Abstract
Distal femur fractures account for 4-6% of osteoporosis related fractures of the femur in the elderly population. They represent a relevant cause of morbidity and mortality in the geriatric population with a reported 1-year mortality reaching 30%. Non-displaced fractures or even displaced fractures in patients with high operative risk can be treated conservatively. However, operative treatment is the most widely accepted management option for displaced fractures. The advantage resides in early mobilization and weight-bearing, reducing risks related with a prolonged immobilization when compared with conservative treatment. On the other hand, the intrinsic difficulty of fixing an osteoporotic bone is a major concern. The presence of osteosynthesis devices or prosthetic implants in the femur can make the surgical treatment more challenging, sometimes limiting therapeutic options. Aim of the present paper is to review the most recent literature about osteoporotic distal femur fractures in the elderly, including periprosthetic and other hardware related fractures, to highlight current evidence on management options and related results as a guide for the daily clinical practice. (www.actabiomedica.it)
Keywords: distal femur, fractures, elderly, osteoporotic
Introduction
Distal femur fractures account for 4-6% of fragility fractures of the femur, with an overall annual incidence of 4,5/100.000 in the general population (1). About 50% of these fractures affect patients over 70 years of age, being a relevant cause of morbidity and mortality in the geriatric population. A 6-months mortality rate of 16% is indeed reported, rising to 30% at 1 year. The presence of a total knee arthroplasty and of severe comorbidities is also related with increasing mortality rates in some literature reports (2-4).
Alike fractures of the proximal femur, early surgical intervention (within 48 h) of distal femur fractures is related with a decrease in mortality rates in the elderly population and allows to reduce complications rate associated with prolonged immobilization (1, 2, 5).
Most fragility fractures of the distal femur are due to low-energy trauma in patients with osteopenia or osteoporosis, predominantly women. The most common mechanism of injury is a direct axial load or, less frequently, the consequence of torsional or rotational forces applied to the lower limb (6, 7).
The fracture is predominantly located at the distal metaphysis of the femur and the most typical deformity is represented by shortening associated with extension and varus deviation of the distal segment. Distal femur fractures in the elderly are frequently comminuted and very distally located. Interestingly, Hill et al. reported the presence of a coronal plane fracture (Hoffa fragment) in 44% of a cohort of patients over 65 years of age who sustained a supracondylar femur fracture, as a result of low energy trauma in most cases. The same authors reported a 66% incidence of Hoffa fractures in a younger cohort who sustained high energy trauma. Distribution was also reported to be different, with elderly patients having lateral condyle coronal fractures more frequently compared with younger patients. As reported by the authors, these percentages are higher than previously reported and should be considered relevant as a missed Hoffa fracture could lead to early fracture displacement and fixation failure (8).
Unlike the young adult population, the associated vascular and neurological lesions are rare in these cases, being usually the fracture a consequence of low-energy trauma in elderly patients (6).
A subgroup of distal femoral fractures is represented by periprosthetic knee fractures. They have a prevalence of 0.5%-2.2% after primary total knee arthroplasty and 1.6-38% after revision total knee arthroplasty, increasing proportionally with age (particularly over 80 years) and with the increasing number of implanted prostheses (9-11, 12).
Management of these fractures is challenging and requires advanced skills in both trauma and prosthetic revision surgery.
Classifications
The classification most commonly used for distal femur fractures is the AO-OTA classification (33 - femur) which divides them in extra-articular fractures (type A), partial articular fractures (type B) and articular fractures (type C).
For periprosthetic fractures of the distal femur, the most commonly used classification is that of Rorabeck and Taylor (13), which takes into account the extent of fracture displacement and prosthesis stability (stable or mobilized), dividing fractures in 3 groups: nondisplaced fracture with stable prosthesis (type 1), fracture with displacement greater than 5 mm or angulation greater than 5° with stable prosthesis (type 2), and any supracondylar fracture with loosened prosthesis (type 3).
However, Rorabeck and Taylor do not consider in their classification the distance of fracture line from the prosthetic implant, that is an important factor for the choice of surgical technique (9).
