Abstract
Background and aim of the work: To describe a valid option for the treatment of locked posterior fracture-dislocation of the shoulder (LPFDS) and to compare it to the literature about this topic. Methods: We present a small case series (3 patients), with a medium follow up at 4 years and 5 months. We accurately describe our surgical strategies, underlining the choice of approach, reduction and fixation. Results: The three patients showed excellent functional and radiological results at the follow up examinations, with a full range of shoulder movements and complete regain of pre-trauma activities. A lateral approach (standard or minimally invasive), a reduction technique with a Shantz pin in the head and in the humeral shaft, and fixation with a locking plate were used in the three patients. Conclusion: LPFDS is a challenging lesion, hard to recognize and to treat. Our suggested method of treatment is highly reproducible and has revealed itself to be very effective in achieving good results. (www.actabiomedica.it)
Keywords: locked posterior fracture-dislocation of the shoulder (LPFDS), trans-deltoid lateral approach, Shantz pins, locking plate
Introduction
Posterior dislocation of the shoulder is not common, representing between 3% and 5% of all shoulder dislocations (1, 2). 1% of shoulder dislocations involve a fracture, with an incidence estimated at 0.6 in 100,000 per year (3-6), but only 0.9% of the 1500 cases reported by Neer concerned posterior fracture dislocations (7, 8).
The mechanisms that cause posterior shoulder dislocation can be classified in two main groups: atramautic (forced muscle contractions during epileptic seizures, electric shock or electroconvulsive therapy) and traumatic (high energy trauma such as motor vehicle accidents, where the injury consists in axial loading of the arm in an adducted, flexed, and internally rotated position) (9).
In a posterior dislocation, the anatomo-pathologic findings can consist in a pure capsulo-labral lesion eventually associated to an impacted fracture of the humeral head (revers Hills-Sachs). In some cases, the lesion is complicated by a fracture of the proximal humerus, usually at the level of the anatomic neck. This fracture is defined “complex” by some authors (10), or locked posterior fracture-dislocation of the shoulder (LPFDS) by others, with the latter term indicating the complexity of the bone lesion (that can be two, three or four parts fracture sec. Neer classification) and the difficulty of the treatment of this injury.
LPFDS (as other posterior shoulder dislocations) can be easily missed; up to 79% of missed diagnoses are given in some reports (11) if a proper x-ray and CT scan investigation are not performed in the acute setting. As a matter of fact, the impossibility in patients with a proximal humeral fracture to obtain an axillary view of the shoulder can strongly underestimate the real pattern of this lesion (4). A physical examination of the patient is extremely useful, demonstrating a locked internally rotated shoulder with the impossibility of external rotation and elevation; the pain caused by minimal mobilization can be an obstacle to an accurate examination. In case of missed diagnosis - “neglected” (within three weeks) or “chronic posterior fracture-dislocation” (after three weeks) -, the possibility of a proper open reduction and internal fixation could be impossible due to the vascular impairment of the humeral head and to the reabsorption of the tuberosities. Thus, the only possible treatment can be joint replacement.
There are some x-ray signs that can give suspicion to a posterior dislocation. A conventional anterior-posterior (AP) view of the shoulder shows an overlapping halfmoon appearance because of the intersection of the head and glenoid; but this peculiar sign can be lacking in LPFDS because of the head-splitting fracture-dislocation (12). Another sign that can be noticed is the lightbulb sign, which refers to the abnormal AP radiologic appearance of the humeral head in posterior shoulder dislocation (11). Perhaps the most characteristic radiologic sign of LPFDS is the double shadow line sign: it indicates the posterior dislocation of the shoulder with head-splitting fracture of the head (13). If LPFDS is diagnosed, or even suspected, a CT scan is recommended to better understand the bony anatomy and to properly plan the operation. Axial cuts and 3D reconstruction are particularly helpful to show the rate of involvement of the articular surface of the humerus. MRI is not considered useful before the operation.
Meanwhile, in cases of a posterior dislocation with an impaction fracture, on axial cuts of the CT scan one can have a suspicion of an engaging lesion. In cases of fracture dislocation, it is impossible to know before reduction of the head if the lesion is at risk of engaging.
