Abstract
Background and aim of the work: Suprapatellar synovial plica is caused by a congenital thickening of the synovial membrane and is generally asymptomatic. In the literature, suprapatellar plicae are described as one of the causes of anterior knee pain however, their real role in determining symptoms is controversial. The aim of the current paper is to describe the anatomy, classifications, pathophysiology, symptoms and management of suprapatellar plica syndrome, as well as the differential diagnosis from other causes of anterior knee pain. Method: Via a search within the MEDLINE/PubMed database, a current review was conducted, and the results summarized. Results: Due to idiopathic, traumatic or inflammatory conditions, plicae can become pathological, causing anterior knee pain with possible knee clicking, swelling, giving way and locking after prolonged flexion of the knee. The diagnosis should be formulated based on an accurate medical history and clinical examination, followed by an appropriate imaging study. However, arthroscopy remains the “golden standard” for detecting all synovial plica. Conclusions: In patients with anterior knee pain, where doubt is present in the imaging investigation for intraarticular or periarticular lesions, pathological suprapatellar synovial plica must be suspected. The treatment should initially be conservative, but in cases where symptoms persist, patients should undergo arthroscopy to confirm diagnosis and to determine a suitable treatment. In the presence of pathological plica associated with cartilage damage of the femoral condyle or patella at the time of diagnostic arthroscopy, plicae excision leads to favourable results in a high number of cases. (www.actabiomedica.it)
Keywords: suprapatellar synovial plica, anterior knee pain, plica management, knee arthroscopy, review.
Introduction
Knee synovial plicae are anatomically normal duplications of the synovial membrane and can be classified, based on their location around the knee, as suprapatellar, mediopatellar, lateropatellar or infrapatellar (ligamentum mucosum) (1). The most common is suprapatellar plica, which is reported in 20% to 90% of cases but has little clinical manifestation in comparison with the more frequently studied medial plica, which is reported in 20% to 60% of persons, and where knee symptoms are present in 2% to 9% of cases (2).
The role of suprapatellar synovial plica or plica sinovialis suprapatellaris in determining anterior knee pain is still controversial, because some asymptomatic suprapatellar synovial plica are a normal finding during arthroscopy or cadaveric studies. However, in some conditions, in both children and adults, they can become symptomatic due to idiopathic, traumatic, or inflammatory conditions of the synovial membrane (3). In a meta-analysis including 23 studies, 969 patients underwent surgical treatment for symptomatic synovial plicae; the average age was 25 years and no differences were present between male and female patients (2). Anterior knee pain is reported anteriorly around the patella and can be due to traumatic causes or repetitive micro traumas related to athletic movements, or can be a result of patellofemoral dysplasia, idiopathic chondromalacia of the patella, osteochondritis or synovial folds (4). This pain can originate from various anatomical structures of the knee: subchondral bone, synovial tissue, retinacula, skin, muscle, nerves, tendons or adipose tissue.
The aim of the current paper is to describe the anatomy, classifications, pathophysiology, symptoms and management of suprapatellar plica syndrome, as well as the differential diagnosis from other causes of anterior knee pain.
Anatomy and Pathophysiology
Plicae are remnants synovial structures occurring due to the lack of septa reabsorption that divides the knee into three compartments, the superior, medial and lateral, during embryonic development (2). Suprapatellar synovial plicae is a fold generally located above the proximal pole of the patella. Its location morphology and size can vary, and it can completely or partially separate the suprapatellar bursa from the knee cavity.
