Abstract
Children with ventilator assistance have been supported in living at home since 1981 when parental advocacy ushered in a change to Medicaid policy. As the population of children who use medical technology such as long-term ventilation increases, we must critically evaluate our systems for preparing families for home life. Discharge delays persist in the modern era because of fragmentation between hospital and home systems. These discharge delays result in children spending time in less developmentally rich environments, further exacerbating the health and development disparities of children with complex disabilities. In this article, we discuss the complication of hospital discharge and how it contributes to health and developmental disparities. We also describe a hospital-to-home transitional care model, which presents a home-like environment to provide developmental support while focusing on parental training, home nursing, and public-funding arrangements.
More than 35 years ago Julie and Mark Beckett, the parents of Katie Beckett, led an advocacy campaign, which led to a 2-fold change in federal Medicaid policy that benefited children with technology dependence. First, parents could qualify for Medicaid based on having a child with severe disabilities and needing community health and rehabilitation services. Second, Medicaid insurance would pay for this complex care in the home.1,2 Prior to this time, children with ventilator dependency were often unable to receive services at home, and instead remained indefinitely in a hospital or a skilled nursing facility.
On June 22, 1999, the United States Supreme Court upheld the right of people with disabilities to live in the community through the Olmstead v. L.C. decision.3 This landmark case maintained that public entities should make reasonable accommodations for community-based services for people with disabilities. For example, when possible, health care services should be provided in community settings, such as acute care, intermediate care, rehabilitative care, or nursing homes, instead of more restrictive hospital settings.4 Ten years later, the Americans with Disabilities Act prohibited discrimination against people with disabilities in regard to employment, government entities, and private places of public accommodation.5 Similarly, the Convention on the Rights of the Child, generated by the United Nations, states that, “State Parties recognize that a mentally or physically disabled child should enjoy a full and decent life, in conditions which ensure dignity, promote self-reliance and facilitate the child’s active participation in the community.”6 These acts and declarations illustrate that there is both local and global precedent to ensure that children with disabilities integrate within their communities.
Over time, it has been estimated that the number of children with ventilators is increasing in our pediatric population,7,8 and they are overrepresented as a percentage of hospital admissions.9 Despite growing as a visible population of children, these complex patients and their families are faced with many disparities in health care access and community supports. Children with ventilator assistance are more likely to have prolonged hospital stays, which deprive them of important learning opportunities in the community. In this article, we describe the reasons behind long hospital stays, and explore why hospitalizations contribute to the health disparities of children with disabilities who are already at a disadvantage because of their disability status. We also briefly describe a hospital-to-home transitional care model, which seeks to improve this health disparity by offering a childand family-centered alternative to acute care.
ILLUSTRATIVE CASE
An infant boy who was born at 24 weeks gestational age had a neonatal intensive care unit (NICU) course complicated by retinopathy of prematurity, Escherichia coli sepsis, severe respiratory distress progressing to chronic lung disease of prematurity, and grade IV intraventricular hemorrhage resulting in hydrocephalus. At 9 months postnatal age, he was medically ready to be discharged home with his mother, who actively trained on his tracheostomy and ventilator care, as well as his feeding tube for formula and medication administration.
After the tracheostomy was placed, the NICU interdisciplinary team started the application to the state agency to receive home care support; however, the waiver process was not completed at the time of his planned discharge. Furthermore, the family and nursing agency had not identified nurses for his care. Although his mother was eager to take him home, she and the team agreed that because she is the sole caregiver for him and his toddler sibling, it was safest to wait to discharge him until home nursing was secure.
WHY IS DISCHARGE COMPLICATED?
Children with complex medical needs, particularly those with technology dependence, have complex discharges (Figure 1).10 Successful discharges require coordination to occur between the family, multiple medical subspecialists, nurses, respiratory therapists, pharmacies, discharge planners, social workers, durable medical equipment companies, home nursing agencies, and state funding agencies. Oftentimes discharges are delayed by nonmedical issues, such as public funding approval and home nursing availability.10–12 Throughout this extended discharge process, children with medical technology dependency may not require inpatientlevel hospital care; yet, they remain hospitalized because for most patients there is no alternative location for hospital-tohome transitional care.
