Abstract
Purpose
To characterize and compare the initial clinical and imaging features of coronavirus disease 2019 (COVID-19) in pediatric and adult patients undergoing chest CT.
Materials and Methods
A total of 61 patients, consisting of 47 adults (aged 18 years or older) and 14 pediatric patients (aged younger than 18 years) with laboratory-confirmed COVID-19 confirmed by real-time reverse-transcription polymerase chain reaction between January 25 and February 15, 2020, were enrolled in this study. All patients underwent chest CT within 3 days after the initial reverse transcription polymerase chain reaction test. The clinical presentation, serum markers, and CT findings were assessed and compared between the adult and pediatric patients.
Results
Fever was less common in pediatric patients than in adults (six of 14, 42.9% vs 39 of 47, 83%; P = .008). Leukopenia or normal, lymphopenia or normal, and increased or normal C-reactive protein level were common in both groups with no difference (P > .05). Compared with the adults, pediatric patients had a lower rate of positive CT findings and a milder clinical grade (P = .004 and P = .001, respectively). At chest CT, the number of pulmonary lobes involved was found to be reduced in pediatric patients when compared with adults (P = .012). Subpleural distribution of lung opacities was a dominant feature in both groups, whereas bronchial distribution was more common in the pediatric group (P = .048). Among the CT features in adults, ground-glass opacities (GGOs) were the most common finding (24 of 43, 53.5%), followed by GGO with consolidation (14 of 43, 27.9%). In pediatric patients, GGOs accounted for 42.9% (three of seven), bronchial wall thickening occurred in 28.6% (two of seven), and GGOs with consolidations and nodular opacities occurred in 14.3% (one of seven). However, these CT features did not differ in the two groups, except for bronchial wall thickening, which was more commonly found in pediatric patients (P = .048). In addition, the semiquantitative scores of lung involvement were higher in adults than in pediatric patients (8.89 ± 4.54 vs 1.86 ± 2.41; P < .001).
Conclusion
Compared with adults, pediatric patients with COVID-19 showed distinctive clinical and CT features. Pediatric patients tend to have milder clinical symptoms, fewer positive results at CT, and less extensive involvement at imaging. Bronchial wall thickening was relatively more frequent on CT images from pediatric patients with COVID-19 in comparison with adults.
Supplemental material is available for this article.
© RSNA, 2020
Summary
Compared with adults, pediatric patients with COVID-19 showed distinctive characteristics in clinical presentation and CT imaging; pediatric patients tended to have milder clinical symptoms, fewer CT findings, and lesser extent of disease in the lungs. Moreover, peribronchial distribution and bronchial wall thickening, less frequent findings in the adult population with COVID-19, were more commonly seen in pediatric patients.
Key Points
■ Fever was less prevalent in pediatric patients with COVID-19 than in adults (six of 14, 42.9% vs 39 of 47, 83%; P = .008).
■ Compared with adults, pediatric patients had a lower rate of positive CT findings and milder clinical grade (P = .004 and P = .001, respectively).
■ CT features did not differ for the two groups, except for bronchial wall thickening, which was more common in pediatric patients (P = .048).
Introduction
In December 2019, several cases of an unexplained respiratory disease emerged in Wuhan, China, with clinical presentation resembling viral pneumonia. Deep sequencing analysis of respiratory samples revealed a novel coronavirus (severe acute respiratory syndrome coronavirus 2), and the disease it causes was subsequently named coronavirus disease 2019 (COVID-19) (1). Cases of COVID-19 rapidly increased in China and globally (2-4). On March 11, 2020, the World Health Organization declared COVID-19 a pandemic (28).
Similar to other types of pneumonia caused by coronaviruses, such as severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (5–7), patients with COVID-19 also present with fever, cough, dyspnea, and pulmonary parenchymal opacities on chest radiographs (8–10). Reports of SARS in 2003 showed that all age groups were susceptible, but children appeared to be less affected by the disease, with fewer and less severe cases (11). The exact number of children affected globally by SARS is not known because of incomplete age classification in reported cases. It was estimated that only about 5% of people affected were under the age of 18 years, with no child deaths reported (World Health Organization SARS surveillance team) (12,13). Recently, epidemiologic, clinical, and radiologic imaging studies of COVID-19 have emerged, but almost all of them have focused on adult cases, with only a few reporting findings in children (8–10,14). In this study, we conducted a retrospective analysis of the clinical and radiologic features of COVID-19, further comparing the differences between pediatric and adult patients.