In cases of posterior dislocation of the shoulder with a reverse Hill-Sachs lesion, the treatment options are well known and described: disimpaction of the fracture with lesser tubercle transfer, reconstruction with allograft or filling of the defect with bone substitutes. These options depends on the amount of impaction (14, 15).
Arthroplasty is preferred in cases in which 50% or more of the articular surface is affected. In cases of LPFDS there is not a gold standard treatment: the surgery can vary from reduction and pinning to open reduction and internal fixation to replacement arthroplasty. In the choice of open reduction and internal fixation, even the surgical approach is a matter of debate and it can sometimes be the first problem for the surgeon.
Robinson (10) was the first to accurately describe this lesion, which had been misdiagnosed or confused with other shoulder injuries in previous literature. He noted that, in the past, this fracture-dislocation was treated prevalently with a replacement arthroplasty of the humeral head, considering its high risk of avascular necrosis (16). However, the literature has shown that this complication is less frequent than previously thought and the poor outcomes of arthroplasty in these lesions has led to a more conservative treatment of this injury. Thus reduction and fixation of this fracture dislocation has become the preferred method of treatment, aiming to maintain the integrity and the vitality of the humeral head (3, 17-19).
We present a small case series, emphasizing our choice of approach, reduction manoeuvres and fixation strategies of this injury.
Case series
We analysed 3 patients who underwent surgery in our department.
Gender, age, side, type of fracture according to the Neer classification and mechanism of injury are shown in table 1.
Table 1.
Series of 3 patients treated. Characteristics of patients, fracture and scores at follow-up
| Patient and sex | Age | Side | Neer classification | Mechanism of injury | Day of surgery from the admission date | Tiem of follow-up | Quickdash score | Constant score |
| G.F., male (Fig. 1) | 42 | Right | 2 parts | Bicycle | Same day | 4 years and 6 months | 12 | 100 |
| G.M., male (Fig. 2) | 44 | Right | 2 parts | Motorbike | 1 | 4 years and 5 months | 11 | 100 |
| T.D., male (Fig. 3) | 68 | Right | 3 parts | Bicycle | 2 | 4 years and 4 months | 13 | 95 |
All the patients were treated by two experienced trauma surgeons (L.B.V. and S.L.) using the same surgical approach, the same reduction strategies and the same hardware (Philos plate, DePuy Synthes, Johnson & Johnson, Oberdorf, Switzerland), which will be described later.
In the post-operative period we avoided immobilisation of the joint, inviting the patient to immediately start with gentle movements of the shoulder and active mobilization of their elbow, wrist and hand. The wounds healed uneventfully and stitches were removed 2 weeks after surgery. The active therapy started after 3 weeks, usually 3 days a week under the supervision of a physiotherapist.
The patients were evaluated at 1, 3 and 6 months after discharge, with a clinical examination and an x-ray of the shoulder. After the first check-up (1 month) the patients were invited to increase the load of physiotherapy and to slow down with the exercises only in case of pain.
The three patients were available at the follow-up call (average interval of 4 years and 5 months).
They were evaluated with the Quick Dash score and with the Constant score (table 1) and with an x-ray of the shoulder. The clinical results were surprisingly excellent despite the severity of the initial injury. The medium Quick Dash score was 12 (maximum 11) and the medium Constant score was 98.3 (maximum 100).
In the x-ray examinations, all the fractures showed complete healing with regained anatomical relationship between the head and the tuberosities. None of them had radiological signs of head necrosis or gleno-humeral arthritis.
All the patients sustained to have regained complete functionality of their shoulder, without any limitations of their work, sport and recreational activities. They confirmed that they were very satisfied. At the follow-up examination, one of the patients (G.M.), revealed a hypotrophy of the anterior third of the deltoid. This was perhaps due to a partial lesion of some fibres of the axillary nerve. This problem had never given any problems to the patient during daily work or leisure activities. Two patients (G.F. and T.D.) returned to work (office work) at about 5 weeks after surgery. The other (G.M., metal-worker) after 9 weeks. One of the patients (G.M.) restarted his favourite sport (cross motor biking) 40 days after surgery, despite this activity being discouraged by the examining physician at the first follow-up. The other two began their sporting activities (cycling) again at about 8 weeks from trauma.
