Most people who develop COVID-19 after severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection present with paucisymptomatic and non-severe disease.1 However, approximately 20% of patients develop severe COVID-19 requiring hospitalisation, including 5% who are admitted to the intensive care unit (ICU).2 The ongoing COVID-19 outbreak has led to an unprecedented health crisis. Hence, it is crucial to identify individuals who are susceptible to developing severe COVID-19 and could require hospitalisation, especially in the ICU.
Evidence is emerging that obesity-related conditions seem to worsen the effect of the virus. Studies from Chinese cohorts of patients with COVID-19 have identified several risk factors of severe COVID-19 including age, cardiomyopathy, and obesity-related complications such as type 2 diabetes and hypertension.3
However, to our knowledge, only few studies so far have included information regarding the BMI of patients with COVID-19, which suggest a high prevalence of obesity in patients with severe COVID-19.4, 5, 6, 7 Data from New York City suggest that obesity, as defined by BMI of at least 30 kg/m2, might be a risk factor for ICU admission among patients with COVID-19, especially among those younger than 60 years.8 Additionally, preliminary analyses from Lille University Hospital have reported differences in BMI distribution in ICU patients with COVID-19 compared with ICU patients without COVID-19.7
Given the growing epidemic of COVID-19 in countries such as the USA, UK, and Mexico that have a high prevalence of obesity, there is an urgent need to clarify the relationship between obesity and severity of COVID-19. Therefore, we aimed to assess the prevalence of obesity, as defined by BMI of at least 30 kg/m2, among patients requiring hospitalisation for severe COVID-19, including those with critical COVID-19 admitted to an ICU.
On March 27, 2020, 357 patients were hospitalised in Lyon University Hospital with COVID-19, of whom 17 patients had no data on BMI (appendix p 5). We found no relevant differences in clinical features between patients with and without BMI (data not shown). 340 patients with confirmed, severe COVID-19 were included in our population, including 230 (68%) patients with non-critical COVID-19 and 110 (32%) patients with critical COVID-19 (appendix p 5). Our retrospective non-COVID-19 ICU comparison group included 1210 patients with BMI values admitted to ICU units in Lyon University Hospital on March 27 each year between 2007 and 2019 (appendix p 5).
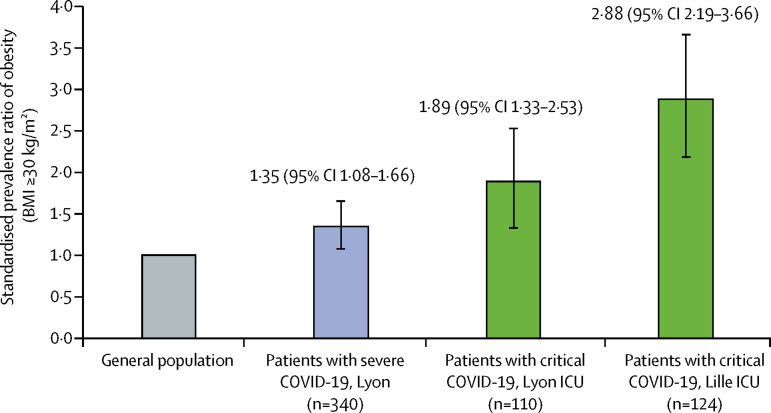
85 (25%) of 340 patients with severe COVID-19 had obesity, compared with 15·3% in the French adult population in 2014 (appendix p 8). After standardisation on age and sex, the prevalence of obesity was 1·35 times (95% CI 1·08–1·66) higher in patients with severe COVID-19 than in the general French population (p=0·0034; figure 1 ; appendix pp 6–8). Likewise, in ICU, the prevalence of obesity was 1·89 times (1·33–2·53) higher than in the general French population (p=0·0011) after standardisation on age and sex (figure 1).
Figure 1.
Prevalence of obesity in patients with severe COVID-19 compared with the general population
Severe COVID-19 was defined as any case requiring hospital admission (including admission to the ICU); among patients with severe COVID-19, critical COVID-19 was defined as requiring ICU admission. ICU=intensive care unit.
In multivariable logistic regression adjusted for age and sex, the prevalence of obesity remained higher in patients with critical COVID-19 than in those with non-critical COVID-19 (OR 1·96 [95% CI 1·13–3·42]; p=0·018; appendix pp 7–8).
