost half (46.6%) reported having provided services to TW at some point (detailed demographic data are presented in Table 1).
Measures.
Three instruments were used to collect the data for this study: 1) a Demographic Data Questionnaire (DDQ), 2) a semi-structured in-depth interview guide, and 3) a survey. The DDQ included 29 multiple choice items to assess participants’ gender, sexual orientation, income, religion, specialty area, and number of years practicing medicine, among others.
For Phase 1, we developed a semi-structured in-depth interview guide based on the existing literature on transgender health services and data from our previous research with TW in PR,5,10,25,44 in which participants reported a number of difficulties in accessing appropriate health care. The guide was designed to examine in depth physicians’ knowledge and training in transgender health, stigmatizing attitudes towards TW, willingness to provide services to them, and overall competencies and experience in delivering transgender health care. A transgender woman and two transgender health experts evaluated the guide before deployment in the field. The final version included 22 open-ended questions and two vignettes about hypothetical transgender patients. Some examples of questions included in the guide are: What do you know about gender dysphoria?; What do you think are the main medical needs that transgender women have? (the interviewer had to explore each of the following areas: primary care, mental health, hormone therapy, breast implants, and aesthetic and genital surgeries); and Tell me how do you usually proceed when clinically interviewing a patient who is a transgender woman (or hypothetically in the case you have never treated one) for the first time?
Through the use of vignettes, we explored physicians’ clinical approach in providing health care to TW For example, in one vignette we described a transgender woman who had started to take hormones without medical supervision as part of her transitioning process. We asked physicians to share what kind of recommendations they would provide, how they would feel interacting with this patient, and what would be the challenges in doing so, among other questions.
Data from the Phase 1 qualitative interviews helped us to develop three quantitative measures: the Transgender Stigma Scale; the Transgender Health Competencies Scale; and the Transgender Health Willingness Scale. Data from Phase 1 also helped us to adapt the Transgender Knowledge Scale for use in Phase 2. We also included a social desirability scale as part of the quantitative instrument, measuring participants’ tendency to respond in a socially desirable manner to attitudinal questions, which could influence responses to stigma-related questions. Our final quantitative instrument (survey) included the five measures described below.
Transgender Knowledge Index.
This measure is an adaptation of the Transgender Information Scale, which had 17 items.51 It assesses health professionals’ knowledge of trans-specific health needs. Our version is an index composed of 10 items with True/False response options (sample item: There are professional guidelines for practitioners working with transgender clients). Items are summed to create the total score. Higher scores indicate more transgender-related knowledge.
Transgender Stigma Scale.
We developed this scale to measure stigma related to transgender identities among health care providers. Initially, 20 items were generated to assess stigma, with response options on a five-point Likert-type scale ranging from Strongly Disagree (1) to Strongly Agree (5) (sample item: Men who act like women should be ashamed of themselves). Exploratory factor analyses, described below, reduced the number of items from 20 to 12. Items are summed to create the total score. Higher scores indicate higher levels of stigma.
Transgender Health Competencies Scale.
We developed this eight-item scale to assess physicians’ perceived competencies to interact with and provide health care to transgender people. Response options on a five-point Likert-type scale ranged from Definitively Can’t (1) to Definitively Can (5) (sample item: I can ask about body modifications she/he has conducted). Items are summed to create the total score. Higher scores indicate higher self-perceived competence to provide care to transgender individuals.
Transgender Health Willingness Scale.
Our team also developed a nine-item scale to assess physicians’ willingness to provide transgender-sensitive health care to TW. Response options on a five-point Likert-type scale ranged from Definitively Can’t (1) to Definitively Can (5) (sample item: I can listen to a transgender person in a clinical scenario without being judgmental). Items are summed to create the total score. Higher scores indicate greater willingness to discuss transgender-specific health concerns with transgender patients.
Social Desirability Scale.
We used a translated and adapted version of the Marlowe-Crowne Social Desirability Scale,52,53 one of the most widely used scales to measure social desirability with reliability coefficients in the high 70s. Since negative attitudes towards transgender people can be influenced by social desirability, we incorporated this 14-item scale with True/False response options (sample item: I am always willing to admit when I am wrong). Items are summed to create the total score. Higher scores indicate a greater tendency to be influenced by concerns over people’s evaluations of oneself and therefore more social desirability.
Analysis.
Qualitative analysis.
Phase 1 qualitative interviews were transcribed. All transcripts were coded and analyzed using NVivo software (V10).54 Coding occurred in two stages. Stage 1 included in vivo coding, which involved the use of brief summaries or restatements of narratives given by participants that are used to reduce the quantity of meaningful data and to identify an initial set of core themes. This stage also involved the writing of analytic memos describing behavioral and perceptual patterns in the data, which contributed to the development of a code hierarchy including main themes and sub-themes. This process led to the development of a focused codebook. Stage 2 entailed the systematic application of a fixed set of codes that were used to guide all subsequent coding. Three coders worked independently at applying the codebook to all interviews in the NVivo database. Throughout this process, coders met regularly and discussed coding decisions, any difficulties or ambiguities in assigning codes, and presented variations or marginal cases to resolve. Once data were fully coded in NVivo, we performed axial coding procedures involving the examination of patterns in the expression of codes across our sample as well as case analyses that examined the meaning of a code in the lives of specific individuals. The former procedures permitted trends and convergence in the sample, while the latter emphasized the variability and situational expression of themes of interest.
Our analysis of qualitative data in Phase 1 informed the creation of survey items for Phase 2. For example, when we found that stigma presented itself in tacit or indirect ways, we refined our provisional survey measures to detect a broader variability and subtlety of stigmatization. In addition, qualitative data provided some grounded, feasible explanation for certain patterns in the survey data that emerged in Phase 2, as described further below.
Quantitative analysis.