Materials and Methods
Patients
Our institutional review board approved the study and waived the requirement for informed written consent. In this study, we reviewed a convenience sample of 62 consecutive patients with COVID-19 diagnosed between January 25 and February 15, 2020, at four tertiary medical units from Guangzhou, China. Inclusion criteria for this study were as follows: (a) patients with COVID-19 confirmed by a real-time reverse-transcription polymerase chain reaction test with nasopharyngeal swabs; (b) patients with a chest CT scan obtained within 3 days from the initial swab test. Suboptimal CT image quality, as judged by the CT readers, was the only exclusion criterion. One patient was excluded because of excessive motion artifacts at CT. Thus, a total of 61 patients were included and were divided into two groups: patients younger than 18 years were included in the pediatric group, whereas patients aged 18 years or older were included in the adult group. According to COVID-19 guidelines (Trial Version 6) released by the National Health Commission of the People’s Republic of China (15), the patients were subdivided into four clinical severity groups: mild, common, severe, and fatal type.
CT Acquisition
The median time from symptom onset to CT scan was 5 days, ranging from 1 to 14 days. Chest CT examinations were performed using multislice helical CT scanners (Philips Brilliance 64-slice CT; Philips, Amsterdam, the Netherlands; Aquilion ONE; Toshiba Medical Systems, Otawara, Japan; Revolution CT; GE Healthcare, Milwaukee, Wis; Siemens Somatom Definition CT scanner; Siemens Healthineers, Erlangen, Germany) without intravenous contrast material. The scanning range was set from the level of thoracic inlet to the lowest costophrenic angle. The imaging parameters were as follows: adults: tube voltage, 120 kV; effective mAs, 180–400 mAs; collimation, 0.625 mm or 0.5 mm; pitch, 0.8 or 1; reconstruction algorithm, filtered back projection; reconstruction slice thickness, 1 mm; interslice gap, 0.2 mm. The estimated effective radiation dose in adults ranged from 2.8 mSv to 3.5 mSv. For children, the parameters were: tube voltage, 100–120 kV; 100–200 mA with automatic exposure control; collimation, 2.0 mm; pitch, 1; reconstruction algorithm, iterative-based reconstruction; reconstruction slice thickness, 0.5 mm; interslice gap, 0 mm. The estimated effective radiation dose in pediatric patients ranged from 0.8 mSv to 1.2 mSv. During the clinical examination, 10% chloral hydrate (5–10 mg/kg) was given to children younger than 3 years or those unable to cooperate (orally administered 30 minutes before the scan) to ensure calm breathing during the scan.
CT Analysis
The CT scans were independently reviewed by two radiologists (D.C. and A.C., with 5 and 18 years of thoracic radiology experience, respectively), who were blinded to the clinical information. Any discrepancies in the interpretation were resolved by consensus reading. The distribution of lung opacities was recorded as peripheral (predominantly involving the outer one-third of the lungs), central (predominantly involving the inner two-thirds of the lungs), central and peripheral (no clear predominance), or peribronchial (predominantly along the bronchovascular bundles). CT images were assessed for the presence of pure ground-glass opacity (GGO), GGO with consolidation, pure consolidation, nodules, bronchial wall thickening, reticular or linear opacities, lymphadenopathy, and pleural effusions (16). A semiquantitative lung severity score was used to assess the extension of pulmonary involvement. Each of the five lung lobes was visually scored from 0 to 4 as follows: 0: no involvement; 1: 1%–25% involvement; 2: 26%–50% involvement; 3: 51%–75% involvement; 4: 76%–100% involvement. The total CT score was the sum of the individual lobar scores and ranged from 0 (no involvement) to 20 (maximum involvement) (10).
Statistical Analysis
The statistical analyses were performed in R (version 3.5.1, https://www.Rproject.org) and Python (version 3.5.6, https://www.python.org). Continuous variables were presented as mean ± standard deviation and categorical data were presented as the percentage of the total, unless otherwise specified. The χ2 test or Fisher exact test was used for testing differences in categorical data between groups. The Kruskal-Wallis H-test was used for testing differences in ordinal variables. A two-tailed P value < .05 indicated statistical significance.
Results
Demographics
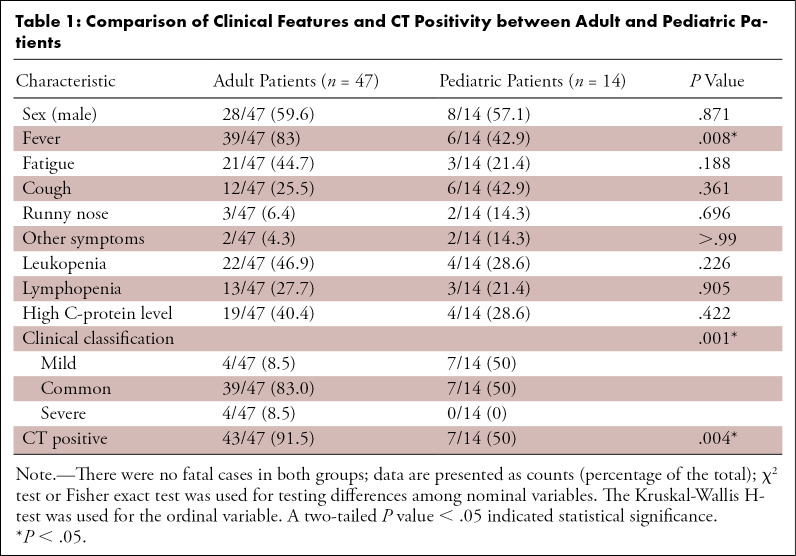
The clinical and laboratory data of the 61 patients are summarized in Table E1 (supplement). The comparison between adult and pediatric patients is shown in Table 1. The age among the 61 patients ranged from 2 months to 81 years (mean age, 39.9 years ± 23.9). There were 14 patients in the pediatric group (aged from 2 months to 10 years, mean, 4.7 years ± 3.4) and 47 patients in the adult group (aged from 20 to 81 years, mean, 50.34 years ± 16.00). The male-to-female ratios in the pediatric and adult groups were 28:21 and 8:6, respectively. No significant difference was found between the two groups in terms of sex composition (P = .871).