Figure 1.
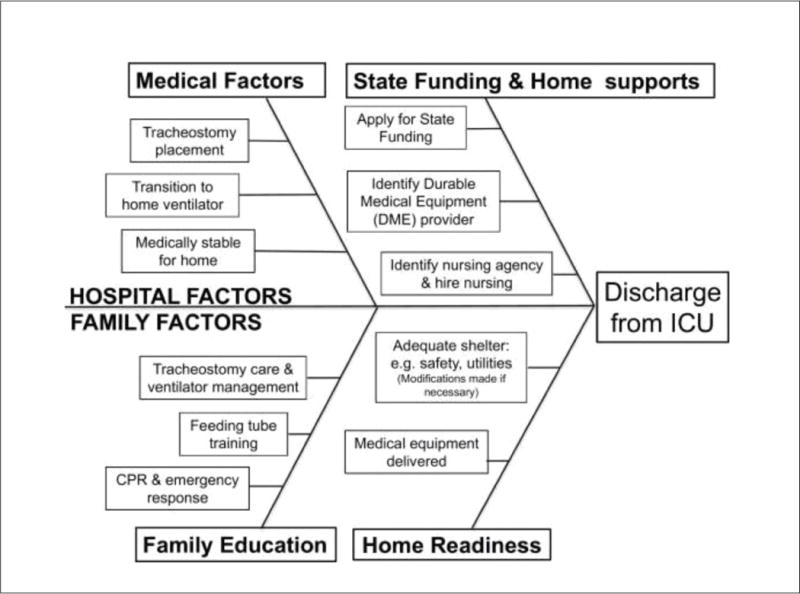
Factors affecting the timeline for discharge from the hospital for children with long-term ventilation assistance. CPR, cardiopulmonary resuscitation; ICU, intensive care unit. Adapted from Sobotka et al.10
There have been promising signs that standardizing the discharge process for children with chronic ventilation may decrease hospital length of stay (LOS). Baker et al.13 describe a quality improvement program at the Children’s Hospital of Colorado that used process mapping, educational materials, team-based care coordination, case management, and integrated electronic medical records to decrease hospital LOS for children with ventilator assistance. Continuing to aim for standardization of care and focused quality initiatives may help to lessen prolonged hospitalizations and this health care disparity for children with technology dependency.
WHY IS PROLONGED DISCHARGE A HEALTH DISPARITY?
Prolonged hospitalization is a health disparity because hospitalization is detrimental to a child’s overall development and children with complex medical needs are disproportionately hospitalized. When hospitalized, children with complex medical needs are far more likely to have prolonged hospital stays than children who are developing typically.14 Moreover, children hospitalized for long periods of time are disproportionately developmentally delayed, disabled, or considered at high risk of disability. Feldman et al.15 completed a retrospective study looking at all children younger than age 3 years discharged from a tertiary care center after hospital stays of at least 1 month. Fifty-four percent of these children were considered eligible for early intervention (EI) services based on the documentation of a developmental delay or the presence of a physical condition with a high probability of resulting in developmental delay or disability.15 A subsequent prospective study evaluated children age 6 months to 17 years hospitalized for acute care in a tertiary care center and found that the total prevalence of developmental and behavioral disorders in this population was 33.5%,16 substantially higher than the overall population prevalence of about 14%.17
One might understandably argue about causality: are more children with developmental delays hospitalized, or are longer hospitalizations associated with developmental delays? However, there is at least some evidence supporting the latter. In a population of children with congenital heart disease, it has been shown that longer LOS after heart surgery is associated with worse cognitive outcome, even when accounting for demographic and surgical outcome variables.18
HOSPITALIZATION NEGATIVELY AFFECTS DEVELOPMENT
Hospitalization is detrimental for development for many basic, yet often underappreciated factors, and children with complex medical needs are more susceptible to the negative impacts of hospitalization because of their overall developmental vulnerability. First, hospitalization restricts development and independent functioning. The child is often restricted to his or her bed or crib, which is unlike the flexibility and variability of a home environment, and often the child is no longer able to do tasks for him or herself when ill and hospitalized. The unfamiliarity of the hospital environment may be perceived as threatening, and this, coupled with separation from primary caregivers, may cause a regression in behaviors and skills.19
Second, hospitalizations impede development due to chronic and acute stressors. Children with medical complexity frequently require hospitalizations either entirely or partially within a pediatric intensive care unit (PICU) setting. Previous studies have found that 15% to 21% of children and 27% to 48% of parents experience posttraumatic stress disorder symptoms after PICU discharge.20–22 Critical illness can also affect other aspects of cognitive function, such as children’s memory and attention.23
