Abstract
Background and aim of the work: World Health Organization states that is possible evaluating projects’ qualities via Health Impact Assessment (HIA) but there are not specific HIA tools on hospital buildings assessment. Researchers show significant relationships between built environment and health. The research purpose is investigating how existing tools for healthcare building assessment are encouraging the development of possible hospital HIA evaluation. Methods: Based on previous works, 13 assessment tools have been included and a comparison of the criteria has been conducted to understand which the most prevalent topics are. The tools have been analyzed through literature, technical manuals and official websites. The authors identified 12 thematic categories where criteria from different tools have been clustered and discussed. Results: The most prevalent criteria are related to Indoor Environmental Quality (IEQ) (20%). In the oldest tools the evaluation was mainly on technical features while in recent instruments several indicators are related to Architectural features and innovation (48%), Education (23%) and Food (11%). Conclusions: There is growing interest in tools capable of addressing healthy hospitals encouraging IEQ, physical activity and healthy food provision related to occupants’ health outcomes. This preliminary study set the basis for further development on hospital facility HIA tools. (www.actabiomedica.it)
Keywords: evidence based design, assessment tool, hospital, built environment, quality, public health, healthcare facility, health impact assessment
Background and aim of the work
Public health and architecture
Recent trends such as globalization, digitalization and urbanization, combined with an ageing population and population growth, result in new challenges for public health and healthcare settings (1, 2). To address those complex issues a social multidisciplinary approach has to be considered and various professional figures have to collaborate in analysis, advocacy and action. In this paper the authors argue that decision makers, healthcare managers and public health workforce can benefit from the support of architects, designers and urban planners when dealing with complex decisions about healthcare facilities and built environment in terms of health promotion possibilities both at the urban and at the building scale (3, 4). In particular, contemporary healthcare systems are facing the challenge of delivering high level services in complex economic and social environments. Hospital facilities reflect this complexity and, as building type, they host diverse and multiple daily users, try to integrate advanced technologies and systems and have a public role as health venue and promoters, constantly transforming during time (5-7).
The Italian context and built environment criticalities
In the Italian context one hospital over three has been built before 1970 demonstrating the obsolescence of this important asset (8). This figure is reinforced by data from Piedmont region where 42% of the healthcare estate is not adequate to the contemporary organizational models and technological innovation due to their construction period or the need for consistent extraordinary maintenance (9). Moreover, recent declaration from the Italian Minister of Health confirms the needs of a consistent investment plan of about Euro 32 billion for the improvement of the overall quality and safety of hospital architectural assets (10). Although this consistent amount of money is requested for the economic sustainability of the system, strategic tools are needed to target the most important aspects to design or refurbish high quality hospital, eventually avoiding the repetition of obsolete and inefficient models.
Hospital built environment and Health Impact Assessment
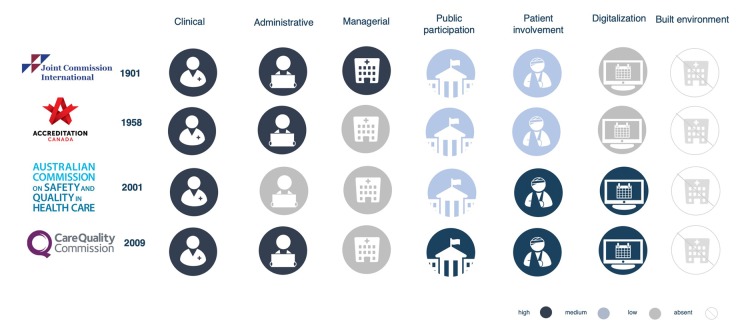
Researchers demonstrated that physical healthcare environment is an important factor in the overall health care performance outcomes. Architecture and physical space are considered an important component that contributes to the creation of a high-quality health service to promote health and well-being (11-13). Indeed, the Donabedian’s quality assurance model states that the quality of healthcare is related to three domains: process, outcome and, lastly, structure, which is defined as the “physical and organizational characteristics where health care occurs” (14). In western countries well established systems (i.e. Joint Commission International) are important in the process of quality measurement and improvement with criteria and indicators related to clinical, organizational and managerial fields. Nevertheless, they rarely mention the built environment and no indicators are provided to evaluate the physical settings where healthcare is delivered (Figure 1).
Figure 1.
