Abstract
Coronavirus disease 2019 (COVID-19) has quickly spread since it was first detected in December 2019 and has evolved into a global pandemic with over 1.7 million confirmed cases in over 200 countries around the world at the time this document is being prepared. Owing to the novel nature of the virus and the rapidly evolving understanding of the disease, there is a great deal of uncertainty surrounding the diagnosis and management of COVID-19 pneumonia in pediatric patients. Chest imaging plays an important role in the evaluation of pediatric patients with COVID-19; however, there is currently little information available describing imaging manifestations of COVID-19 in pediatric patients and even less information discussing the utilization of imaging studies in pediatric patients. To specifically address these concerns, a group of international experts in pediatric thoracic imaging from five continents convened to create a consensus statement describing the imaging manifestations of COVID-19 in the pediatric population, discussing the potential utility of structured reporting during the COVID-19 pandemic, and generating consensus recommendations for utilization of chest radiographs and CT in the evaluation of pediatric patients with COVID-19. The results were compiled into two structured reporting algorithms (one for chest radiographs and one for chest CT) and eight consensus recommendations for the utilization of chest imaging in pediatric COVID-19 infection.
© RSNA, 2020
Summary
A group of international experts in pediatric thoracic imaging from five continents convened to create a consensus statement describing the imaging manifestations of pediatric COVID-19, describing two structured reporting algorithms for pediatric radiology reports (one for chest radiographs and one for chest CT) and defining eight consensus recommendations for the utilization of chest imaging in pediatric patients with known or suspected COVID-19 infection.
Key Points
■ Imaging is not indicated for pediatric patients presenting with mild clinical symptoms unless the patient has risk factors for disease progression or develops worsening clinical symptoms.
■ Sequential chest radiograph examinations, ordered on an as-needed clinical basis, are indicated for pediatric patients with COVID-19 to assess response to therapy, evaluate clinical deterioration, or assess the positioning of life support devices.
■ Post-recovery follow-up imaging is not recommended for asymptomatic pediatric patients with a mild COVID-19 disease course; however, it may be considered in asymptomatic individuals with an initial moderate-to-severe disease course or symptomatic individuals regardless of initial disease severity depending on the level of clinical concern for long-term lung injury.
Introduction
Coronavirus disease 2019 (COVID-19) is a viral infection caused by the severe acute respiratory syndrome coronavirus 2, a member of the β-coronavirus cluster of enveloped single-stranded RNA viruses. This novel viral infection first presented as a series of unexplained cases of pneumonia in Wuhan, China, in December 2019 (1,2). The virus spread rapidly, predominantly through person-to-person transmission via respiratory droplets or direct contact and was declared a pandemic by the World Health Organization on March 11, 2020 (3). As of April 13, 2020, there have been 1,773,084 confirmed cases of COVID-19 and 111 652 deaths across 200 countries and territories globally. In the United States, there have been 524 514 confirmed cases and 20 444 reported deaths (4).
Although COVID-19 predominantly affects the adult population, recently there have been increasing reports in the media of infected pediatric patients and young adults, especially in the United States. Furthermore, although pediatric patients are more likely to have a milder clinical course, they are just as likely as adults to become infected and thus play an important role in ongoing disease transmission (5,6). Unfortunately, despite increasingly reported pediatric cases and their potential role in disease spread, the published literature for pediatric COVID-19 infections is limited, particularly with regard to imaging manifestations of pediatric COVID-19 pneumonia. However, within the currently available scarce literature, there are differences emerging in imaging features between pediatric and adult cases of COVID-19 pneumonia of which both radiologists and referring physicians should be aware.
Given the nonspecific clinical presentation of COVID-19, imaging studies are likely to play an important role in the diagnostic workup for affected pediatric patients. The lack of published information can lead to unease and diagnostic uncertainty for pediatric and general radiologists, both in identifying findings suggestive of COVID-19 and in determining appropriate use of imaging for the pediatric population with suspected COVID-19 infection. As the pandemic continues to flourish, practical guidance is needed to address both of these concerns for practicing radiologists and referring physicians.
Therefore, the aim of this study is to generate a consensus statement for chest imaging in pediatric patients with COVID-19 infection by international experts from five continents. Existing literature and clinical experience among the expert panel was utilized to describe imaging manifestations of COVID-19 in the pediatric population, discuss the potential utility of structured reporting during the COVID-19 pandemic, and report consensus recommendations for the utilization of chest radiographs and CT in the evaluation of COVID-19.
Methods
This consensus statement is based on expert opinions from six pediatric thoracic radiologists from six countries across five continents, such as the United States, Spain, Hong Kong, Brazil, South Africa, and United Emirates. Several members of the panel have experience with managing pediatric patients during the current pandemic, as well as during prior pandemics including severe acute respiratory syndrome, Middle East respiratory syndrome, and swine-origin influenza A (7–14). The panel met via a single live audio-conference and videoconference call in addition to extensive discussions via direct phone calls and email communications among members of the panel. Standardized reporting recommendations grouping chest radiograph and CT findings into four diagnostic categories were also discussed until consensus was achieved.
The final document is supported by an extensive literature review utilizing the search terms “((COVID-19 OR Coronavirus 2019 OR SARS-CoV2 OR nCoV) AND (pediatric OR children) AND (radiology OR imaging OR CT OR computed tomography OR CXR))” that revealed 46 related articles in the English literature. These articles were reviewed for content, and eight articles with sufficient pediatric COVID-19 pneumonia-related imaging data were used to generate a summary of imaging findings. The institutional review board waived informed consent as all imaging studies reviewed were obtained as part of routine patient care and patient risk is minimal. New images from two previously reported patients (American Journal of Roentgenology article in press), which are different than the images used in that article, are included in this article for illustrative purposes rather than the imaging data analyzed for the original research (14).
Imaging in Pediatric Patients with COVID-19
The role of radiologic examinations in initial diagnosis, evaluation of disease progression, and prognostication is currently an area of active research and discussion among the medical community. Multiple factors including sensitivity and specificity of radiologic examinations, availability and accuracy of reverse-transcription polymerase chain reaction (RT-PCR) tests, and radiation dose considerations should be considered when making decisions regarding imaging in pediatric patients suspected of having COVID-19 infection. Ultimately, many pediatric patients will undergo some level of imaging evaluation, and thus, an understanding of imaging findings in COVID-19 is essential for practicing general and pediatric radiologists.
Considerations for Standardized Reporting of Imaging Findings for COVID-19 in Pediatric Patients
Given the rapid onset of the COVID-19 pandemic, the continually evolving understanding of the imaging manifestations of the disease, and the implications of the diagnosis for both patients and providers, many radiologists feel hesitant about when or whether to specify COVID-19 pneumonia in the differential diagnosis. Structured reporting may help address this concern by creating defined categories for imaging findings and standard language that can lead to improved understanding between the radiologist and ordering provider. Utilization of structured radiology reports has been shown to improve recall and decrease incorrect diagnoses by referring physicians compared with unstructured reports (15). Furthermore, structured reporting may offer additional potential benefits such as improved reporting of key imaging features and increased confidence and clarity of terminology used by the radiologist (16,17).
