Abstract
Uterine leiomyomas are benign tumors that develop from smooth muscle tissue and are present in up to 77% of women in menacme. They are often asymptomatic but can cause pelvic pain, compression, abnormal uterine bleeding, and degeneration. We present the first case report of a perimenopausal woman who exhibited complete and spontaneous expulsion of uterine fibroids without embolization or use of medication. She complained of a mass extruding from the vaginal orifice associated with bleeding and pain for a couple of hours. The anatomopathological findings showed a myomatous lesion. Complete expulsion of a uterine fibroid is a rare condition that may be associated with profuse hemorrhage and can pose a risk to the patient. When it occurs during perimenopause, it can mimic several clinical conditions. Therefore, gynecologists must remain alert to make the correct diagnosis and treatment.
Keywords: Uterine fibroid spontaneous expulsion, degeneration, pre-menopausal
Introduction
Myoma is a frequent benign muscle tumor found in the uterus. It has a multifactorial etiology and occurs during reproductive period.1 It is one of the major causes of morbidity in women. The main symptoms related to uterine fibroids are menstrual changes and pelvic organ compression.2 The fibroids can be classified as submucosal, intramural, subserosal, and cervical.1 The submucosal myomas grow in the myometrium and project toward the endometrial cavity. Further if they are attached to a pedicle, in some cases they can project into the cervical canal and appears on the vagina.1,3
Case report
A 48-year-old, mixed-ethnicity woman arrived at our Unit with a complaint of a mass extruding from the vaginal orifice that was associated with bleeding and pain for a couple hour. The patient had brought the mass in a container. She denied any history of menstrual delay as well as use of medications. A previous ultrasound had revealed an endometrial nodule with a vascular pedicle measuring 20 × 12 cm2, suggestive of a polyp or submucous myoma. At the time of admission, the patient appeared calm without severe pain, but with abdominal tenderness. Speculum examination showed a closed cervix with a moderate amount of bleeding. The uterus was of a fibroelastic consistency and tender on examination. After the examination of the patient, the team dissected the extruded structure, thinking that it was a clot; however, it was found to be very hard. It was a long mass that was difficult to diagnose (Figure 1).
Figure 1.

Eliminated degenerative fibroid with the exact shape of the endometrial cavity.
Therefore, we subjected it to anatomopathological analysis which indicated that it was a myomatous lesion measuring 3.4 × 1.7 × 1.0 cm3. Microscopy revealed well-delimited nodular formation, formed by multidirectional bundles of spindle cells, and oval nuclei without atypia. It was diagnosed as a leiomyoma (Figure 2).
Figure 2.
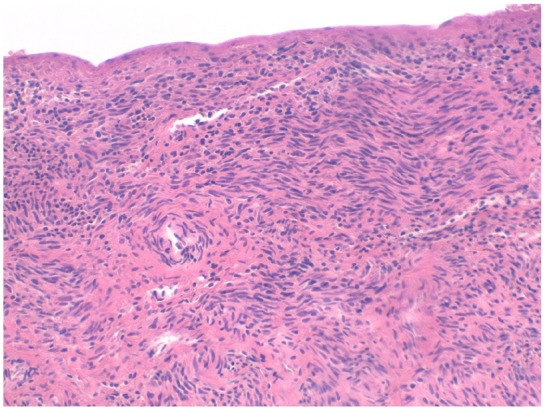
Histopathological image of the fibroid.
The patient was treated with broad-spectrum antibiotic. Patient follow-up at 1 and 3 months was clinically and ecographically normal (Figure 3).
Figure 3.