Table 1:
Comparison of Clinical Features and CT Positivity between Adult and Pediatric Patients
Presenting Clinical Symptoms
Patients exhibited various symptoms on admission, including fever (45/61, 73.8%), fatigue (24/61, 39.3%), cough (18/61, 29.5%), runny nose (5/61, 8.2%), and diarrhea (2/61, 3.3%). In adults, fever was the dominant symptom (39/47, 83%), followed by fatigue (21/47, 44.7%), cough (12/47, 25.5%), runny nose (3/47, 6.4%), and diarrhea (2/47, 4.3%). In the pediatric group, fever and cough were both seen in 42.9% (6/14), while fatigue and runny nose were seen in 21.4% (3/14) and 14.3% (2/14) of the patients, respectively. Overall, fever was less common in pediatric patients than in adults (6/14, 42.9% vs 39/47, 83%; P = .008).
Laboratory Markers
The prevalence of leukopenia, lymphopenia, and increased C-reactive protein level in adults was 46.9% (22/47), 27.7% (13/47), and 40.4% (19/47), while in the pediatric patients it was 28.6% (4/14), 21.4% (3/14), and 28.6% (4/14), respectively. There were no significant differences between the two groups (P = .226, P = .905, and P = .422, respectively).
Clinical Severity
Mild, common, and severe cases accounted for 8.5% (4/47), 83.0% (39/47), and 8.5% (4/47) of the cases in the adult group, respectively, as well as accounted for 50% (7/14), 50% (7/14), and 0% (0/14) of the cases in the pediatric group, respectively. No fatalities were seen in both groups. There was a significant difference between the two groups in clinical classification (P < .001), with no severe cases seen in the pediatric group.
CT Positivity
CT scans were abnormal in 91.5% (43/47) of adult patients, compared with 50% (7/14) of pediatric patients, resulting in a statistically significantly difference (P = .004).
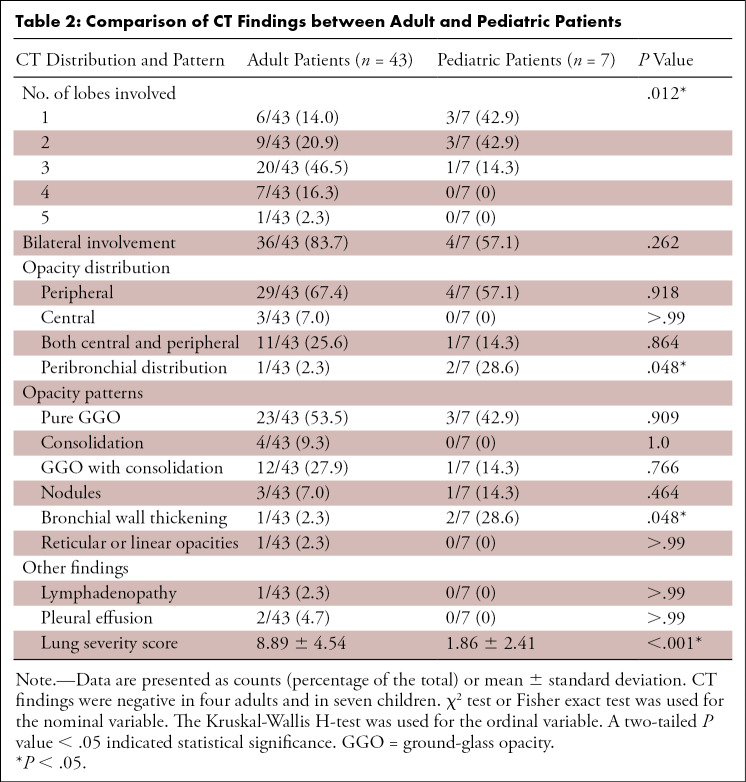
CT Analysis
The imaging characteristics of 50 patients with positive CT findings and the comparisons of CT features between pediatric and adult patients are displayed in Table 2. The number of pulmonary lobes involved by parenchyma opacities was significantly higher in the adult group when compared with the pediatric group (P < .001). Bilateral lung involvement was seen in 83.7% (36/43) of adult patients and in 57.1% (4/7) of pediatric patients, which was not significantly different (P = .262). Subpleural distribution was the most common pattern in both groups, occurring in 67.4% (29/43) of adult patients and 57.1% (4/7) of pediatric patients. Peribronchial distribution was seen in 28.6% (2/7) of pediatric patients versus in 2.3% (1/43) of adult patients (P = .048).
