Abstract
Purpose: To demonstrate the advantages of CT-guided biopsy of subdiaphragmatic small renal nodule with the coaxial technique using MPR images. Methods: The study included retrospectively 12 patients who underwent CT-guided biopsy with 18 G needle of subdiaphragmatic small renal nodule (<15 mm) suspected. Histology reports have been the reference standard. Results: The histology was diagnostic in 12 biopsies (100%): out of 10 neoplastic nodule (83.3%), 8 were malignant (80%) and 2 were benign (20%); 2 out of 12 were non-neoplastic (16.6%). No procedural complications were observed (0%). Conclusions: By using MPR images there is an effective improvement during coaxial CT-guided biopsy of subdiaphragmatic small renal nodule difficult to reach and to reduce the complication as pneumothorax. (www.actabiomedica.it)
Keywords: small renal nodule, CT-guided biopsy, MPR images, coaxial technique
Introduction
Diagnostic imaging is very important in the detection of tumors in the histological characterization through imaging-guided biopsies (1, 2).
At present, percutaneous CT-guided Biopsy is a highly diagnostic and minimally invasive procedure, and it is often possible to avoid removing tissue to be examined surgically thanks to the support of imaging (3, 4).
The Multiplanar Reconstructions (MPR) technique during CT-Guided Biopsy, can significantly increase the number of lesions which can be biopsied percutaneously thus reducing the need of surgical techniques (2, 5-6).
MPR images are helpful in the pre-operative assessment of the most useful course of the needles that are used for biopsies of thoracic, abdominal and retroperitoneal lesions (7-10).
The renal lesion located at the subdiaphragmatic space is difficult to reach with a traditional coaxial Ct-guided biopsy, without having a pass through the lung, with the risk of pneumothorax.
Both ultrasound (US) and multi-detector computed tomography (MDCT) are used as guide for biopsy procedures; while US allows the real-time evaluation of the course of the needle and is not associated to ionizing radiations (11-14), MDCT is helpful in the detection of small lesions that are located in anatomic sites difficult to evaluate with US (15-16).
There is no study that analyzes the positive contribution of MPR images to CT-guided biopsy for small renal lesion (<15 mm) difficult to reach, in particular renal lesion located into the subdiaphragmatic space.
The aim of this study was to demonstrate the advantages of CT-guided biopsy of subdiaphragmatic small renal nodule with the coaxial technique using MPR images, which are impossible to reach with conventional non-surgical biopsy techniques.
Materials and methods
Patient population
We retrospectively included in our study 12 patients (7 males, 5 females; age ranging from 52 to 68 years) that underwent CT-guided biopsy for small renal lesions (size of the lesion between 9 and 14.8 mm) in the period from May 2017 to February 2018. The indication to the CT-guided biopsy was represented by a nodule that could not be biopsied through ultrasound or axial CT scans, for his difficult position.
We have excluded patients with a known tumor history, pediatric patients and those with bleeding diathesis.
CT-guided Biopsy Technique
The patients’ informed consent was obtained in all cases.
The procedures were all performed with a 64-detector helical scanner (Optima CT540, GE Healthcare, USA), without the administration of contrast media; the following technical parameters were used: 100 kV, 100 mAs, 2 mm collimation, 2.5 slice thickness with 1 mm of reconstruction increment. The multi-planar reformatted images were obtained through a dedicated software of a post-processing workstation (AW Server, GE Healthcare, USA). All patients were biopsied with a coaxial technique, using MPR images (Fig. 1).