Comparison between the most common organizational quality assessment tools
Research gap and problem statement
Although the concept of design quality is very difficult to define (15), several studies at the edge of architecture, environmental psychology, health management and service design fields, demonstrated the impact of built environment on the final building users (16-20). Moreover, the World Health Organization (WHO) states that is possible to evaluate the quality of a project via Health Impact Assessment (HIA) which is a means of assessing the health impacts of policies, plans and projects in diverse economic sectors using qualitative, quantitative and participatory techniques (21). To the best of our knowledge, no HIA tools are available for the assessment of hospital design qualities. However, Ulrich’s Evidence Based Design (EBD) studies demonstrated the importance of green views and several other design elements on different health-related outcomes and organizational domains such as patient stay reduction, fall reduction and staff satisfaction (22-25). Furthermore, in the last 20 years, within the real estate sector of corporate office buildings a similar approach started to be diffused mainly in the field of environmental sustainability with the development of some evaluation instruments, also applicable to hospital settings (26-28). Since in Italy hospital design regulations are generic, prescriptive and obsolete there is an urgent need to study and develop specific assessment tools.
Purpose and research questions
Therefore, the general research purpose is to investigate how the existing tools for hospital built environment assessment can encourage the development of possible HIA tools. Specifically, two research questions have been framed in order to clarify the boundaries of the study:
If hospital’s physical qualities are measurable through assessment tools, on which criteria those evaluations are based, which topics are the most prevalent and, therefore, important in the evaluation?
Within the available tools, are there emerging topics that were not present in the past and, therefore, can define a possible trend for the future?
Methods
In order to collect most of the information about the topic a literature review has been conducted and different tolls have been extracted and differently analyzed. With the objective of highlighting blank or weakly covered areas for grounding incremental studies in the field, the search has been conducted with sets of keywords derived from preliminary search and relevant references (29-32) (Table 1). Based on previous works by the authors (24, 33) 13 tools have been included.
Table 1.
Synthesis of the literature search and review conducted, upon which the analysis presented in the paper is based; extensive description and PRISMA flow diagram is provided in previous works by the authors (23, 32)
| Date of search | May and April 2018 |
| Keywords | Quality
|
| Repositories |
|
| Papers collected | 2228 |
| Inclusion criteria | Physical qualities; Assessment or evaluation methodology; Published after 2010; English language |
| Papers included | 172 |
| Tools founded | 44 |
| Inclusion criteria | Post Occupancy Evaluation; Applicable to hospital building |
| Tools included | 13 |
| Full methodology available in: | Brambilla et al, 2019 (24); Brambilla & Capolongo, 2019 (33) |
A comparison of the criteria has been conducted in order to understand which the most prevalent topics are. Each tool has been analyzed based on the criteria level of detail and in line with previous studies on the topic (28, 33-37). All the included tools have a hierarchic structure of macro areas, criteria and indicators. The analysis has been conducted exclusively at the criteria level and the importance of each criterion has been considered based on the total number of indicators related to that specific criterion. The tools have been analyzed through the literature, technical manuals and official websites by the authors. During the tools screening the authors identified a series of thematic areas in which criteria from different tools can be related and clustered them in 12 categories. The prevalence of a category (p) within each tool has been calculated according to the following formula:
p = n/T×100
where n is the number of indicators related to a specific criterion and T is the total number of indicators of the tool. The prevalence has been calculated for each single tool (p1; p2; …; p13) and for the overall set of criteria collected (P).
The included tools, with the corresponding number of indicators (n) are:
BREEAM - Building Research Establishment Environmental Assessment Method (n=193)
LEED - Leadership in Energy and Environmental Design (n=49)
CASBEE - Comprehensive Assessment System for Building Environment Efficiency (n=20)
GS - Green Star (n=30)
ASPECT - A Staff and Patient Environment Calibration Toolkit (n=46)
AEDET - Achieving Excellence Design Evaluation Toolkit (n=57)
GGH - Green Guide for Healthcare (n=57)
SUSTHEALTH - Sustainable High Quality Healthcare (n=37)
BUDSET - Birthing Unit Design Spatial Evaluation Tool 2.0 (n=92)
HBS - Healthcare Building Sustainability Assessment tool (n=52)
DQI - Design Quality Indicator (n=66)
WELL - Well Building Standard (n=117)
CHD-CHC - Community Health Center Facility Evaluation Tool (n=94)
Results
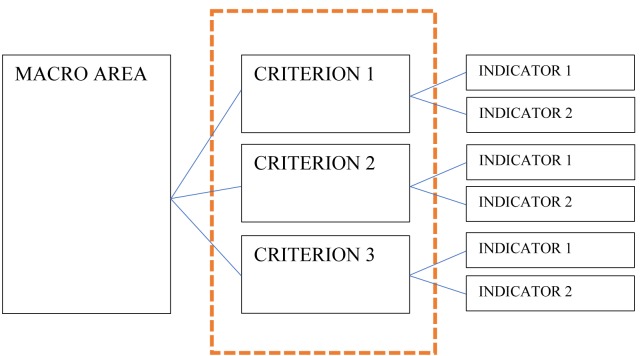
All the tools are based on a hierarchic structure, the framework is composed by fundamental and interconnected macro-areas (39) and each one is evaluated through a hierarchic set of criteria and indicators (Figure 2). The tools collected have up to 5 macro areas, between 6 and 24 criteria and between 21 and 193 indicators. Each indicator might have one or more item with different techniques of measurement, either qualitative or quantitative. Globally the total number of indicators is 910.