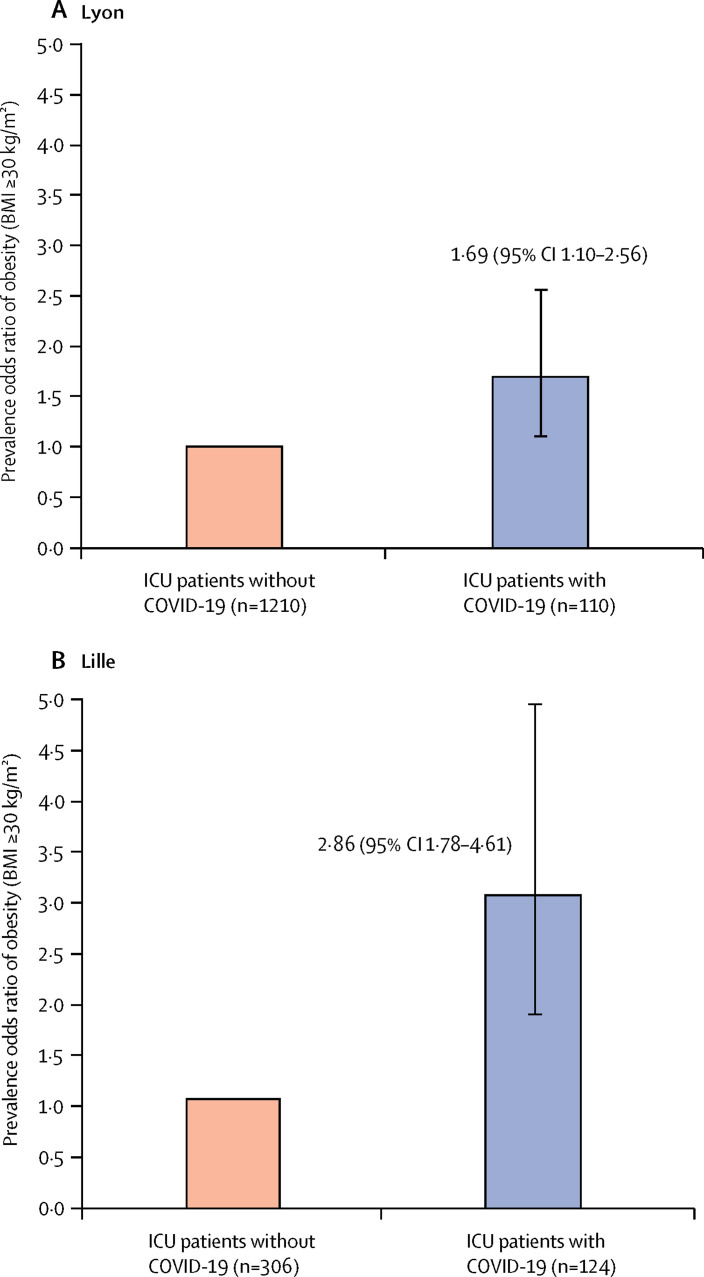
Among the 1210 patients in our retrospective ICU non-COVID-19 comparison group, 314 (26%) patients had obesity (appendix p 9). The prevalence of obesity was numerically higher in patients with critical COVID-19 than in ICU patients without COVID-19 (p=0·066; appendix p 9). After adjustment for age and sex, odds of obesity were significantly higher in patients with critical COVID-19 (OR 1·69 [95% CI 1·10–2·56]; p=0·017; figure 2A ).
Figure 2.
Prevalence of obesity in patients with critical COVID-19 compared with ICU patients without COVID-19 in the Lyon (A) and Lille (B) populations
Critical COVID-19 was defined as any case of COVID-19 requiring ICU admission. ICU=intensive care unit.
Our findings are in agreement with preliminary findings from a population comprising 124 patients with critical COVID-19 and 306 ICU patients without COVID-19 from Lille University Hospital (appendix p 5).7 As observed in the Lyon population, the prevalence of obesity in patients with critical COVID-19 in the Lille population was 2·88 times (95% CI 2·19–3·66) higher than in the French general population after standardisation on age and sex (p<0·0001; figure 1; appendix p 6).
Among the 306 ICU patients in the Lille population without COVID-19, 79 (26%) had obesity. The prevalence of obesity was higher in patients with critical COVID-19 than in ICU patients without COVID-19 (p<0·0001; appendix p 9). The prevalence of obesity in patients with critical COVID-19 was higher than in ICU patients without COVID-19 in the Lille population (OR 2·86 [95% CI 1·78–4·61]; p=0·017; figure 2B) after standardisation on age and sex.
