A 16-year-old male with chromosome 18q deletion and well controlled epilepsy presented to the Children's National Hospital (Washington, DC, USA) with haemodynamic shock after 4 days of fever and one generalised seizure at home. Although he had no respiratory symptoms, his mother was ill with a cough. Upon arrival (hospital day 0), he was intubated and resuscitated with intravenous crystalloid fluids (>40 mL/kg), an intravenous epinephrine infusion (0·4 μg/kg per min), and intravenous stress-dose hydrocortisone (100 mg). His initial infectious disease evaluation, including testing for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), did not detect an infectious aetiology; however, a second test for SARS-CoV-2 on day 3 after hospital admission was positive.
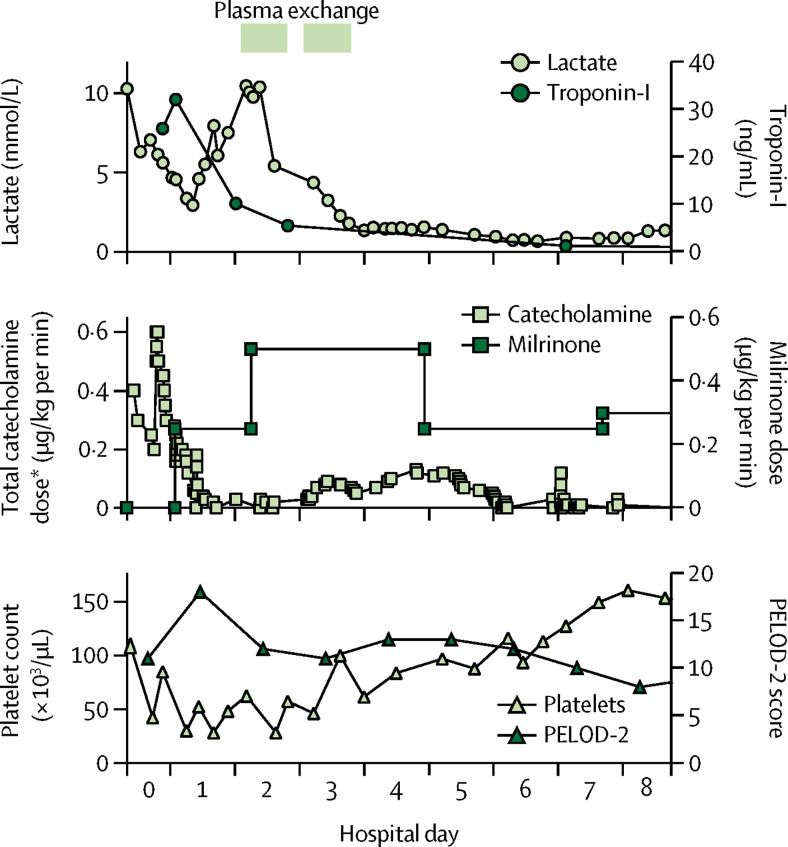
In addition to kidney injury, liver injury, and coagulopathy (table ), the patient met criteria for mild paediatric acute respiratory distress syndrome, with bilateral hazy opacities on chest radiographs and a peak oxygenation index of 4·8. He also showed significant myocardial injury, with a peak troponin-I concentration of 32 ng/mL (figure ), above that expected in paediatric sepsis.1 Serial electrocardiograms showed non-specific ST segment abnormalities, and an echocardiogram suggested the development of new moderately depressed biventricular function (ejection fraction 42%; normal range >55%) and moderate tricuspid valve regurgitation. He was started on an intravenous milrinone infusion on hospital day 1 (figure). His N-terminal brain natriuretic peptide peaked at 9959 pg/mL (normal range <1384 pg/mL) on hospital day 6.
Table.