Table 2:
Comparison of CT Findings between Adult and Pediatric Patients
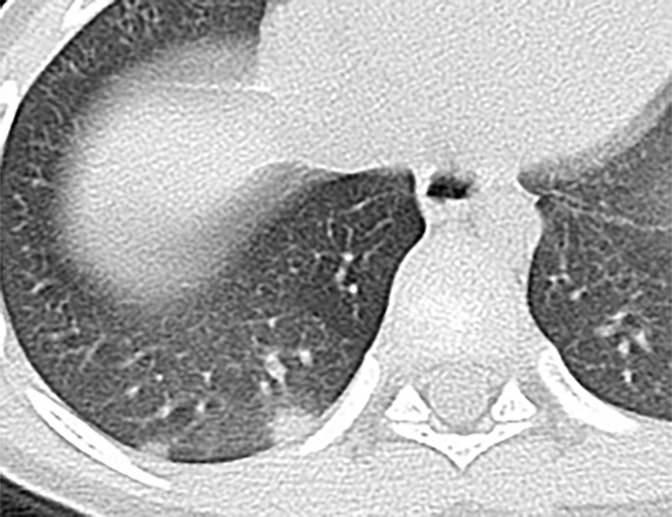
In adults, GGOs were the most common feature (24/43, 53.5%), followed by GGO with consolidations (12/43, 27.9%). In the pediatric group, GGO accounted for 42.9% (3/7), bronchial wall thickening occurred in 28.6% (2/7), and both GGO with consolidations and nodules occurred in 14.3% (1/7) of the CT scans. Other abnormalities, such as mediastinal lymphadenopathy and pleural effusions were rare in both adults (1/43, 2.3% and 2/43, 4.7%, respectively) and pediatric patients (0/14, 0%, for both). In addition, lung severity scores in adults (8.89 ± 4.54) were significantly higher than those of pediatric patients (1.86 ± 2.41; P < .001). CT findings in adult and pediatric patients with COVID-19 are shown in Figures 1 and 2.
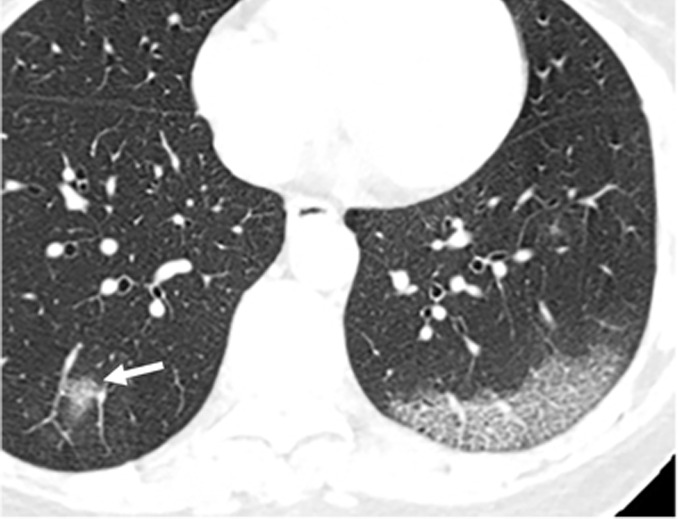
Figure 1a:
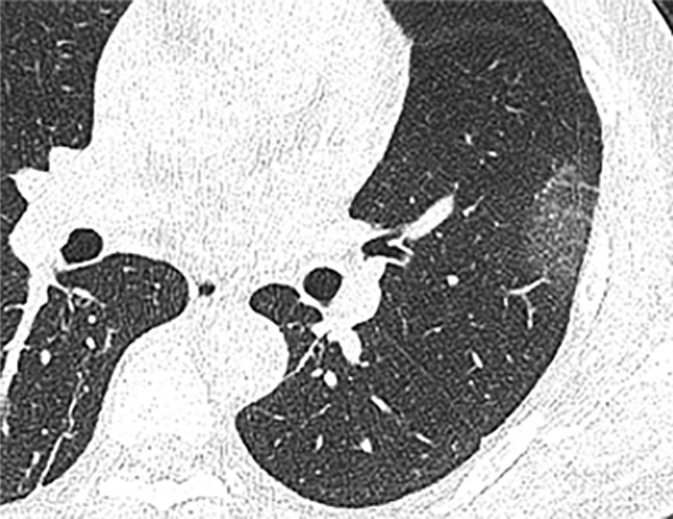
Chest CT findings in adult patients with COVID-19 on transaxial images. (a) Woman, 36 years old, 1 day after symptom onset. Subpleural ground-glass opacity in left lower lobe. (b) Man, 54 years old, 4 days after symptom onset. Subpleural ground-glass opacity in left lower lobe with inter- and intralobular septal thickening (crazy paving) and a ground-glass nodule in the right lower lobe (arrow). (c) Man, 28 years old, 3 days after symptom onset. Subpleural ground-glass opacity in the left lower lobe with central consolidation. (d) Woman, 49 years old, 7 days after symptom onset. Pure consolidation in right lower lobe. (e) Man, 42 years old, 6 days after symptom onset. Bilateral multifocal pure ground-glass opacities. (f) Man, 62 years old, 14 days after symptom onset, bilateral foci of consolidation in both lower lobes, with early linear opacities in a perilobular pattern (arrows).