Initially, we conducted the following independent statistical analyses of the survey data. One-way frequency tables were generated using SPSS to characterize the survey sample. Because the transgender stigma, competencies, and willingness scales were newly created for this study, we used exploratory factor analyses (EFA) to explore their factor structure and identify items which did not load strongly on latent factors. The number of factors to extract was determined via scree plots. Items whose factor loadings were not statistically and practically significant (i.e., factor loadings whose values were less than |.50|) were dropped from subsequent analyses.55 Exploratory factor analyses were performed using Mplus 7.456 with an extraction method suitable for ordinal data (Mplus estimator WLSMV).57 Internal reliability for the resulting scales was computed using Cronbach’s coefficient alpha.58
Following validation of the scales, a structural equation model (SEM) was fitted in which a latent transgender stigma factor measured by the Transgender Stigma Scale items was regressed onto the Transgender Knowledge Index score and the latent willingness and competencies factors measured by their respective scales’ items. The SEM was chosen to leverage the presence of multiple indicators of transgender stigma, willingness, and competencies so that the structural associations between these latent constructs could be estimated free of measurement error. The latent transgender stigma factor was also regressed onto the following covariates: age in years, gender (1=male, 2=female), sexual orientation (1=heterosexual, 2=gay/lesbian), geographic location (1=urban, 2=rural), religious affiliation (1=Catholic, 2=Protestant, 3=None, 4=Other), religious importance (1=not important, 2=a little important, 3=important, 4=very important), religious participation (1=no, 2=yes), having received any formal instruction on working with transgender patients (0=no, 1=yes), and social desirability score. Each of the three religion variables were represented by a series of dummy variables with the lowest value set as the reference category. The SEM was fitted using Mplus with the WLSMV estimator. Due to the presence of missing data, 100 multiply-imputed (MI) data sets were generated with the SEM fitted to each imputed dataset and the results summarized using Rubin’s rules for combining results from analyses of MI data.59 Global model fit was determined using the well-established approximate fit criteria recommended by Hu and Bentler60 and Yu61 that any two of the following three conditions be met: Comparative fit index (CFI) ≥ .95, root mean square error of approximation (RMSEA) ≤ .06, and weighted root mean square residual (WRMR) ≤ 1.00. Wald chi-square tests were performed to assess the statistical significance of the multi-category religion variables. For each regression coefficient, we report the unstandardized coefficient B, the standard error of B, the Z-test of the null hypothesis that B is zero, and the corresponding p-values for all effects along with the standardized regression coefficient β.
Triangulation of qualitative and quantitative data.
Following our qualitative and quantitative analyses, we engaged in a series of triangulation discussions in which we compared and contrasted key findings from our qualitative and quantitative analyses. As described in discussions of mixed-methods explanatory designs, qualitative and quantitative findings can permit the identification of provisional hypotheses or extend explanatory power when placed into dialogues while being explicit about the limitations of the specific analytic strategy.62 In particular, our analytic approach focused on: (1) determining the degree to which findings from qualitative and quantitative findings converged on certain common or salient factors; (2) drawing the qualitative data to identify how certain factors (e.g., stigmatization) were perceived or expressed in individual lives; and (3) providing some provisional hypotheses for any patterns in survey analyses that might inform interpretation or future studies. In the Discussion, we reflect on the results of these mixed-methods considerations for our conclusions.
Results
Qualitative interview findings.
Phase 1 participants expressed stigmatization in a variety of ways. One of the most pernicious and subtle was a range of responses from physicians that we described in our analysis as tacit stigma. Expressions of tacit stigma were veiled, and, in some cases, may have expressed beliefs or attitudes that the participants themselves did not perceive to be stigmatizing, but were nevertheless identified as stigmatizing by our team. For example, in response to one of the vignettes in which physicians were required to comment on a hypothetical 18-year-old adolescent male who expressed a desire to change her body in accordance with her female gender identity, one participant [general medicine doctor] explained that a person of such young age is unlikely to have the “maturity” to make such a decision:
The decision at 18 years old is made, but the steps to arrive at a happy ending is going to be a little—to me—more uncomfortable in the young person than in a person 10 years more mature … In my understanding, because the 28-year-old person is more conscious about decision-making, to me, reflecting a decision that is more thought-out.
The decision to wait 10 years, presumably to make the physician feel more comfortable with the patient’s need for gender-affirming medical interventions, does not follow clinical guidelines of most standard transgender health protocols, such as those set forth by the World Professional Association for Transgender Health (WPATH).63 Moreover, this response to a patient likely underestimates the gender dysphoria and potential suffering experienced by many transgender individuals whose gender identity is not affirmed with appropriate clinical support.
The above physician’s discomfort with gender transition is akin to another expression of tacit stigma that involved expressions of moral opinion, rather than reference to medical protocols, in formulating opinions about how to advise transgender patients. Such comments suggest that justifications for clinical decisions can be appropriately made based on personal or moral preferences, rather than protocols based on scientific evidence and expert clinical consensus. For example, when asked about their opinion regarding hormone therapy among TW, one physician specializing in internal medicine explained,
I don’t support that. I think that, well, that each person must accept himself, okay? If they want to do that kind … of thing. Well, no. Because hormones have side effects … And we have to consider that. So, to repeat: that is individual. I don’t recommend it to any patient.
It is difficult to imagine a physician responding in such fashion to almost any other health condition, but when it involves gender dysphoria and the need to transition, apparently the physician quoted found it appropriate to express his opinion in terms of morality, rather than according to established evidence-based clinical guidelines.
Another expression of tacit stigma involved an acknowledgment that transgender people fall between the cracks of the medical system, but rather than this provoking some sense of overall concern for their well-being, this was expressed simply as a fact about medicine. One participant reflected, for instance, on the fact that transgender patients fall between clinical categories for service delivery. This obstetrics/gynecology doctor asked rhetorically, “One thinks, ‘Who does this patient correspond to? In what discipline can we locate this patient?’” However, he did not express any urgency to offer a solution to this hypothetical patient, stating simply “It is because of the system. If she has no reproductive system, she can’t go to OBGYN … She can’t go to a gynecologist who supposedly only sees women.”