Laboratory data at presentation
| Patient's value | Institutional normal range | |
|---|---|---|
| Troponin-I (ng/mL) | 25·92 | <0·04 |
| Lactate (mmol/L) | 7·05 | 1·00–2·40 |
| White blood cells (× 103/μL) | 10·39 | 3·84–9·84 |
| Segmented neutrophils (%) | 79 | 41–75 |
| Band neutrophils (%) | 1 | 0–1 |
| Lymphocytes (%) | 3 | 13–44 |
| Haemoglobin (g/dL) | 11·5 | 11·0–14·5 |
| Haematocrit (%) | 34 | 33·9–43·5 |
| Platelets (× 103/μL) | 42 | 175–332 |
| Blood urea nitrogen (mg/dL) | 43 | 7–21 |
| Creatinine (mg/dL) | 1·38 | 0·50–1·09 |
| Aspartate aminotransferase (U/L) | 716 | 10–41 |
| Alanine aminotransferase (U/L) | 88 | 24–54 |
| Total bilirubin (mg/dL) | 1·2 | <0·8 |
| Prothrombin time (s) | 27·6 | 11·9–14·1 |
| International normalised ratio | 2·59 | 0·90–1·12 |
| Activated partial thromboplastin time (s) | 59·9 | 22·9–26·5 |
| Fibrinogen (mg/dL) | 317 | 159–499 |
| ADAMTS13 activity (%) | 35 | 68–163 |
| von Willebrand factor activity (%) | >300 | 48–200 |
| Lactate dehydrogenase (U/L) | 2383 | 117–217 |
| Ferritin (ng/mL) | 7051 | 18–158 |
| Triglycerides (mg/dL) | 68 | 32–134 |
| Creatine kinase (U/L) | 1129 | 34–147 |
Figure.
Laboratory findings and medication trends in relation to therapeutic plasma exchange
Plasma exchange treatments were prescribed on hospital days 2 and 3. PELOD-2=Paediatric Logistic Organ Dysfunction 2. *Epinephrine plus norepinephrine doses.
The patient's presentation met the criteria for the thrombocytopenia-associated multiple organ failure (TAMOF) inflammation phenotype: he had organ failure in at least three organ systems, as well as thrombocytopenia, acute kidney injury, and a lactate dehydrogenase concentration of more than 250 U/L (table).2, 3 Further supportive of this clinical syndrome was low ADAMTS13 activity, elevated von Willebrand factor activity, and a normal fibrinogen concentration (table).4, 5 As treatment for TAMOF, we prescribed two sessions of plasma exchange on hospital days 2–3 using plasma as replacement fluid (1·2–1·3 plasma volumes). Given the patient's clinical improvement (figure) and new diagnosis of COVID-19, subsequent cycles were withheld because of theoretical concern for the removal of endogenous antibodies against the novel coronavirus, and because there is insufficient evidence to support the use of plasma exchange in viral sepsis specifically.
Hydroxychloroquine (200 mg, enteral) was initiated on hospital day 4 but discontinued after one dose because of significant prolongation of the patient's corrected QT interval. He received no other antiviral agents or biologics. At the time of this report, he has since been discharged to a rehabilitation facility after a 46-day ICU admission. His coagulopathy resolved, and his cardiac function recovered, with cessation of milrinone on hospital day 9. His oliguric renal failure also improved, requiring only intermittent dialysis on hospital days 16 and 17 for refractory uraemia. His course was complicated by bacterial tracheitis on hospital day 23, and he underwent tracheostomy on hospital day 38. He had no further seizures and appears to have returned to behavioural baseline.
The degree of cardiac injury reported here is especially unusual for a paediatric patient with a respiratory virus. This patient's genetic mutation does not appear to be associated with any baseline immune deficiencies or cardiac dysfunction that could justify the severity of illness in response to SARS-CoV-2 infection.6 His previous echocardiogram from 2016, done for evaluation of a possible atrial septal defect, did not show any abnormal cardiac anatomy, and his cardiac function was normal. Our patient's degree of cardiac injury mimics that observed in adults with COVID-19, in which cardiac insults can be seen in the absence of ischaemic heart disease7 and have been associated with a substantially elevated mortality risk.8
Hyperinflammatory syndromes and coagulopathy have gained attention in severe cases of COVID-19 in adults,9, 10, 11 while reports of paediatric critical illness remain rare12 and few detailed accounts exist. Hospitalised adults frequently have coagulopathy with elevated fibrinogen early in infection, while non-survivors often develop disseminated intravascular coagulation10 and a hyperferritinaemic inflammatory state.13 To our knowledge, TAMOF, which exists on a spectrum of inflammatory phenotypes,2 has not yet been associated with COVID-19. Beyond ferritin concentration (table), we were not routinely monitoring inflammatory markers or cytokine levels in our paediatric patients with COVID-19, as seems to be more commonly practiced in adult patients. Nevertheless, our patient's clinical course seems to have improved with plasma exchange, consistent with data from past observational studies in paediatric TAMOF.3, 5 We believe that the prevalence of COVID-19-associated coagulopathy and organ failure in paediatric patients and the utility of plasma exchange in severe COVID-19 cases require further investigation.14