There are a few limitations of structured reporting for COVID-19 that merit mention. First, the utilization of a COVID-19 structured template will be best employed in regions where there is a high prevalence of the disease. There is some overlap in the imaging presentation of COVID-19 and other entities, including infections (influenza A, influenza B, or Mycoplasma pneumoniae), inflammatory processes (electronic cigarette vaping–associated lung injury or hypersensitivity pneumonitis), and eosinophilic lung disease in the pediatric population, and therefore, a low COVID-19 prevalence could lead to false-positive results (13,14,18–24). Second, introducing the term COVID-19 pneumonia into the patient’s clinical record may cause ordering physicians to feel constrained in future clinical decision making. Open and careful discussion with the referring doctor concerning the level of clinical suspicion for COVID-19 should help mitigate these issues. In some cases, following discussion with the clinical team, it may be appropriate to utilize more broad terms such as viral or atypical pneumonia depending on the clinical picture.
Ultimately, the decision to pursue standardized reporting for pediatric COVID-19 pneumonia will depend on individual practice patterns, as well as disease incidence within the practice location, and is likely best achieved through discussion between radiologists and referring providers. This study provides recommendations of what structured vocabulary would look like for groups that choose to pursue this option.
Chest Radiography
Imaging Findings of COVID-19 on Chest Radiographs in Pediatric Patients
Although chest radiography is frequently the first imaging study in the evaluation of a pediatric patient presenting with fever, cough, and/or shortness of breath, the current literature describing COVID-19 findings on chest radiographs is relatively scare. The limited data available suggest that chest radiography, at least in adults, is less sensitive than CT for identifying imaging findings associated with COVID-19. In one study of nine COVID-19 positive adults, chest radiographs showed bilateral patchy consolidation with associated ground-glass opacity in a peripheral and lower lung zone predominant pattern in 33.3% (three of nine) of cases. while chest CT demonstrated lung parenchymal abnormality in 88.9% (eight of nine) of cases (25). In a follow-up study, which included the aforementioned nine patients plus eight additional adult cases, chest radiography had a median sensitivity of 25% (among eight thoracic radiologists; interquartile range, 20%–26.3%) and median specificity of 90% (interquartile range, 88.8%–96.3%) for identifying lung opacities identified on same-day chest CT (26). Ng et al reported normal chest radiographs in 40% (two of five) and ground-glass opacities in 60% (three of five) of adult patients with COVID-19, although all (five of five, 100%) patients were found to have peripheral predominant ground-glass opacities on CT (27). Sequential chest radiography in the three radiographically positive cases showed initial progression of lung consolidation followed by improvement in 66.7% (two of three) of patients and no change in 33.3% (one of three), suggesting radiography may be helpful in evaluating disease progression/resolution (27).
Published data of chest radiograph findings of COVID-19 pneumonia are even more scarce in the pediatric population, although one case series with 10 pediatric patients observed unilateral patchy opacities in 40% (four of 10) of cases (28). In the clinical experience of this expert panel of pediatric chest radiologists, both unilateral and bilateral opacities have been observed in pediatric COVID-19, although bilateral opacities are more typical (Figs 1, 2). Chest radiography is perhaps even more essential in this patient population due to the increased radiation sensitivity of children and hesitancy to pursue cross-sectional imaging such as CT; thus, continued investigation and reporting of observed pediatric chest radiograph abnormalities in COVID-19 is imperative.
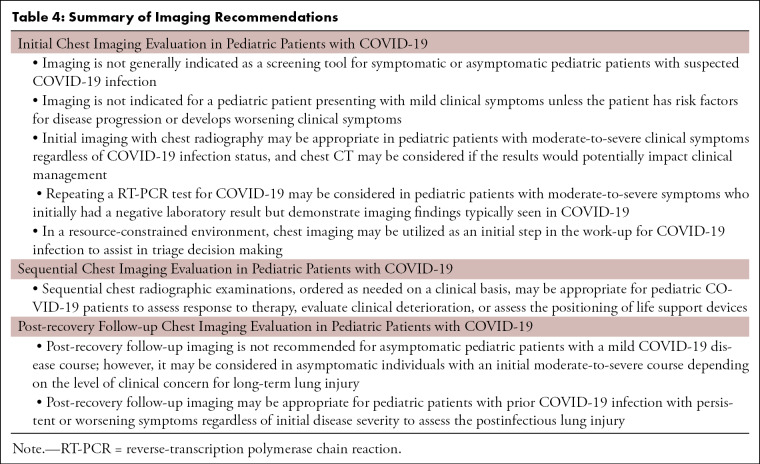
Figure 1:
A 16-year-old female with tuberous sclerosis and a positive COVID-19 RT-PCR test who presented with acute hypoxic respiratory distress. The frontal chest radiograph shows bilateral lower-lung zone-predominant consolidation and ground-glass opacities, which are typical chest radiographic findings of pediatric COVID-19 pneumonia. Also noted are the endotracheal tube and nasogastric tube.
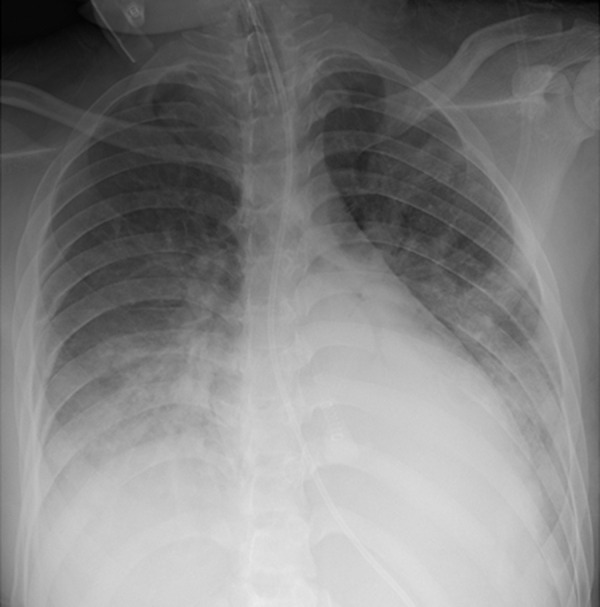
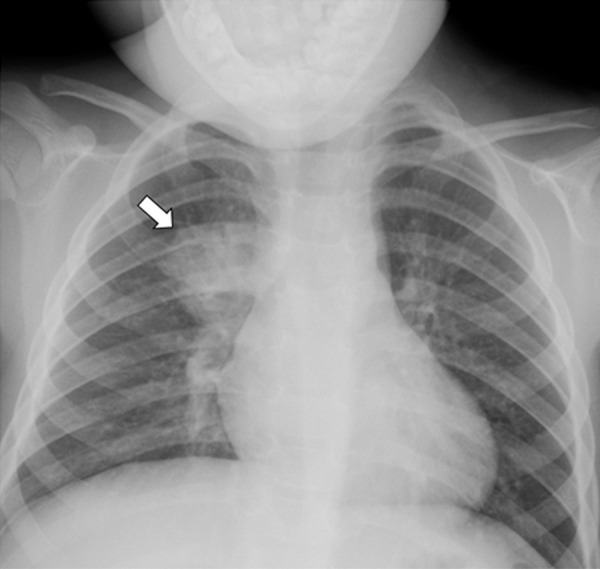
Figure 2:
A 15-year-old female with asthma and a positive COVID-19 RT-PCR test who presented with fever and respiratory distress. The frontal chest radiograph shows ground-glass opacities in both peripheral (*) and central (arrow) distribution, which are indeterminate chest radiographic findings of pediatric COVID-19 pneumonia. Also noted is the right apical pneumothorax.