In the literature, there are various suprapatellar plica classifications based on embryology, shape, size, location and extension across the suprapatellar bursa (5). The embryological classification reported by Zidorn divides the plicae into four types, based on their embryology and location with respect to the proximal pole of the patella, according to the following pattern.; Type I: a complete septum that separates the suprapatellar bursa and knee cavity, type II: a perforated septum with one or more small central holes, type III: a residuals septum with a remaining fold usually in a medial location; and type IV: a completely involute septum (6). Dandy identified 10 different types according to the septum extension through the suprapatellar bursa and found a complete septum in 4.2%, a perforated septum in 20.6%, a partial septum in 66.4%, and an absence of the septum in 8.8% of cases (7). On the other hand, Kim classified the fold, based on arthroscopic plicae anatomy, as an absent, vestigial, medial, lateral, arch, hole, or complete septum, with each type subdivided further according to size and extension (8). We prefer to use the simpler four type arthroscopic Sakakibara classification as follows. Type A: a complete septum or centrally perforated septum with a small hole and types B, C and D: an arcuate partial septum with medial, lateral and superior prevalence respectively (9).
The role of suprapatellar synovial plicae in determining anterior knee pain is controversial. Suprapatellar synovial plicae is a normal, very frequent finding during arthroscopy, but pathological symptomatic suprapatellar plicae is rarely reported. The complete septum and the centrally perforated septum with a small opening, corresponding to type A in the arthroscopic Sakakibara classification and representing 2% to 11% of all suprapatellar plicae (10), are closely associated with knee symptoms. There are two theories that explain the pathological patterns of plicae: the mechanical theory (11) and Pipkins’s hydraulic theory (12).
The hypertrophic pathological plicae with mechanical impingement against the femoral condyle or the patella, is due to a complete septum (Fig. 1) or to a transformation of a non-pathological plicae via an inflammatory process after idiopathic, traumatic or repetitive micro traumatic events, or to some other conditions that affects the pliability of the knee synovial folds. Trauma in synovial plicae is reported in between 13% and 57% of cases by various authors (2, 3, 10), while symptomatic perforated septum is associated with the hydraulic theory, due to its one-way valvar mechanism with pain and swelling of the knee. (Fig. 2).
Figure 1.
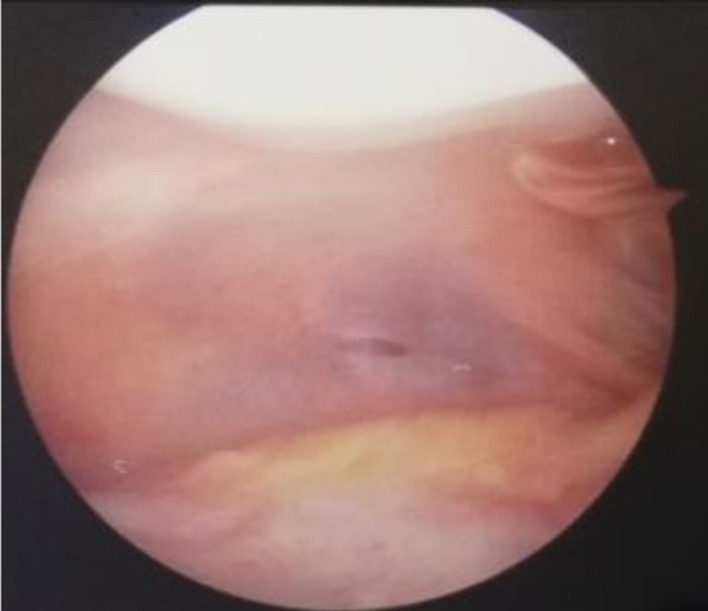
Suprapatellar synovial plica of the complete septum type situated above the superior patella pole
Figure 2.