The diagnosis of COVID-19 was delayed in our patient until a second test was obtained on hospital day 3. The risk of a nosocomial SARS-CoV-2 infection was very low, given the absence of the infection in our hospital at the time and the extensive use of personal protective equipment, including precautions against possible airborne transmission, when tending to any patient with a high index of suspicion for COVID-19. Although SARS-CoV-2 is often undetectable early in the course of infection, a post-hoc review revealed that the first negative test in this patient was due to a laboratory error; repeat RT-PCR analysis of both samples (from hospital days 0 and 3) returned detectable quantities of SARS-CoV-2 that were consistent between the two timepoints. Notably, our patient presented with no upper respiratory symptoms, and testing was done on samples attained from nasopharyngeal swabs. Although our assays are unable to provide truly quantitative results, both samples suggested a qualitatively low–moderate viral load. Following this case, to increase the likelihood of detection of SARS-CoV-2, our institution has implemented the practice of obtaining a second test for the virus at least 24 h after admission for all critically ill patients with a negative first test and high clinical suspicion for COVID-19.
Contributors
All authors were involved in the care of the patient. The literature search was done by GL and TD, with significant contributions from CC, RD, and MD. Data collection was done by GL. All authors contributed equally to analysing and interpreting the data. GL drafted the manuscript, with editing by TD and significant contributions by CC, RD, BJ, MD, CJ, and MB. This case report has been acknowledged by our institutional review board and did not require review or oversight.
Declaration of interests
We declare no competing interests.
References
- 1.Li J, Ning B, Wang Y. The prognostic value of left ventricular systolic function and cardiac biomarkers in pediatric severe sepsis. Medicine (Baltimore) 2019;98 doi: 10.1097/MD.0000000000015070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carcillo JA, Halstead ES, Hall MW. Three hypothetical inflammation pathobiology phenotypes and pediatric sepsis-induced multiple organ failure outcome. Pediatr Crit Care Med. 2017;18:513–523. doi: 10.1097/PCC.0000000000001122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fortenberry JD, Nguyen T, Grunwell JR. Therapeutic plasma exchange in children with thrombocytopenia-associated multiple organ failure: the Thrombocytopenia-Associated Multiple Organ Failure Network prospective experience. Crit Care Med. 2019;47:e173–e181. doi: 10.1097/CCM.0000000000003559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nguyen TC, Han YY, Kiss JE. Intensive plasma exchange increases a disintegrin and metalloprotease with thrombospondin motifs-13 activity and reverses organ dysfunction in children with thrombocytopenia-associated multiple organ failure. Crit Care Med. 2008;36:2878–2887. doi: 10.1097/ccm.0b013e318186aa49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sevketoglu E, Yildizdas D, Horoz OO. Use of therapeutic plasma exchange in children with thrombocytopenia-associated multiple organ failure in the Turkish Thrombocytopenia-Associated Multiple Organ Failure Network. Pediatr Crit Care Med. 2014;15:e354–e359. doi: 10.1097/PCC.0000000000000227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Organization for Rare Disorders Chromosome 18q– syndrome. https://rarediseases.org/rare-diseases/chromosome-18q-syndrome/
- 7.Inciardi RM, Lupi L, Zaccone G. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1096. published online March 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shi S, Qin M, Shen B. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.0950. published online March 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jose RJ, Manuel A. COVID-19 cytokine storm: the interplay between inflammation and coagulation. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30216-2. published online April 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dong Y, Mo X, Hu Y. Epidemiology of COVID-19 among children in China. Pediatrics. 2020;145 doi: 10.1542/peds.2020-0702. [DOI] [PubMed] [Google Scholar]
- 13.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05991-x. published online March 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keith P, Day M, Perkins L, Moyer L, Hewitt K, Wells A. A novel treatment approach to the novel coronavirus: an argument for the use of therapeutic plasma exchange for fulminant COVID-19. Crit Care. 2020;24:128. doi: 10.1186/s13054-020-2836-4. [DOI] [PMC free article] [PubMed] [Google Scholar]