Third, hospitalization disrupts parent-child attachment. Quality caregiver attachment in early childhood has been found to improve problem-solving and emotional regulation in later childhood.24 In a pediatric hospitalization, children are often separated from their primary caregivers for prolonged periods of time due to the child’s overall illness as well as their parent’s need to tend to other responsibilities such as other children and work. In addition, health professionals, who could potentially serve as caregiver surrogates, change frequently. This creates an unusual environment for relationship-building, which is detrimental to forming typical secure attachment relationships with primary caregivers.
Fourth, hospitalization is detrimental to development because peer interaction is limited. Children at many developmental stages learn from peer modeling, peer engagement, and typical peer social environments, yet due to concerns about medical stability and infection risk, hospitalized children infrequently engage with same-age children. At times, infection risk even precludes contact with the child’s own siblings. Limited peer exposure can be detrimental to child development, and can be socially isolating for older children and adolescents.
Finally, hospitalized children and their parents experience substantial disruption to sleep due to unfamiliar environments, nighttime nursing assessments, disruptive sounds from hospital equipment, and usual hospital activities.25 Because sleep is essential for learning, memory, and emotional regulation, one should not underestimate the potential impact of sleep disturbance on a child’s emotional and behavioral regulation and overall development. Furthermore, parents who have had substantial disruption of sleep during a hospital admission may have less stamina to care and advocate for the still-recovering child after hospital discharge.
Additionally, long hospitalizations can cause substantial disruption to work and family life. Parents often face unanticipated leave from work and experience the stress of securing alternative caretakers for other dependents. Children are affected by both the effects on their adult caregivers and by their own lost opportunities for learning and development outside of the hospital. During prolonged hospitalizations, children younger than age 3 years cannot access community-based services such as EI; children older than age 3 years miss out on educational opportunities at school and the therapeutic interventions offered through a child’s individualized education program.
Hospitalization and development create a vicious cycle: children with neurodevelopmental delays are more likely to be hospitalized, and children who are hospitalized are more likely to have neurodevelopmental delays. Thus, the double jeopardy of developmental delay and medical fragility adds to the overall health and developmental disparity of children with technology dependency. The intervention to break this cycle may be to expedite discharge to home whenever possible, and when not possible, to enable the child to be in the most developmentally stimulating environment that not only optimizes physical health, but also learning.
AN ALTERNATIVE TO INPATIENT HOSPITAL-TO-HOME TRANSITION
Almost Home Kids (AHK) is a freestanding transitional and respite center established in Illinois in 1999 with the primary goal of combining supportive and educational transitional care with respite care over time to empower families to care for children with long-term health care needs at home (Figure 2). Children who are admitted to AHK are admitted for either hospital-to-home transition care or respite care. Some children are admitted for more than one hospital-to-home transition care stay if there is an unplanned acute care readmission or a change in the child’s medical needs that requires renewed training or substantial changes to the home care plan. Over time, AHK reports low rates of readmission, and many families who complete the hospital-to-home transitional care stay decide to return to AHK for respite care.
Figure 2.