Figure 2.
Hierarchic framework of a generic assessment tool with highlighted the criteria level where the analysis has been conducted
Data analysis
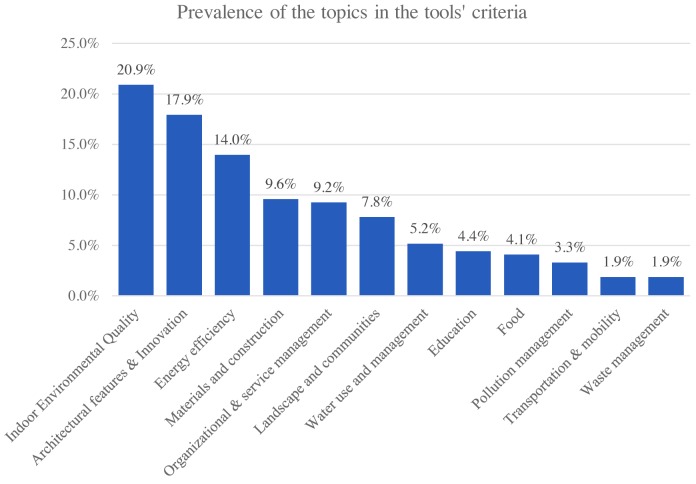
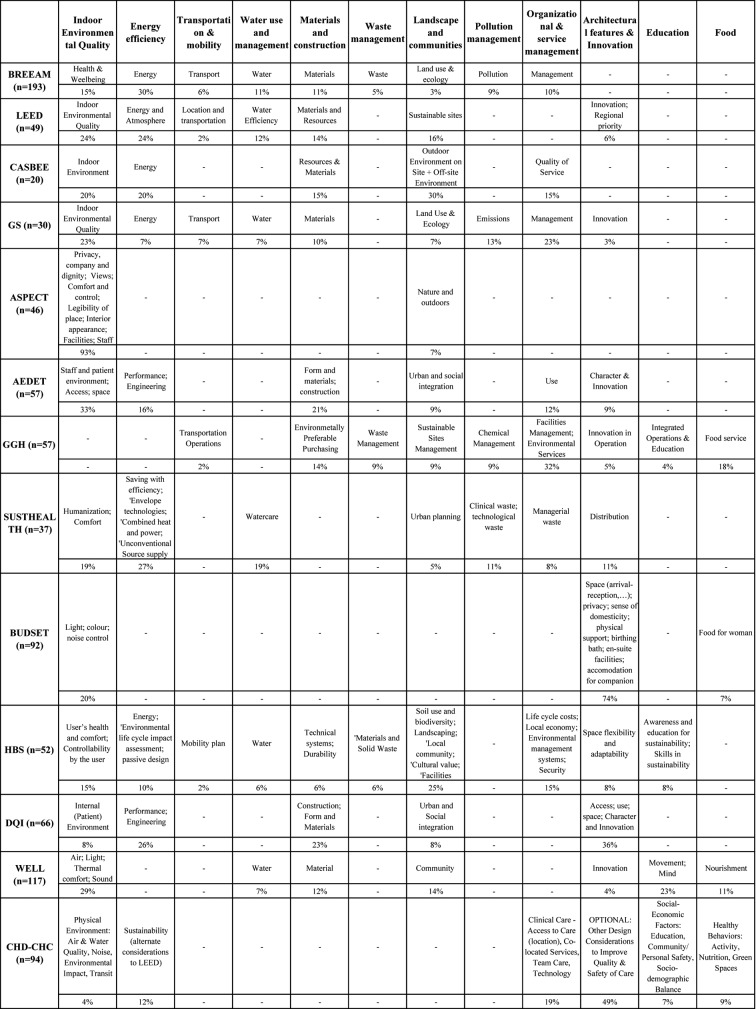
Among the total number of tools and criteria, 12 categories have been highlighted by the authors in order to be able to cluster a significant number of similar topics of measurement. The categories are hereafter listed and described from the most prevalent to the least (Table 3).