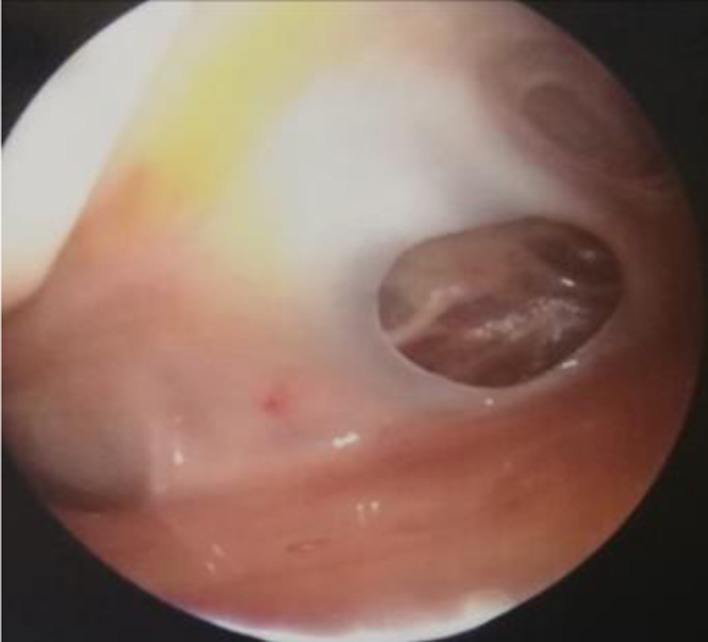
Perforated suprapatellar plicae with central small hole associated with the physiopathological hydraulic mechanism based on Pipkin’s theory
Clinical Presentation and Differential Diagnosis
Anterior pain is the most common symptom of suprapatellar plica, located anterior to the patella above the joint line (4). Other symptoms include swelling, the knee giving way, the presence of a snapping sensation during the flexion movement, and the very important painful knee locking after prolonged knee flexion in a sitting position that we call “cinema sign”. Symptoms must be distinguished from other causes of anterior knee pain.
The difficulties in diagnosing the anterior knee pain and determining the consequent treatment are linked to the non-specificity of the symptoms and signs. In 103 patients with synovial plica syndrome, in the absence of a meniscal tear or cartilage damage in the weight- bearing area, we found that suprapatellar and mediopatellar plicae were associated in 27% of cases. Pathological supra and/or mediopatellar plica were linked in 100% of cases with pain and in 86% of cases with knee locking after prolonged flexion of the knee “cinema sign” (personal communication at the Fourth International Conference of Orthopaedics, Biomechanics and Sports Rehabilitation, Assisi, December 1st-3rd, 2000).
Based on the aetiology, anterior knee pain can have several forms.
- Post-Traumatic
- Acute trauma: contusion, fracture of the patella or femur, dislocations, ruptures of the quadriceps or the patellar tendon.
- Repetitive trauma: patellar tendonitis (jumper’s knee), quadriceps tendonitis, pre-patellar bursitis or apophysitis (Osgood-Schlatter disease or Sinding-Larsen-Johansson syndrome).
- Late effects of trauma: post-traumatic chondromalacia, patellofemoral osteoarthritis, Hoffa’s disease, reflex sympathetic dystrophy of the patella, bone dystrophy of the patella, acquired patella baja or acquired quadriceps fibrosis.
- Patellofemoral Dysplasia
- Excessive lateral patellar pressure syndrome, chronic patellar subluxation, recurrent patellar luxation or, chronic patellar dislocation.
Idiopathic Patellar Chondromalacia.
Osteochondritis Dissecans of the Patella and/or the Femoral Trochlea.
Synovial Plicae: Suprapatellar, Mediopatellar, Lateropatellar or Infrapatellar.
Pathological plicae are not common but must be suspected in all cases of anterior knee pain, especially when pain is associated with knee locking after prolonged flexion. Dupont reported three cases of symptomatic suprapatellar plicae from among 12,000 patients (13).
Appropriate imaging studies include radiography, ultrasound, magnetic resonance imaging (MRI) and computerized tomography (CT) scanning (3, 14). Bilateral knee ultrasound is important for soft- tissue investigation and CT scanning in patellofemoral evaluation is mandatory in cases of dysplasia or high-riding patella. MRI is helpful for highlighting the presence of the synovial fold and for its measurement and the determination of its exact location (15). ( Fig. 3) . Suprapatellar plica is visualized better on a sagittal MRI view, where it appears behind the patella, with a low-signal-bands type of aspect, sometimes delineated by high-signal joint fluid (16, 17). MRI is the examination of choice for investigating plicae, but arthroscopy remains the “golden standard” for detecting all synovial folds (16-18).
Figure 3.