Conversely, Backstein et al. have proposed a classification that takes into account the extension of distal fracture segment, stability of the prosthetic implant and bone quality, with the aim to distinguish between periprosthetic fractures that can be treated with osteosynthesis (extension of the distal fragment sufficient for the insertion of locking screws, stable prosthesis, good bone quality), from those that require a revision of the implant (distal fragment not sufficiently extended for locking screws insertion, loosened prosthesis) (14).
Treatment
The treatment of distal femur fractures in the elderly can be conservative or operative depending on fracture morphology and patients’ characteristics. Simple, nondisplaced and extra-articular fractures can be successfully treated conservatively with plaster casts or braces. More complex fractures may be treated conservatively as well in patients with increased operative risks or with very low functional demands, especially non-ambulatory patients. However, the risks related to a prolonged immobilization and related complication must be weighed carefully with benefits of conservative treatment in these cases.
Nonetheless, operative treatment remains the main indication for most displaced and intra-articular fractures, with the aim to restore length, alignment and rotation, as well as restoring articular congruence of intra-articular fractures.
Various surgical options exist for treating distal femur fractures. Closed, minimally invasive or open reduction and internal fixation with a nail or a plate are the most commonly used techniques (5, 6, 15).
Some authors have proposed acute knee prosthetic replacement to treat distal femur fractures in elderly patients. However, evidence on indications and outcome is lacking at present (16).
Technical difficulties associated with fragility fractures osteosynthesis are related to structural and mechanical alterations that characterize the osteoporotic bone (Figure 1). The imbalance between resorption and formation of bone tissue leads to thinning and increased porosity of the cortical bone, as well as density reduction of the cancellous bone that reduces its mechanical resistance. The outcome of surgical treatment depends on various factors that includes patient’s characteristics, fracture type and the respect of soft tissues which allows preserving the biology of bone healing.
Figure 1.
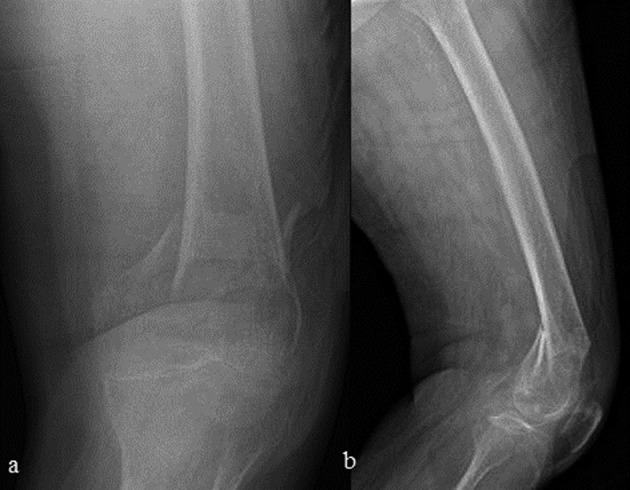
AP (a) and lateral (b) radiographs of a distal femur fragility fracture in a 90 years old woman with severe osteoporosis
From a biomechanical point of view technical difficulties arise from metaphyseal comminution, presence of small articular fragments and the risk to create a too rigid or unstable construct that reduces screws grip in the osteoporotic bone with the risk of implant failure (17).
Another aspect to take into account is the presence of osteosynthesis devices or prosthetic implants (hip or knee prosthesis) that is not infrequent in distal femur fractures in elderly patients. Nonetheless, Loosen et al. reported the presence of preexisting implants in 58% of geriatric patients reporting a distal femur fracture (18). This eventuality complicates the surgical treatment, sometimes limiting therapeutic options. In these cases, for displaced fractures in patients in clinical conditions that allow surgical treatment, proper planning is essential to avoid the formation of stress raisers between the implants, which increases the risk of further fractures (19) (Figure 2).
Figure 2.