Indoor Environmental Quality (IEQ) is the most prevalent category among all the criteria and it collects 20,9% (n=190) of the total amount of indicators. IEQ performance of buildings affects lifecycle costs and energy consumption but also the wellbeing, health and productivity of building occupants (39). It includes the subtopics of health and wellbeing (BREEAM p=15%), humanization, comfort and in general the qualities of the indoor environment (LEED p=24%), including privacy, views, colours, air and sound (WELL p=29%). Researches in this direction shown the importance of qualitative issues for the hospital’s occupants, patients and staff (40, 41).
Architectural features and innovation category have a prevalence of 17,9% (n=163) and embeds several topics such as distribution, layout features, space flexibility and adaptability (HBS=8%), character and innovation (DQI=36%) and other design considerations able to improve overall safety and quality of care (CHD-CHC=49%). Indeed, within the evolution of hospital typology several strategies such as flexibility have been recognized as very effective in terms of medium and long term management by several authors as well as practitioners that are constantly experimenting new technological systems for improving the ability of a space to change function during time (42).
The third most prevalent category is Energy efficiency that contains 127 indicators (P=14%) with specific performance-based criteria such as envelope technologies, environmental life cycle, engineering systems, sustainability and energy measurements (SUSTHEALTH=27%). Hospital facilities are energy demanding systems and although several aspects are demanded to technical regulations and standards, the different tools provide clear and performance-based indicators to improve the overall energy management, reduce the cost and contribute to the contemporary environmental issues related to climate change.
Below a prevalence of 10% is possible to find the Materials and construction topics (P=9,6%; n=87), the Organizational and service management (P=9,2%; n=84), the Landscape and communities issues (P=7,8%; n=71) and the Water use and management (P=5,2%; n=47) categories.
The least prevalent criteria are Education (P=4,4%; n=40), Food (P=4,1%; n=37), Pollution management (P=3,3%; n=30), Transportation and mobility (P=1,9%; n=17) and, finally, Waste management (P=1,9%; n=17) (Figure 3).
Figure 3.
Prevalence of the different categories in the whole tools’ criteria
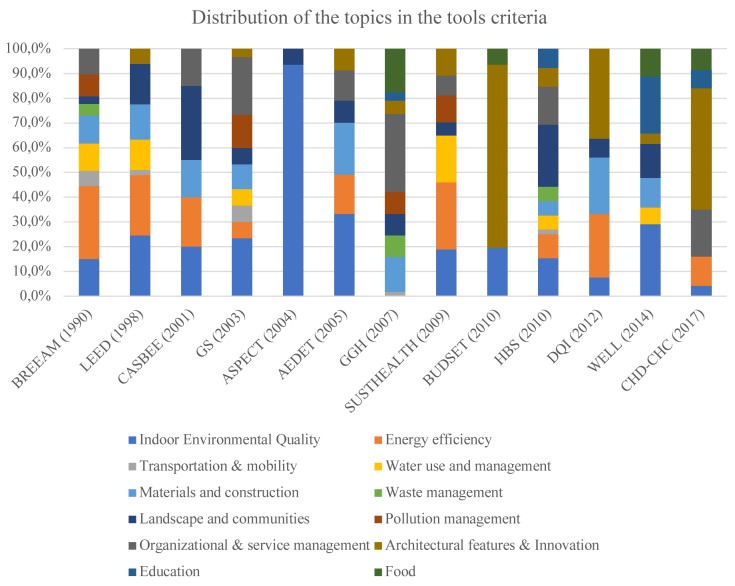
Evolution during time and innovative criteria
Most of the criteria highlighted are related to environmental sustainability categories such as Energy efficiency, Materials, etc. Nevertheless, looking at the included tools from a chronological point of view it is interesting to notice that an increasing attention in the assessment criteria is devoted to the categories of: Architectural features & innovation, Education and Food strategies.