Current Recommendations for Chest Radiography in Pediatric Patients with Suspected or Known COVID-19
On the basis of very limited data, chest radiographs may show patchy opacities with peripheral and lower lung zone predominance; however, they are less sensitive than CT for detecting parenchymal abnormalities in pediatric patients with COVID-19. According to the American College of Radiology Appropriateness Criteria, imaging is not indicated in a well-appearing immunocompetent child ≥ 3 months of age who does not require hospitalization. However, if the child is not responding to outpatient management, requires hospitalization, or is suspected of having hospital-acquired pneumonia, chest radiography is considered the most appropriate first step in imaging evaluation (29). Thus, as with other viral pulmonary infections, initial chest radiographs are not indicated in pediatric patients with mild symptoms but should be considered in pediatric patients with suspected COVID-19 presenting with moderate-to-severe acute respiratory illness symptoms. However, due to limited sensitivity and specificity, a negative chest radiograph does not exclude pulmonary involvement in patients with laboratory-confirmed COVID-19 nor does it indicate the absence of COVID-19 infection in cases of suspected COVID-19 infection not yet confirmed by using RT-PCR testing.
Serial chest radiography to assess response to supportive treatment and/or disease progression may be beneficial in pediatric COVID-19 patients with positive findings on initial chest radiographs and/or in cases of clinical deterioration.
Structured Chest Radiography Reporting Recommendations in Pediatric Patients with Suspected or Known COVID-19
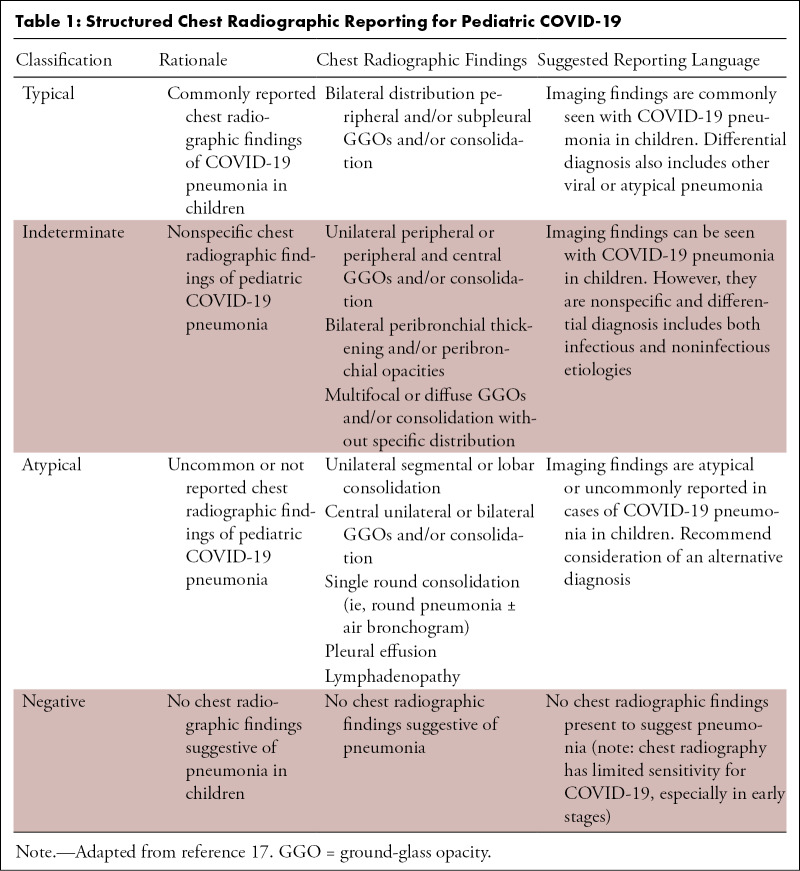
Suggested structured reporting for chest radiographic findings for pediatric patients undergoing a workup for COVID-19 pneumonia divides imaging manifestations into four distinct categories: typical, indeterminate, atypical, and negative. Given the extremely limited pediatric data for chest radiographic findings in COVID-19 pneumonia, recommendations are based on a combination of patterns observed in the literature for adults and observational experience of the expert panel at the time of meeting (Table 1). These recommendations may evolve as the understanding of COVID-19 continues to improve.
Table 1:
Structured Chest Radiographic Reporting for Pediatric COVID-19
Typical chest radiographic finding classification.—The typical chest radiographic finding classification is used to denote the imaging pattern most suggestive of COVID-19 pneumonia, namely, bilateral peripheral and/or subpleural ground-glass opacities and/or consolidation (Fig 1). The structured reporting language for this group should reflect that the chest radiographic imaging pattern is commonly seen in children with COVID-19 pneumonia; however, other viral or atypical pneumonia would also be differential considerations.
Indeterminate chest radiographic finding classification.— The indeterminate chest radiographic finding classification includes imaging findings that have been observed in COVID-19 pneumonia but are less specific than those of the typical group such as unilateral nonsegmental/lobar ground-glass or consolidative opacities or multifocal ground-glass/consolidative opacities without any particular distribution (Fig 2). Features typical of viral pneumonia and reactive small airways disease, such as peribronchial thickening and/or opacities, are also included in this group and have been observed more frequently in pediatric COVID-19 pneumonia cases than in adults (30).
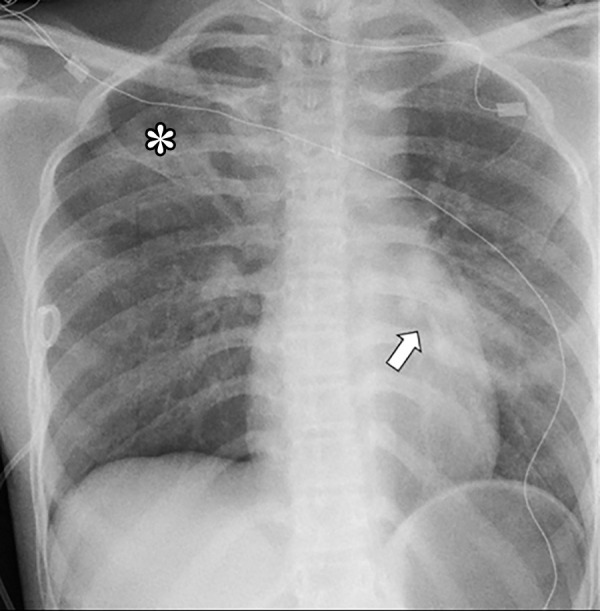
Atypical chest radiographic finding classification.—The atypical chest radiographic finding classification is reserved for the chest radiographic imaging findings that are infrequently observed in COVID-19 pneumonia and suggest that an alternative diagnosis should be considered. Chest radiographic findings for this group include unilateral segmental or lobar consolidation suggestive of bacterial pneumonia (Fig 3), a central distribution of parenchymal opacities, a single round consolidation (ie, round pneumonia with or without an air bronchogram) (Fig 4), pleural effusion, and lymphadenopathy.