Stress riser related fracture a) 82 years-old woman treated with a too short locking plate for periprosthetic knee fracture and a previously implanted trochanteric nail, b) stress raiser related fracture between the implants as a consequence of low energy trauma
Intramedullary nail osteosynthesis
Intramedullary nail osteosynthesis is predominantly indicated for AO / OTA type A fractures, provided a sufficient extent of intact distal femur for housing distal locking screws. Indication might be extended to nondisplaced or minimally displaced intra-articular fractures associated to meta-diaphyseal fractures (AO / OTA type C1- C2) provided stable preliminary fixation of articular fragments with screws, which might not be easily reached in osteoporotic bone. The advantages of this technique reside in the possibility of closed reduction, minimally invasiveness that allows to respect fracture’s biology and early weight bearing. Intramedullary nail osteosynthesis is not practicable in the presence of hip femoral stem and some types of knee prosthesis, as well as if the medullary canal is obstructed by osteosynthesis devices such as nails or screws.
Retrograde nail is nowadays the mostly used osteosynthesis device for treating distal femoral fractures. Compared to antegrade osteosynthesis, retrograde nails allow for an easier intraoperative control on small distal fragments and facilitates reduction if the correct entry point is respected. Moreover, modern retrograde nails have designs that offer multiple options for distal locking which determine its preferential use in clinical practice. The major concern in distal femur fractures is distal anchorage. Data from biomechanical studies suggest that distal locking patterns have a significant influence on the mechanical stability of the bone-implant construct and on the mode of failure in fragility fractures. In osteoporotic bone, distal fixed angle locking constructs show a mean load to failure 38% greater compared with conventional locking technique. The presence of a condyle washer in the distal locking screw increases further the mean load to failure of 30% compared with conventional fixed angle locking technique when two anchoring distal screws are used (20).
Retrograde nails with a three-plane configuration of distal interlocking anchorage provides enhanced torsional and axial stability in osteoporotic bone, compared with other distal anchorage systems (21).
In the literature, concern has been issued regarding possible articular surface and posterior cruciate ligament’s lesions due to retrograde nail insertion into the femoral groove. In elderly patients, limited iatrogenic damage to the articular surface may be tolerated considering the advantages resulting from limited surgical exposure required for nailing. On the other hand, despite the possible anatomical variability and the unavoidable entry point through the articular cartilage, a safe entry portal can be found anterior to the posterior cruciate ligament insertion and slightly medial to center of the intercondylar groove (22).
Retrograde nail osteosynthesis is also commonly used for treating periprosthetic knee fractures, as many modern prosthetic designs have an open femoral box that allows passing through of the nail (5, 15, 19, 23).
Antegrade nail osteosynthesis is currently used for treating distal femoral fractures in few cases. To allow its use, the fracture line must be located at least 5 cm proximal to the articular surface with most nail designs and at least 3 cm from the most proximal distal locking screw to allow adequate fixation. To maximize fixation stability, driving the nail tip as distally as possible is paramount, ideally just above the Blumensaat line (5, 15). Antegrade nails with multiplanar and angular stable interlocking options have the advantage of obtaining very high stability in the distal fragment, providing the possibility of nailing fractures close to the joint (24, 25).
Plate osteosynthesis
Plate osteosynthesis is indicated for all distal femur fractures types (AO / OTA type A, B and C). In literature, the possibility of using various devices for treating distal femoral fractures in elderly patients, such as conventional compression plates, fixed angle devices and the DCP system (Dinamic Condylar Screw, Synthes, CH) is reported. However, modern trends head towards the use of plates and screws with locking technology, especially in osteoporotic fractures due to the increased pull out resistance. The fixation technique with conventional plate relies on contact at the bone-plate interface to create stability, causing compression damage to the periosteum or the need for extensive periosteal stripping which negatively affects bone vascularization. Moreover, compression of an osteoporotic fracture might be difficult because of comminution and bone brittleness at the fracture site.
Latest generation of plate technology relies on the locking of screws on the plate holes to create a stable construct. The advantage of this system is that plates behave like an internal fixator, reducing periosteal damage and therefore optimizing the biological conditions for fracture healing. Modern plates allow the simultaneous use of angular stability screws (monoaxial or polyaxial depending on the implants used) and cortical screws, maximizing both systems advantages (5-6).