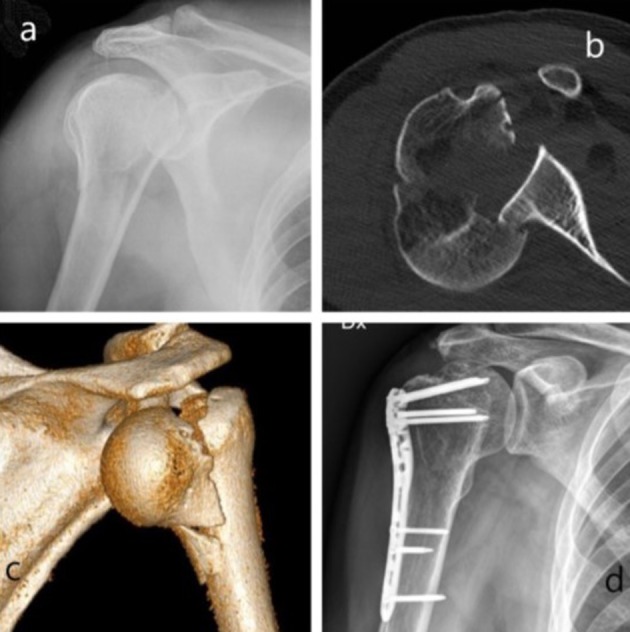
Figure 1.

Imaging of patient G.F.: x-ray after trauma (a), axial ct of the fracture (b), 3d reconstruction of the fracture-dislocation (c), x-ray at follow-up (d)
Figure 2.

Imaging of patient G.M.: x-ray after trauma (a), axial ct of the fracture (b), 3d reconstruction of the fracture-dislocation (c), x-ray at follow-up (d)
Figure 3.
Imaging of patient T.D.: x-ray after trauma (a), axial ct of the fracture (b), 3d reconstruction of the fracture-dislocation (c), x-ray at follow-up (d)
Surgical approach
The choice of the approach is, in the Authors’ opinion, the most important variable when addressing LPFDS. The approach must allow both the manipulation and the reduction of the dislocated humeral head as well as the fixation of the fracture.
In previous literature, the problem of the approach has been raised many times and different strategies have been used to handle this injury (10, 20-22). The deltopectoral approach has been widely used in shoulder surgery. It is useful in nearly all fractures of the proximal humerus and is mandatory in case of anterior fracture-dislocation of the shoulder. In LPFDS, the head lies behind the glenoid or the neck of the scapula and typically the upper arm is shortened because of the proximalization of meta-diaphysis of the humerus; the lesser tuberosity is frequently intact and the tendon of the subscapularis interferes with the access to the humeral head. Therefore, it would very challenging, if not impossible, from an anterior approach, to reach the humeral head without the tenotomy of the subscapularis at its origin.
Gokkus (12) proposed a modification of the deltopectoral approach, with subperiostal detachment of supraspinatus and subscapularis from their humeral origin. This exposure allows wide access to the joint and to humeral head. The Authors describe good results at the 1-year follow up. This strategy surely allows extensive access to the proximal humerus but it expects a post-operative loss of time to start physical treatment and rehabilitation, time which is necessary to allow the healing of the detached tendons. Furthermore, avoiding the release of tendons’ insertions is usually recommended during any surgical approach.
Stableforth (20), in 1992, realized the difficulty in treating this lesion with a standard anterior approach. He therefore proposed the use of a “superior subacromial approach”, which is the extension of the Author’s approach for rotator cuff surgery. He extended the deep incision in a transversal plane, from 3 cm medial to the acromion-clavicular joint to 4 cm distal to the edge of the acromion. After detaching subperiostally the deltoid origin from the anterior acromion, he reached the humeral head with the incision of the supraspinatus tendon 5 mm behind the cuff interval. This approach only allows the fixation of the epiphysis of the humerus and it did not describe the distal extension necessary for the fixation of the fracture with plate and screws.