Figure 3:
A 9-year-old female with a renal transplant and a positive COVID-19 RT-PCR test who presented with respiratory distress. The frontal chest radiograph shows consolidation (*) in the left lower lobe, which is atypical for pediatric COVID-19 pneumonia.
Figure 4:
A 4-year-old male with fever and respiratory distress. The frontal chest radiograph shows a round consolidation (arrow) in the medial right upper lung zone which is atypical for pediatric COVID-19 pneumonia. This patient’s round pneumonia was due to bacterial infection.
Negative chest radiographic finding classification.—Finally, the negative chest radiographic finding classification is used to describe a chest radiographic study with no evidence of pneumonia. However, given the limited sensitivity of chest radiography for detection of COVID-19 pneumonia, a statement to this effect may be included in the structured language for this category.
Chest CT
Imaging Findings of COVID-19 on Chest CT in Pediatric Patients
The chest CT findings observed in COVID-19, most commonly described as bilateral multifocal peripheral and/or subpleural ground-glass opacities, often in a posterior and/or lower lobe predominant distribution, with or without consolidation, have mainly been described in the literature on adults (31–40). Although the imaging literature in pediatric patients is less robust, overall, pediatric patients tend to demonstrate milder imaging findings compared with those of adults. A study evaluating CT findings in 98 COVID-19 positive patients across multiple age groups found that pediatric patients (< 18 years old) had a lower total number of pulmonary lesions and smaller size of pulmonary lesions compared with adults (41). Similarly, a comparison study of CT findings in 14 pediatric patients compared with 47 adults, all with RT-PCR–confirmed COVID-19 infections, found that the pediatric patients had a significantly lower rate of positive CT findings, lower number of pulmonary lobes involved, and lower overall semiquantitative lung score (30).
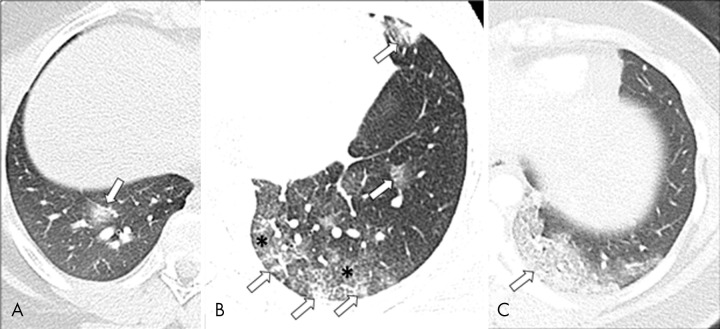
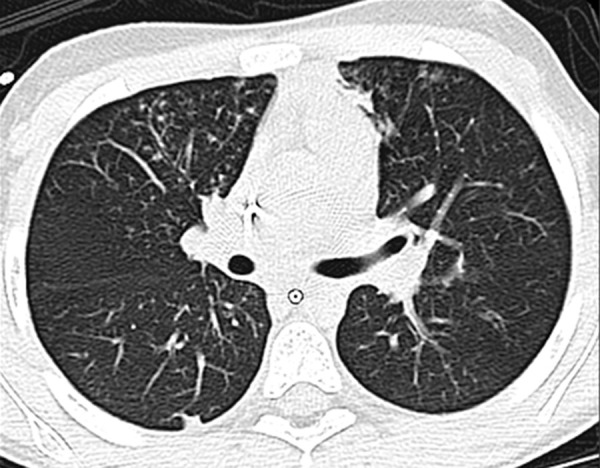
In pediatric patients with abnormalities found on CT, the most common findings are bilateral peripheral and/or subpleural ground-glass and/or consolidative opacities often in the lower lobes of the lungs (Fig 5) (30,42–45). The “halo” sign, which describes a focal consolidation with a rim of surrounding ground-glass opacity, has been reported in up to 50% (10 of 20) of cases and can help narrow the differential diagnosis when present (45). On the basis of the experience of this expert panel, three phases of evolution have been observed in pediatric COVID-19 cases demonstrating the “halo” sign: the “halo” sign is generally observed early in the disease course (early phase) and progresses to ground-glass (progressive phase) and eventually develops into consolidative opacities (developed phase) (Fig 6). Peribronchial thickening and inflammation along the bronchovascular bundle are observed more frequently in the pediatric population compared with adults (30). Fine mesh reticulations and “crazy paving” sign have also been reported, although with less frequency across the literature (45,46). Pleural effusion and lymphadenopathy are rare (30,45).
Figure 5:

A 21-month-old female with Hurler disease after bone marrow transplant and a positive COVID-19 RT-PCR test who presented with fever and respiratory distress. The axial lung window CT image shows bilateral peripheral and subpleural ground-glass opacities, which are typical CT findings in pediatric COVID-19.
Figure 6:
Three different phases (early, progressive, and developed) of COVID-19 pneumonia in three different pediatric patients. A, Early phase of pediatric COVID-19 pneumonia in a 14-year-old female with Hodgkin lymphoma and a positive COVID-19 RT-PCR test who presented with fever and cough. The axial lung window CT image shows a rounded ground-glass opacity (arrow) with a subtle area of central consolidation in keeping with the “halo” sign that is often seen in the early phase of pediatric COVID-19 pneumonia. B, Progressive phase of pediatric COVID-19 pneumonia in a 15-year-old female with traveling history in an endemic area in Europe and a positive COVID-19 RT-PCR test who presented with increasing cough and shortness of breath. The axial lung window CT image demonstrates rounded ground-glass opacities (arrows) with a subtle area of central consolidation. Between these areas, ground-glass opacities (*) start to fill the lung parenchyma. C, Developed phase of pediatric COVID-19 pneumonia in a 16-year-old female with a positive COVID-19 RT-PCR test who presented with severe shortness of breath. The axial lung window CT image shows predominantly confluent consolidation (arrow) in the posterior left lower lobe.
Data regarding chest CT findings of subacute COVID-19 infection in pediatric patients are limited. In one study with six pediatric patients who underwent follow-up CT within 0.5–2 weeks of presentation, two (33.3%) patients demonstrated complete resolution of pneumonia, three (50%) patients demonstrated partial resolution of consolidation, and three (50%) patients demonstrated a residual fibrous strip (45).