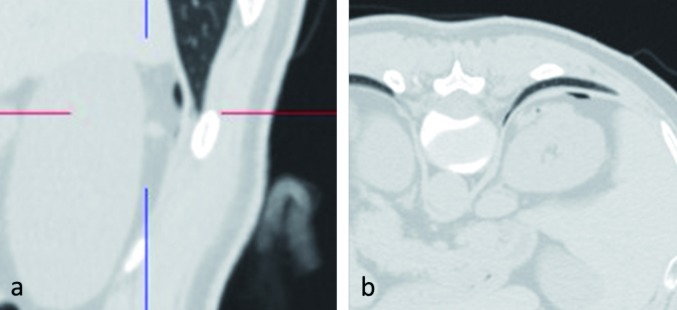
Figure 1.
a-c. 62 years old male with renal nodule (arrow) located at the upper lobe, very difficult to achieve with a traditional coaxial biopsy, without having to pass through the lung with the risk of having a pneumothorax. CT-guided biopsy in three different scanning planes, with coaxial technique with MPR images (a-c), with needle-track in the subdiaphragmatic space
The extemporaneous microscopic evaluation of the biopsy’s samples to be analyzed has been evaluated by our laboratory.
One experienced radiologist with 7 years of experience in CT-guided biopsies performed the procedures.
The patients were placed on the CT bed in various positions depending on the site of the lesion that should be biopsied.
The first step was the acquisition of the axial scans, followed by the multi-planar reconstruction in order to decide the most adequate trajectory of the 14-Gauge needle (Cook Medical, Bloomington, USA).
Once the stylet of the guide was removed, a second needle was introduced, namely a 16-Gauge needle.
A second CT scan and the respective MPR images allowed evaluating if the needle was in the correct position and if position was adequate the biopsy sample was taken.
To exclude any procedure-related complication, a third scan was obtained after the needle was removed; the patients were kept under clinical observation for 4 hours after the biopsy in order to exclude major complications.
The histologic report was used as reference standard for assessing the accuracy of the procedure.
Statistical Analysis
The overall diagnostic accuracy of CT-guided biopsy of renal small lesions was calculated as: true positive (TP) + true negative (TN)/TP+TN+ false positive (FP) + false negative (FN) (17).
Results
Twelve CT-guided biopsy with coaxial technique and MPR images were performed (Table 1) (Fig. 1, 2).
Table 1.
Bioptical diagnosis after CT-guided coaxial biopsy with MPR technique (n: number of cases)
| n (%) | n (%) | ||
| Renal Tumor | 10 (83.3) | Renal Cell Carcinoma | 8 (66.6) |
| Oncocytoma | 2 (16.6) | ||
| Angiomyolipoma | 2 (16.6) |
Figure 2.
a-c. 57 years old male with renal nodule located at the upper lobe. CT-guided biopsy in three different scanning planes, with coaxial technique with MPR images (a-c), with needle-track in the subdiaphragmatic space
All the target lesions subjected to biopsy were all located at the upper renal level.
In all cases, the CT-guided biopsy technique coaxial with MPR images enabled us to detect the tip of the needle within the target lesion (100%).
The biological material was considered to be suitable for biopsy study, with a diagnostic value, in 12 biopsies (100%); we did not have inadequate sample.
Among these, 10 out of 12 (83.3%) were found to be neoplasms (Table 1), of which:
- 8 were malignant primary renal lesions (66.6%);
- 2 were oncocytoma (16.6%);
Two out 12 (16.6%) were Angiomyolipoma (Table 1).
The overall diagnostic accuracy of the method was 100%.
Procedural complications did not occur in any of the 12 cases (0%) (Fig. 3).
Figure 3.
Control after Ct-guided biopsy: the needle track has been subdiaphragmatic without the onset of a pneumothorax
Discussion
The MPR images allowed collecting biological samples useful for a diagnosis through CT-guided biopsies with coaxial technique in 100% of cases (Figs. 1, 2); the diagnosis of renal small lesions was obtained in 100% of the cases, without the need to perform a surgical biopsy.
In case of small renal lesions as our population, unreachable through US, CT-guided biopsy represents the best option to obtain tissue samples (2, 15-16); moreover by using reformatted images it is possible to biopsy lesions that cannot be reached with axial CT images alone (7-10).
Our study population presented renal small lesions (<15 mm) suspected of malignancy in previous radiological imaging; all the nodules were located at the subdiaphragmatic level, very difficult to achieve with a traditional coaxial biopsy, without having to pass through the lung with the risk of having a pneumothorax (Fig. 3) (17-20).
With the MPR images we have found the best and safest needle trajectory (6, 18-21).
