Abstract
Background and aim of work: Musculoskeletal injuries are the most common cause of severe, chronic pain and physical disability for the majority of all sport-related injuries. Platelet-rich plasma is being used more frequently to promote healing of muscle injuries. We report a case of 39 years old non professional soccer player who came to our attention for a quadriceps muscle pain onset after kicking the ball during a match. Methods: Clinical and instrumental evaluation revealed a myotendinous junction rupture of the rectus femoris with retraction of 1.5 cm from the anterior inferior iliac spine. We decided to treat the patient with PRP ultrasound guided injections and a specific rehabilitation protocol. Results: Clinical evaluation 45 days following the end of the treatment showed the resolution of the pain and the full recovery of strength and range of motion. Muscle healing was documented by magnetic resonance imaging. Conclusions: Even if the role of PRP in muscle injury is not still clear, the result observed confirms that it could be used in the treatment of muscle lesions. (www.actabiomedica.it)
Keywords: rectus femoris, rupture, injury, PRP, muscle
Introduction
Musculoskeletal injuries represent a challenging problem for traumatology and sports medicine, as they are the most common cause of severe long-term pain and physical disability for the majority of athletes (1).
The quadriceps and hamstring muscle groups are more commonly affected by strains and avulsions.
The most common type of quadriceps injury is an intramuscular strain at the myotendinous junction (2, 3).
Proximal lesions of the rectus femoris in adult athletes are not commonly reported. Their optimal treatment is controversial; it is usually conservative but in some cases, especially in high level athletes with myotendinous retraction ≥ 1.5 cm or in adolescent with avulsion and displacement ≥ 2cm, surgery may be indicated (4-7).
In those lesions treated conservatively healing occurs slowly and it depends on their gravity (approximately 4-12 weeks); athletes are discouraged to resume their sport activity until walking without pain is possible. During this period, it has been demonstrated that the long recovery period may be also due to the structural alterations of the myotendinous junction induced by too long immobilization (8-10). For this reason, it is commonly accepted that a quick mobilization associated with specific rehabilitation and physical therapies facilitates an adequate structural resolution of the lesion (11). Also platelet rich plasma (PRP) injections may favour this process.
PRP is a biological blood product obtained from the patient, which has anti-inflammatory and pro-regenerative functions (12-14).
It has been demonstrated that PRP is able to induce proliferation of muscle cells, differentiation of satellite cells, and facilitate angiogenesis (15, 16). In a clinical context, it has been reported that full recovery of functional capabilities could be restored in a smaller time when compared to other treatments (17-19).
However, results described by different research groups are conflicting and did not provide full support to the use of PRP for the treatment of muscle injuries.
For these reasons additional investigations should be important to better clarify PRP clinical applications (20, 21).
Case report
A 39-year-old non professional soccer player arrived in our Emergency Department complaining of pain in his anterior thigh near the insertion of the rectus femoris on the anterior inferior iliac spine (AIIS), which happened during a football match; he referred a feeling of snapping in the same zone.
The patient walked with the help of two crutches because he was unable to weight bear freely due to pain.
An evident hematoma in the region mentioned above was noticeable.
On physical examination there was pain due to manual pressure, a deficit of strength in hip flexion against manual resistance and a gap in the AIIS region which was clinically palpable. For this reason we suspected a lesion/avulsion of proximal rectus femoris.
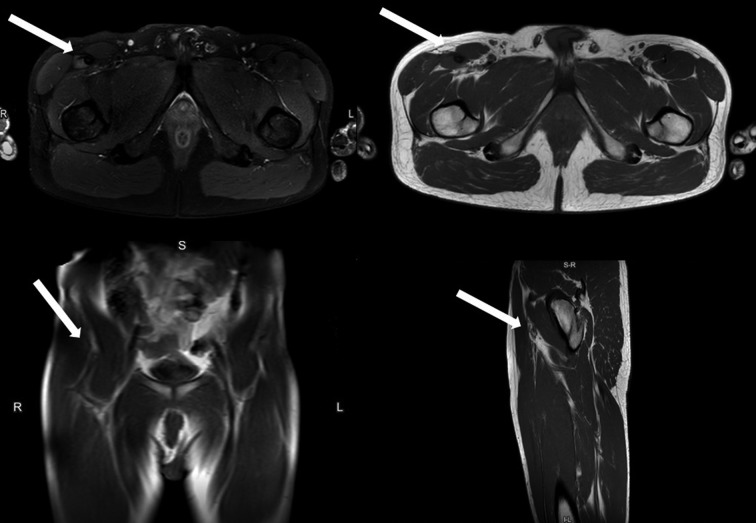
An ultrasound study confirmed our suspicion and showed the presence of hematoma at the myo-tendinous junction with fascial blood layers and tendon rupture of the proximal rectus femoris (Figure 1).