Current Recommendations for Chest CT in Pediatric Patients with Suspected or Known COVID-19
Although the chest CT findings of COVID-19 in the pediatric population are not pathognomonic, a bilateral peripheral subpleural lower lobe predominant pattern of ground-glass opacities is suggestive of the diagnosis in the appropriate clinical setting. However, RT-PCR test is considered to be the standard of reference for the diagnosis of COVID-19 pneumonia as it has been shown to have comparable (high COVID-19 prevalence areas) to superior sensitivity (low COVID-19 prevalence areas) and overall better specificity compared with chest CT (47). Thus, the American College of Radiology currently recommends against using CT as a first line screening test to diagnose COVID-19 and states that chest CT should be reserved for symptomatic hospitalized patients with specific clinical indications (48).
Chest CT is not recommended as the initial diagnostic test in pediatric patients suspected of having COVID-19. However, it may be considered to answer a specific clinical question in the acute setting (eg, to exclude a pulmonary embolism in a patient with an elevated d-dimer level). In addition, chest CT may be considered for pediatric COVID-19 patients with a worsening clinical course and/or who are not responding appropriately to supportive therapy. Finally, follow-up chest CT may be helpful to assess for development and/or evolution of fibrotic lung disease in patients with persistent alterations in pulmonary function tests following resolution of the acute infection. For all pediatric patients in whom chest CT is being entertained, additional factors including contamination of the CT scanner room (which may require subsequent room down time for air exchange and cleaning) and radiation dose are important to keep in mind.
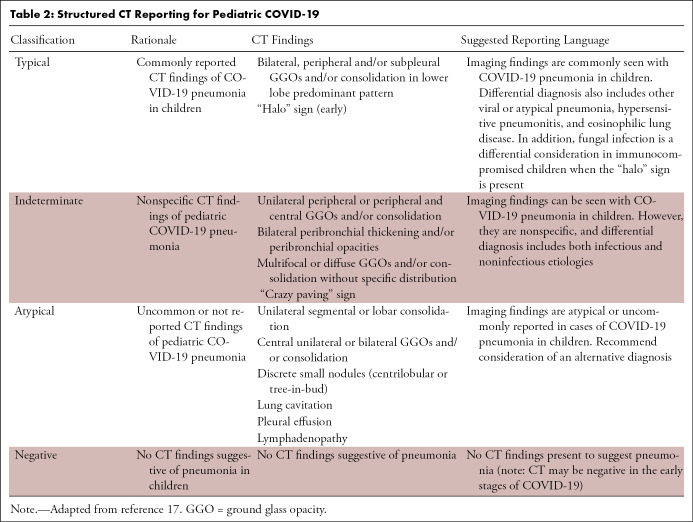
Structured CT Reporting Recommendations for Pediatric Patients with Suspected or Known COVID-19
The recommended structured reporting for pediatric chest CT evaluation in cases of suspected COVID-19 pneumonia is divided into the same four categories described in the chest radiography section of this article (ie, typical, indeterminate, atypical, and negative) and adapted from the structured CT reporting for adult COVID-19 patients (Figs 5–10) (17). CT findings for each category in this group are based on imaging patterns observed in pediatric studies across the literature as well as the experience of the international pediatric thoracic radiologists involved in this consensus statement. The summary of the imaging findings and suggested structured CT reporting for each category are shown in Table 2.
Figure 10:

A 16-year-old female who presented with fever and cough. The axial lung window CT image shows a peripherally located lung lesion with cavitation in the right lower lobe, which are atypical CT findings for pediatric COVID-19 pneumonia. This patient’s CT findings are due to a Staphylococcus aureus infection.
Table 2:
Structured CT Reporting for Pediatric COVID-19
Figure 7:

A 16-year-old female with a positive COVID-19 RT-PCR test who presented with shortness of breath. The axial lung window CT image shows ground-glass opacity with a small component of consolidation in the posterior left lower lobe, which are indeterminate CT findings of pediatric COVID-19 pneumonia.
Figure 8:

A 16-year-old female who presented with fever, cough, and chest pain. The axial lung window CT image shows bilateral central consolidation and ground-glass opacities, which are atypical CT findings of pediatric COVID-19 pneumonia. This patient’s CT findings are due to biopsy-proven varicella pneumonia.
Figure 9:
An 8-year-old girl who presented with fever and worsening cough. The axial lung window CT image shows bilateral discrete small nodules in the tree-in-bud pattern in the right middle lobe and lingula, which are atypical CT findings for pediatric COVID-19 pneumonia. This patient’s CT findings are due to a Mycobacterium infection.
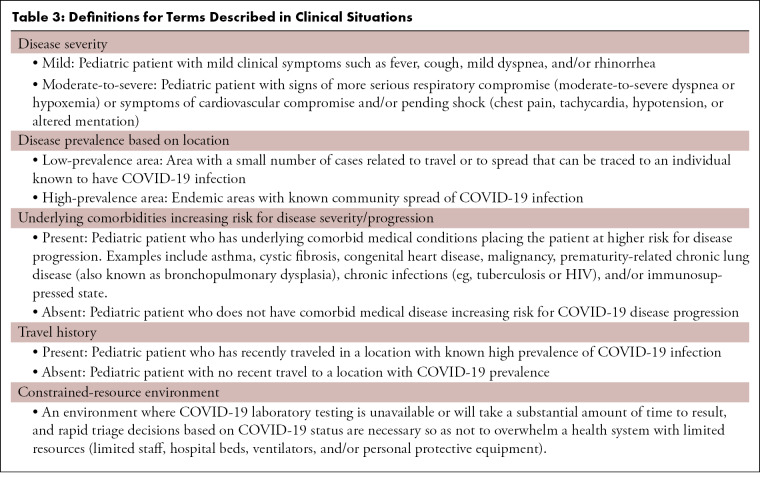
Imaging Recommendations Based on Clinical Indications
Imaging recommendations are described for pediatric patients in three distinct clinical situations at the time of initial presentation, similar to the recent Fleischner Society consensus statement for adult patients (49) (Table 3). These situations include pediatric patients presenting with mild clinical features of COVID-19, with moderate-to-severe clinical features of COVID-19 in a without resource–constrained environment, and with moderate-to-severe clinical features of COVID-19 in a resource-constrained environment. Additional recommendations are described for situations involving sequential studies and post-recovery follow-up imaging.
Table 3:
Definitions for Terms Described in Clinical Situations
There are potential risks of imaging that include a potentially nondiagnostic study, radiation exposure, COVID-19 exposure to radiology staff, and increased imaging equipment/room turnaround time for appropriate cleaning and air turnover. These risks must be weighed against the potential benefits of imaging, such as informed decision making regarding patient triage and isolation, establishing baseline imaging, and identification of an alternative diagnosis or comorbid conditions when deciding to pursue chest radiography or chest CT in the pediatric population. Additional factors, including the prevalence of COVID-19 in the local population, travel history to a high COVID-19 prevalence area, and the presence of comorbid medical conditions that could increase the risk of disease progression/severity (such as asthma, cystic fibrosis, congenital heart disease, chronic lung disease of prematurity [also known as bronchopulmonary dysplasia], malignancy, chronic infection [eg, tuberculosis or HIV], and/or an immunosuppressed state as may be observed in pediatric patients with bone marrow or other visceral transplants) should also play a role in imaging decisions.