Figure 2a:
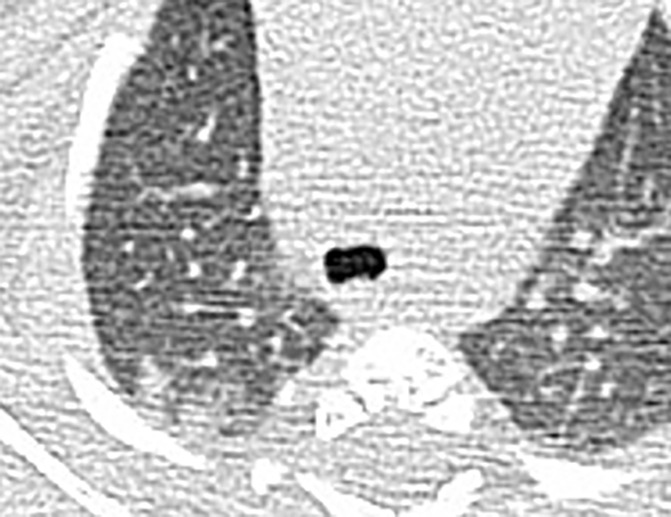
Chest CT findings of pediatric patients with COVID-19 on transaxial images. (a) Male patient, 2 months old, 2 days after symptom onset. Patchy ground-glass opacities (GGOs) in the right lower lobe. (b) Female patient, 4 years old, 4 days after symptom onset, two subpleural nodules in the right lower lobe. (c) Male patient, 8 months old, 6 days after symptom onset. Bronchial wall thickening and peribronchial GGOs and consolidation are noted in the left lower lobe.
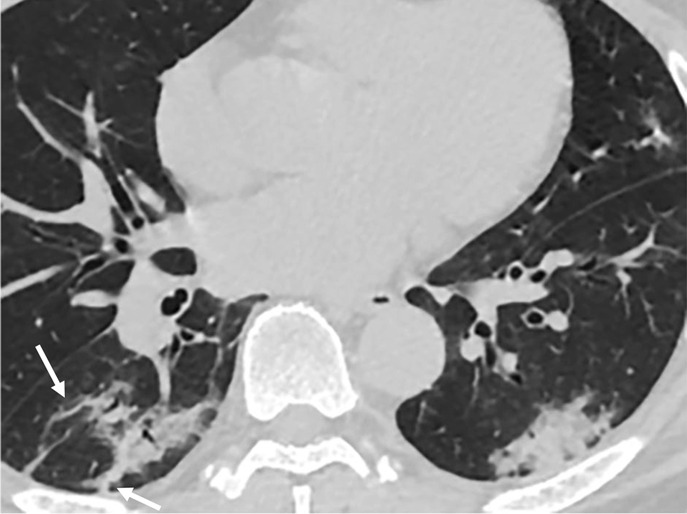
Figure 1b:
Chest CT findings in adult patients with COVID-19 on transaxial images. (a) Woman, 36 years old, 1 day after symptom onset. Subpleural ground-glass opacity in left lower lobe. (b) Man, 54 years old, 4 days after symptom onset. Subpleural ground-glass opacity in left lower lobe with inter- and intralobular septal thickening (crazy paving) and a ground-glass nodule in the right lower lobe (arrow). (c) Man, 28 years old, 3 days after symptom onset. Subpleural ground-glass opacity in the left lower lobe with central consolidation. (d) Woman, 49 years old, 7 days after symptom onset. Pure consolidation in right lower lobe. (e) Man, 42 years old, 6 days after symptom onset. Bilateral multifocal pure ground-glass opacities. (f) Man, 62 years old, 14 days after symptom onset, bilateral foci of consolidation in both lower lobes, with early linear opacities in a perilobular pattern (arrows).