Another physician (a pain management doctor) observed that he had problems connecting socially with or understanding lesbian, gay, bisexual, and transgender patients while his nurses were able to talk to them “very naturally,” which he attributed to generational differences: “In fact, they [the nurses] intervene more with these transgender or transsexuals, homosexuals, and talk about their relationships with the nurses, and they tell jokes … And they do it very naturally … I, more professionally, don’t get into that kind of chat.” In other words, some physicians seemed to identify serious gaps in health communication but justified maintaining their distance as a characteristic of appropriate professionalism. These physicians seemed unaware of how challenging health communication may be for many transgender people or the ways this may alienate transgender individuals from medicine entirely.64
Another expression of stigma that was quite common coalesced in our analysis around the notion of “equal treatment to all.” Based on the clinical value of treating the body or physiological system rather than the person, stigmatizing responses in this category tended to sidestep questions of transgender health care access by making rather bland statements such as, “I treat all patients equally.” This was a kind of equality narrative that was ironically used to undermine more substantive consideration of serious gaps in services for transgender people in PR. For example, when asked in the interview about how they would manage an initial clinical interview with a transgender patient, several of our participants responded with phrases such as, “Well, the same as any other patient” [general/alternative medicine doctor], or “One tries to maintain the same line and tries to be the most standardized possible” [psychiatrist] or “Well, I would do the [initial clinical interview] like it is usually done with a feminine woman” [psychiatrist]. This was often connected to a norm expressed by physicians regarding general clinical standards, which they then applied to all patients, even when the patients may have transgender-specific concerns. One participant expressed this explicitly:
[I use] more or less standards or procedures for everyone. I don’t think it [transgender health] is something particular, right? For good health, for everyone, right? Prevention of diseases, screening for diseases, right? [cardiologist/internal medicine doctor]
These physicians were apparently unaware of the multiplicity of needs that transgender people have that simply cannot be subsumed within standard protocols not designed for them or for their specific health concerns.
In sum, while physicians generally viewed themselves as supportive of their patients, many expressed tacit attitudes that delegitimized patients’ concerns, gender-related anxieties, or specific health care needs. When they identified factors that potentially undermined TW’s health or when they were not responsive or communicative about TW’s needs, physicians were generally not solution-oriented and were unaware of existing protocols to support clinicians in providing transgender health care. These factors contributed to a high level of tacit and explicit stigmatization among our participants.
Quantitative survey findings.
The results from Phase 2 (N=255) regarding knowledge, competencies, and willingness to provide services to TW indicated that 39% of respondents believed they had the necessary competencies to provide health services to TW, even though 82% of the sample did not have any formal training on transgender-specific health care. Almost half (47%) reported having provided health services to TW and 30% indicated they do not collect information about gender identity versus sex assigned at birth in their place of work (Table 1). Most participants (71%) were unaware that Gender Dysphoria is classified as a mental health disorder and 40% of them lacked information about standards of care for treating transgender individuals.
With regard to stigma-related attitudes towards TW, 70% of participants were against encouraging male children to explore their feminine side, and 58% had made jokes about men who dress as women. Almost half of the sample (44%) were undecided or against supporting gender-affirmation surgery for a patient. Moreover, 36% of participants believed that people are either men or women with no one in the middle, and 33% thought that men who see themselves as women have mental health problems. Finally, 34% believed that gender-affirmation surgery is an affront to God.
Exploratory factor analysis of the Transgender Stigma Scale found support for a single dominant transgender stigma factor as shown in Figure 1. All factor loadings were equal to or greater than the cutoff of |.50|, except: “If I were providing services to a patient that looked like a female but I suspected to be male, I would ask if he were a transgender person,” “The health needs of transgender women require specialized attention,” “In light of my specialty in medicine, I feel I already have the necessary knowledge for providing services to a transgender person,” “Personnel from my practice do not require specialized training to provide services for transgender women,” “My friends and I on occasions have made jokes about men who look like women,” “If a patient wanted to change sex I would support him/her,” “People should be allowed to experiment with their gender freely,” and “Boys should be encouraged to explore their feminine side.” Two- and three-factor EFA solutions were checked to determine if the eight items with poor loadings in the single-factor solution would group together into a second subscale; however, these solutions revealed multiple split loadings of items across factors, weak factor loadings, and unclear interpretability of the solutions. Accordingly, the single-factor solution was adopted with the eight items not loading strongly onto the stigma factor being dropped. Removal of the eight poorly-performing items resulted in a final Transgender Stigma Scale consisting of 12 items with an alpha reliability of .89 versus the 20 items in the original scale yielding a reduced alpha of .83. The original 20-item scale and the improved shorter 12-item scale correlated at r=.95, indicating that the two versions of the scale share over 90% of their variance.
Figure 1.
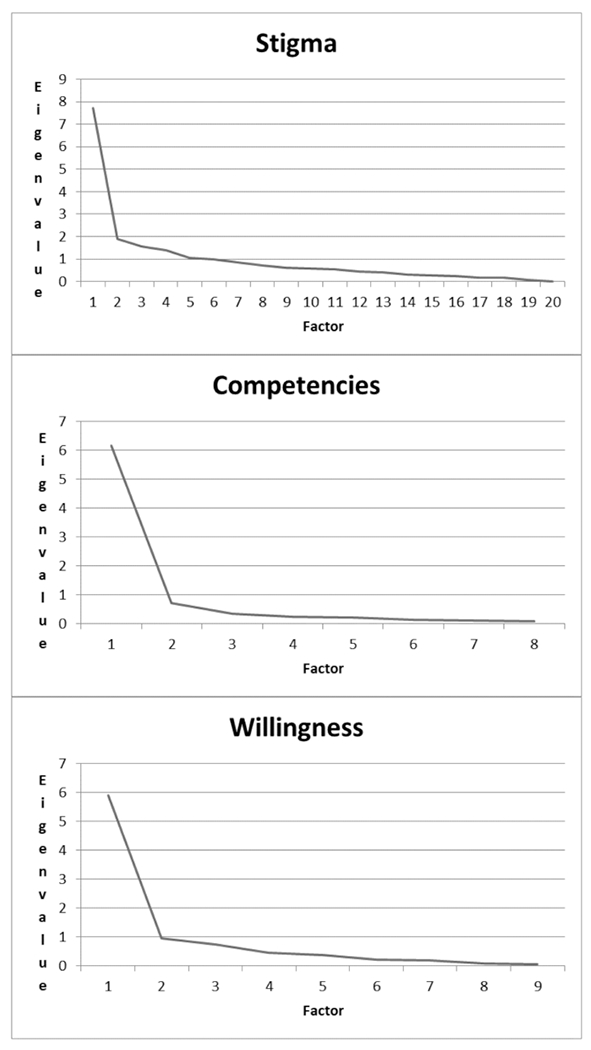
Eigenvalues from exploratory factor analyses.