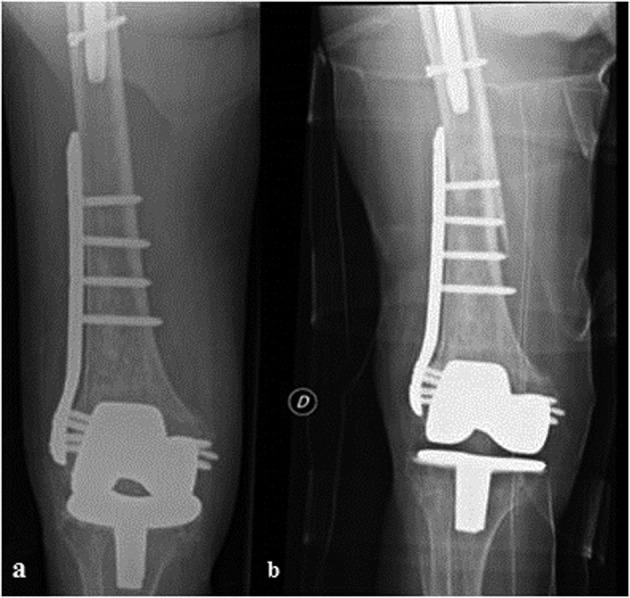
The main advantage of osteosynthesis with plate lies in the versatility that allows its use in almost any fracture configuration, especially in presence of hip prosthesis and some types of knee prosthesis, or in the presence of osteosynthesis devices that obstruct the femoral medullary canal, where nail fixation is not feasible (Figure 3).
Figure 3.

a) 79 years-old woman reporting a distal femur fragility fracture between a total knee arthroplasty and a previously implanted antegrade intramedullary nail b) radiographic control 2 years after open reduction and internal fixation with a locking plate stabilized with screws and cerclages (reprinted with permission from “Canton G. et al., Acta Biomed. 2017 Jun 7;88(2S):118-128. doi: 10.23750/abm.v88i2 -S.6522”).
Moreover, it can be performed through a minimally invasive approach (MIPO technique) for simple extra-articular fractures that can be reduced with external maneuvers (19).
Conversely, in displaced articular fractures, osteosynthesis is carried out with a standard lateral open approach since an accurate reduction of fragments is imperative. Alternatively, it is possible to use a minimally invasive approach for proximal fixation combined with an open distal epiphyseal approach.
The main pitfall in locking plate osteosynthesis of distal femur fractures in osteoporotic bone is the risk of creating a too stiff construct that negatively influences the bone healing process. Multiple factors influence the mechanical strength or stiffness of a distal femoral locking plate construct. Bone quality and the fracture’s pattern represent non-modifiable factors, but many others can be modulated under the surgeon’s control. Some of these modifiable factors include quality of reduction, screws type, screws configuration, the length and position of the plate and the working length of the construct (26, 27).
Although without a solid evidence from literature and without definite indications for clinical practice, some authors suggest the use of combined cortical and locking screws for proximal fragment fixation, to avoid the risk of both fixation failure (all cortical screws) and of excessive stiffness leading to nonunion or implant breakage (all locking screws) (26-28).
Treatment of knee periprosthetic distal femur fractures
Periprosthetic distal femoral fractures are difficult to treat and require advanced skills in trauma and prosthetic surgery.
The goal of treatment is to get both fracture healing and a stable knee without residual malalignment to avoid prosthetic implant failure. Treatment choice depends on the stability of the femoral component, fracture type, patient clinical condition and eventual associated presence of other implants in the proximal femur (Figure 3).
As for other osteoporotic distal femur fractures, conservative treatment with plaster casts or braces is indicated for nondisplaced fractures or for patients not eligible for surgery.
Osteosynthesis can be performed with a stable prosthetic femoral component. Retrograde nail osteosynthesis is possible for most femoral prosthetic designs provided a femoral box wide enough for nail passing through. Moreover, an adequate bone stock and sufficient distal fragment extension for placing distal locking screws is paramount, with differences from non-periprosthetic fractures given by the femoral component encumbrance and possible bone loss from stress shielding. (29) Plate osteosynthesis can be used to treat very distal fractures or in the presence of proximal osteosynthesis / prosthetic components requiring for proximal fixation with monocortical screws and/or cerclages. In these cases, plate/stem or plate/nail overlapping is fundamental to avoid fractures between implants, with some authors suggesting a minimum overlap of 6 screw holes or twice the outer cortical diameter of the diaphyseal femur (30). Prosthetic implant revision is indicated in very distal and comminuted fractures in which an adequate fixation is not feasible, as well as in presence of a loosened femoral component. In these cases, implant revision with a stemmed femoral component allows for stable fixation, early mobilization of the patient and early weight-bearing. If an inadequate metaphyseal bone-stock is present, the use of constrained prostheses with or without grafts may be necessary (9, 10, 31, 32).