Fiorentino (21) suggests a double approach. Firstly, a straight posterior approach through the deltoid fibres, developing the space between infraspinatus and teres minor. In their experience, with this approach, the humeral head can easily be reduced with gentle manual pressure. Then, a standard deltopectoral approach is carried out to fix the fracture with plate and screws.
Robinson (10), in his 26-case series, describes a shoulder-strap skin incision and a modified deltoid-splitting surgical approach with identification and protection of the axillary nerve when it traverses the distal extent of the incision. A similar approach was then described by Shin who uses a straight lateral incision with protection and mobilization of the axillary nerve (23).
In our experience, and according to other authors (10), the key factor in facilitating the relocation of the humeral head is a lateral approach. The standard trans-deltoid lateral approach (Fig. 4), with distal extension and isolation of the axillary nerve or its variant with two incisions for minimally invasive plate osteosynthesis, has been widely used for proximal humerus fractures and it is extremely useful in LPFDS. Indeed, with this approach, the humeral head can be palpated and manipulated permitting the reduction of the dislocation. Furthermore, the lateral approach allows the standard fixation with plate and screws of the proximal humerus without adding other incisions and, most importantly, without detaching muscular insertion. Robinson (10) adds an arthrotomy through the rotator cuff interval to assess the extent of the reverse Hill-Sachs and, consequently, to treat this adjunctive lesion with elevation of the osteo-chondral impaction and bone packing of the defect. In our series, this adjunctive exposure has never been done because, after reduction and fixation of the fracture, not any of the shoulders resulted in having an engaging revers Hill-Sachs. In fact, the passive range of movement of the shoulders was completely free in all the three cases.
Figure 4.

drawing of skin incision, with expected position of the axillary nerve (letter A)
Reduction technique of the fracture-dislocation
The literature on LPFDS rarely mentions the opportunity to attempt a closed reduction; with this attempt being unsuccessful in the cases reported (10, 12). We do not recommend trying this manoeuvre. First of all, because a locked posterior humeral head is virtually impossible to mobilize and relocate only by traction and rotation and then there is the high risk of further damage to the dislocated epiphysis.
The first surgical step in LPFDS is to disengage the humeral head from the posterior margin of the glenoid. Every attempt has to be made to avoid any further injury to the joint surface and to the vascularization of the epiphysis.
Even if some authors describe an easy reduction only by pushing the humeral head with their fingers in a postero-anterior direction (21), in practical experience this manoeuvre is rarely (or exceptionally) successful. In our cases, we could not get the reduction only with our fingers because of the strong lock of the head between the bone and the swollen posterior capsule, muscles and soft tissues.
The use of a sharp or a smooth Hohmann retractor, placed just posteriorly to the humeral head and pushed anteriorly acting as a lever, is an option as a reduction tool (12); this procedure needs gentle handling of the soft tissues behind the dislocated humeral head because there is high risk of further damage to the muscles of the rotator cuff (infraspinatus and teres minor) and to the posterior capsule. In our series, we did only one attempt with a smooth Hohmann in the first case but it failed therefore we decided to abandon this step in the subsequent cases.
The metaphysis and the humeral shaft need to be mobilised laterally and distally, to give space to allow the reduction of the humeral head. Then, the humeral head has to be gently pushed in place after a slight external rotation to disengage it from the border of the glenoid. We obtained this with the use of two Shantz pins acting as joysticks (Fig. 5); one in the head and one in the shaft of the humerus. This technique was also described by Sadaat through a deltopectoral approach with the use of only the pin in the head (22). There is the risk of perforation of the articular surface with the head Shantz screw but the damage caused by the tip of the pin is deemed insignificant.
Figure 5.