To our knowledge, studies concerning the effectiveness of the coaxial technique using MPR images for CT-guided biopsies for small renal lesion, located in a difficult area like the subdiaphragmatic region, have not yet been carried out.
Our study suggests that the advancement of CT-guided coaxial biopsy technique in small renal lesions can be successfully performed thanks to this addiction to MPR methods, having the possibility to reduce the complication, in particularly the pneumothorax, and to find the best needle trajectory.
Our study presents a certain amount of limitations; the study was retrospectively and the number of cases was small.
This is explained by the exclusion of all those lesions in which it was possible to perform a biopsy with simple coaxial technique without using MPR reconstructions, such as the lesion located at the mid and lower renal pole and with the exclusion of lesions above 15 mm.
In conclusion by using MPR images there is an effective improvement during coaxial CT-guided biopsy of subdiaphragmatic small renal nodule difficult to reach and to reduce the complication, as pneumothorax.
The paper was performed as the Declaration of Helsinki: ethical principles for medical research involving human subjects.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Mehdi G, Maheshwari V, Afzal S, Ansari HA, Ahmad I. Image-guided fine-needle aspiration of retroperitoneal masses: the role of cytopathologist. J Cytol. 2013;30(1):36–41. doi: 10.4103/0970-9371.107511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Filippo, Saba L, Azzali E, Milanese G, Mostardi M, Borgia D, et al. CT-guided fine-needle aspiration of abdominal and retroperitoneal small lesions with the coaxial technique using MPR images. Acta Biomed. 2016 Jul 28;87(Suppl 3):57–62. [PubMed] [Google Scholar]
- 3.Guo Z, Kurtycz DF, De Las Casas LE, Hoerl HD. Radiologically guided percutaneous fine-needle aspiration biopsy of pelvic and retroperitoneal masses: a retrospective study of 68 cases. Diagn Cytophathol. 2001;25(1):43–49. doi: 10.1002/dc.2000. [DOI] [PubMed] [Google Scholar]
- 4.Gupta S. New techniques in image-guided percutaneous biopsy. CardioVasc Interv Radiol. 2004;27(2):91–104. doi: 10.1007/s00270-003-0056-3. [DOI] [PubMed] [Google Scholar]
- 5.De Filippo M, Onniboni M, Rusca M, Carbognani P, Ferrari L, Guazzi A, et al. Advantages of multidetector-row CT with multiplanar reformation in guiding percutaneous lung biopsies. Radiol Med. 2008 Oct;113(7):945–953. doi: 10.1007/s11547-008-0325-y. [DOI] [PubMed] [Google Scholar]
- 6.De Filippo, Saba L, Rossi E, Nizzoli R, Tiseo M, Pedrazzi G, et al. Curved Needles in CT-Guided Fine Needle Biopsies of Abdominal and Retroperitoneal Small Lesions. Cardiovasc Intervent Radiol. 2015 Dec;38(6):1611–1616. doi: 10.1007/s00270-015-1107-2. [DOI] [PubMed] [Google Scholar]
- 7.Bandoh S, Fujita J, Tojo Y, Yokomise H, Satoh K, Kobayashi S, et al. Diagnostic accurancy and safety of flexible bronchoscopy with multiplanar reconstruction images and ultrafast Papanicolaou stain: evaluating solitary pulmonary nodules. Chest. 2003;124:1985–1992. doi: 10.1378/chest.124.5.1985. [DOI] [PubMed] [Google Scholar]