Complications and outcomes
Main complications related to osteosynthesis of distal femur fractures reported in literature are non-unions, infections and osteosynthesis failure.
Non-union is the most common cause of re-operation in distal femur fractures (33). Many factors increase the risk of non-union, related to patient characteristics, fracture type and osteosynthesis method. Some factors are not modifiable by the surgeon, as smoking, diabetes, vascular diseases (causing a decrease in bone blood supply), advanced age, obesity, chronic use of NSAIDS or corticosteroids and tumors (which adversely affect patients’ immune response). In a retrospective case-control study, Rodriguez et al. found a significant association between non-union and stainless-steel plates compared to titanium implants due to stiffness (34).
In literature, nonunion rates up to 35% are reported in studies performed at trauma centers mostly dealing with high-energy trauma (35). In fact, non-unions of distal femur fractures occur most frequently after high-energy trauma, in open fractures with huge comminution and in case of segmental bone loss (36). According to Ebraheim et al. non-unions occur more frequently when a metaphyseal comminution fracture pattern is present (37).
In a retrospective cohort study conducted by Moloney et al., the nonunion rate resulted to be higher in the 60-74 years old group than in the over 75 years old group (38). Nonetheless, according to Wenger et al., elderly patients treated with lateral locking plates suffer from nonunion less frequently compared to younger patients as a consequence of the lower trauma energy that is rarely related to severe soft tissues damage compromising fracture biology (35).
However, Moloney et al found in their study early complications after surgical treatment of distal femur fractures to be more frequent in the elderly population, with a 37,5% incidence of patients having at least one early post-operative complication such as respiratory/urinary tract infections or cardiac problems (38).
Kammerlander et al. found a significant reduction of mobility after distal femur fracture in geriatric population, with 23% of the population of the study (46 patient- mean age 80+/-9.3) being totally homebound, 26% unable to conduct any social activity and only 18% capable of social activities without assistance (7).
Interestingly, the importance of ensuring a mechanically stable construct allowing prompt rehabilitation with early motion in order to avoid bed-rest syndrome must be balanced with the higher failure rate of internal fixation in geriatric patients that are usually unable to adhere to partial weight-bearing protocols (39).
Athar et al. in a retrospective study of 78 patients (mean age 80-48% over 85) with distal femur fracture reported knee stiffness as the most common complication, although establishing if the stiffness was pre - existing or due to injury or treatment was impossible in most cases (2).
For distal femur fractures treated with total knee replacement, a 1-year mortality rate of 20%, a periprosthetic fracture risk of 2,4% and a 1-year revision rate of 3,4% are reported (16).
In a review of periprosthetic knee fractures internal fixation by Herrera et al., a nonunion rate of 9%, an implant failure rate of 4%, an infection rate of 3% and a reoperation rate of 13% are reported, without differences in outcomes between osteosynthesis with retrograde nail and locking plate (40).
Complications related with revision total knee arthroplasty for managing periprosthetic fractures do not differ from those faced during other revision knee procedures. However, treatment for periprosthetic fractures is frequently more challenging because of older age, comorbidities and often poor bone stock. These factors can raise the risk of perioperative complications. In the literature, fourteen percent of patients are reported to experience a medical complication postoperatively and 16% of patients are reported to suffer from a surgical complication requiring revision within the first 3 years postoperatively (41).
Conclusions
Distal femur fractures are severe injuries burdened by high rates of complications and mortality in the elderly. Allowing early mobilization is essential to prevent complications occurring in bedridden elderly patients. Early surgery can significantly reduce mortality and complications rates. Surgical treatment is frequently challenging as a consequence of osteoporotic bone characteristics and the frequent presence of osteosynthesis devices or hip/knee prosthesis which may limit available treatment options. Periprosthetic knee fractures represent a particularly challenging subtype of distal femur fractures, requiring advanced skills in both trauma and prosthetic surgery.