Indeed, in the tools developed in the early 90s (i.e. BREEAM or LEED) only few criteria related to architectural features and innovation were present. On the contrary, in the most recent hospital built environment quality evaluation instruments, up to 48% of the indicators are related to Architectural features and innovation (i.e. CHD CHC) and up to 23% and 11% are respectively related to Education and Food (i.e. WELL). This evolution confirms what highlighted in previous works (33) and an overview of this pattern is provided in Figure 4.
Figure 4.
Distribution of the 12 categories in the 13 different tools during time
Discussion
Several categories have a direct or indirect impact on hospital performances, quality of the service and on occupant’s health. For example, in the Indoor Environmental Quality category, criteria like DQI’s “Internal patient environment” contains several indicators that allow a better patient or staff satisfaction i.e. layout legibility, wayfinding, provision of natural light, views and accesses to green areas (43, 44). Additionally, in the WELL’s “Movement” criteria, most of the indicators are related to the possibility of enhancing, through different layout and organizational strategies, the use of stairs for the buildings’ occupants or the provision of gym services in order to foster a culture of physical activities and health prevention in the workplaces (45, 46). Furthermore, the whole “Food” category embeds, through the different tools, several strategies to provide healthy diets with attention to the different intolerances and culture-related issues, not just with organizational strategies but also with the implementation of graphical signages, layout interventions and ad-hoc surveys (45, 47). Finally, even if the criteria related to sustainability might seem very technical, as defined by WHO and the Health Care Without Harm initiative, those strategies are capable of addressing healthy hospitals, healthy planet and healthy people in the view of climate change (48, 49).
Conclusions
Although most of the hospital service evaluation instruments do not consider the built environment, criteria from hospital facility assessment tools can be related to well defined categories and embeds several indicators of measurement that have a direct or indirect impact on hospital occupant’s health. Qualitative issues in the field of IEQ, sustainability, organizational qualities are evaluated and recently released tools includes specific issues from the architectural field, the education of the occupants and the services related to the provision of healthy food. Hospital built environment have an important role within the whole national health system and therefore the design of those facilities has to be based on the best available knowledge from solid research (43). Therefore, Public Health and Built Environment researchers have to collaborate in developing strategic tools and methods for the improvement of the physical qualities of the healthcare settings that can have important impacts on occupants’ health and wellbeing (50). Further investigation of the tools and their relationship with the direct or indirect health outcomes will provide the basis to structure HIA tools for the evaluation of hospitals built environment design and operations.
Limitations
The tools have been studied assuming that all the indicators included in each criterion are coherent with the criterion main objective. Further investigation at the indicator level might result in slightly different outcomes in terms of category prevalence. Nevertheless, the authors are confident that the methodology is solid enough to provide consistent results.
Future developments
Starting from the results achieved and the limitations highlighted, further researches are encouraged to deepen specific categories and unfold the possible relationship that the built environment variables have with the health outcomes. This development is encouraged to be fostered with collaborations between built environment and public health scholars in order to possibly define hospital facility HIA tools.
Acknowledgements
The authors certify that the submitted manuscript is an original article. Moreover, the authors would like to acknowledge that a wider version of the research based on the same literature and tools set is available as declared in chapter Methodology (24, 33) and has been presented at 2019 ASPHER (The Association of Schools of Public Health in the European Region) Deans’ and Directors’ Retreat.
Annex 1.