Situation 1: Mild Clinical Features of COVID-19 in Pediatric Patients
Pediatric patients in this group often present in the outpatient setting with mild clinical symptoms such as fever, cough, and/or rhinorrhea. In this situation, COVID-19 testing with RT-PCR should be the first step in screening evaluation. If COVID-19 testing is not readily available, these pediatric patients can be stratified into a suspected COVID-19 positive group in endemic areas with known community spread and suspected negative group in locations with low disease prevalence. Given the overall milder clinical course of COVID-19 in the pediatric population and the increased radiation sensitivity of pediatric patients, imaging is not recommended for the majority of patients in the mild group at the time of presentation regardless of RT-PCR results. However, for patients with a positive COVID-19 status (either by laboratory diagnosis or presumed positive status based on local disease prevalence) who have underlying comorbidities (ie, asthma, cystic fibrosis, congenital heart disease, malignancy, bronchopulmonary dysplasia, chronic infections [eg, tuberculosis or HIV], and/or an immunosuppressed state) placing them at risk for disease progression, chest imaging is recommended to serve as a baseline as well as to evaluate for alternative diagnoses possibly related to a comorbid condition (eg, pulmonary edema in congenital heart disease). Even in pediatric patients with an elevated risk for progression, chest CT is not recommended at the time of presentation for diagnosis of COVID-19 but may be considered in cases of clinical progression, inadequate clinical improvement, or when an alternative diagnosis (such as a concern for pulmonary embolism) necessitates further evaluation. Regardless of underlying clinical risk factors or COVID-19 disease status, worsening respiratory function in a pediatric patient initially considered to have mild clinical features is an indication for further evaluation with chest imaging.
Situation 2: Moderate-to-Severe Clinical Features of COVID-19 in Pediatric Patients in a Without Resource–Constrained Environment
Pediatric patients with suspected COVID-19 in this group present with clinical signs of a more serious respiratory compromise, including moderate-to-severe dyspnea or hypoxemia, or symptoms such as chest pain, tachycardia, hypotension, or altered mentation that may indicate cardiovascular compromise and/or pending shock. COVID-19 testing with RT-PCR is the initial screening test recommended for this group without resource constraints. If testing or timely results are not readily available, these patients can be further classified into presumed positive or presumed negative COVID-19 status based on local disease prevalence. Regardless of the COVID-19 status, chest radiography is recommended for initial evaluation of the pediatric patient presenting with moderate-to-severe clinical features to establish an imaging baseline and evaluate for an alternative diagnosis. Chest CT may also be considered in this group if the outcome will impact clinical decision making (ie, imaging findings would affect how closely a patient is clinically followed and possibly followed with imaging to assess for change or potential complication); however, it should not serve as the screening examination to assess COVID-19 status. One important note for the moderate-to-severe group is that in pediatric patients initially categorized into the negative COVID-19 group (either by RT-PCR test results or by low community prevalence) who are found to have imaging manifestations commonly seen in COVID-19, repeat laboratory COVID-19 testing (or initial testing if grouped based on community prevalence) is recommended.
Situation 3: Moderate-to-Severe Clinical Features of COVID-19 in Pediatric Patients in a Resource-Constrained Environment
Situation 3 describes a plan for COVID-19 screening in an environment where laboratory testing is unavailable or a lengthy turnaround time for results would preclude rapid triage decisions, potentially overwhelming a health system with limited resources (limited hospital beds, ventilators, personal protective equipment, etc). In this specific situation, imaging may be used as an initial step to evaluate for findings suggestive of COVID-19 (presumed positive) versus findings suggestive of an alternative diagnosis. Given the limited sensitivity of chest radiography, chest CT, specifically tailored to a low-dose technique for pediatric patients closely following the as-low-as-reasonably-achievable (ALARA) principle, may be considered for the assessment of this group either initially or following unrevealing chest radiography results (50,51). If no alternative diagnosis is identified and imaging findings are nonspecific but extensive enough to be worrisome, the hospital will then have to make triage decisions related to concerns for COVID-19 based on overall clinical picture, local disease prevalence, and known resource limitations.
Sequential Imaging in Moderate-to-Severe Pediatric COVID-19
Sequential chest radiographic examinations are appropriate in pediatric COVID-19 patients on an as-clinically-needed basis to monitor response to supportive measures, assess clinical deterioration, or evaluate the positioning of life support devices. Similar to recommendations for the adult population, daily routine chest radiographic examinations are not indicated for clinically stable, intubated pediatric intensive care unit patients with COVID-19. Although there is less literature on the use of daily chest radiography in pediatric intensive care unit patients, one large study with over 1500 pediatric patients showed no significant difference in average pediatric intensive care unit length of stay, hospital length of stay, or days on ventilator support and absence of reported adverse outcomes between patients with a standing order for daily chest radiography versus patients with chest radiography ordered for a specific clinical indication (52).
A chest CT in this group may be considered, especially if not pursued at the time of initial presentation, in pediatric patients who are not responding appropriately to supportive care or demonstrate clinical deterioration. However, given the increased radiation dose, chest CT is only recommended if it would directly impact clinical decision making in pediatric patients given their increased sensitivity to radiation compared with adults.
Post-Recovery Follow-up Chest Imaging in Pediatric COVID-19 Patients
The decision to pursue posttreatment follow-up chest imaging should be based both on the severity of disease (mild vs moderate-to-severe) and the presence (or absence) of clinical symptoms (ie, dyspnea, decreased exercise tolerance, etc) at the time of follow-up. As long-term data are not yet available for pediatric COVID-19 patients, recommendations currently presented in this article are based on the consensus of expert opinion as well as on long-term follow-up experience with severe acute respiratory syndrome and Middle East respiratory syndrome (8,11).
For asymptomatic pediatric patients who had a mild disease course, no long-term imaging follow-up is recommended. However, even pediatric patients with a mild disease course may develop long-standing pulmonary injury and thus a follow-up standard two-view (posteroanterior and lateral) chest radiography should be considered in symptomatic patients with prior mild COVID-19 infection. Follow-up imaging in this group can evaluate for evidence of pulmonary scarring/fibrosis and also evaluate for other potentially treatable causes for the patients’ symptoms.
In pediatric patients with a moderate-to-severe COVID-19 infection, a follow-up standard two-view chest radiography is recommended for symptomatic pediatric patients for the same reasons as described earlier for symptomatic mild cases and may be considered in asymptomatic pediatric patients depending on the level of clinical concern for long-term lung injury. Long-term follow-up studies of both patients with severe acute respiratory syndrome and patients with Middle East respiratory syndrome have demonstrated chronic pulmonary parenchymal abnormalities, including air trapping and pulmonary fibrosis, in up to approximately 33.3% (one of three) of patients (8,11). Therefore, a follow-up standard two-view chest radiography, even in asymptomatic pediatric patients, may be appropriate for this group.