Ethical approval:
“All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.”
Informed consent:
“Informed consent was obtained from all individual participants included in the study.”
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Myers P, Laboe P, Johnson KJ, Fredericks PD, Crichlow RJ, Maar DC, et al. Patient Mortality in Geriatric Distal Femur Fractures. J Orthop Trauma. 2018 Mar;32(3):111–115. doi: 10.1097/BOT.0000000000001078. [DOI] [PubMed] [Google Scholar]
- 2.Athar SM, Fazal MA, Hassan M, Ashwood N. Distal Femoral Fractures in the Elderly: Does Early Treatment with Locking Plates Reduce Mortality Rates. Clin Res Open Access. 2017;3(1) [Google Scholar]
- 3.Streubel PN, Ricci WM, Wong A, Gardner MJ. Mortality After Distal Femur Fractures in Elderly Patients. Clin Orthop Relat Res. 2011 Apr;469(4):1188–1196. doi: 10.1007/s11999-010-1530-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jordan RW, Chahal GS, Davies M, Srinivas K. A Comparison of Mortality following Distal Femoral Fractures and Hip Fractures in an Elderly Population. Adv Orthop Surg. vol. 2014 Article ID 873785, 4 pages, 2014. https://doi.org/10.1155/2014/873785 . [Google Scholar]
- 5.Ehlinger M, Ducrot G, Adam P, Bonnomet F. Distal femur fractures. Surgical techniques and a review of the literature. Orthop Traumatol Surg Res. 2013 May;99(3:3):53–60. doi: 10.1016/j.otsr.2012.10.014. [DOI] [PubMed] [Google Scholar]
- 6.Link BC, Babst R. Current concepts in fractures of the distal femur. Acta Chir Orthop Traumatol Cech. 2012;79(1):11–20. [PubMed] [Google Scholar]
- 7.Kammerlander C, Riedmüller P, Gosch M, Zegg M, Kammerlander-Knauer U, Schmid R, et al. Functional outcome and mortality in geriatric distal femoral fractures. Injury. 2012;43(7):1096–1101. doi: 10.1016/j.injury.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 8.Hill BW, Cannada LK. Hoffa Fragments in the Geriatric Distal Femur Fracture: Myth or Reality. Geriatr Orthop Surg Rehabil. 2017;8(4):252–255. doi: 10.1177/2151458517744076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnston AT, Tsiridis E, Eyres KS, Toms AD. Periprosthetic fractures in the distal femur following total knee replacement: A review and guide to management. Knee. 2012 Jun;19(3):156–62. doi: 10.1016/j.knee.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 10.Nauth A, Ristevski B, Bégué T, Schemitsch EH. Periprosthetic distal femur fractures: current concepts. J Orthop Trauma. 2011 Jun;25(Suppl 2):S82–5. doi: 10.1097/BOT.0b013e31821b8a09. [DOI] [PubMed] [Google Scholar]
- 11.Whitehouse MR, Mehendale S. Periprosthetic fractures around the knee: current concepts and advances in management. Curr Rev Musculoskelet Med. 2014;7(2):136–144. doi: 10.1007/s12178-014-9216-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singh JA, Jensen M, Lewallen D. Predictors of periprosthetic fracture after total knee replacement: an analysis of 21,723 cases. Acta Orthop. 2013;84(2):170–177. doi: 10.3109/17453674.2013.788436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rorabeck CH, Taylor JW. Classification of periprosthetic fractures complicating total knee arthroplasty. Orthop Clin North Am. 1999;30:209–214. doi: 10.1016/s0030-5898(05)70075-4. [DOI] [PubMed] [Google Scholar]
- 14.Backstein D, Safir O, Gross A. Periprosthetic fractures of the knee. J Arthroplasty. 2007;22(4 Suppl 1):45–9. doi: 10.1016/j.arth.2006.12.054. [DOI] [PubMed] [Google Scholar]