List of the 13 tools included in the analysis with the most relevant information
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Fara GM, D’Alessandro D. Population ageing: impacts on the satisfaction of social demand and medical needs. Techne. 2015;9:21–26. doi: 10.13128/Techne-16099. [Google Scholar]
- 2.Capolongo S, Rebecchi A, Brambilla A. E-collection - Urban design and health. European Journal of Public Health 2019. Available on: https://academic.oup.com/eurpub/pages/urban_design_and_health/ [Last accessed: 2019, June 10] [Google Scholar]
- 3.Fehr R, Capolongo S. Healing environment and urban health. Epidemiol Prev. 2016;40(3-4):151–2. doi: 10.19191/EP16.3-4.P151.080. doi: 10.19191/EP16.3-4.P151.080. [DOI] [PubMed] [Google Scholar]
- 4.Signorelli C, Capolongo S, Buffoli M, et al. Italian Society of Hygiene (SItI) recommendations for a healthy, safe and sustainable housing. Epidemiol Prev. 2016;40(3-4):265–270. doi: 10.19191/EP16.3-4.P265.094. 10.19191/EP16.3-4.P265.094. [DOI] [PubMed] [Google Scholar]
- 5.Latimer HS, Gutknecht H, Hardesty K. Analysis of Hospital Facility Growth: Are We Super-Sizing Healthcare. HERD. 2008;1(4):70–88. doi: 10.1177/193758670800100407. 10.1177/193758670800100407. [DOI] [PubMed] [Google Scholar]
- 6.Mauri M. The future of the hospital and the structures of the NHS. Techne. 2015;9:27–34. doi: 10.13128/Techne-16100. [Google Scholar]
- 7.Miedema E, Lindahl G, Elf M. Conceptualizing Health Promotion in Relation to Outpatient Healthcare Building Design: A Scoping Review. HERD. 2019;12(1):69–86. doi: 10.1177/1937586718796651. doi: 10.1177/1937586718796651. [DOI] [PubMed] [Google Scholar]
- 8.Resconi C. La sicurezza in ospedale Strumenti di valutazione e gestione del rischio. Vol 1. INAIL, 2012. Available on: https://www.inail.it/cs/internet/docs/alg-la-sicurezza-in-ospedalefascicolo-1.pdf. [Last accessed: 2019, June 10] [Google Scholar]
- 9.Joachino C, Sileno L, Tresalli G. Le analisi a sostegno della programmazione degli investimenti in edilizia sanitaria. Nota di sintesi. Ires Piemonte, 2017. Available on: https://www.ires.piemonte.it/images/Ricerca/Sanita_edilizia/materiali/2017_IRES_Edilizia_NotaSintesi.pdf. [Last accessed: 2019, June 10] [Google Scholar]
- 10.Quotidiano Sanità. Grillo sui nuovi ospedali: “Già stanziati 6,6 mld ma ne servono 32 per riqualificarli tutti”. Available at: https://www.quotidianosanita.it/governo-e-parlamento/articolo.php?articolo_id=72550. [Last accessed: 2019, June 10] [Google Scholar]
- 11.Henriksen K, Isaacson S, Sadler BL, Zimring CM. The Role of the Physical Environment in Crossing the Quality Chasm. Jt Comm Qual Patient Saf. 2007;33(11):68–80. doi: 10.1016/s1553-7250(07)33114-0. https://doi.org/10.1016/S1553-7250(07)33114-0 . [DOI] [PubMed] [Google Scholar]
- 12.Zhao Y, Mourshed M. Design indicators for better accommodation environments in hospitals: inpatients’ perceptions. Intelligent Buildings International. 2012;4:199–215. doi:10.1080/17508975.2012.701186. [Google Scholar]
- 13.Sadler L, Blair L, Berry L, et al. Fable Hospital 2.0: The Business Case for Building Better Health Care Facilities. Hastings Cent Rep. 2011;41(1):13–23. doi: 10.1002/j.1552-146x.2011.tb00093.x. 10.1002/j.1552-146x.2011.tb00093.x. [DOI] [PubMed] [Google Scholar]
- 14.Donabedian A. Oxford University Press: Oxford; 2003. An Introduction to Quality Assurance in Health Care. [Google Scholar]
- 15.Anaker A, Heylighen A, Nordin S, Elf M. Design Quality in the Context of Healthcare Environments: A Scoping Review. HERD. 2016;10(4):136–50. doi: 10.1177/1937586716679404. 10.1177/1937586716679404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nightingale F. Longman, Roberts and Green: London; 1863. Notes on Hospitals. [Google Scholar]
- 17.Evans GW, McCoy JM. When buildings don’t work: the role of architecture in human health. Journal of Environmental Psychology. 1998;18(1):85–94. 10.1006/jevp.1998.0089. [Google Scholar]