Figure 1.
Ultrasonography performed at the Emergency Department with muscle rupture (arrows)
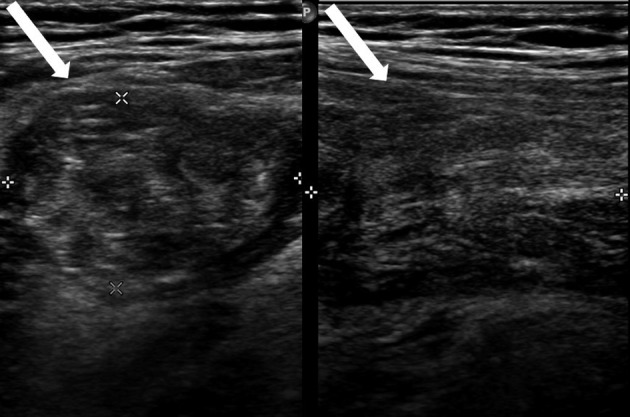
Furthermore, magnetic resonance imaging (MRI) performed 7 days later confirmed the diagnosis and showed a lesion of the myotendinous junction characterized by partial lesion of the direct head and total lesion of the indirect head of the tendon with retraction of 1.5 cm associated to edema and hematoma (Figure 2).
Figure 2.
MRI performed 6 days after injury with the signs of myotendinous lesion and retraction (arrows); coronal and axial views
In that moment the patient got better. He did not use crutches, he had less pain during his daily life and he had less pain both in manual pressure and in tests against manual resistance.
In the face of this clinical improvement we decided to not consider the surgical option and to treat the patient with ultrasound guided PRP injections and a specific rehabilitation program, which was initially based on isometric exercises and, later, on eccentric work exercises and it was always accompanied by tecartherapy.
An autologous blood sample of the patient was taken by the Transfusion Center of the University Hospital of Parma. From this sample, 3 stocks of PRP were obtained. The injections were done 10, 20 and 30 days after injury (5 ml of PRP and 1 of thrombin) under ultrasound guidance.
Following the first infiltration the patient reported a progressive improvement in symptoms and a progressive decrease in pain.
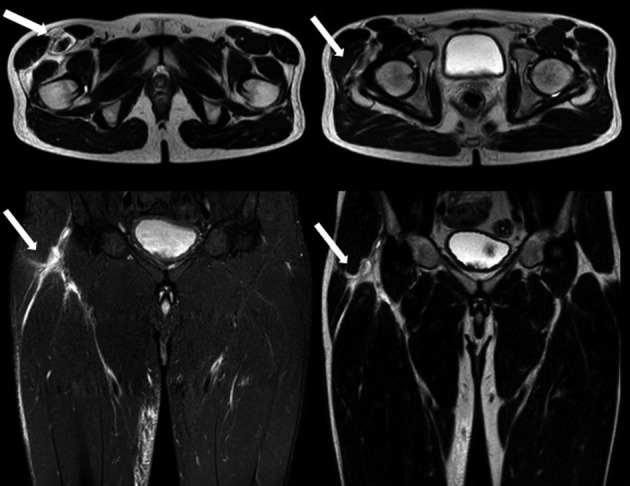
Fifteen days after the end of the infiltrative cycle another evaluation showed the absence of pain and the patient referred to walk freely without limitations in his daily life, even if a deficit of strength against manual resistance was present (Figure 3).
Figure 3.

Clinical evalutation 15 days after the end of the infiltrative cycle
We therefore planned a new MRI and clinical evaluation 45 days after the end of the infiltrative cycle.
In the meantime, the patient continued the rehabilitation program, including concentric exercises against elastic resistance.
At the final clinical check the patient did no longer complain of pain. There was no more gap in the AIIS region, the range of motion was 0°-130° bilaterally and there was no deficit of strength against manual resistance. The MRI confirmed the advanced stage of healing as no longer hematoma was appreciable and edema had almost completely disappeared (Figure 4 and 5).