- 15.Obakponovwe O, Kallala R, Stavrou PZ, Harwood P, Giannoudis P. The management of distal femoral fractures: a literature review. Orthop Trauma. June 2012;26(3):176–183. [Google Scholar]
- 16.Senthilkumaran S, MacDonald DRW, Rankin I, Stevenson I. Total knee arthroplasty for distal femoral fractures in osteoporotic bone: a systematic literature review. Eur J Trauma Emerg Surg. 2019 Feb 28 doi: 10.1007/s00068-019-01103-7. [DOI] [PubMed] [Google Scholar]
- 17.Yaacobi E, Sanchez D, Maniar H, Horwitz DS. Surgical treatment of osteoporotic fractures: An update on the principles of management. Injury. 2017 Dec;48(Suppl 7):S34–S40. doi: 10.1016/j.injury.2017.08.036. [DOI] [PubMed] [Google Scholar]
- 18.Loosen A, Fritz Y, Dietrich M. Surgical Treatment of Distal Femur Fractures in Geriatric Patients. Geriatr Orthop Surg Rehabil. 2019;10 doi: 10.1177/2151459319860723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Piétu G, Ehlinger M. Minimally invasive internal fixation of distal femur fractures. Orthop Traumatol Surg Res. 2017 Feb;103(1S):S161–S169. doi: 10.1016/j.otsr.2016.06.025. [DOI] [PubMed] [Google Scholar]
- 20.Paller DJ, Frenzen SW, Bartlett CS 3rd, Beardsley CL, Beynnon BD. A three-dimensional comparison of intramedullary nail constructs for osteopenic supracondylar femur fractures. J Orthop Trauma. 2013. February;27(2):93–9. doi: 10.1097/BOT.0b013e31825199c9. [DOI] [PubMed] [Google Scholar]
- 21.Wähnert D, Hoffmeier K, Fröber R, Hofmann GO, Mückley T. Distal femur fractures of the elderly—different treatment options in a biomechanical comparison. Injury. 2011;42(7):655–659. doi: 10.1016/j.injury.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 22.Carmack DB, Moed BR, Kingston C, Zmurko M, Watson JT, Richardson M. Identification of the optimal intercondylar starting point for retrograde nailing: an anatomic study. J. Trauma. 2003;55:692–695. doi: 10.1097/01.TA.0000088857.47194.7E. [DOI] [PubMed] [Google Scholar]
- 23.Thompson SM, Lindisfarne EAO, Bradley N, Solan M. Periprosthetic Supracondylar Femoral Fractures Above a Total Knee Replacement: Compatibility Guide for Fixation With a Retrograde Intramedullary Nail. J. Arthroplasty. August 2014;29(8):1639–1641. doi: 10.1016/j.arth.2013.07.027. [DOI] [PubMed] [Google Scholar]
- 24.Kulkarni SG, Varshneya A, Kulkarni GS, Kulkarni MG, Kulkarni VS, Kulkarni RM. Antegrade Interlocking Nailing for Distal Femoral Fractures. J Orthop Surg. Apr. 2012:48–54. doi: 10.1177/230949901202000110. [DOI] [PubMed] [Google Scholar]
- 25.Rommens PM, Küchle R, Hofmann A, Hessmann MH. Intramedullary Nailing of Metaphyseal Fractures of the Lower Extremity. Acta Chir Orthop Traumatol Cech. 2017;84(5):330–340. [PubMed] [Google Scholar]
- 26.Kandemir U. Distal femur: dynamization of plating. Injury. 2018 Jun;49(Suppl 1):S44–S48. doi: 10.1016/S0020-1383(18)30302-4. [DOI] [PubMed] [Google Scholar]
- 27.Harvin WH, Oladeji LO, Della Rocca GJ, Murtha YM, Volgas DA, Stannard JP, et al. Working length and proximal screw constructs in plate osteosynthesis of distal femur fractures. Injury. 2017 Nov;48(11):2597–2601. doi: 10.1016/j.injury.2017.08.064. [DOI] [PubMed] [Google Scholar]
- 28.Park KC, Lim SJ, Song YS, Hwang KT. Factors affecting peri-implant fracture following locking plate for osteoporotic distal femur fractures. Orthop Traumatol Surg Res. 2017 Dec;103(8):1201–1204. doi: 10.1016/j.otsr.2017.08.008. [DOI] [PubMed] [Google Scholar]