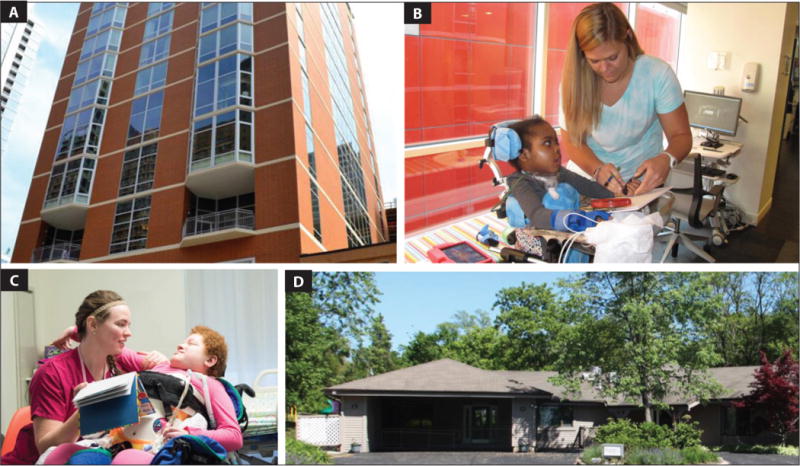
(A) Almost Home Kids Chicago downtown site. (B) Child life specialist plays with a patient. (C) Nurse reads to a patient. (D) Almost Home Kids Chicago suburban site.
The Hospital-to-Home Transitional Care Program at AHK is for children who are medically stable (ie, no longer require hospital-level care), but cannot yet go home due to social or resource obstacles. The program focuses on training parents and preparing children for the hospital-to-home transition. In Illinois, the Health Facilities Planning Act developed the certificate of need program, which requires new facilities to justify that a proposed project is needed and financially feasible. However, the Alternative Health Care Delivery Act enabled AHK to deliver transition and respite care without the high costs associated with obtaining a certificate of need. AHK is not built upon a fee-for-service billing model, but rather all services are included in a daily rate. Hospital-tohome transitional care stays at AHK are financed primarily through a patient’s insurance, mostly Illinois Medicaid, and respite care is supplemented by charitable donations. The center has a 120-day length of stay cap as determined by the Illinois Department of Healthcare and Family Services.
AHK is not a hospital, rehabilitation hospital, or long-term care facility. Each of the two AHK sites is set up like a home with 12 inpatient beds, a large kitchen, and play areas. Patient rooms, although stocked with medical equipment, more closely resemble children’s bedrooms than hospital rooms. Families learn how to care for their child in realistic family settings; they calculate medications on a kitchen counter and navigate their child’s technology needs while playing in a family room. Children receive nursing support (as they would at home) and have access to an on-call physician or advanced practice nurse. Children are transported to and from the center to attend outpatient appointments. Children are referred to EI services, and are able to receive these typically home-based services in the center. Parent training at AHK consists of bedside teaching from nurses on medical equipment and medication administration, including understanding their complex administration and interactions. Parents must demonstrate mastery of medical tasks before discharge. For example, in addition to concrete skills such as cardiopulmonary resuscitation training and responding to ventilator alarms, parents of children on ventilators are taught skills in troubleshooting equipment malfunction.
The family experience of this program has several potential benefits. First, the home-like setting enables training in a natural environment. Second, all children who stay at AHK have medical complexity, thus creating opportunities for supportive peer networks for both children and families. Third, the AHK staff is primarily focused on the goal of transitioning children with medical complexity to home; therefore, they are experts in navigating community and governmental resources for children with technology dependence.
Without AHK, most of these families would spend additional weeks or months hospitalized while completing parent training on medical equipment, awaiting home nursing assignment, or approval of public funding. Critical to this transition program’s success is supporting families in learning and trouble-shooting the care of their child in a family centered way. The center aims to evaluate the ongoing supports and care coordination that families require to promote their child’s health, development, and functioning.
ALMOST HOME KIDS’ ROLE IN THE ILLUSTRATIVE CASE
The boy was admitted to AHK for hospital-to-home transition, and his mother continued to train on ventilator and tracheostomy management, now using the same equipment her son would have at home. In the process of the state agency’s home assessment, it was discovered that the home required an electricity upgrade to safely sustain a ventilator. The AHK case management team worked with the state agency to facilitate the upgrade and complete the state waiver process. After 2 additional months in AHK, the boy was discharged home with his mom and supportive home care team.