Figure 1c:

Chest CT findings in adult patients with COVID-19 on transaxial images. (a) Woman, 36 years old, 1 day after symptom onset. Subpleural ground-glass opacity in left lower lobe. (b) Man, 54 years old, 4 days after symptom onset. Subpleural ground-glass opacity in left lower lobe with inter- and intralobular septal thickening (crazy paving) and a ground-glass nodule in the right lower lobe (arrow). (c) Man, 28 years old, 3 days after symptom onset. Subpleural ground-glass opacity in the left lower lobe with central consolidation. (d) Woman, 49 years old, 7 days after symptom onset. Pure consolidation in right lower lobe. (e) Man, 42 years old, 6 days after symptom onset. Bilateral multifocal pure ground-glass opacities. (f) Man, 62 years old, 14 days after symptom onset, bilateral foci of consolidation in both lower lobes, with early linear opacities in a perilobular pattern (arrows).
Figure 1d:

Chest CT findings in adult patients with COVID-19 on transaxial images. (a) Woman, 36 years old, 1 day after symptom onset. Subpleural ground-glass opacity in left lower lobe. (b) Man, 54 years old, 4 days after symptom onset. Subpleural ground-glass opacity in left lower lobe with inter- and intralobular septal thickening (crazy paving) and a ground-glass nodule in the right lower lobe (arrow). (c) Man, 28 years old, 3 days after symptom onset. Subpleural ground-glass opacity in the left lower lobe with central consolidation. (d) Woman, 49 years old, 7 days after symptom onset. Pure consolidation in right lower lobe. (e) Man, 42 years old, 6 days after symptom onset. Bilateral multifocal pure ground-glass opacities. (f) Man, 62 years old, 14 days after symptom onset, bilateral foci of consolidation in both lower lobes, with early linear opacities in a perilobular pattern (arrows).
Figure 1e:

Chest CT findings in adult patients with COVID-19 on transaxial images. (a) Woman, 36 years old, 1 day after symptom onset. Subpleural ground-glass opacity in left lower lobe. (b) Man, 54 years old, 4 days after symptom onset. Subpleural ground-glass opacity in left lower lobe with inter- and intralobular septal thickening (crazy paving) and a ground-glass nodule in the right lower lobe (arrow). (c) Man, 28 years old, 3 days after symptom onset. Subpleural ground-glass opacity in the left lower lobe with central consolidation. (d) Woman, 49 years old, 7 days after symptom onset. Pure consolidation in right lower lobe. (e) Man, 42 years old, 6 days after symptom onset. Bilateral multifocal pure ground-glass opacities. (f) Man, 62 years old, 14 days after symptom onset, bilateral foci of consolidation in both lower lobes, with early linear opacities in a perilobular pattern (arrows).
Figure 1f:
Chest CT findings in adult patients with COVID-19 on transaxial images. (a) Woman, 36 years old, 1 day after symptom onset. Subpleural ground-glass opacity in left lower lobe. (b) Man, 54 years old, 4 days after symptom onset. Subpleural ground-glass opacity in left lower lobe with inter- and intralobular septal thickening (crazy paving) and a ground-glass nodule in the right lower lobe (arrow). (c) Man, 28 years old, 3 days after symptom onset. Subpleural ground-glass opacity in the left lower lobe with central consolidation. (d) Woman, 49 years old, 7 days after symptom onset. Pure consolidation in right lower lobe. (e) Man, 42 years old, 6 days after symptom onset. Bilateral multifocal pure ground-glass opacities. (f) Man, 62 years old, 14 days after symptom onset, bilateral foci of consolidation in both lower lobes, with early linear opacities in a perilobular pattern (arrows).
Figure 2b:
Chest CT findings of pediatric patients with COVID-19 on transaxial images. (a) Male patient, 2 months old, 2 days after symptom onset. Patchy ground-glass opacities (GGOs) in the right lower lobe. (b) Female patient, 4 years old, 4 days after symptom onset, two subpleural nodules in the right lower lobe. (c) Male patient, 8 months old, 6 days after symptom onset. Bronchial wall thickening and peribronchial GGOs and consolidation are noted in the left lower lobe.
Figure 2c:

Chest CT findings of pediatric patients with COVID-19 on transaxial images. (a) Male patient, 2 months old, 2 days after symptom onset. Patchy ground-glass opacities (GGOs) in the right lower lobe. (b) Female patient, 4 years old, 4 days after symptom onset, two subpleural nodules in the right lower lobe. (c) Male patient, 8 months old, 6 days after symptom onset. Bronchial wall thickening and peribronchial GGOs and consolidation are noted in the left lower lobe.