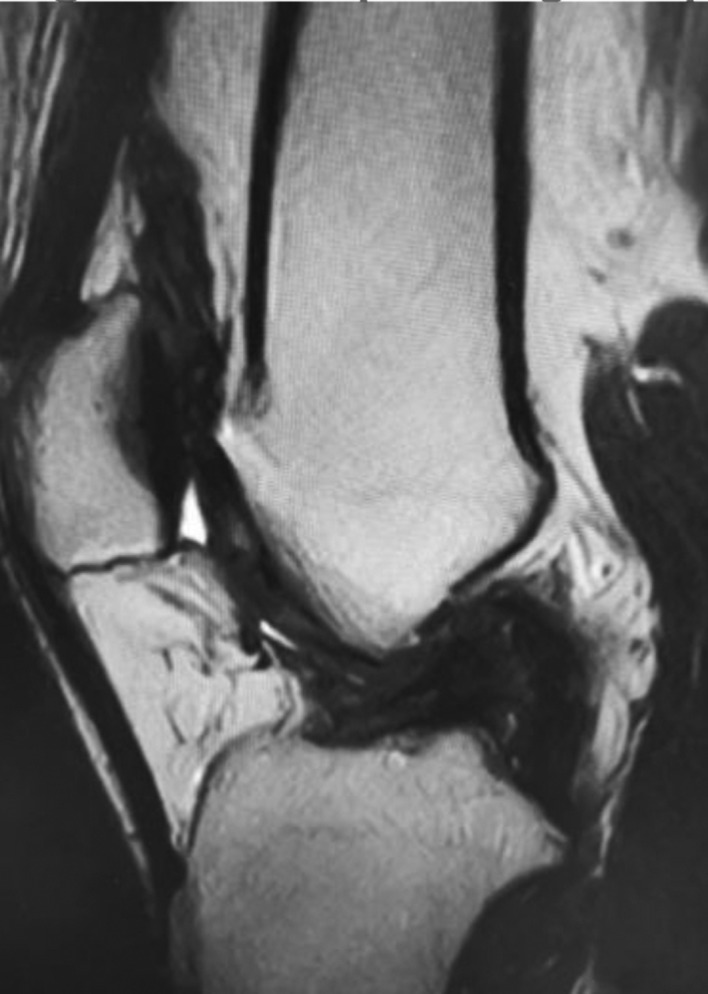
MRI of pathologic suprapatellar synovial plica
Treatment
The treatment of chronic anterior knee pain is initially conservative and includes resting, non-steroidal anti-inflammatory drug consumption, the use of braces and taping, proper athletic training with structured exercises and stretching for the hamstrings, gastrocnemius, and quadriceps, adequate footwear, weight loss, physiotherapy and in some cases, local articular injections (3, 19, 20).
This treatment usually aims at reduction of the pain and the state of inflammation, followed by a rehabilitation program in order to correct the biomechanics of the extensor apparatus. Amatuzzi reported a favourable outcome in 40% of cases after conservative treatment, in patients affected by synovial plica (20). The treatment of chronic anterior knee pain should be based on an accurate medical history and clinical examination, followed by an appropriate imaging investigation (3). In many cases, if conservative therapy fails after three to six months, surgical arthroscopic treatment is required. Pain is the major indication for knee arthroscopy (21-23).
The arthroscopic procedure is important for diagnosis and treatment (24) of all intraarticular lesions, and it can be done under general, spinal or local anaesthesia, but we must take into consideration the fact that plicectomy in local intraarticular anaesthesia is not helpful due to the fluid diffusion in suprapatellar bursa related to the high pressure pump. A tourniquet is not mandatory.
Pathological suprapatellar plica, diagnosed as the cause of knee symptoms, must be excised totally, using and antero-lateral, antero-medial or occasionally supero-lateral approach, leaving a thin synovial edge.