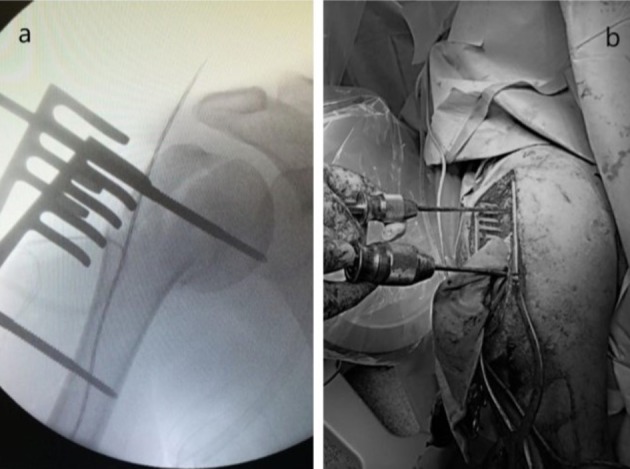
Reduction technique with Shantz pins (a- fluoro imaging; b- clinical picture)
Once the head is relocated, the reduction to the humerus can be done with clamps (Weber or similar) (Fig. 6) and provisionally secured with Kirschner wire. In case of fracture of the tuberosities, they can be loaded on suture or can be directly reduced and fixed with K wires too, as in a simple fracture of the proximal humerus.
Figure 6.

Provisional reduction with a Weber clamp
Osteosynthesis
In the first reports, the fixation consisted only of single compression screws directed from the lateral wall of the humerus or from the tuberosities toward the humeral head (20). This osteosynthesis requests a post-operative period of immobilization, with consequent risk of articular stiffness, and has also revealed many failures due to lack of resistance to pull-out. A stronger construct can be obtained with a formal internal fixation with plate and screws.
Traditional plates have been used for several years in proximal humerus, demonstrating good results. Their use in osteoporotic bone and in comminuted fractures has revealed the limits of traditional plates (24). Angular stability has completely changed the approach to many fractures, especially in the meta-epiphyseal ones (Fig. 7). Over the past decade, locking plates have been shown to be biomechanically superior to standard non-locking plates in terms of stability and resistance to pull-out, both in normal and in osteoporotic bone (25, 26). The design of the proximal locking plate has progressively changed and improved during the years, especially the direction of the epiphyseal screws. With the proximal screws, the humeral head can be fully filled by hardware.
Figure 7.

Final picture of internal fixation with a locking plate via a trans-deltoid lateral approach with isolation of the axillary nerve
In previous literature, other hardware for fixation of LPFDS such as proximal humeral nails have not been mentioned.
Replacement arthroplasty, widely used in chronic LPFDS, is an option even in acute lesions, especially if 50% or more of the articular surface is affected (27). On the other hand, as mentioned before, the fair results of substitution in these injuries has led to a more conservative attitude when deemed feasible. The Authors’ opinion is that arthroplasty can be a salvage option in cases of failure of the osteosynthesis (avascular necrosis, degenerative arthritis or non-union).
The operation should be conducted as soon as possible; it does not mean that this lesion has to be operated in an emergency/urgency setting but our preference goes to operate within 24-48 hours. With this strategy, the shoulder is not already too swollen and the reduction can be easier, without muscle contracture. Obviously, this is better for the patient, avoiding discomfort and prolonged use of painkillers.
Post-operative treatment and rehabilitation
It is well known that, after surgical treatment of a proximal humeral fracture, the key point is the early start of movement and rehabilitation to avoid capsular contracture and consequent shoulder stiffness. A passive range of movements with a therapist, auto-assisted or with mechanical devices is encouraged from the very early post-operative period, as tolerated by the pain. The assumption of early rehabilitation is based on an adequate analgesic therapy, i.v. or i.m. the first days and per os after hospital discharge. Paracetamol or opioids are preferred to nsaids for better tolerance and less side effects.
An active range of movements can be started 3 weeks after the operation, after the so called fibrous callus have formed. In cases of involvement of the tuberosities, active movement can be delayed to the 4th or the 5th week after surgery.
For our patients, passive rehabilitation started 24-48 hours after surgery. A sling was prescribed only for patient comfort. Self-assisted exercises of pendulum and oscillations of the shoulder and active flexion and extension of the elbow were shown and immediately begun after drain removal. The addition of other exercises, self-assisted by the healthy arm, were encouraged 2-3 times a day and assisted kinesiotherapy was prescribed. After 3 weeks the patients were allowed to start gentle active movements, under the supervision of a rehabilitation therapist.