Discussion
Fever, fatigue, cough, runny nose, and diarrhea were the most common clinical manifestations in our cohort of adult and pediatric patients with COVID-19. These symptoms are in concordance with previous reports on SARS and Middle East respiratory syndrome, which are also caused by coronaviruses (6,17,18). However, we noted that fever was relatively less common in pediatric patients (42.9% vs 83%). Of note, about half of the pediatric patients had no systemic symptoms, except for mild upper respiratory symptoms such as cough and runny nose; some pediatric patients were asymptomatic. Similar findings were reported in a previous study on SARS (13). This clinical picture is indistinguishable from other viral infections of the upper respiratory tract, thus posing a diagnostic challenge for pediatric patients with COVID-19. In addition, two adult patients only presented with diarrhea, whereas it was not seen in pediatric cases.
Most of the patients in both groups presented normal leukocyte/lymphocyte counts and elevated C-reactive protein level, unlike in a previous study that reported 73% prevalence of leukopenia in adults with COVID-19 (19). We speculate that this discrepancy could be due to differences in patient population and interval between disease onset and hospital presentation. Although the laboratory findings are not specific for viral pneumonia, the lack of leukocytosis may be helpful to distinguish COVID-19 from common bacterial infections. According to the clinical severity classification proposed by the COVID-19 guidelines (Trial Version 6) in China (15), pediatric patients were more likely to have milder clinical presentation than adults, with a higher proportion of normal CT scans (50% vs 8.5%), and less extensive disease on imaging. Therefore, health care systems should consider judicious utilization of routine chest CT for assessing COVID-19 in the pediatric population, balancing the potential risks posed by ionizing radiation against the most common scenario of milder clinical and radiologic disease. Currently, the Society of Thoracic Radiology and the American College of Radiology do not support the use of chest CT for routine screening of COVID-19 (29,30).
In accordance with several recent reports on COVID-19 CT findings (10,20,21), in the adult and pediatric groups, pulmonary opacities involved both lungs and multiple lobes in a predominant peripheral distribution. Although peribronchial distribution was uncommonly seen in both populations, it was relatively more frequent in the pediatric group. In addition, bronchial wall thickening was also more prevalent in the pediatric group. The explanation for these observations is still unclear and could be related to differences in distribution of the coronavirus infection along the respiratory epithelium between the two groups or to the occurrence of coinfection. Further studies focusing on histologic findings of COVID-19 may shed light on these differences.
COVID-19 shares common CT findings with other coronavirus infections, such as SARS and Middle East respiratory syndrome (12,22,23). Notably, the pediatric population generally displayed a milder and slightly diverse range of CT manifestations when compared with adults. None of these manifestations are specific for COVID-19; therefore, differentiation from other viral and opportunistic pneumonias is needed based on clinical and laboratorial workup (24-27). Exposure history and access to reverse transcription polymerase chain reaction testing is essential for making the diagnosis of COVID-19.
There were several limitations in our study. First, the sample size is small in the pediatric group, which can limit the study power. Second, we could not control for geographic factors, as our patients were from different medical centers, or for CT scanning parameters. However, we assume that these observations may reflect the most typical scenario encountered across centers globally. Third, we only analyzed the clinical and CT manifestations at initial medical center presentation. Further studies including clinical follow-ups are needed to determine if the observations in the pediatric group are sustained throughout the course of disease. Finally, given the retrospective nature of the study, we were not able to determine the presence or impact of coinfection on the observed CT findings.
In summary, pediatric patients with COVID-19 have relatively milder clinical symptoms, a higher prevalence of negative CT scans, and decreased disease extension on imaging than adult patients. These observations should be heavily weighted when balancing the risk-benefit ratio for using chest CT in the pediatric population with COVID-19. Currently, most of the imaging societies and the Centers for Disease Control and Prevention do not recommend routine screening for COVID-19 with chest CT, and the confirmatory diagnosis relies on reverse-transcription polymerase chain reaction testing. Although peribronchial distribution of the lung opacities and bronchial wall thickening are atypical CT findings in COVID-19, they were relatively more frequent in the pediatric population.
SUPPLEMENTAL TABLE
Disclosures of Conflicts of Interest: A.C. disclosed no relevant relationships. J.H. disclosed no relevant relationships. Y.L. disclosed no relevant relationships. Z.L. disclosed no relevant relationships. D.C. disclosed no relevant relationships. C.Y. disclosed no relevant relationships. R.Y. disclosed no relevant relationships. X.W. disclosed no relevant relationships.
Abbreviations:
- COVID-19
- coronavirus disease 2019
- GGO
- ground-glass opacity
- SARS
- severe acute respiratory syndrome
References
- 1.World Health Organization . Novel coronavirus – China. http://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/. Published January 12, 2020. Accessed January 19, 2020. [Google Scholar]
- 2.World Health Organization . Novel coronavirus – Thailand (ex-China). http://www.who.int/csr/don/14-january-2020-novel-coronavirus-thailand/en/. Published January 14, 2020. Accessed January 19, 2020.
- 3.World Health Organization . Novel coronavirus – Japan (ex-China). http://www.who.int/csr/don/17-january-2020-novel-coronavirus-japan-ex-china/en/. Published January 17, 2020. Accessed January 19, 2020.