According to Patel, plicae showing thickening, fibrosis and abnormal size, are to be considered pathological (1) (Fig. 4). Strover describes the contact between the suprapatellar plica and the medial femoral condyle, with the plicae trapped between the quadriceps mechanism and the trochlea when the knee is flexed beyond 70°, using the arthroscopic supero-lateral view (25). The complete septum must be perforated with a smooth instrument before being excised. Arthroscopic aspects that guide us to perform plica excision are the shape, size, thickness and fibrosis of the plica. Another element maybe the presence of lesions on the articular cartilage of the non-weight-bearing femoral condyle area and on the patella, with limited synovitis due to plica impingement (26). If there is no other intraarticular lesion, plica of the complete septum type or the perforated septum type, and all synovial folds showing thickening fibrosis and alternate shape, must be removed. However, in the case of other associated intraarticular lesions, such as meniscus tears or cartilage lesions in the weight-bearing area, medical history and preoperative physical examination and investigation must help us to decide whether the plica must be removed or not. Plicae can be removed via basket, motorized shaver or radiofrequency methods. Accurate haemostasis must be performed to avoid postoperative hematoma (27). Patients underwent plica resection are able to resume normal daily activities, and complete recovery is achieved four to six weeks after arthroscopy (23, 25, 26).
Figure 4.
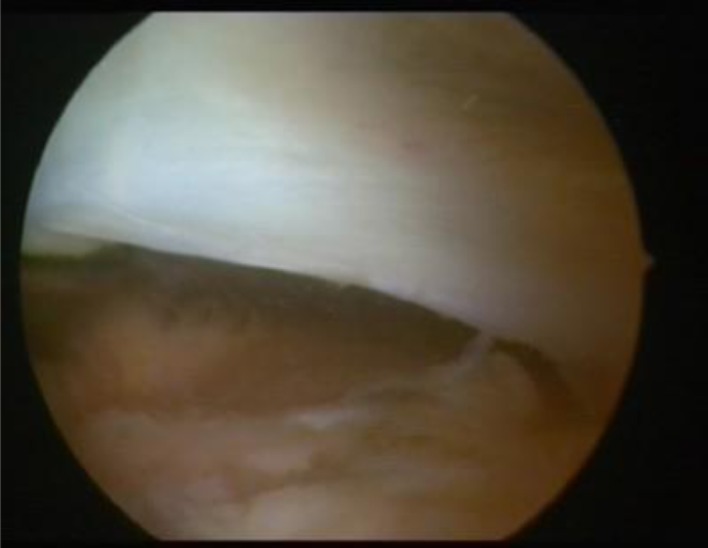
Pathological arcuate type of plica, associated with fibrosis, thickening of the border and abnormal size
The arthroscopic procedure for well-selected patients with plica syndrome results in a successful outcome (2, 3, 10, 17, 18). In fact, in a clinical trial, Johnson et al. reported a more than 80% success rate after arthroscopic plica resection in well-selected patients, and nearly 50% poor results in the control group; these patients were later returned for a definitive arthroscopic plicectomy (10). Kassim and Fulkerson reported a good outcome in 88% of cases at a four year follow-up after arthroscopic pathological plicae resection (28). In Schindler’s meta-analysis, out of 969 patients at a 27-month follow-up, 90% reported a favourable outcome, with 10% failure (2). It was found that a good outcome was associated with younger age and well-localized pain with a short duration of symptom onset. On the other hand, a poor outcome was associated with incorrect diagnosis, the presence of severe chondromalacia, and extensor apparatus malalignment (2, 29, 30).