- 18.Gesler W, Bell M, Curtis S, Hubbard P, Francis S. Therapy by Design: Evaluating the UK Hospital Building Program. Health & Place. 2004;10(2):117–28. doi: 10.1016/S1353-8292(03)00052-2. 10.1016/s1353-8292(03)00052-2. [DOI] [PubMed] [Google Scholar]
- 19.Huisman ERCM, Morales E, Van Hoof J, Kort HSM. Healing Environment: A Review of the Impact of Physical Environmental Factors on Users. Building and Environment. 2012;58:70–80. 10.1016/j.buildenv.2012.06.016. [Google Scholar]
- 20.Suess C, Mody M. The influence of hospitable design and service on patient responses. The Service Industries Journal. 2018;38(1-2):127–147. doi: 10.1080/02642069.2017.1385773. [Google Scholar]
- 21.World Health Organization, Regional Office for Europe (WHO-EURO) and European Centre for Health Policy (ECHP), 1999. Gothenburg consensus paper, December 1999. Health impact assessment: main concepts and suggested approach. Brussels: WHO-EURO and ECHP (online) Available at: http://www.hiaconnect.edu.au/files/Gothenburg_Consensus_Paper.pdf . [Last accessed: 2019, June 10] [Google Scholar]
- 22.Ulrich R. View Through a Window May Influence Recovery from Surgery. Science. 1984;224(4647):420–1. doi: 10.1126/science.6143402. doi: 10.1126/science.6143402. [DOI] [PubMed] [Google Scholar]
- 23.Ulrich R, Zimring C, Zhu X, et al. A review of the research literature on evidence-based healthcare design. HERD. 2008;1(3):65–125. doi: 10.1177/193758670800100306. [DOI] [PubMed] [Google Scholar]
- 24.Brambilla A, Rebecchi A, Capolongo S. Evidence Based Hospital Design. A literature review of the recent publications about the EBD impact of built environment on hospital occupants’ and organizational outcomes. Ann Ig. 2019;31(2) doi: 10.7416/ai.2019.2269. DOI: 10.7416/ai.2019.2269. [DOI] [PubMed] [Google Scholar]
- 25.Zhang Y, Tzortzopoulos P, Kagioglou M. Healing built- environment effects on health outcomes: environment-occupant-health framework. Building Research & Information. 2019;47(6):747–766. DOI: 10.1080/09613218.2017.1411130. [Google Scholar]
- 26.Crawley D, Aho I. Building environmental assessment methods: Applications and development trends. Build. Res. Inf. 1999;27:300–308. [Google Scholar]
- 27.Waas T, Hugé J, Block T, Wright T, Benitez-Capistros F, Verbruggen A. Sustainability Assessment and Indicators: Tools in a Decision-Making Strategy for Sustainable Development. Sustainability. 2014;6:5512–5534. doi:10.3390/su6095512. [Google Scholar]
- 28.Bernardi E, Carlucci S, Bohne RA. An Analysis of the Most Adopted Rating Systems for Assessing the Environmental Impact of Buildings. Sustainability. 2017;9:1226. DOI:10.3390/su9071226. [Google Scholar]
- 29.Phiri M, Chen B. Sustainability and Evidence-Based Design in the Healthcare Estate, Springer 2014. doi 10.1007/978-3-642-39203-0. [Google Scholar]
- 30.Mills GRW, Phiri M, Erskine J, Price DFA. Rethinking healthcare building design quality: an evidence-based strategy, Building Research & Information. 2015;43(4):499–515. DOI: 10.1080/09613218.2015.1033880. [Google Scholar]
- 31.Pati D, Lorusso LN. How to Write a Systematic Review of the Literature. HERD. 2017;11(1):15–30. doi: 10.1177/1937586717747384. doi: 10.1177/1937586717747384. [DOI] [PubMed] [Google Scholar]
- 32.Elf M, Nordin S, Wijk H, Mckee KJ. A Systematic Review of the Psychometric Properties of Instruments for Assessing the Quality of the Physical Environment in Healthcare. J Adv Nurs. 2017;73(12):2796–816. doi: 10.1111/jan.13281. DOI:10.1111/jan.13281. [DOI] [PubMed] [Google Scholar]
- 33.Brambilla A, Capolongo S. Healthy and Sustainable Hospital Evaluation—A Review of POE Tools for Hospital Assessment in an Evidence-Based Design Framework. Buildings. 2019;9:76. doi:10.3390/buildings9040076. [Google Scholar]
- 34.Bottero MC, Buffoli M, Capolongo S, Cavagliato E, di Noia M, Gola M, et al. A multidisciplinary sustainability evaluation system for operative and in-design hospitals. Improving Sustainability During Hospital Design and Operation: A Multidisciplinary Evaluation Tool. In: Capolongo S, Bottero MC, Buffoli M, Lettieri E, editors. Cham: Springer; 2015. pp. 31–114. doi: 10.1007/978-3-319-14036-0_4. [Google Scholar]