Exploratory factor analysis of the Transgender Competencies Scale revealed a single dominant factor (Figure 1). Factor loadings ranged from .78 to .94 and therefore exceeded |.50| and were statistically significant, so all eight competencies items were retained. Internal reliability assessment across these items yielded an alpha of .91. Exploratory factor analysis of the Transgender Willingness Scale yielded a single dominant factor (Figure 1). Factor loadings ranged from .61 to .97 and therefore exceeded |.50|, so all nine willingness items were retained. Internal reliability assessment across the nine items resulted in alpha = .90.
The structural equation modeling (SEM) analysis found that the model fit the data well: CFI=.954, RMSEA=.042, and WRMR=1.199 (Figure 2). Higher levels of willingness and knowledge to provide health services to TW were negatively associated with stigma. Self-assessed competencies to provide services to TW was, however, not significantly associated with stigma (Table 2). Religious affiliation exerted a statistically significant effect on stigma levels, with Protestant participants exhibiting more stigma than Catholics. Religious importance was also statistically significant, but the degree of religious participation was not significantly associated with stigma levels. Participants who reported a history of training to work with transgender people reported significantly less stigma than participants who had not received such training. Finally, social desirability was positively associated with stigma. Collectively, the explanatory variables accounted for 59% of the variance in the latent stigma factor.
Figure 2.

Structural equation model results: standardized estimates for structural coefficients (N = 255).a
Notes
aStructural equation model results were estimated using Mplus 7.4’s WLSMV estimator based on 100 multiply-imputed data sets. Estimates are shown for structural associations among focal explanatory variables and transgender stigma only to preserve clarity and are conditional on the following covariates listed in Table 2: Age, gender, sexual orientation, religious affiliation, religion importance, religion participation, previous training in working with transgender populations, and social desirability.
* p < .05
** p < .01
*** p < .001
Table 2.
STRUCTURAL EQUATION MODELING RESULTS (N = 255)a
| Variables | B | SE(B) | Z | p | β |
|---|---|---|---|---|---|
| Competence measured by: | |||||
| I can ask a person directly if she/he is a transgender person. | 1 | — | — | — | 0.738 |
| I can ask about bodily modifications she/he has conducted. | 0.067 | 18.066 | <.001 | 0.887 | |
| I can explore the side effects or health consequences of gender transitioning procedures. | 1.217 | 0.075 | 16.228 | <.001 | 0.898 |
| I can ask if a patient is currently using hormones. | 1.336 | 0.081 | 16.525 | <.001 | 0.986 |
| I can ask if a patient has ever been injected with silicone. | 1.292 | 0.079 | 16.427 | <.001 | 0.954 |
| I can ask him/her about illegal drug use. | 1.116 | 0.085 | 13.108 | <.001 | 0.824 |
| I can ask about engagement in sex work. | 1.131 | 0.072 | 15.688 | <.001 | 0.834 |
| I can explore history of mental health problems with a transgender patient. | 1.125 | 0.077 | 14.591 | <.001 | 0.830 |
| Willingness measured by: | |||||
| If I were to require information on how to improve my clinical services for transgender persons, I can obtain such information. | 1 | — | — | — | 0.653 |
| I can provide general health related services to a transgender person. | 1.145 | 0.085 | 13.497 | <.001 | 0.747 |
| I can speak with a transgender person in a clinical scenario with a feeling anxious. | 1.427 | 0.114 | 12.544 | <.001 | 0.931 |
| I can listen to a transgender person in a clinical scenario without being judgmental. | 1.484 | 0.116 | 12.759 | <.001 | 0.968 |
| I can feel comfortable when interacting with a transgender person in a clinical scenario. | 1.377 | 0.112 | 12.336 | <.001 | 0.898 |
| I can provide a referral to another physician that offers services to transgender persons. | 1.06 | 0.107 | 9.948 | <.001 | 0.691 |
| I can provide quality health services to the transgender population with the information I already have. | 1.088 | 0.09 | 12.099 | <.001 | 0.710 |
| I can provide specialized services to transgender persons based in my specific area of expertise. | 1.073 | 0.092 | 11.65 | <.001 | 0.700 |
| I can feel comfortable with a transgender person in a social scenario. | 1.332 | 0.111 | 12.027 | <.001 | 0.869 |
| Stigma measured by: | |||||
| If I found out that my best friend was changing their sex I would not support him/her. | 1 | — | — | — | 0.764 |
| Changing one sex is an affront God. | 1.213 | 0.112 | 10.869 | <.001 | 0.877 |
| Men who act like women should be ashamed of themselves. | 1.103 | 0.113 | 9.734 | <.001 | 0.820 |
| Children should play with toys appropriate to their own sex. | 0.625 | 0.102 | 6.158 | <.001 | 0.516 |
| Men who see themselves as women have a mental health problem. | 0.929 | 0.1 | 9.263 | <.001 | 0.721 |
| Feminine boys should be treated for their problems by a qualified health professionals. | 0.431 | 0.103 | 4.192 | <.001 | 0.366 |
| I would discourage my son/daughter from having a transgender friend. | 0.912 | 0.104 | 8.811 | <.001 | 0.710 |
| Sex change operation are morally wrong. | 1.123 | 0.113 | 9.899 | <.001 | 0.831 |
| Feminine men make me feel uncomfortable. | 1.151 | 0.097 | 11.886 | <.001 | 0.846 |
| People are either men or women; there should be no middle point. | 1.036 | 0.102 | 10.194 | <.001 | 0.783 |
| I would prefer that colleagues did not refer transgender women to my clinic. | 1.28 | 0.121 | 10.616 | <.001 | 0.910 |
| I would avoid sharing a practice with a colleague that provide services to transgender women. | 1.275 | 0.13 | 9.845 | <.001 | 0.907 |
| Stigma regressed on: | |||||
| Competence | −0.158 | 0.116 | −1.356 | 0.180 | −0.133 |
| Willingness | −0.414 | 0.140 | −2.963 | <.001 | −0.308 |
| Knowledge | −0.994 | 0.344 | −2.886 | 0.004 | −0.189 |
| Age (years) | −0.023 | 0.013 | −1.780 | 0.075 | −0.315 |
| Female Gender | −0.083 | 0.124 | −0.669 | 0.503 | −0.095 |
| Gay/Lesbian Orientation | −0.035 | 0.203 | −0.174 | 0.862 | −0.040 |
| Rural Location | 0.102 | 0.138 | 0.739 | 0.460 | 0.117 |
| Religionb | Wald χ2(3) = 22.46 | <.001 | |||
| Protestant | 0.556 | 0.155 | 3.590 | <.001 | 0.635 |
| None | −0.368 | 0.214 | −1.717 | 0.086 | −0.420 |
| Other | −0.283 | 0.206 | −1.373 | 0.170 | −0.322 |
| Religion Importancec | Wald χ2(3) = 8.17 | 0.043 | |||