Figure 4.
Clinical evaluation 45 days following the infiltrative cycle
The patient returned to his sports activity without any problems 90 days after injury.
Figure 5.
MRI 45 days following the infiltrative cycle with advanced signs of healing (arrows)
Discussion
Musculoskeletal injuries represent a challenging problem for traumatology and sports medicine; they are the most common cause of severe, chronic pain and physical disability for the majority of all sport-related injuries (1, 22, 23).
In addiction to the clinical examination, imaging plays a key role in the diagnosis of these lesions; in fact clinical assessment may not be sufficient for distinguishing contusions from tears or for estimating the size of the lesion and the entity of the muscular retraction (24).
Ultrasound offers both static and dynamic views of the quadriceps; given the low cost and expanding availability of the technology it has to be considered an excellent first step in evaluation (25).
Nevertheless, MRI is the gold standard to define the gravity of these lesions and it allows a more global multidimensional assessment. Hematoma may be observed in case of complete tears and may have various signal intensities according to the time elapsed since the injury. These imaging tools are also important to follow the healing process and to detect complication occurrence thus reducing sports inactivity duration (26).
Quadriceps and hamstring muscle groups are more commonly affected by strain and avulsion injuries.
The most common type of quadriceps injury is an intramuscular strain at the myotendinous junction (3, 27).
From a histochemical point of view, in fact, the most evident effect is a dramatic reduction of glycosaminoglycans at the level of the muscle-tendon interface; moreover, there is an increase in type 3 collagen compared to type 1 collagen.
Type 3 collagen appears weaker from a biomechanical point of view than type 1, which is the basic collagen of myotendinous junction and tendon. Wrong training and inactivity accentuate this.
There is, in fact, growing evidence that these conditions play a key role in these structural modifications thus leading to a reduction in strength and elasticity at the level in the tendon and myotendinous junction (26).
Proximal lesions of the rectus femoris in adult athletes are not commonly reported, and their optimal treatment may vary (4). It is usually conservative and surgery has limited indications (high level athletes with myotendinous retraction ≥ 1.5 cm or in adolescent with avulsion and displacement ≥ 2cm) (4-7).
Healing time depends on the grade of rupture and athletes are discouraged to resume their sport activity until walking without pain is possible (approximately 4-12 weeks). During this period, it has been demonstrated that the long recovery period may be also due to the structural alterations of the myotendinous junction induced by the excessive immobilization after the injury (8, 10).
For this reason, it is commonly accepted that a quick mobilization, followed by a specific rehabilitation program and physical therapies, may facilitate an adequate structural resolution of the injury. PRP injections can further favour this process (11).
The therapeutic program initially starts with isometric exercises. After few days, and after the acute phase and the articular excursion is recovered, eccentric and concentric isotonic exercises were introduced as well as progressive stretching. Exercises must always be performed below the pain threshold for the duration of rehabilitation and can be associated to physical therapies.
PRP is a biological blood product obtained from the patient, which has anti-inflammatory and pro-regenerative functions (12) and is being used more frequently to promote healing of muscle injuries (28-30).
There is abundant evidence suggesting that growth factors may play a key role in the healing process, especially in the early stages of inflammation (13); in fact it has been demonstrated that PRP is able to induce proliferation of muscle cells, differentiation of satellite cells, and facilitate angiogenesis (15, 16).
In a clinical context, it has been reported that full recovery of functional capabilities was restored in a smaller time when compared to other treatments (11).
Despite the reported clinical successes with the use of growth factors there is still a lack of knowledge on the biological mechanism underlying the activity of platelet-rich plasma during the process of muscle healing (13); results of studies performed by different research groups are conflicting and did not provide full support to the use of PRP for the treatment of muscle injuries. For these reasons additional investigations would be important to better clarify PRP clinical applications in these kinds of injuries (20,21).
The satisfactory outcome of this case report confirms that PRP injections associated to specific rehabilitation may play a key role in the treatment of muscular lesions. Authors believe that PRP injections has to be performed with the assistance of ultrasound and in the early stage of inflammation.