CONCLUSION
In conclusion, children with technology dependency are a relatively new population in pediatric health care, which has grown substantially over the last 3 decades. We now understand that despite the legislative support for home services, in reality children with technology dependence spend a long time in the hospital awaiting discharge, and this contributes to stark disparities in their health, development, and family well-being. Too often children have prolonged hospitalizations because current policy does not support fluid transition and access to community services. We must seek evidence-based solutions to inefficiencies and consider alternative models of care, such as the AHK hospital-to-home transitional care program, to reduce health and developmental disparities for this vulnerable population.
Acknowledgments
S. A. S. received support from The University of Chicago Patient-Centered Outcomes Research K12 Training Program (5K12HS023007). S. A. S. and M. E. M. received funding from the Illinois LEND (Leadership Education in Neurodevelopmental and Related Disabilities) program (grant T73MC11047; US Department of Health and Human Services [HHS], Health Resources and Services Administration [HRSA]) training program.
Footnotes
Disclaimer: The views, policies, and opinions expressed are those of the authors and do not necessarily reflect those of the HRSA/HHS or the National Institutes of Health.
Disclosure: The authors have no relevant financial relationships to disclose.
Contributor Information
Sarah A. Sobotka, Instructor, Section of Developmental and Behavioral Pediatrics, Department of Pediatrics, The University of Chicago.
Rishi K. Agrawal, Associate Professor, Division of Hospital-Based Medicine, Department of Pediatrics, Northwestern University Feinberg School of Medicine.
Michael E. Msall, Professor of Pediatrics, and the Associate Director, Kennedy Research Center on Intellectual and Neurodevelopmental Disabilities, The University of Chicago Pritzker School of Medicine; and the Chief, Section of Developmental and Behavioral Pediatrics, Comer Children’s Hospital.
References
- 1.Johnson BH. Family-centered care: four decades of progress. Fam Syst Health. 2000;18(2):137–156. doi: 10.1037/h0091843. [DOI] [Google Scholar]
- 2.King AC. Long-term home mechanical ventilation in the United States. Respir Care. 2012;57(6):921–930. doi: 10.4187/respcare.01741. [DOI] [PubMed] [Google Scholar]
- 3.Olmstead v. L. C 527, 581 (Supreme Court 1999)
- 4.United States Department of Justice. Civil Rights Division. Olmstead: community integration for everyone. https://www.ada.gov/olmstead/olmstead_about.htm. Accessed September 19, 2017.
- 5.Equal Employment Opportunity Commission. Americans With Disabilities Act of 1990. https://www.eeoc.gov/eeoc/history/35th/thelaw/ada.html. Accessed September 19, 2017.
- 6.United Nations General Assembly. Convention on the rights of the child. http://www.refworld.org/docid/3ae6b38f0.html. Accessed September 19, 2017.