| Somewhat important | −0.159 | 0.209 | −0.759 | 0.448 | −0.181 |
| Important | −0.061 | 0.225 | −0.269 | 0.788 | −0.069 |
| Very important | 0.299 | 0.244 | 1.227 | 0.220 | 0.341 |
| Religion Participationd | Wald χ2(2) = 4.33 | 0.115 | |||
| Various yearly | 0.094 | 0.145 | 0.65 | 0.516 | 0.108 |
| Weekly | 0.374 | 0.193 | 1.941 | 0.052 | 0.427 |
| Years Practicing | 0.024 | 0.013 | 1.888 | 0.059 | 0.330 |
| Transgender Training | −0.467 | 0.164 | −2.843 | 0.004 | −0.534 |
| Social Desirability | 0.44 | 0.103 | 4.25 | <.001 | 0.314 |
Notes:
Estimates (B) are averaged over 100 multiply-imputed data sets. Standard errors of B are based on Rubin’s rules for combining standard errors from multiple imputations. Z is the estimate divided by its standard error. p is the p-value for the test that the estimate is zero in the population. β is the standardized regression coefficient.
Reference group: Catholic
Reference group: Not important
Reference group: No participation
Discussion
In the past decade, the transgender population has become more visible in society by means of activism and media presence. There is growing public discourse about gender identity, gender expression, gender nonconformity, and their implications for everyday interactions. Discussions over the use of bathrooms, identity changes in legal documents, and access to work have garnered much attention. In this growing, intense policy debate, scholars should foster a critical reflection on the health disparities faced by the transgender population and the delivery of transgender-specific health care, in order to contribute to an awareness of the challenges faced by this community and the potentially negative impact of stigma on their overall health. Health care providers have a key role to play in reducing TW’s health disparities. Without the engagement of physicians and other health care providers, the delivery of care is inevitably limited. Physicians who are well-informed about transgender health, willing to provide services, and able to do so in a non-stigmatizing manner are therefore of crucial importance to improve the health and well-being of TW in PR and around the globe.65
The findings from our study reflect a challenging scenario for the transgender community in PR. Although the past decade has witnessed efforts to reduce stigma towards specific vulnerable populations, negative attitudes towards those who are perceived to be outside norms still prevail. Our qualitative findings indicate that manifestations of stigma among physicians are often tacit. Our mixed-methods approach was particularly well suited to understand a range of stigma expressions. Although some might interpret tacit expressions of stigma as less severe, our qualitative findings showed how individual moral preferences and the stigma embedded in the logic behind hypothetical medical encounters can shape clinical decision-making, rather than allowing such decision-making to be guided by existing, evidence-based standards of care for working with the transgender population. Perhaps most disconcerting is our finding that some physicians described their management of TW “the same as any other patient” or with similar phrases emphasizing the universality of human biology and the standardization of care without recognition of the specific needs of the transgender population, the health disparities they face, and the intervention strategies required to address their health concerns. These manifestations of transgender stigma are particularly worrisome because they are harder to define and hence may be more difficult to confront in stigma-reduction interventions. Together with our finding that social desirability is associated with higher levels of stigma, tacit stigma manifestations may reflect the ambivalence or limitations experienced by physicians, presenting a barrier to internalizing the clinical importance of recognizing and confronting stigma in their interactions with their transgender patients. For example, tacit stigmatization could be evidence that physicians are aware that social stigma towards transgender individuals is problematic and are able to temper those attitudes in response to general questions, yet are still unable to avoid its manifestation in their relationships with their patients, colleagues, and the public.
These tacit manifestations of stigma were also present in our quantitative findings. A sense of entitlement, commonly ascribed to physicians in positions of power and knowledge, was evident in the fact that even though most had not received formal training to understand TW’s needs and health concerns, participants felt they had the needed competencies to do so. This contrasted with their practices, as those who had provided services to TW had not asked about their gender identity, a crucial part of service delivery. Probably of greatest concern, and a reflection of the gap between TW’s needs and physician’s awareness of such needs, was the fact that most of the sample did not know that Gender Dysphoria is classified as a mental health disorder.
Our quantitative results also provided evidence of more explicit manifestations of stigma. Participants reported difficulty with the exploration of femininity among males and had addressed the issue jokingly. Almost half of the sample understood gender as a binary notion and saw challenges to this fact as a religious affront. We theorize that the anonymity and privacy provided by the survey while gathering data allowed participants to be open about these stigmatizing perspectives.
Conclusion.
To engage physicians in the provision of effective health services for the transgender population, physicians must be properly trained in transgender health and existing evidence-based standards of care to attend to transgender persons’ unique health care needs. Most physicians in our sample, however, lacked this type of training, yet many still felt prepared to provide services. This reflects a serious gap between the reality of their training and their self-reported ability to provide quality care to the transgender population. Physicians’ lack of awareness about Gender Dysphoria as a mental health diagnosis exemplifies the urgent need for training. Such training must consider the cultural context (e.g., religion) in which physicians are embedded, which may influence their attitudes. Moreover, our findings highlight the importance of addressing the knowledge gaps physicians have about TW and their health, along with physicians’ willingness to address patients’ transgender-specific health needs.