Conclusions
Proximal lesions of the rectus femoris in adult athletes are not commonly reported and their therapeutic management remains controversial. MRI is the diagnostic and prognostic gold standard exam. Although the surgical option is a choice in selected cases, conservative approach is the standardized treatment in most patients. In this perspective, PRP associated with rehabilitation and physical therapy may play a key role both in the healing of the lesion and in the early recovery of physical activity.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Woolf AD, Pfleyer B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81:646–56. [PMC free article] [PubMed] [Google Scholar]
- 2.Armfield DR, Kim DH, Towers JD, Bradley JP, Robertson DD. Sports related muscle injury in the lower extremity. Clin Sports Med. 2006;25:803–42. doi: 10.1016/j.csm.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 3.Hasselman CT, Best TM, Hughes C, Martinez S, Garrett WE. An explanation for various rectus femoris strain injuries using previously undescribed muscle architecture. Am J Sports Med. 1995;23:493–9. doi: 10.1177/036354659502300421. [DOI] [PubMed] [Google Scholar]
- 4.Gamradt SC, Brophy RH, Barnes R, Warren RF, Byrd JWT, Kelly BT. Nonoperative treatment for proximal avulsion of the rectus femoris in professional american football. The American Journal of Sports Medicine. 2009;37:1370–4. doi: 10.1177/0363546509333477. [DOI] [PubMed] [Google Scholar]
- 5.Pogliacomi F, Costantino C, Pedrini MF, Pourjafar S, De Filippo M, Ceccarelli F. Anterior groin pain in athlete as consequence of bone diseases: aetiopathogenensis, diagnosis and principles of treatment. Medicina dello Sport. 2014;67(1):1–27. [Google Scholar]
- 6.Pogliacomi F, Calderazzi F, Paterlini M, Pompili M, Ceccarelli F. Anterior iliac spines fractures in the adolescent athlete: surgical or conservative treatment. Medicina dello Sport. 2013;66(2):231–40. [Google Scholar]
- 7.Calderazzi F, Nosenzo A, Galavotti C, Menozzi M, Pogliacomi F, Ceccarelli F. Apophyseal avulsion fractures of the pelvis. A review. Acta Biomed. 2018;89(4):470–6. doi: 10.23750/abm.v89i4.7632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lovering RM, Roche JA, Bloch RJ, De Deyne PG. Recovery of function in skeletal muscle following 2 different contractioninduced injuries. Arch Phys Med Rehabil. 2007;88:617–25. doi: 10.1016/j.apmr.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 9.Orchard J, Best TM, Verrall GM. Return to play following muscle strains. Clin J Sport Med. 2005;15:436–41. doi: 10.1097/01.jsm.0000188206.54984.65. [DOI] [PubMed] [Google Scholar]
- 10.Kannus P, Jozsa L, Kvist M, Lehto M, Järvinen M. The effect of immobilization on myotendinous junction: an ultrastructural, histochemical and immunohistochemical study. Acta Physiol Scand. 1992;144:387–94. doi: 10.1111/j.1748-1716.1992.tb09309.x. [DOI] [PubMed] [Google Scholar]
- 11.Järvinen M. Healing of a crush injury in rat striated muscle. 2. A histological study of the effect of early mobilization and immobilization on the repair processes. Acta Pathol Microbiol Scand. 1975;83:269–82. [PubMed] [Google Scholar]
- 12.Osterman C, McCarthy MBR, Cote MP, Beitzel K, Bradley J, nPolkowski G, et al. Platelet-rich plasma increases anti-inflammatory markers in a human culture model for osteoarthritis. Am J Sports Med. 2015;43:1474–84. doi: 10.1177/0363546515570463. [DOI] [PubMed] [Google Scholar]
- 13.Borrione P, Grasso L, Chierto E, Geuna S, Racca S, Abbadessa G, et al. Experimental model for the study of the effects of platelet-rich plasma on the early phases of muscle healing. Blood Transfus. 2014;12(Suppl 1):s221–8. doi: 10.2450/2013.0275-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Di Benedetto P, Di Benedetto ED, Beltrame A, Gisonni R, Cainero V, Causero A. Arthroscopic rotator cuff repair with or without PrP: our experience. Acta Biomed. 2016;87(Suppl 1):75–83. [PubMed] [Google Scholar]