Finally, in exploratory analyses, we looked at whether specific risk factors other than obesity were associated with critical COVID-19 versus non-critical COVID-19 in univariable analyses (appendix pp 9–10). In multivariable analyses, odds of critical COVID-19 versus non-critical COVID-19 were higher in patients with obesity than in patients without obesity when adjusted for age and sex (appendix p 9). The association remained significant after adjustment for the other potential specific risk factors, with age-sex-adjusted ORs ranging between 1·80 and 2·03 (appendix p 9).
This study reports a significant association between the prevalence of obesity and severe COVID-19, including critical COVID-19, and suggests that obesity might be a risk factor of pejorative evolution of COVID-19, increasing the risk of ICU admission. Preliminary analyses from Lille University Hospital, using the same cohort of patients, have also reported a higher prevalence of invasive mechanical intubation in male patients and those with higher BMI, especially at least 35 kg/m2 in ICU patients with COVID-19.7 However, whether these observations were influenced by a higher prevalence of obesity in these populations or important confounding factors such age and sex was not clear.9 Our study helps to fill this gap in knowledge by providing evidence of a higher prevalence of obesity among patients with severe COVID-19, especially those admitted to the ICU.
However, this cross-sectional study did not capture other possible confounding factors such as viral load, biological data, socioeconomic factors, or other obesity-related comorbidities such as non-alcoholic fatty liver disease. Additionally, this study does not include any longitudinal follow-up as several patients are still hospitalised. Some patients in the non-ICU group might yet require ICU admission. We acknowledge that the findings in our study might not be generalised to other centres depending on the clinical algorithm implemented for ICU admission and ICU capacity and recommendations for the intensive care management of COVID-19 should be considered in future research.10 Finally, the comparison of the prevalence of obesity with the general population is based only on our sample of patients with COVID-19, and a population-based study would be needed to precisely assess the demographics of patients with COVID-19 with respect to the general population.
Given the dual pandemics of COVID-19 and obesity in high-income countries, our findings have major implications for the clinical care of patients with obesity and COVID-19, as well as for public health interest. Further independent multicentre studies including longitudinal assessment of outcomes such as duration of hospitalisation and mortality are needed to confirm that obesity is a risk factor for severe COVID-19, and further analyses are planned on our datasets once follow-up is complete. These findings can help clinicians to better identify specific populations with higher risk of severe disease, which could lead to an increase in protective measures, proposal of serological screening for immunisation, and recommendation of a vaccination once available for people with obesity.
Acknowledgments
We declare no competing interests. This work was partially supported by grants from the European Commission (FEDER 12003944), Agence National de la Recherche (European Genomic Institute for Diabetes ANR-10-LABX-46), and Foundation Coeur et Arteres (FCA number R15112EE).
Supplementary Material
References
- 1.Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shi Y, Yu X, Zhao H, Wang H, Zhao R, Sheng J. Host susceptibility to severe COVID-19 and establishment of a host risk score: findings of 487 cases outside Wuhan. Crit Care. 2020;24:108. doi: 10.1186/s13054-020-2833-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen Q, Zheng Z, Zhang C, et al. Clinical characteristics of 145 patients with corona virus disease 2019 (COVID-19) in Taizhou, Zhejiang, China. Infection. 2020 doi: 10.1007/S15010-020-01432-5. published online April 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mahase E. Covid-19: most patients require mechanical ventilation in first 24 hours of critical care. BMJ. 2020;368 doi: 10.1136/bmj.m1201. [DOI] [PubMed] [Google Scholar]
- 6.Bhatraju PK, Ghassemieh BJ, Nichols M, et al. Covid-19 in critically ill patients in the Seattle region—case series. N Engl J Med. 2020 doi: 10.1056/NEJMoa2004500. published online March 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simonnet A, Chetboun M, Poissy J, et al. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity (Silver Spring) 2020 doi: 10.1002/oby.22831. published online April 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lighter J, Phillips M, Hochman S, et al. Obesity in patients younger than 60 years is a risk factor for COVID-19 hospital admission. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa415. published online April 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Caussy C, Wallet F, Laville M, Disse E. Obesity is associated with severe forms of COVID-19. Obesity (Silver Spring) 2020 doi: 10.1002/oby.22842. published online April 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Phua J, Weng L, Ling L, et al. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30161-2. published online April 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.