- 35.Dell’Ovo M, Capolongo S. Architectures for health: Between historical contexts and suburban areas Tool to support location strategies. Technè. 2016;12:269–276. 10.13128/Techne-19362. [Google Scholar]
- 36.Zimmermann RK, Skjelmose O, Jensen KG, Jensen KK, Birgisdottir H. Categorizing Building Certification Systems According to the Definition of Sustainable Building. IOP Conf. Ser: Mater. Sci. Eng. 2019;471:092060. [Google Scholar]
- 37.Faroldi E, Fabi V, Vettori MP, Gola M, Brambilla A, Capolongo S. Health tourism and thermal heritage. Assessing Italian Spas with innovative multidisciplinary tools. Tourism Analysis. 2019;24(3) (in press) doi:10.3727/108354219X15511865533121. [Google Scholar]
- 38.Buffoli M, Capolongo S, di Noia M, Gherardi G, Gola M. Healthcare sustainability evaluation systems. Improving Sustainability During Hospital Design and Operation: A Multidisciplinary Evaluation Tool. In: Capolongo S, Bottero MC, Buffoli M, Lettieri E, editors. Cham: Springer; 2015. pp. 23–30. doi: 10.1007/978-3-319-14036-0_3. [Google Scholar]
- 39.Heinzerling D, Schiavon S, Webster T, Arens E. Indoor environmental quality assessment models: A literature review and a proposed weighting and classification scheme. Build. Environ. doi: 2013; 70, 210-222. 10.1016/j.buildenv.2013.08.027. [Google Scholar]
- 40.Buffoli M, Nachiero D, Capolongo S. Flexible healthcare structures: analysis and evaluation of possible strategies and technologies. Ann Ig. 2012 Nov-Dec;24(6):543–552. [PubMed] [Google Scholar]
- 41.Astley P, Capolongo S, Gola M, Tartaglia A. Operative and design adaptability in healthcare facilities. Technè. 2015;9:162–170. DOI: 10.13128/Techne-16118. [Google Scholar]
- 42.Buffoli M, Bellini E, Bellagarda A, di Noia M, Nickolova M, Capolongo S. Listening to people to cure people: The LpCp - tool, an instrument to evaluate hospital humanization. Ann Ig. 2014;26(5):447–55. doi: 10.7416/ai.2014.2004. doi: 10.7416/ai.2014.2004. [DOI] [PubMed] [Google Scholar]
- 43.Ulrich R, Berry LL, Quan X, Parish JT. A Conceptual Framework for the Domain of Evidence-Based Design. HERD. 2010;4(1):95–114. doi: 10.1177/193758671000400107. 10.1177/193758671000400107. [DOI] [PubMed] [Google Scholar]
- 44.Origgi L, Buffoli M, Capolongo S, Signorelli C. Light wellbeing in hospital: research, development and indications. Ann Ig. 2011;23(1):55–62. [PubMed] [Google Scholar]
- 45.WHO/WEF. Geneva: World Health Organisation / World Economic Forum; 2008. Preventing noncommunicable diseases in the workplace through diet and physical activity: WHO/World Economic Forum report of a joint event. Available at: https://www.who.int/dietphysicalactivity/WHOWEF_report_JAN2008_FINAL.pdf. [Last accessed: 2019, June 10] [Google Scholar]
- 46.Jirathananuwat A, Pongpirul K. Promoting physical activity in the workplace: A systematic meta-review. J Occup Health. 2017;59:385–393. doi: 10.1539/joh.16-0245-RA. doi: 10.1539/joh.16-0245-RA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Anthes E. The Office Experiment: Can Science Build the Perfect Workspace. Nature. 2016;537:294–296. doi: 10.1038/537294a. doi: 10.1038/537294a. [DOI] [PubMed] [Google Scholar]
- 48.World Health Organization, Health Care Without Harm. Geneva, Switzerland: World Health Organization; 2009. Healthy hospitals, healthy planet, healthy people: Addressing climate change in healthcare settings [Internet] Available at: www.who.int/entity/globalchange/ publications/climatefootprint_report.pdf?ua=1. [Last accessed: 2019, June 10] [Google Scholar]
- 49.Storz MA. A practical guide for physicians and health care workers to reduce their carbon footprint in daily clinical work. Perm J. 2018;22:17–145. doi: 10.7812/TPP/17-145. doi: https://doi.org/10.7812/TPP/17-145 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pilkington P, Grant M, Orme J. Promoting integration of the health and built environment agendas through a workforce development initiative. Public Health. 2008;122:545–551. doi: 10.1016/j.puhe.2008.03.004. doi: 10.1016/j.puhe.2008.03.004. [DOI] [PubMed] [Google Scholar]