We recommend that the training of physicians in transgender health start early on as part of their medical school education and extend throughout their medical, residency, and continuing medical education. As suggested by our quantitative findings, future interventions for this population must specifically address their willingness and knowledge to provide health services to TW, as these are related to transgender stigma. This will allow for the provision of up-to-date, evidence-based knowledge, while simultaneously internalizing the notion that cultural sensitivity is a process that must include confronting the social stigmatization of transgender individuals. Far from treating “every patient the same” as a strategy to reduce transgender stigma, medical education and training must prepare physicians to acknowledge and address the specific needs of this marginalized population.
Acknowledgments
This study was supported by a grant from the National Institute of Mental Health (NIMH) (1R21MH102025-01). The content is solely the responsibility of the authors and does not necessarily represent the official views of NIMH or the National Institutes of Health. Dr. Nelson Varas-Díaz is also included in this study via NIDA support from grant 1K02DA035122. Dr. Rivera-Segarra is included in this study via the Research Center for Minority Institutions support from the NIMHD (G12MD007579).
Contributor Information
Sheilla L. Rodríguez Madera, Florida International University, School of International and Public Affairs.
Nelson Varas Díaz, Florida International University, School of International and Public Affairs.
Mark Padilla, Florida International University, School of International and Public Affairs.
Alíxida Ramos Pibernus, Ponce Health Sciences University, School of Behavioral and Health Sciences.
Torsten B. Neilands, University of California, San Francisco, Center for AIDS Prevention Studies.
Eliut Rivera Segarra, Ponce Health Sciences University, School of Behavioral and Health Sciences.
Carmen M. Pérez Velázquez, University of Puerto Rico, School of Public Health.
Walter Bockting, Columbia University Medical Center, Department of Psychiatry and the School of Nursing.
References
- 1.Institute of Medicine. The health of lesbian, gay, bisexual, and transgender people: building a foundation for better understanding. Washington, DC: The National Academies Press, 2011. [PubMed] [Google Scholar]
- 2.Reisner SL, White JM, Bradford JB, et al. Transgender health disparities: comparing full cohort and nested matched-pair study designs in a community health center. LGBT Health. 2014. September 1;1(3):177–84. 10.1089/lgbt.2014.0009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brennan J, Kuhns LM, Johnson AK, et al. Syndemic theory and HIV-related risk among young transgender women: the role of multiple, co-occurring health problems and social marginalization. Am J Public Health. 2012. September;102(9):1751–7. Epub 2012 Feb 16 10.2105/AJPH.2011.300433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bradford J, Reisner SL, Honnold JA, et al. Experiences of transgender-related discrimination and implications for health: results from the Virginia Transgender Health Initiative Study. Am J Public Health. 2013. October;103(10):1820–9. Epub 2012 Nov 15 10.2105/AJPH.2012.300796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Padilla MB, Rodríguez-Madera S, Varas-Díaz N, et al. Trans-migrations: border-crossing and the politics of body modification among Puerto Rican transgender women. Int J Sex Health. 2016;28(4):261–77. Epub 2016 Oct 4 10.1080/19317611.2016.1223256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bockting WO, Miner MH, Swinburne Romine RE, et al. Stigma, mental health, and resilience in an online sample of the US transgender population. Am J Public Health. 2013. May;103(5):943–51. Epub 2013 Mar 14 10.2105/AJPH.2013.301241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Socias ME, Marshall BDL, Aristegui I, et al. Factors associated with healthcare avoidance among transgender women in Argentina. Int J Equity Health. 2014. September 27;13(1):81 10.1186/s12939-014-0081-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodríguez-Madera SL, Padilla M, Varas-Díaz N, et al. Experiences of violence among transgender women in Puerto Rico: an underestimated problem. J Homosex. 2017;64(2):209–17. Epub 2016 Apr 7 10.1080/00918369.2016.n74026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coulter RW, Kenst KS, Bowen DJ, et al. Research funded by the National Institutes of Health on the health of lesbian, gay, bisexual, and transgender populations. Am J Public Health. 2014. February;104(2):105–12. Epub 2013 Dec 12 10.2105/AJPH.2013.301501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rodríguez-Madera SL, Díaz NV, Pibernus AR, et al. Exploring the feasibility of bio-marker collection for HIV infection and chronic stress among transwomen in Puerto Rico. Rev Puertorriquena Psicol. 2017. Jul-Dec;28(2):268–81. [PMC free article] [PubMed] [Google Scholar]
- 11.Committee on Health Care for Underseved Women. Health care for transgender individuals. Washington, DC: American College of Obstetricians and Gynecologists, 2011. December;512 Available at: https://www.acog.org/Clinical-Guidance-and-Publications/Committee-Opinions/Committee-on-Health-Care-for-Underserved-Women/Health-Care-for-Transgender-Individuals?IsMobileSet=false. [Google Scholar]
- 12.Canadian Council on Social Determinants of Health. A review of frameworks on the determinants of health. Ottawa, Canada: Canadian Council on Social Determinants of Health, 2015. Available at: http://ccsdh.ca/images/uploads/Frameworks_Report_English.pdf. [Google Scholar]
- 13.HealthyPeople 2020. Healthy People 2020 transgender health fact sheet. Washington, DC: U S Department of Health ans Human Services, 2010. Available at: http://callenlorde.org/graphics/2013/03/TransgenderHealthFact.pdf. [Google Scholar]
- 14.McGibbon E, Etowa J, McPherson C. Health-care access as a social determinant of health. Can Nurse. 2008. September;104(7):22–7. [PubMed] [Google Scholar]