- 7.Graham RJ, Fleegler EW, Robinson WM. Chronic ventilator need in the community: a 2005 pediatric census of Massachusetts. Pediatrics. 2007;119(6):e1280–1287. doi: 10.1542/peds.2006-2471. [DOI] [PubMed] [Google Scholar]
- 8.McDougall CM, Adderley RJ, Wensley DF, Seear MD. Long-term ventilation in children: longitudinal trends and outcomes. Arch Dis Child. 2013;98(9):660–665. doi: 10.1136/archdischild-2012-303062. [DOI] [PubMed] [Google Scholar]
- 9.Feudtner C, Villareale NL, Morray B, Sharp V, Hays RM, Neff JM. Technology-dependency among patients discharged from a children’s hospital: a retrospective cohort study. BMC Pediatr. 2005;5(1):8. doi: 10.1186/1471-2431-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sobotka SA, Hird-McCorry LP, Goodman DM. Identification of fail points for discharging pediatric patients with new tracheostomy and ventilator. Hosp Pediatr. 2016;6(9):552–557. doi: 10.1542/hpeds.2015-0277. [DOI] [PubMed] [Google Scholar]
- 11.Edwards EA, O’Toole M, Wallis C. Sending children home on tracheostomy dependent ventilation: pitfalls and outcomes. Arch Dis Child. 2004;89(3):251–255. doi: 10.1136/adc.2003.028316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Graf JM, Montagnino BA, Hueckel R, McPherson ML. Children with new tracheostomies: planning for family education and common impediments to discharge. Pediatr Pulmonol. 2008;43(8):788–794. doi: 10.1002/ppul.20867. [DOI] [PubMed] [Google Scholar]
- 13.Baker CD, Martin S, Thrasher J, et al. A standardized discharge process decreases length of stay for ventilator-dependent children. Pediatrics. 2016;137(4):e20150637. doi: 10.1542/peds.2015-0637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Simon TD, Berry J, Feudtner C, et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 2010;126(4):647–655. doi: 10.1542/peds.2009-3266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Feldman HM, Ploof DL, Hofkosh D, Goehring EL., Jr Developmental needs of infants and toddlers who require lengthy hospitalization. Am J Dis Child. 1993;147(2):211–215. doi: 10.1001/archpedi.1993.02160260101034. [DOI] [PubMed] [Google Scholar]
- 16.Petersen MC, Kube DA, Whitaker TM, Graff JC, Palmer FB. Prevalence of developmental and behavioral disorders in a pediatric hospital. Pediatrics. 2009;123(3):e490495. doi: 10.1542/peds.2008-2750. [DOI] [PubMed] [Google Scholar]
- 17.Boyle CA, Boulet S, Schieve LA, et al. Trends in the prevalence of developmental disabilities in US children, 1997-2008. Pediatrics. 2011;127(6):1034–1042. doi: 10.1542/peds.2010-2989. [DOI] [PubMed] [Google Scholar]
- 18.Newburger JW, Wypij D, Bellinger DC, et al. Length of stay after infant heart surgery is related to cognitive outcome at age 8 years. J Pediatr. 2003;143(1):67–73. doi: 10.1016/S0022-3476(03)00183-5. [DOI] [PubMed] [Google Scholar]
- 19.Blom GE. The reactions of hospitalized children to illness. Pediatrics. 1958;22(3):590–600. [PubMed] [Google Scholar]
- 20.Rees G, Gledhill J, Garralda ME, Nadel S. Psychiatric outcome following paediatric intensive care unit (PICU) admission: a cohort study. Intensive Care Med. 2004;30(8):1607–1614. doi: 10.1007/s00134-004-2310-9. [DOI] [PubMed] [Google Scholar]
- 21.Shears D, Nadel S, Gledhill J, Garralda ME. Short-term psychiatric adjustment of children and their parents following meningococcal disease. Pediatr Crit Care Med. 2005;6(1):39–43. doi: 10.1097/01.PCC.0000144705.81825.EE. [DOI] [PubMed] [Google Scholar]
- 22.Knoester H, Grootenhuis MA, Bos AP. Outcome of paediatric intensive care survivors. Eur J Pediatr. 2007;166(11):1119–1128. doi: 10.1007/s00431-007-0573-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Elison S, Shears D, Nadel S, Sahakian B, Garralda ME. Neuropsychological function in children following admission to paediatric intensive care: a pilot investigation. Intensive Care Med. 2008;34(7):1289–1293. doi: 10.1007/s00134-008-1093-9. [DOI] [PubMed] [Google Scholar]
- 24.Matas L, Arend RA, Sroufe LA. Continuity of adaptation in 2nd year: the relationship between quality of attachment and later competence. Child Dev. 1978;49(3):547–556. [Google Scholar]
- 25.Meltzer LJ, Davis KF, Mindell JA. Patient and parent sleep in a children’s hospital. Pediatr Nurs. 2012;38(2):64–71. [PubMed] [Google Scholar]