- 4.World Health Organization . Novel coronavirus – Republic of Korea (ex-China). http://www.who.int/csr/don/21-january-2020-novel-coronavirus-republic-of-korea-ex-china/en/. Published January 21, 2020. Accessed January 23, 2020.
- 5.Ksiazek TG, Erdman D, Goldsmith CS, et al. A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med 2003;348(20):1953–1966. [DOI] [PubMed] [Google Scholar]
- 6.de Groot RJ, Baker SC, Baric RS, et al. Middle East respiratory syndrome coronavirus (MERS-CoV): announcement of the Coronavirus Study Group. J Virol 2013;87(14):7790–7792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuiken T, Fouchier RA, Schutten M, et al. Newly discovered coronavirus as the primary cause of severe acute respiratory syndrome. Lancet 2003;362(9380):263–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395(10223):497–506 [Published correction appears in Lancet 2020;395(10223):496.]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shi H, Han X, Zheng C. Evolution of CT Manifestations in a Patient Recovered from 2019 Novel Coronavirus (2019-nCoV) Pneumonia in Wuhan, China. Radiology 2020;295(1):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chung M, Bernheim A, Mei X, et al. CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV). Radiology 2020;295(1):202–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leung CW, Chiu WK. Clinical picture, diagnosis, treatment and outcome of severe acute respiratory syndrome (SARS) in children. Paediatr Respir Rev 2004;5(4):275–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Assiri A, Al-Tawfiq JA, Al-Rabeeah AA, et al. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect Dis 2013;13(9):752–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hon KL, Leung CW, Cheng WT, et al. Clinical presentations and outcome of severe acute respiratory syndrome in children. Lancet 2003;361(9370):1701–1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fang Y, Zhang H, Xu Y, Xie J, Pang P, Ji W. CT Manifestations of Two Cases of 2019 Novel Coronavirus (2019-nCoV) Pneumonia. Radiology 2020;295(1):208–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.China National Health Commission . Diagnosis and treatment of pneumonitis caused by new coronavirus (trial version 6). Beijing: China National Health Commission. http://www.nhc.gov.cn/yzygj/s7653p/202001/4294563ed35b43209b31739bd0785e67.shtml. Published January 27, 2020. Accessed February 5, 2020. [Google Scholar]
- 16.Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology 2008;246(3):697–722. [DOI] [PubMed] [Google Scholar]
- 17.Peiris JS, Lai ST, Poon LL, et al. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet 2003;361(9366):1319–1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee N, Hui D, Wu A, et al. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med 2003;348(20):1986–1994. [DOI] [PubMed] [Google Scholar]
- 19.Song F, Shi N, Shan F, et al. Emerging 2019 Novel Coronavirus (2019-nCoV) Pneumonia. Radiology 2020;295(1):210–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lei J, Li J, Li X, Qi X. CT Imaging of the 2019 Novel Coronavirus (2019-nCoV) Pneumonia. Radiology 2020;295(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kanne JP. Chest CT Findings in 2019 Novel Coronavirus (2019-nCoV) Infections from Wuhan, China: Key Points for the Radiologist. Radiology 2020;295(1):16–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paul NS, Roberts H, Butany J, et al. Radiologic pattern of disease in patients with severe acute respiratory syndrome: the Toronto experience. RadioGraphics 2004;24(2):553–563. [DOI] [PubMed] [Google Scholar]
- 23.Ooi GC, Khong PL, Müller NL, et al. Severe acute respiratory syndrome: temporal lung changes at thin-section CT in 30 patients. Radiology 2004;230(3):836–844. [DOI] [PubMed] [Google Scholar]
- 24.Dela Cruz CS, Wunderink RG. Respiratory Viral and Atypical Pneumonias. Clin Chest Med 2017;38(1):xiii–xiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gong L, Zhang CL, Zhen Q. Analysis of clinical value of CT in the diagnosis of pediatric pneumonia and mycoplasma pneumonia. Exp Ther Med 2016;11(4):1271–1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang Q, Zhang Z, Shi Y, Jiang Y. Emerging H7N9 influenza A (novel reassortant avian-origin) pneumonia: radiologic findings. Radiology 2013;268(3):882–889. [DOI] [PubMed] [Google Scholar]
- 27.Bai L, Gu L, Cao B, et al. Clinical features of pneumonia caused by 2009 influenza A(H1N1) virus in Beijing, China. Chest 2011;139(5):1156–1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organization . WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. Published March 11, 2020. Accessed January 23, 2020. [Google Scholar]
- 29.American College of Radiology . ACR Recommendations for the use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection. https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection. Published March 11, 2020. Accessed March 22, 2020. [Google Scholar]
- 30.Society of Thoracic Radiology . STR/ASER COVID-19 Position Statement, March 11, 2020. https://thoracicrad.org/. Published March 11, 2020. Accessed March 22, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.