- 29.Mau-Moeller A, Behrens M, Felser S, Bruhn S, Mittelmeier W, Bader R, et al. Modulation and Predictors of Periprosthetic Bone Mineral Density following Total Knee Arthroplasty. Biomed Res Int. 2015;2015:418168. doi: 10.1155/2015/418168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kubiak EN, Haller JM, Kemper DD, Presson AP, Higgins TF, Horwitz DS. Does the lateral plate need to overlap the stem to mitigate stress concentration when treating Vancouver C periprosthetic supracondylar femur fracture. J Arthroplasty. 2015 Jan;30(1):104–8. doi: 10.1016/j.arth.2014.07.021. [DOI] [PubMed] [Google Scholar]
- 31.McGraw P, Kumar A. Periprosthetic fractures of the femur after total knee arthroplasty. J Orthop Traumatol. 2010;11(3):135–141. doi: 10.1007/s10195-010-0099-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Canton G, Ratti C, Fattori R, Hoxhaj B, Murena L. Periprosthetic knee fractures. A review of epidemiology, risk factors, diagnosis, management and outcome. Acta Biomed. 2017 Jun 7;88(2S):118–128. doi: 10.23750/abm.v88i2-S.6522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Koso RE, Terhoeve C, Steen RG, Zura R. Healing, nonunion, and re-operation after internal fixation of diaphyseal and distal femoral fractures: a systematic review and meta-analysis. Int Orthop. 2018 Nov;42(11):2675–2683. doi: 10.1007/s00264-018-3864-4. [DOI] [PubMed] [Google Scholar]
- 34.Rodriguez EK, Boulton C, Weaver MJ, Herder LM, Morgan JH, Chacko AT, et al. Predictive factors of distal femoral fracture nonunion after lateral locked plating: A retrospective multicenter case-control study of 283 fractures. Injury. 2014 Mar;45(3):554–9. doi: 10.1016/j.injury.2013.10.042. [DOI] [PubMed] [Google Scholar]
- 35.Wenger D, Andersson S. Low risk of nonunion with lateral locked plating of distal femoral fractures - A retrospective study of 191 consecutive patients. Injury. 2019 Feb;50(2):448–452. doi: 10.1016/j.injury.2018.10.039. [DOI] [PubMed] [Google Scholar]
- 36.Gardner MJ, Toro-Arbelaez JB, Harrison M, Hierholzer C, Lorich DG, Helfet DL. Open Reduction and Internal Fixation of Distal Femoral Nonunions: Long-Term Functional Outcomes Following a Treatment Protocol. J Trauma. 2008 Feb;64(2):434–8. doi: 10.1097/01.ta.0000245974.46709.2e. [DOI] [PubMed] [Google Scholar]
- 37.Ebraheim NA, Martin A, Sochacki KR, Liu J. Nonunion of Distal Femoral Fractures: a Systematic Review. Orthop Surg. 2013;5:46–50. doi: 10.1111/os.12017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moloney GB, Pan T, Van Eck CF, Patel D, Tarkin I. Geriatric distal femur fracture: Are we underestimating the rate of local and systemic complications. Injury. August 2016;47(8):1732–1736. doi: 10.1016/j.injury.2016.05.024. [DOI] [PubMed] [Google Scholar]
- 39.von Rüden C, Augat P. Failure of fracture fixation in osteoporotic bone. Injury. June 2016;47(2):S3–S10. doi: 10.1016/S0020-1383(16)47002-6. [DOI] [PubMed] [Google Scholar]
- 40.Herrera DA, Kregor PJ, Cole PA, Levy BA, Jönsson A, Zlowodzki M. Treatment of acute distal femur fractures above a total knee arthroplasty: systematic review of 415 cases (1981-2006) Acta Orthop. 2008;79:22–7. doi: 10.1080/17453670710014716. [DOI] [PubMed] [Google Scholar]
- 41.Kuzyk PRT, Watts E, Backstein D. Revision Total Knee Arthroplasty for the Management of Periprosthetic Fractures. J Am Acad Orthop Surg. 2017 Sep;25(9):624–633. doi: 10.5435/JAAOS-D-15-00680. [DOI] [PubMed] [Google Scholar]