Conclusion
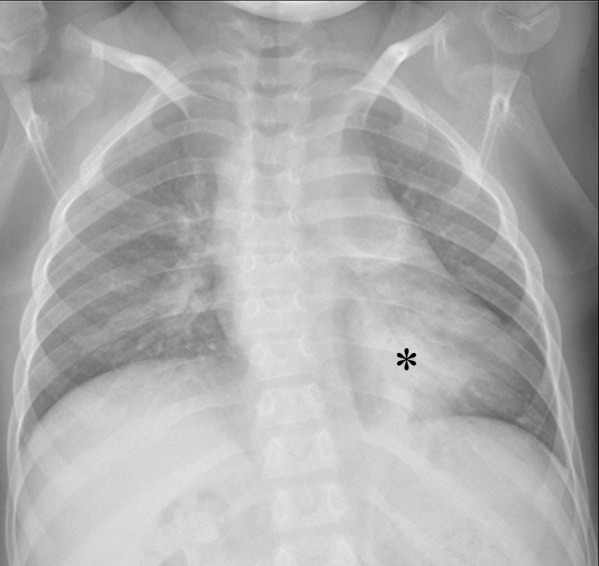
In conclusion, the COVID-19 pandemic is currently a rapidly evolving situation and has created an environment of uncertainty. The purpose of this consensus statement is to help address COVID-19–related uncertainty in pediatric patients for practicing radiologists and referring clinicians by providing up-to-date knowledge about the imaging manifestations of COVID-19 pneumonia in children, proposing a template for structured radiologic reporting in this patient population and offering practical guidance regarding utilization of chest imaging in the pediatric patient population (Table 4).
Table 4:
Summary of Imaging Recommendations
As knowledge about the presentation and evolution of COVID-19 pneumonia in pediatric patients continues to grow, the information and recommendations provided by this document may undergo additional refinement. Practice patterns will vary across institutions, and thus, this consensus statement is meant to offer guidance; however, best results will likely be achieved through candid discussions between individual radiology groups and their respective referring providers.
Disclosures of Conflicts of Interest: A.M.F. disclosed no relevant relationships. G.S.P. disclosed no relevant relationships. W.C.C. disclosed no relevant relationships. P.D. disclosed no relevant relationships. K.M.D. disclosed no relevant relationships. P.G.P. disclosed no relevant relationships. T.K. disclosed no relevant relationships. A.J.W. disclosed no relevant relationships. E.Y.L. Activities related to the present article: disclosed no relevant relationships. Activities not related to the present article: Guerbet supported author’s traveling and accommodation to 2019 AOSPR meeting in Seoul, Korea for luncheon lecture of contrast agent for pediatric imaging study; author paid by Michigan Professional Insurance Exchange for medical legal consultation work ($3529.17); author receives royalties for editorial work for textbook publication from Wolters Kluwer Health (book royalty = $1008.55) and Elsevier (book royalty = $1000). Other relationships: disclosed no relevant relationships.
Abbreviations:
- COVID-19
- coronavirus disease 2019
- RT-PCR
- reverse-transcription polymerase chain reaction
References
- 1.Su S, Wong G, Shi W, et al. Epidemiology, Genetic Recombination, and Pathogenesis of Coronaviruses. Trends Microbiol 2016;24(6):490–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sun P, Lu X, Xu C, Sun W, Pan B. Understanding of COVID-19 based on current evidence. J Med Virol 2020 Feb 25 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . The Coronavirus Disease 2019 (COVID-19) Situation Report-51. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10. Accessed March 22, 2020.
- 4.World Health Organization . Coronavirus disease 2019 (COVID-19) Situation Report-84. https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Published 2020. Accessed April 13, 2020.
- 5.Dong Y, Mo X, Hu Y, et al. Epidemiology of COVID-19 Among Children in China. Pediatrics 2020 Mar 16 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 6.Zimmermann P, Curtis N. Coronavirus Infections in Children Including COVID-19: An Overview of the Epidemiology, Clinical Features, Diagnosis, Treatment and Prevention Options in Children. Pediatr Infect Dis J 2020;39(5):355–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hon KLE, Leung CW, Cheng WTF, et al. Clinical presentations and outcome of severe acute respiratory syndrome in children. Lancet 2003;361(9370):1701–1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chu WCW, Li AM, Ng AWH, et al. Thin-section CT 12 months after the diagnosis of severe acute respiratory syndrome in pediatric patients. AJR Am J Roentgenol 2006;186(6):1707–1714. [DOI] [PubMed] [Google Scholar]
- 9.Das KM, Lee EY, Enani MA, et al. CT correlation with outcomes in 15 patients with acute Middle East respiratory syndrome coronavirus. AJR Am J Roentgenol 2015;204(4):736–742. [DOI] [PubMed] [Google Scholar]
- 10.Das KM, Lee EY, Al Jawder SE, et al. Acute middle east respiratory syndrome coronavirus: Temporal lung changes observed on the chest radiographs of 55 patients. AJR Am J Roentgenol 2015;205(3):W267–W274. [DOI] [PubMed] [Google Scholar]
- 11.Das KM, Lee EY, Singh R, et al. Follow-up chest radiographic findings in patients with MERS-CoV after recovery. Indian J Radiol Imaging 2017;27(3):342–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Das KM, Lee EY. Middle East Respiratory Syndrome Coronavirus in Children. Indian Pediatr 2016;53(8):752. [PubMed] [Google Scholar]
- 13.Lee EY, McAdam AJ, Chaudry G, Fishman MP, Zurakowski D, Boiselle PM. Swine-origin influenza a (H1N1) viral infection in children: initial chest radiographic findings. Radiology 2010;254(3):934–941. [DOI] [PubMed] [Google Scholar]
- 14.Foust AM, Winant AJ, Chu WC, Das KM, Phillips GS, Lee EY. Pediatric SARS, H1N1, MERS, EVALI, and Now Coronavirus 2019 (COVID-19) Pneumonia: What Radiologists Need to Know. AJR Am J Roentgenol 2020 (in press). [DOI] [PubMed] [Google Scholar]
- 15.Buckley BW, Daly L, Allen GN, Ridge CA. Recall of structured radiology reports is significantly superior to that of unstructured reports. Br J Radiol 2018;91(1083):20170670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wildman-Tobriner B, Allen BC, Davis JT, et al. Structured Reporting of Magnetic Resonance Enterography for Pediatric Crohn’s Disease: Effect on Key Feature Reporting and Subjective Assessment of Disease by Referring Physicians. Curr Probl Diagn Radiol 2017;46(2):110–114. [DOI] [PubMed] [Google Scholar]
- 17.Simpson S, Kay FU, Abbara S, et al. Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. Radiol Cardiothorac Imaging 2020;2(2):e200152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jeong YJ, Kim KI, Seo IJ, et al. Eosinophilic lung diseases: a clinical, radiologic, and pathologic overview. RadioGraphics 2007;27(3):617–637; discussion 637–639. [DOI] [PubMed] [Google Scholar]
- 19.Cho YJ, Han MS, Kim WS, et al. Correlation between chest radiographic findings and clinical features in hospitalized children with Mycoplasma pneumoniae pneumonia. PLoS One 2019;14(8):e0219463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fan LL. Hypersensitivity pneumonitis in children. Curr Opin Pediatr 2002;14(3):323–326. [DOI] [PubMed] [Google Scholar]
- 21.John SD, Ramanathan J, Swischuk LE. Spectrum of clinical and radiographic findings in pediatric mycoplasma pneumonia. RadioGraphics 2001;21(1):121–131. [DOI] [PubMed] [Google Scholar]