Conclusion
Anterior knee pain is one of the most frequent symptoms in knee disorders. The treatment is initially conservative. However, patients resistant to conservative therapy must undergo a surgical arthroscopic procedure. Preoperative diagnosis is very important and is closely related to the success of arthroscopic treatment. Diagnosis must be based on medical history, physical examination, and correct instrumental investigation (radiography, ultrasound and MRI). Synovial plicae is very common, but it is generally asymptomatic and of little clinical consequence. However, it must be suspected in every patient with anterior knee pain that is resistant to conservative treatment, especially when pain is associated with knee locking after prolonged flexion. In the presence of pathological plicae with cartilage damage of the femoral condyle or patella at the time of diagnostic arthroscopy, a plicectomy will be performed. In such cases, surgical treatment leads to good results in a high number of patients. Poor results are associated with severe patellar or trochlear chondromalacia or occur as a result of an inappropriate or inaccurate diagnosis. Open surgical treatment is rarely indicated.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Patel D. Arthroscopy of the plicae: synovial folds and their significance. Am J Sports Med. 1978;6:217–225. doi: 10.1177/036354657800600502. [DOI] [PubMed] [Google Scholar]
- 2.Schindler OS. ‘The Sneaky Plica’ revisited: morphology, pathophysiology and treatment of synovial plicae of the knee. Knee Surg Sports Traumatol Arthrosc. 2014;22(2):247–262. doi: 10.1007/s00167-013-2368-4. [DOI] [PubMed] [Google Scholar]
- 3.Zmerly H, Akkawi I, Citarella R, El Ghoch M. Clinical Management of Medial Patellar Plica Syndrome: Expert Point of View from Diagnosis to Treatment. Curr Rheumatol Rev. 2018 doi: 10.2174/1573397115666181123182633. [DOI] [PubMed] [Google Scholar]
- 4.Patel D. Plica as a cause of anterior knee pain. Orthop Clin North Am. 1986;17:273–7. [PubMed] [Google Scholar]
- 5.Akao M, Ikemoto T, Takata T, Kitamoto K, Deie M. Suprapatellar plica classification and suprapatellar plica syndrome. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2019;17:10–15. doi: 10.1016/j.asmart.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zidorn T. Classification of the suprapatellar septum considering ontogenetic development. Arthroscopy. 1992;8(4):459–464. doi: 10.1016/0749-8063(92)90008-y. [DOI] [PubMed] [Google Scholar]
- 7.Dandy DJ. Anatomy of the medial suprapatellar plica and medial synovial shelf. Arthroscopy. 1990;6(2):79–85. doi: 10.1016/0749-8063(90)90002-u. [DOI] [PubMed] [Google Scholar]
- 8.Kim SJ, Choe WS. Arthroscopic findings of the synovial plicae of the knee. Arthroscopy. 1997;13(1):33–41. doi: 10.1016/s0749-8063(97)90207-3. [DOI] [PubMed] [Google Scholar]
- 9.Sakakibara J. Arthroscopic study on Iino’s band (plica synovialis mediopatellaris) J Jap Orthop Assoc. 1974;50:513–7. [Google Scholar]
- 10.Johnson DP, Eastwood DM, Witherow PJ. Symptomatic synovial plicae of the knee. J Bone Joint Surg Am. 1993;75(10):1485–1496. doi: 10.2106/00004623-199310000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Tindel NL, Nisonson B. The plica syndrome. Orthop Clin North Am. 1992;23(4):613–618. [PubMed] [Google Scholar]
- 12.Pipkin G. Lesions of the suprapatellar plica. J Bone Joint Surg [Am] 1950;32:363–9. [PubMed] [Google Scholar]
- 13.Dupont JY. Synovial plicae of the knee. Controversies and review. Clin Sports Med. 1997;16(1):87–122. doi: 10.1016/s0278-5919(05)70009-0. [DOI] [PubMed] [Google Scholar]
- 14.Vassiou K, Vlychou M, Zibis A, Nikolopoulou A, Fezoulidis I, Arvanitis D. Synovial plicae of the knee joint: the role of advanced MRI. Postgrad Med J. 2015;91(1071):35–40. doi: 10.1136/postgradmedj-2013-132176. [DOI] [PubMed] [Google Scholar]