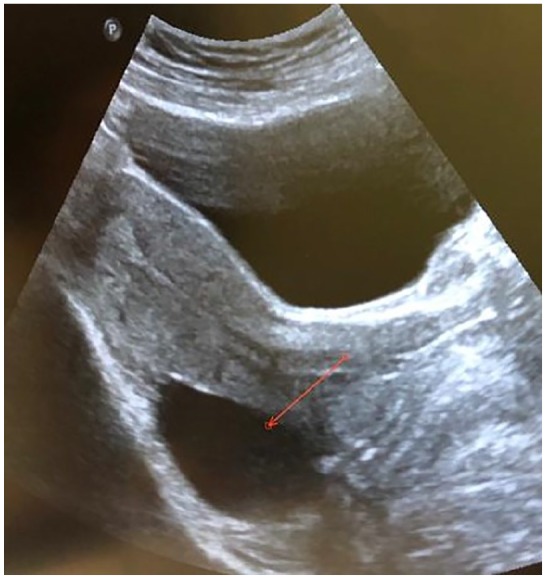
Ultrasound of the uterus after the fibroid expulsion.
Discussion
This is the first case of a perimenopause patient who had degeneration and complete spontaneous expulsion of a myoma, with no history of embolization or use of medication. According to our knowledge, there is no record of such a case in the literature. Usually the fibroid remains prolapsed and attached to the uterus, and even after degeneration, fibroids are not completely eliminated, as observed in the nascent fibroids.3
Among the few published cases reports of spontaneous expulsion of fibroids, some occurred during the pregnancy-puerperium cycle, but most were seen following magnetic resonance-guided focused ultrasound, use of drugs, or uterine artery embolization.4–6 The mechanism of spontaneous fibroid degeneration and expulsion is not clear. Degeneration could occur due to excessive fibroid growth leading to a decrease in blood supply and this excessive growth could also compress the irrigating arteries of the fibroids.7 De Cure et al.4 published a case of spontaneous expulsion in which most likely the fibroid “self-embolized” after reduced vascularity and early ischemia.
In addition, the degeneration may have been triggered due to hormonal imbalance, because in perimenopause there is a reduction in levels of the hormone estradiol and progesterone associated with the irregularity of the menstrual periods.8 One mechanism proposed for the necrosis is reduction of the blood flow in the vessel that irrigate the myoma secondary to perimenopause.9 These hormonal changes would also affect angiogenesis and culminate in fibroid degeneration.8 One other type of myoma necrosis is red fibroids degeneration which usually occurs in the pregnancy, probably due to hormonal changes that lead to fibroid growth and this growth is larger and faster than the supply of blood vessels. In the postpartum period, myomatous degeneration could occur due to reduced blood flow. Lack of menstrual cycling may also be implicated in the mechanism of fibroids degeneration.5 It is known that pregnancy leads to elevated levels of estrogen while menopause reduces their levels. Both of these alterations are related to the change in the periodicity of the menstrual cycle which is necessary for the growth and maintenance of fibroids.8
Our patient reported bleeding, pain, and the sensation of a mass being eliminated via the vagina. This is similar to the study published by Zhang et al.5 who reported that common symptoms of fibroid degeneration and expulsion included vaginal bleeding, fever, and the sensation of a mass being eliminated by the vagina along with smelly discharge. Most often myomatous degeneration is associated with pain. This pain is often localized at the site of the myoma and could be severe. This pain use to appears for days or weeks before the patient look for assistance. The other symptoms associated with myomatous degeneration are low fever, the elevation of leukocytes, and in case of hemorrhage, a decrease in hemoglobin levels.10
Cases of bleeding need to be investigated, especially in peri-menopausal women. Although our patient had only moderate bleeding and was hemodynamically stable, expulsion of the myoma may lead to significant hemorrhage. There are many diseases that lead to abnormal uterine bleeding in a perimenopausal women. Thus, it is necessary to make a differential diagnosis based on the criteria of the Federation of Gynecology and Obstetrics. They use the PALM-COEIN mnemonic that means polyp, adenomyosis, leiomyoma (or fibroids), malignancy (or neoplasia) and hyperplasia, coagulopathy, ovulatory dysfunction (as polycystic ovary syndrome), endometrial ( as endometritis), iatrogenic (as uterine perforation), and not yet classified.11 The correct diagnosis of a fibroid is made following imaging studies. Ultrasonography is the best imaging examination in a patient with suspected uterine fibroids.12
The treatment of myoma should be individualized always aiming at the best for the patient. Consideration should be given to the age of the patient, as well the desire or not to become pregnant, and the myoma size and location.13 The nascent fibroids are usually removed vaginally because they are easily accessible and cause minimal bleeding during surgery. If the tumor is a pedunculated, prolapsed or nascent but not completely eliminated, the best indicated surgery is vaginal myomectomy because it is a safe and fast procedure with good success rates.3 If the myoma is completely and spontaneously expulsed, as in the case of our patient, broad-spectrum antibiotic along with observation is sufficient.5
Conclusion
The specialist should consider the diagnosis of myomatous degeneration and complete elimination when a patient presents with bleeding and pain as the prolapse of a fibroid into the vagina can cause tremendous distress to the patient. Although complete and spontaneous expulsion of the fibroid is an unusual situation, it may mimic various clinical conditions, especially during the peri-menopausal phase, and an accurate diagnosis prevents the patient from being at risk of inadequate and delayed treatment.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the patient for her anonymized information to be published in this article.