- 15.Alsousou J, Thompson M, Hulley P, Noble A, Willett K. The biology of platelet-rich plasma and its application in trauma and orthopaedic surgery: a review of the literature. J Bone Joint Surg B. 2009;91:987–96. doi: 10.1302/0301-620X.91B8.22546. [DOI] [PubMed] [Google Scholar]
- 16.McClure MJ, Garg K, Simpson DG, Ryan JJ, Sell SA, Bowlin GL, et al. The influence of platelet-rich plasma on myogenic differentiation. J Tissue Eng Regen Med. 2016;10:E239–49. doi: 10.1002/term.1755. [DOI] [PubMed] [Google Scholar]
- 17.Hamid MS, Mohamed Ali MR, Yusof A, George J, Lee LPC. Platelet-rich plasma injections for the treatment of hamstring injuries: a randomized controlled trial. Am J Sports Med. 2014;42:2410–8. doi: 10.1177/0363546514541540. [DOI] [PubMed] [Google Scholar]
- 18.Bubnov R, Yevseenko V, Semeniv I. Ultrasound guided injections of platelets rich plasma for muscle injury in professional athletes. Comparative study. Med Ultrason. 2013;15:101–5. doi: 10.11152/mu.2013.2066.152.rb1vy2. [DOI] [PubMed] [Google Scholar]
- 19.Anitua E, Andia I, Ardanza B, Nurden P, Nurden AT. Autologous platelets as a source for healing and tissue regeneration. Thromb Haemost. 2004;91:4–15. doi: 10.1160/TH03-07-0440. [DOI] [PubMed] [Google Scholar]
- 20.Reurink G, Goudswaard GT, Moen MH, Weir A, Verhaar JA, Bierma-Zeinstra SM, et al. Platelet rich plasma injections in acute muscle injury. N Engl J Med. 2014;370:2546–7. doi: 10.1056/NEJMc1402340. [DOI] [PubMed] [Google Scholar]
- 21.Mosca MJ, Rodeo SA. Platelet-rich plasma for muscle injuries: game over or time out. Curr Rev Muscoloskelet Med. 2015;8:145–53. doi: 10.1007/s12178-015-9259-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beiner JM, Jokl P. Muscle contusion injuries: current treatment options. J Am Acad Orthop Surg. 2001;9:227–37. doi: 10.5435/00124635-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Järvinen M, Lehto MUK. The effect of early mobilization and immobilization on the healing process following muscle injuries. Sports Med. 1993;15:78–89. doi: 10.2165/00007256-199315020-00002. [DOI] [PubMed] [Google Scholar]
- 24.Pasta G, Nanni G, Molini L, Bianchi S. Sonography of the quadriceps muscle: examination technique, normal anatomy, and traumatic lesions. J Ultrasound Jun. 2010;13(2):76–84. doi: 10.1016/j.jus.2010.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Esser S, Jantz D, Hurdle MF, Taylor W. Proximal rectus femoris avulsion: ultrasonic diagnosis and nonoperative management. J Athl Train. 2015;50(7):778–80. doi: 10.4085/1052-6050-50.2.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pesquer L, Poussange N, Sonnery-Cottet B, Graveleau N, Meyer PB, Dallaudiere MF. Imaging of rectus femoris proximal tendinopathies. Skeletal Radiology. 2016;45:889–97. doi: 10.1007/s00256-016-2345-3. [DOI] [PubMed] [Google Scholar]
- 27.Armfield DR, Kim DH, Towers JD, Bradley JP, Robertson DD. Sports related muscle injury in the lower extremity. Clin Sports Med. 2006;25:803–42. doi: 10.1016/j.csm.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 28.Bernuzzi G, Petraglia F, Pedrini FM, De Filippo M, Pogliacomi F, Verdano MA, et al. Use of platelet-rich-plasma in the care of sports injuries: our experience with ultrasound guided injection. Blood Transfus. 2014;12:s229–34. doi: 10.2450/2013.0293-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Follo F, Dejana DO, Belletti M, Bongiovanni N, Scarpa G, Pezzali P, et al. Management and effect of platelet-rich plasma on wound healing: small reality of Oglio Po Hospital. Acta Biomed. 2017 Nov 30;88(5-S):66–70. doi: 10.23750/abm.v88i5-S.6895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pogliacomi F, Schiavi P, Paraskevopoulos A, Leigheb M, Pedrazzini A, Ceccarelli F, et al. When is indicated viscosupplementation in hip osteoarthritis. Acta Biomed. 2018 Dec 18;90(1-S):67–74. doi: 10.23750/abm.v90i1-S.8000. [DOI] [PMC free article] [PubMed] [Google Scholar]