Conclusions
LPFDS is a rare entity and the literature reports only a small series of cases.
There is a high risk of overlooking this injury but some radiologic signs can pose strong suspicions of this lesion. Surgical treatment is recommended, with open reduction and internal fixation preferred in acute cases. Many approaches and reduction manoeuvres have been described in medical literature without gaining definitive agreement on the surgical strategies to be taken.
The encouraging results of our series led us to strongly recommend the lateral approach and the reduction steps as described. First of all thanks to the relative simplicity of them and then because these techniques are very respectful to the biology of the proximal humerus.
Finally, as fixation with a locked plate in proximal humerus is gaining more and more agreement, it has to be considered the gold standard in LPFDS.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Claro R, Sousa R, Massada M, et al. Bilateral posterior fracture-dislocation of the shoulder: report of two cases. Int J Shoulder Surg. 2009;3:41–5. doi: 10.4103/0973-6042.57935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ivkovic A, Boric I , Cicak N. One-stage operation for locked bilateral posterior dislocation of the shoulder. J Bone Joint Surg Br. 2007;89:825–8. doi: 10.1302/0301-620X.89B6.18842. [DOI] [PubMed] [Google Scholar]
- 3.Robinson CM, Aderinto J. Posterior shoulder dislocations and fracture dislocations. J Bone Joint Surg Am. 2005;87:639–50. doi: 10.2106/JBJS.D.02371. [DOI] [PubMed] [Google Scholar]
- 4.Basal O, Dincer R, Turk B. Locked posterior dislocation of the shoulder: A systematic review. EFORT Open Rev. 2018 Jan 15;3(1):15–23. doi: 10.1302/2058-5241.3.160089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Altan E, Senaran H, Acar MA, et al. Mozaicplasty technique for treatment of reverse Hill-Sachs lesion. Tech Shoulder Elbow Surg. 2013;14:1–4. [Google Scholar]
- 6.Shams A, El-Sayed M, Gamal O, et al. Modified technique for reconstructing reverse Hill-Sachs lesion in locked chronic posterior shoulder dislocation. Eur J Orthop Surg Traumatol. 2016;26:843–849. doi: 10.1007/s00590-016-1825-4. [DOI] [PubMed] [Google Scholar]
- 7.Neer CS. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–89. [PubMed] [Google Scholar]
- 8.Neer CS. Displaced proximal humeral fractures. II. Treatment of three-part and four-part displacement. J Bone Joint Surg Am. 1970;52:1090–103. [PubMed] [Google Scholar]
- 9.Sheehan SE, Gaviola G, Sacks A, et al. Traumatic shoulder injuries: a force mechanism analysis of complex injuries to the shoulder girdle and proximal humerus. AJR Am J Roentgenol. 2013;201:W409–W424. doi: 10.2214/AJR.12.9987. [DOI] [PubMed] [Google Scholar]
- 10.Robinson CM, Akhtar A, Mitchell M, et al. Complex posterior fracture-dislocation of the shoulder. Epidemiology, injury patterns, and results of operative treatment. J Bone Joint Surg Am. 2007;89(7):1454–66. doi: 10.2106/JBJS.F.01214. [DOI] [PubMed] [Google Scholar]
- 11.Kokkalis ZT, Iliopoulos ID, Antoniou G, et al. Posterior shoulder fracture dislocation: an update with treatment algorithm. Eur J Orthop Surg Traumatol. 2017;27:285–294. doi: 10.1007/s00590-016-1840-5. [DOI] [PubMed] [Google Scholar]
- 12.Gokkus K, Sagtas E, Kara H, et al. Posterior Shoulder Dislocation Associated With the Head (Splitting) and Humeral Neck Fracture: Impact of Understanding Radiologic Signs and Experience With an Extended Deltopectoral Approach. Tech Hand Up Extrem Surg. 2018 Jun;22(2):57–64. doi: 10.1097/BTH.0000000000000190. [DOI] [PubMed] [Google Scholar]