- 22.Liu CY, Wang JD, Yu JT, et al. Influenza B virus-associated pneumonia in pediatric patients: clinical features, laboratory data, and chest X-ray findings. Pediatr Neonatol 2014;55(1):58–64. [DOI] [PubMed] [Google Scholar]
- 23.Giovannini-Chami L, Hadchouel A, Nathan N, et al. Idiopathic eosinophilic pneumonia in children: the French experience. Orphanet J Rare Dis 2014;9:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Artunduaga M, Rao D, Friedman J, et al. Pediatric Chest Radiographic and CT Findings of Electronic Cigarette or Vaping Product Use-associated Lung Injury (EVALI). Radiology 2020;295(2):430–438. [DOI] [PubMed] [Google Scholar]
- 25.Yoon SH, Lee KH, Kim JY, et al. Chest Radiographic and CT Findings of the 2019 Novel Coronavirus Disease (COVID-19): Analysis of Nine Patients Treated in Korea. Korean J Radiol 2020;21(4):494–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Choi H, Qi X, Yoon SH, et al. Extension of Coronavirus Disease 2019 (COVID-19) on Chest CT and Implications for Chest Radiograph Interpretation. Radiol Cardiothorac Imaging 2020;2(2):e200107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ng MY, Lee EY, Yang J, et al. Imaging Profile of the COVID-19 Infection: Radiologic Findings and Literature Review. Radiol Cardiothorac Imaging 2020;2(1):e200034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cai J, Xu J, Lin D, et al. A Case Series of children with 2019 novel coronavirus infection: clinical and epidemiological features. Clin Infect Dis 2020 Feb 28 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American College of Radiology . ACR Appropriateness Criteria: Pneumonia in the Immunocompetent Child. https://acsearch.acr.org/docs/3102387/Narrative/. Published 2019. Accessed April 18, 2020.
- 30.Chen A, Huang J, Liao Y, et al. Differences in Clinical and Imaging Presentation of Pediatric Patients with COVID-19 in Comparison with Adults. Radiol Cardiothorac Imaging 2020;2(2):e200117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang Y, Dong C, Hu Y, et al. Temporal Changes of CT Findings in 90 Patients with COVID-19 Pneumonia: A Longitudinal Study. Radiology 2020 Mar 19:200843 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lu X, Zhang L, Du H, et al. SARS-CoV-2 Infection in Children. N Engl J Med 2020;382(17):1663–1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pan Y, Guan H, Zhou S, et al. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol 2020 Feb 13 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xu X, Yu C, Qu J, et al. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging 2020;47(5):1275–1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhou S, Wang Y, Zhu T, Xia L. CT Features of Coronavirus Disease 2019 (COVID-19) Pneumonia in 62 Patients in Wuhan, China. AJR Am J Roentgenol 2020 Mar 5:1–8 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 36.Han R, Huang L, Jiang H, Dong J, Peng H, Zhang D. Early Clinical and CT Manifestations of Coronavirus Disease 2019 (COVID-19) Pneumonia. AJR Am J Roentgenol 2020 Mar 17:1–6 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 37.Zhao W, Zhong Z, Xie X, Yu Q, Liu J. Relation Between Chest CT Findings and Clinical Conditions of Coronavirus Disease (COVID-19) Pneumonia: A Multicenter Study. AJR Am J Roentgenol 2020;214(5):1072–1077. [DOI] [PubMed] [Google Scholar]
- 38.Bernheim A, Mei X, Huang M, et al. Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. Radiology 2020 Feb 20:200463 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chung M, Bernheim A, Mei X, et al. CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV). Radiology 2020;295(1):202–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bai HX, Hsieh B, Xiong Z, et al. Performance of radiologists in differentiating COVID-19 from viral pneumonia on chest CT. Radiology 2020 Mar 10:200823 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen Z, Fan H, Cai J, et al. High-resolution computed tomography manifestations of COVID-19 infections in patients of different ages. Eur J Radiol 2020;126:108972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang D, Ju XL, Xie F, et al. Clinical analysis of 31 cases of 2019 novel coronavirus infection in children from six provinces (autonomous region) of northern China [in Chinese]. Zhonghua Er Ke Za Zhi 2020;58(4):E011. [DOI] [PubMed] [Google Scholar]
- 43.Sun D, Li H, Lu XX, et al. Clinical features of severe pediatric patients with coronavirus disease 2019 in Wuhan: a single center’s observational study. World J Pediatr 2020 Mar 19 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zheng F, Liao C, Fan QH, et al. Clinical Characteristics of Children with Coronavirus Disease 2019 in Hubei, China. Curr Med Sci 2020;40(2):275–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xia W, Shao J, Guo Y, Peng X, Li Z, Hu D. Clinical and CT features in pediatric patients with COVID-19 infection: Different points from adults. Pediatr Pulmonol 2020;55(5):1169–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhou Y, Yang GD, Feng K, et al. Clinical features and chest CT findings of coronavirus disease 2019 in infants and young children [in Chinese]. Zhongguo Dang Dai Er Ke Za Zhi 2020;22(3):215–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kim H, Hong H, Yoon SH. Diagnostic Performance of CT and Reverse Transcriptase-Polymerase Chain Reaction for Coronavirus Disease 2019: A Meta-Analysis. Radiology 2020 Apr 17:201343 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.American College of Radiology . ACR Recommendations for the use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection. https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection. Published 2020. Accessed April 3, 2020.
- 49.Rubin GD, Ryerson CJ, Haramati LB, et al. The Role of Chest Imaging in Patient Management during the COVID-19 Pandemic: A Multinational Consensus Statement from the Fleischner Society. Radiology 2020 Apr 7:201365 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ngo AV, Winant AJ, Lee EY, Phillips GS. Strategies for reducing radiation dose in CT for pediatric patients: how we do it. Semin Roentgenol 2018;53(2):124–131. [DOI] [PubMed] [Google Scholar]
- 51.Sodhi KS, Krishna S, Saxena AK, Sinha A, Khandelwal N, Lee EY. Clinical application of ‘Justification’ and ‘Optimization’ principle of ALARA in pediatric CT imaging: “How many children can be protected from unnecessary radiation?”. Eur J Radiol 2015;84(9):1752–1757. [DOI] [PubMed] [Google Scholar]
- 52.Price MB, Grant MJ, Welkie K. Financial impact of elimination of routine chest radiographs in a pediatric intensive care unit. Crit Care Med 1999;27(8):1588–1593. [DOI] [PubMed] [Google Scholar]