- 8.Kimura T, Naka N, Minato Y, Inoue Y, Kimura T, Mawatari H, et al. Oblique approach of computed tomography guided needle biopsy using multiplanar reconstruction image by multi detector-row CT in lung cancer. Eur J Radiol. 2004;52(2):206–211. doi: 10.1016/j.ejrad.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 9.Seager M, Patel U, Anderson C, Gonsalves M. Image-guided biopsy of small (≤4 cm) renal masses: the effect of size and anatomical location on biopsy success rate and complications. Br J Radiol. 2018 Feb 13:20170666. doi: 10.1259/bjr.20170666. doi: 10.1259/bjr.20170666. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuriyama T, Masago K, Okada Y, Katakami N. Computed tomography-guided lung biopsy: Association between biopsy needle angle and pneumothorax development. Mol Clin Oncol. 2018 Feb;8(2):336–341. doi: 10.3892/mco.2017.1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Porter B, Karp W, Forsberg L. Percutaneous cytodiagnosis of abdominal masses by ultrasound guided fine needle aspiration biopsy. Acta Radiol Diagn (Stockh) 1981;22(6):663–668. doi: 10.1177/028418518102200607. [DOI] [PubMed] [Google Scholar]
- 12.Juul N, Torp-Pedersen S, Holm HH. Ultrasonically guided fine-needle aspiration biopsy of retroperitoneal mass lesions. Br J Radiol. 1984;57(673):43–46. doi: 10.1259/0007-1285-57-673-43. [DOI] [PubMed] [Google Scholar]
- 13.Memel DS, Dodd GD, Esola CC. Efficacy of sonography as guidance tecnique for biopsy of abdominal, pelvic, and retroperitoneal lymphnodes. AJR Am J Roentgenol. 1996;167(4):957–962. doi: 10.2214/ajr.167.4.8819394. [DOI] [PubMed] [Google Scholar]
- 14.Hoare D, Evans H, Richards H, Samji R. Evaluating the role for renal biopsy in T1 and T2 renal masses: A single-centre study. Can Urol Assoc J. 2018 Feb 6 doi: 10.5489/cuaj.4831. doi: 10.5489/cuaj.4831. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stattaus J, Kalkmann J, Kuehl H, Metz KA, Nowrousian MR, Forsting M, et al. Diagnostic yield of computed tomography-guided coaxial core biopsy of undetermined masses in the free retroperitoneal space: single-center experience. Cardiovasc Intervent Radiol. 2008;31(5):919–925. doi: 10.1007/s00270-008-9317-5. [DOI] [PubMed] [Google Scholar]
- 16.Welch TJ, Sheedy PF, Johnson CD, Johnson CM, Stephens DH. CT-guided biopsy: prospective analysis of 1,000 procedures. Radiology. 1989;171(2):493–496. doi: 10.1148/radiology.171.2.2704815. [DOI] [PubMed] [Google Scholar]
- 17.Patrick M. Bossuyt, Johannes B. Reitsma, David E. Bruns, et al. Towards Complete and Accurate Reporting of Studies of Diagnostic Accuracy: The STARD Initiative. Radiology. 2003;226:24–28. doi: 10.1148/radiol.2261021292. [DOI] [PubMed] [Google Scholar]
- 18.Pérez Montilla ME, Lombardo Galera S, Espejo Herrero JJ, Sastoque JM, Zurera Tendero L. Diagnostic performance of imaging-guided core needle biopsy of the mesentery and peritoneum. Radiologia. 2018 Jan 21 doi: 10.1016/j.rx.2017.12.003. pii: S0033-8338(17) 30218-7. doi: 10.1016/j.rx.2017.12.003. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 19.De Filippo M, Saba L, Silva M, Zagaria R, Concari G, Nizzoli R, et al. Predictive factors of diagnostic accuracy of CT-guided transthoracic fine-needle aspiration for solid noncalcified, subsolid and mixed pulmonary, nodules. Radiol Med. 2013 Oct;118(7):1071–1081. doi: 10.1007/s11547-013-0965-4. [DOI] [PubMed] [Google Scholar]
- 20.Bertolini L, Vaglio A, Bignardi L, Buzio C, De Filippo M, Palmisano A, et al. Subclinical interstitial lung abnormalities in stable renal allograft recipients in the era of modern immunosuppression. Transplant Proc. 2011 Sep;43(7):2617–2623. doi: 10.1016/j.transproceed.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 21.Gafà G, Sverzellati N, Bonati E, Chetta A, Franco F, Rabaiotti E, et al. Follow-up in pulmonary sarcoidosis: comparison between HRCT and pulmonary function tests. Radiol Med. 2012 Sep;117(6):968–978. doi: 10.1007/s11547-012-0827-5. [DOI] [PubMed] [Google Scholar]