ORCID iDs: Salete da Silva Rios  https://orcid.org/0000-0003-1162-6263
https://orcid.org/0000-0003-1162-6263
Ana Carolina Rios Chen  https://orcid.org/0000-0003-3104-8106
https://orcid.org/0000-0003-3104-8106
References
- 1. Rice KE, Secrist JR, Woodrow EL, et al. Etiology, diagnosis, and management of uterine leiomyomas. J Midwifery Womens Health 2012; 57(3): 241–247. [DOI] [PubMed] [Google Scholar]
- 2. Khan AT, Shehmar M, Gupta JK. Uterine fibroids: current perspectives. Int J Womens Health 2014; 6: 95–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Golan A, Zachalka N, Lurie S, et al. Vaginal removal of prolapsed pedunculated submucous myoma: a short, simple, and definitive procedure with minimal morbidity. Arch Gynecol Obstet 2005; 271(1): 11–13. [DOI] [PubMed] [Google Scholar]
- 4. De Cure N, Sullivan T, Robertson M, et al. Spontaneous expulsion of large submucosal uterine fibroid without embolisation: a case study. Australas J Ultrasound Med 2013; 16(1): 37–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhang J, Zou B, Wang K. Spontaneous expulsion of a huge cervical leiomyoma from the vagina after cesarean: a case report with literature review. Medicine 2018; 97(33): e11766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chantraine F, Poismans G, Nwachuku J, et al. Expulsion of a uterine myoma in a patient treated with ulipristal acetate. Clin Case Rep 2015; 3(4): 240–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Okamoto T, Koshiyama M, Yamamoto K. Rapidly growing leiomyoma in a postmenopausal woman. J Obstet Gynaecol Res 2004; 30(4): 316–318. [DOI] [PubMed] [Google Scholar]
- 8. Schwartz M, Powell K. Spontaneous rupture of a leiomyoma causing life-threatening intra-abdominal hemorrhage. Case Rep Obstet Gynecol 2017; 2017: 3701450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sah SP, Rayamajhi AK, Bhadani PP. Pyomyoma in a postmenopausal woman: a case report. Southeast Asian J Trop Med Public Health 2005; 36(4): 979–981. [PubMed] [Google Scholar]
- 10. Han SC, Kim MD, Jung DC, et al. Degeneration of leiomyoma in patients referred for uterine fibroid embolization: incidence, imaging features and clinical characteristics. Yonsei Med J 2013; 54(1): 215–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Munro MG, Critchley HO, Broder MS, et al. FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. Int J Gynaecol Obstet 2011; 113(1): 3–13. [DOI] [PubMed] [Google Scholar]
- 12. Wozniak A, Wozniak S. Ultrasonography of uterine leiomyomas. Prz Menopauzalny 2017; 16: 113–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. De La Cruz MS, Buchanan EM. Uterine fibroids: diagnosis and treatment. Am Fam Physician 2017; 95: 100–107. [PubMed] [Google Scholar]