- 13.Chesser TJ, Langdon IJ, Ogilvie C, et al. Fractures involving splitting of the humeral head. J Bone Joint Surg Br. 2001;83:423–426. doi: 10.1302/0301-620x.83b3.11218. [DOI] [PubMed] [Google Scholar]
- 14.Kokkalis ZT, Mavrogenis AF, Ballas EG, et al. Modified McLaughlin technique for neglected locked posterior dislocation of the shoulder. Orthopedics. 2013;36:e912–e916. doi: 10.3928/01477447-20130624-22. [DOI] [PubMed] [Google Scholar]
- 15.Martinez AA, Navarro E, Iglesias D, et al. Long-term follow-up of allograft reconstruction of segmental defects of the humeral head associated with posterior dislocation of the shoulder. Injury. 2013;44:488–491. doi: 10.1016/j.injury.2012.10.027. [DOI] [PubMed] [Google Scholar]
- 16.Hawkins RJ, Switlyk P. Acute prosthetic replacement for severe fractures of the proximal humerus. Clin Orthop Relat Res. 1993;289:156–60. [PubMed] [Google Scholar]
- 17.Wijgman AJ, Roolker W, Patt TW, et al. Open reduction and internal fixation of three and four-part fractures of the proximal part of the humerus. J Bone Joint Surg Am. 2002;84:1919–25. [PubMed] [Google Scholar]
- 18.Boileau P, Krishnan SG, Tinsi L, et al. Tuberosity malposition and migration: reasons for poor outcomes after hemiarthroplasty for displaced fractures of the proximal humerus. J Shoulder Elbow Surg. 2002;11:401–12. doi: 10.1067/mse.2002.124527. [DOI] [PubMed] [Google Scholar]
- 19.Kralinger F, Schwaiger R, Wambacher M, et al. Outcome after primary hemiarthroplasty for fracture of the head of the humerus. A retrospective multicentre study of 167 patients. J Bone Joint Surg Br. 2004;86:217–9. doi: 10.1302/0301-620x.86b2.14553. [DOI] [PubMed] [Google Scholar]
- 20.Stableforth PG, Sarangi PP. Posterior fracture-dislocation of the shoulder. A superior subacromial approach for open reduction. J Bone Joint Surg Br. 1992 Jul;74(4):579–84. doi: 10.1302/0301-620X.74B4.1624520. [DOI] [PubMed] [Google Scholar]
- 21.Fiorentino G, Cepparulo R, Lunini E, et al. A Posterior shoulder fracture-dislocation: double approach treatment. Our experience. Acta Biomed. 2016 13;87(2):184–90. [PubMed] [Google Scholar]
- 22.Waqar S, Puneet M. Open Reduction and Internal Fixation of Posterior Fracture Dislocation of the Shoulder Made Easy! J Orthop Case Rep. 2017;7(6):24–26. doi: 10.13107/jocr.2250-0685.934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shin YH, Lee YH, Choi HS, et al. A modified deltoid splitting approach with axillary nerve bundle mobilization for proximal humeral fracture fixation. Injury. 2017;48:2569–257. doi: 10.1016/j.injury.2017.09.007. [DOI] [PubMed] [Google Scholar]
- 24.Laux CJ, Grubhofer F, Werner CML, et al. Current concepts in locking plate fixation of proximal humerus fractures. J Orthop Surg Res. 2017 25;12(1):137. doi: 10.1186/s13018-017-0639-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jabran A, Peach C, Zou Z, et al. Biomechanical comparison of screw-based zoning of PHILOS and Fx proximal humerus plates. BMC Musculoskelet Disord. 2018 Jul 25;19(1):253. doi: 10.1186/s12891-018-2185-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gavaskar AS, Karthik BB, Tummala NC, et al. Second generation locked plating for complex proximal humerus fractures in very elderly patients. Injury. 2016;47(11):2534–2538. doi: 10.1016/j.injury.2016.08.010. [DOI] [PubMed] [Google Scholar]
- 27.Cheng SL, Mackay MB, Richards RR. Treatment of locked posterior fracture dislocations of the shoulder by total shoulder arthroplasty. J Shoulder Elbow Surg. 1997;6:11–17. doi: 10.1016/s1058-2746(97)90065-3. [DOI] [PubMed] [Google Scholar]