- 15.Kang S, Park J, Kang SB, Chang CB. MRI findings of young male soldiers with atraumatic anterior knee pain. Scand J Med Sci Sports. 2016;26(5):572–578. doi: 10.1111/sms.12486. [DOI] [PubMed] [Google Scholar]
- 16.Liu YW, Skalski MR, Patel DB, White EA, Tomasian A, Matcuk GR., Jr The anterior knee: normal variants, common pathologies, and diagnostic pitfalls on MRI. Skeletal Radiol. 2018;47(8):1069–1086. doi: 10.1007/s00256-018-2928-2. [DOI] [PubMed] [Google Scholar]
- 17.Lee PYF, Nixion A, Chandratreya A, Murray JM. Synovial Plica Syndrome of the Knee: A Commonly Overlooked Cause of Anterior Knee Pain. Surg J. 2017;3(1):e9–e16. doi: 10.1055/s-0037-1598047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sanchis-Alfonso V, Dye SF. How to Deal With Anterior Knee Pain in the Active Young Patient. Sports Health. 2017 Jul/Aug;9(4):346–351. doi: 10.1177/1941738116681269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Erickson BJ, Campbell K, Cvetanovich GL, Harris JD, Bach BR, Jr, Sherman SL. Nonligamentous Soft Tissue Pathology About the Knee: A Review. Orthopedics. 2016;39(1):32–42. doi: 10.3928/01477447-20151218-06. [DOI] [PubMed] [Google Scholar]
- 20.Amatuzzi MM, Fazzi A, Varella MH. Pathologic synovial plica of the knee. Results of conservative treatment. Am J Sports Med. 1990;18:466–469. doi: 10.1177/036354659001800503. [DOI] [PubMed] [Google Scholar]
- 21.Al-Hadithy N, Gikas P, Mahapatra AM, Dowd G. Review article: Plica syndrome of the knee. J Orthop Surg (Hong Kong) 2011 Dec;19(3):354–8. doi: 10.1177/230949901101900319. [DOI] [PubMed] [Google Scholar]
- 22.Dandy DJ. Arthroscopy in the treatment of young patients with anterior knee pain. Orthop Clin North Am. 1986;17(2):221–229. [PubMed] [Google Scholar]
- 23.Geraghty RM, Spear M. Evidence for plical support of the patella. J Anat. 2017;231(5):698–707. doi: 10.1111/joa.12662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Adachi N, Ochi M, Uchio Y, Kawasaki K, Yamasaki K. The complete type of suprapatellar plica in a professional baseball pitcher: consideration of a cause of anterior knee pain. Arthroscopy. 2004;20(9):987–991. doi: 10.1016/j.arthro.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 25.Strover AE, Rouholamin E, Guirguis N, Behdad H. An arthroscopic technique of demonstrating the pathomechanics of the suprapatellar plica. Arthroscopy. 1991;7(3):308–310. doi: 10.1016/0749-8063(91)90133-i. [DOI] [PubMed] [Google Scholar]
- 26.Mine T, Chagawa K, Ihara K, Kawamura H, Kuriyama R, Date R. The Role of Complete Suprapatellar Plicae. Arthrosc Tech. 2016;5(1):e197–e199. doi: 10.1016/j.eats.2015.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kramer DE, Kalish LA, Abola MV, Kramer EM, Yen YM, Kocher MS, Micheli LJ. The effects of medial synovial plica excision with and without lateral retinacular release on adolescents with anterior knee pain. J Child Orthop. 2016;10(2):155–62. doi: 10.1007/s11832-016-0724-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kasim N, Fulkerson JP. Resection of clinically localized segments of painful retinaculum in the treatment of selected patients with anterior knee pain. Am J Sports Med. 2000 Nov-Dec;28(6):811–4. doi: 10.1177/03635465000280060801. [DOI] [PubMed] [Google Scholar]
- 29.Patel DR, Villalobos A. Evaluation and management of knee pain in young athletes: overuse injuries of the knee. Transl Pediatr. 2017 Jul;6(3):190–198. doi: 10.21037/tp.2017.04.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Iliadis AD, Jaiswal PK, Khan W, Johnstone D. The operative management of patella malalignment. Open Orthop J. 2012;6:327–39. doi: 10.2174/1874325001206010327. [DOI] [PMC free article] [PubMed] [Google Scholar]