- 15.Flores AR, Herman JL, Gates GJ, et al. How many adults identify as transgender in the United States? Los Angeles, CA: The Williams Institute, 2016. Available at: https://williamsinstitute.law.ucla.edu/wp-content/uploads/How-Many-Adults-Identify-as-Transgender-in-the-United-States.pdf. [Google Scholar]
- 16.Safer JD, Coleman E, Feldman J, et al. Barriers to healthcare for transgender individuals. Curr Opin Endocrinol Diabetes Obes. 2016. April;23(2):168–71. 10.1097/MED.0000000000000227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention (CDC). HIV and transgender people. Atlanta, GA: CDC, 2019. Available at: https://www.cdc.gov/hiv/group/gender/transgender/index.html . [Google Scholar]
- 18.Hunt J Why the gay and transgender population experiences higher rates of substance use. Washington, DC: Center for American Progress, 2012. Available at: https://cdn.americanprogress.org/wp-content/uploads/issues/2012/03/pdf/lgbt_substance_abuse.pdf. [Google Scholar]
- 19.Nemoto T, Iwamoto M, Perngparn U, et al. HIV-related risk behaviors among kathoey (male-to-female transgender) sex workers in Bangkok, Thailand. AIDS Care. 2013;24(2):210–9. Epub 2011 Jul 25 10.1080/09540121.2011.597709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Administration de Servicos de Salud Mental y Contra la Adiccion (ASSMCA). Substance disorders use of services in Puerto Rico. Household survey—2008. San Juan, Puerto Rico: ASSMCA, 2009. Available at: https://estadisticas.pr/files/BibliotecaVirtual/estadisticas/biblioteca/ASSMCA/ASSMCA_NA_III_Informe_Final_v4-rev-ms.pdf. [Google Scholar]
- 21.Rodríguez-Madera S TRANS Gender: transiting though the grey zones. SanJuan, PR: Terranova Publisher, 2009. [Google Scholar]
- 22.HealthyPeople.gov Lesbian, gay, bisexual and transgender health. Washington, DC: U S Department ofHealth and Human Services, 2014. Available at: https://www.healthypeople.gov/2020/topics-objectives/topic/lesbian-gay-bisexual-and-transgender-health. [Google Scholar]
- 23.National Alliance on Mental Illness (NAMI). Mental health by the numbers. Arlington, VA: NAMI, 2019. Available at: https://www.nami.org/learn-more/mental-health-by-the-numbers. [Google Scholar]
- 24.Bazargan M, Galvan F. Perceived discrimination and depression among low-income latina male-to-female transgender women. BMC Public Health. 2012. August 15;12:663 10.1186/1471-2458-12-663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rodriguez-Madera S, Ramos-Pibernus A, Padilla M, et al. Radiography of trans communities in Puerto Rico: making visible alternative femininities and masculinities In: Vazquez-Rivera M, Martinez-Taboas A, Francia-Martinez M, et al. , eds. LGBT 101: an introductory view. San Juan, PR: Puerto Rican Publications, 2015:290–314. [Google Scholar]
- 26.Link B, Hatzenbuehler M. Stigma as an unrecognized determinant of population health: research and policy implications. J Health Polit Policy Law. 2016. August;41(4):653–73. Epub 2016 Apr 28 10.1215/03616878-3620869 [DOI] [PubMed] [Google Scholar]
- 27.White Hughto JM, Reisner SL, Pachankis JE. Transgender stigma and health: a critical review of stigma determinants, mechanism, and interventions. Soc Sci Med. 2015. December;147:222–31. Epub 2015 Nov 11 10.1016/j.socscimed.2015.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marmot M Social determinants of health inequalities. Lancet. 2005. March 19-25;365(9464): 1099–104. 10.1016/S0140-6736(05)71146-6 [DOI] [PubMed] [Google Scholar]
- 29.James JS. Explicit, implicit, and behavioral stigmatization of mental illness Dissertations. Hattiesburg, MS: University of Southern Mississippi, 2018. Available at: https://aquila.usm.edu/cgi/viewcontent.cgi?article=2492&context=dissertations. [Google Scholar]
- 30.Ramos-Pibernus AG, Rodríguez-Madera SL, Padilla M, et al. Intersections and evolution of ‘Butch-trans’ categories in Puerto Rico: needs and barriers of an invisible population. Glob Public Health. 2016. Aug-Sep;11(7–8):966–80. Epub 2016 May 4 10.1080/17441692.2016.1180703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fletcher JB, Kisler KA, Reback CJ. Housing status and HIV risk behaviors among transgender women in Los Angeles. Arch Sex Behav. 2014. November;43(8):1651–61. Epub 2014 Sep 5 10.1007/s10508-014-0368-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lyons T, Shannon K, Pierre L, et al. A qualitative study of transgender individuals’ experiences in residential addiction treatment settings: stigma and inclusivity. Subst Abuse Treat Prev Policy. 2015. May 7;10(1):17 10.1186/s13011-015-0015-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Perez-Brumer A, Hatzenbuehler ML, Oldenburg CE, et al. Individual- and structural-level risk factors for suicide attempts among transgender adults. Behav Med. 2015;41(3):164–71. Epub 2015 Aug 19 10.1080/08964289.2015.1028322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Su D, Irwin JA, Fisher C, et al. Mental health disparities within the LGBT population: a comparison between transgender and nontransgender individuals. Transgender Health. 2016. January 1;1(1):12–20. 10.1089/trgh.2015.0001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Winter S, Diamond M, Green J, et al. Transgender people: health at the margins of society. Lancet. 2016. July 23;388(10042):390–400. Epub 2016 Jun 17 10.1016/S0140-6736(16)00683-8 [DOI] [PubMed] [Google Scholar]
- 36.Van Boekel LC, Brouwers EP, van Weeghel J, et al. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013. July 1;131(1-2):23–35. Epub 2013 Mar 13 10.1016/j.drugalcdep.2013.02.018 [DOI] [PubMed] [Google Scholar]
- 37.Varas-Díaz N, Malavé Rivera S, Cintrón-Bou F. AIDS stigma combinations in a sample of Puerto Rican health professionals: qualitative and quantitative evidence. P R Health Sci J. 2008. June;27(2):147–57. [PubMed] [Google Scholar]
- 38.Whitehead J, Shaver J, Stephenson R. Outness, stigma, and primary health care utilization among rural LGBT populations. PLoS One. 2016. January 5;11(1):e0146139 10.1371/journal.pone.0146139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Khalili J, Leung LB, Diamant AL. Finding the perfect doctor: identifying lesbian, gay, bisexual, and transgender-competent physicians. Am J Public Health. 2015. June;105(6):1114–9. Epub 2015 Apr 16 10.2105/AJPH.2014.302448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Snelgrove JW, Jasudavisius AM, Rowe BW, et al. “Completely out-at-sea” with “two-gender medicine”: a qualitative analysis of physician-side barriers to providing healthcare for transgender patients. BMC Health Serv Res. 2012. May 4;12:110 10.1186/1472-6963-12-110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sanchez NF, Sanchez JP, Danoff A. Health care utilization, barriers to care, and hormone usage among male-to-female transgender persons in New York City. Am J Public Health. 2009. April;99(4):713–9. Epub 2009 Jan 15 10.2105/AJPH.2007.132035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rachlin K, Green J, Lombardi E. Utilization of health care among female-to-male transgender individuals in the United States. J Homosex. 2008;54(3):243–58. 10.1080/00918360801982124 [DOI] [PubMed] [Google Scholar]
- 43.Rodríguez-Díaz CE, Jovet-Toledo GG, Vélez-Vega CM, et al. Discrimination and health among lesbian, gay, bisexual and trans people in Puerto Rico. Puerto Rico Heal Sci J. 2016. September;35(3):154–9. [PubMed] [Google Scholar]
- 44.Padilla MB, Rodríguez-Madera S, Ramos Pibernus AG, et al. The social context of hormone and silicone injection among Puerto Rican transwomen. Cult Health Sex. 2018. May; 20(5):574–90. Epub 2017 Sep 1 10.1080/13691058.2017.1367035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Varas-Díaz N, Neilands TB, Rodríguez-Madera SL, et al. The role of emotions in the reduction of HIV/AIDS stigma among physicians in training. AIDS Care. 2016;28(3):376–83. Epub 2015 Oct 7 10.1080/09540121.2015.1090537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Varas-Díaz N, Neilands TB, Cintrón-Bou F, et al. Religion and HIV/AIDS stigma in Puerto Rico: a cultural challenge for training future physicians. J Int Assoc Provid AIDS Care. 2014. Jul-Aug;13(4):305–8. 10.1177/2325957412472935 [DOI] [PubMed] [Google Scholar]
- 47.Michaels PJ, Corrigan PW. Measuring mental illness stigma with diminished social desirability effects. J Ment Heal. 2013. June;22(3):218–26. Epub 2013 Jan 16 10.3109/09638237.2012.734652 [DOI] [PubMed] [Google Scholar]
- 48.Manganelli Rattazzi AM, Volpato C. Social desirability of subtle and blatant prejudice scale. Psychol Rep. 2003. February;92(1):241–50. 10.2466/pr0.2003.92.1.241 [DOI] [PubMed] [Google Scholar]
- 49.Varas-Díaz N, Neilands TB, Cintrín-Bou F, et al. Testing the efficacy of an HIV stigma reduction intervention with medical students in Puerto Rico: the SPACES project. J Int AIDS Soc. 2013. November 13;16(3 Suppl 2). 10.7448/IAS.16.3.18670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Puerto Rico College of Physicians and Surgeons. Puerto Rico College of Physicians and Surgeons presentation to the congressional task force on economic growth in Puerto Rico. San Juan, PR: Puerto Rico College of Physicians and Surgeons, 2016. Available at: https://www.finance.senate.gov/imo/media/doc/Puerto%20Rico%20College%20of%20Physicians%20and%20Surgeons.pdf. [Google Scholar]
- 51.Claman EE. Construction and validation of a “counselor knowledge of attitudes toward transgender issues” scale. Columbus, OH: Ohio Department of Higher Education, 2005. Available at: http://rave.ohiolink.edu/etdc/view?acc_num=osu1382966132. [Google Scholar]
- 52.Crowne DP, Marlow D. A new scale of social desirability independent of psychopathology. J Consult Psychol. 1960. August;24(4):349–54. 10.1037/h0047358 [DOI] [PubMed] [Google Scholar]
- 53.Loo R, Thorpe K. Using reflective learning journals to improve individual and team performance. Team Performance Management. 2002;8(5/6):134–9. 10.1108/13527590210442258 [DOI] [Google Scholar]
- 54.QSR International Pty Ltd. NVivo qualitative data analysis software version 10. Australia: QSR International Pty Ltd, 2014. [Google Scholar]
- 55.Hair J, Tatham R, Anderson R, et al. Multivariate data analysis (5th ed.). Upper Saddle river, NJ: Prentice-Hall, 1998. [Google Scholar]
- 56.Muthén LK, Muthén BO. Mplus user’s guide (7th ed.). Los Angeles, CA: Muthén & Muthén, 2012. [Google Scholar]
- 57.Flora DB, Curran PJ. An empirical evaluation of alternative methods of estimation for confirmatory factor analysis with ordinal data. Psychol Methods. 2004. December;9(4):466–91. 10.1037/1082-989X.9.4.466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951. September;16(3):297–34. 10.1007/BF02310555 [DOI] [Google Scholar]
- 59.Rubin D Multiple imputation for nonresponse in surveys. New York, NY: Wiley, 1987. 10.1002/9780470316696 [DOI] [Google Scholar]
- 60.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model A Multidiscip J. 1999;6(1):1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- 61.Yu C-Y. Evaluating cutoff criteria of model fit indices for latent variable models with binary and continuous outcomes. Los Angelas, CA: University of California, 2002. [Google Scholar]
- 62.Small ML. How to conduct a mixed methods study: recent trends in a rapidly growing literature. Annu Rev Sociol. 2011. August;37:57–86. 10.1146/annurev.soc.012809.102657 [DOI] [Google Scholar]
- 63.The World Professional Association for Transgender Health (WPATH). Standards of care for the health of transsexual, transgender, and gender noncomforming people (vol. 7). East Dundee, IL: WPATH, 2012. Available at: https://www.wpath.org/media/cms/Documents/S0C%20v7/Standards%20of%20Care_V7%20Full%20Book_English.pdf. [Google Scholar]
- 64.Redfern JS, Sinclair B. Improving health care encounters and communication with transgender patients. J Commun Healthc. 2014;7(1):25–40. 10.1179/1753807614Y.0000000045 [DOI] [Google Scholar]
- 65.Reisner SL, Poteat T, Keatley J, et al. Global health burden and needs of transgender populations: a review. Lancet. 2016. July 23;388(10042):412–36. Epub 2016 Jun 17 10.1016/S0140-6736(16)00684-X [DOI] [PMC free article] [PubMed] [Google Scholar]


