Abstract
Leaving behind substantial reflections or skepticisms on the shortage of evidences about blood pressure (BP) thresholds for antihypertensive drug therapy and target BPs, major hypertensive guidelines including Korean hypertension guidelines were recently updated for earlier and more intensive control of BP. Because hypertension is one of the major risk factors for death, stroke, cardiovascular (CV) disease, heart failure, and cognitive impairment, substantial improvement of hypertension management is necessary to reduce disease and socioeconomic burdens and to promote CV health. Theoretically, earlier intervention in terms of age and BP level and thorough control of BP into within normal range would prevent or delay major adverse CV events. Revised hypertension guidelines were developed by the American College of Cardiology/American Heart Association, Korean Society of Hypertension, European Society of Cardiology/European Society of Hypertension, and Japanese Society of Hypertension in order. In this article, recent updates and clinical significances of the Korean hypertension guidelines will be discussed with comparison of foreign hypertension guidelines and considerable changes in the management of hypertension will be introduced for cardiologists and general practitioners.
Keywords: Hypertension, Practice guideline, Risk factors, Antihypertensive agents
INTRODUCTION
For the optimal management of hypertension, evidence-based medicine and patient-centered care based on the clinical trials, meta-analyses and systemic review provide the development and implementation of multi-level strategies including education, shared decision-making, preventive collaborative measures, clinical practice guidelines, and health policy. Among them, the development of hypertension guidelines is very important and essential to reduce cardiovascular disease (CVD) outcomes and mortality, to decrease disease and socioeconomic burdens, and to enhance CV healthy aging. The first Korean Society of Hypertension (KSH) recommendations for the management of hypertension were released in 2000 and the following revised hypertension guidelines were published in 2004 together with the companion guideline on blood pressure (BP) monitoring for the accurate BP measurement at clinic, home and 24-hour ambulatory settings. In 2013, updated KSH hypertension guidelines1),2),3) were developed by the adoption of the European Society of Cardiology/European Society of Hypertension (ESC/ESH) guidelines. Meta-analyses of important outcome trials including Systolic Blood Pressure Intervention Trial (SPRINT)4) heavily influenced the American College of Cardiology/American Heart Association (ACC/AHA) hypertension guidelines5) to lower BP threshold to define hypertension as systolic BP (SBP) values ≥130 mmHg or diastolic BP (DBP) values ≥80 mmHg in 2017. However, the majority of global hypertension guidelines except American guidelines have retained the previous definition of hypertension (i.e., office BP ≥140/90 mmHg). Hypertension Canada annually updates evidence-based guidelines for the diagnosis, assessment, prevention, and treatment of hypertension and the latest Canadian hypertension guidelines were published on March 2018.6) New KSH guidelines for the management of hypertension7),8),9) were released on May 2018 during Hypertension Jeju meeting and ESC/ESH guidelines for the management of arterial hypertension10) were also introduced on June 2018 during European hypertension meeting. The Japanese Society of Hypertension guidelines which were publish on September 2019 also defines hypertension as an office BP ≥140/90 mmHg or home BP ≥135/85 mmHg.11)
EPIDEMIOLOGY OF HYPERTENSION IN KOREA
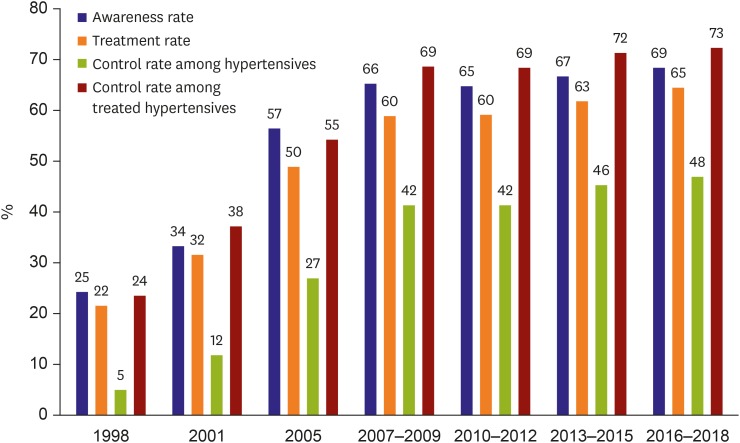
The Hypertension Epidemiology Research Working Group of the KSH recently published the Korea Hypertension Fact Sheet 201812) by the in-death analyses of the Korean National Health and Nutrition Examination Survey Data (1998–2018) and the National Health Insurance Big Data (2002–2016). The prevalence of hypertension has not been changed over the past 20 years, from 29.8% in 1998 to 29.1% in 2016. The level of hypertension management indicated by awareness rate, treatment rate and control rate has been stagnant during the last 10 years (Figure 1). Up to date, 11.7 million people are hypertensive patients, of which 30% are not aware of it, and 35% are not treated, and 48% are controlled at the target BP level of <140/90mmHg. Although overall control rate of hypertension is not quite high enough in general, control rate of treated hypertensive patients is over 70% regardless of age. Surprisingly, both awareness rate and treatment rate in the younger people especially in the third and fourth decades are merely ~20% and ~40%, respectively and the control rates are even lower in both sexes.
Figure 1. Trends of hypertension management in Korea.
Level of hypertension management in Korea improved rapidly since 1998 over a decade but it has been stagnant over another decade since 2007. Data are presented as age-standardized proportion for the adults aged 30 or higher in Korean National Health and Nutritional Examination Survey.
ELEVATED BLOOD PRESSURE AND PREHYPERTENSION, NO MORE 85 mmHg IN DIASTOLIC BLOOD PRESSURE
Hypertension has been defined by the threshold in which efficacy of drug therapy was proven by randomized clinical trials.13) Because of SPRINT study, the threshold of hypertension was declined down to 130/80 mmHg in ACC/AHA 2017 guidelines. For the management of hypertension in cardiology practice, this threshold might seem to be practical especially in high-risk patients, but in general it may provoke unnecessary antihypertensive medication because of the multiple co-morbidities or heterogeneity of CV patients. Therefore, recently revised KSH 2018 guidelines7) maintained the previous definition of hypertension (Table 1) because guideline is primarily targeted for the primary care physicians and the prevalence of hypertension in Korea exceeds 50% if the BP threshold of hypertension defines to ≥130/80 mmHg.
Table 1. Classification of office BP and definitions of hypertension in adults.
| SBP | DBP | KSH 2018 | ACC/AHA 2017 | ESC/ESH 2018 | JSH 2019 | |
|---|---|---|---|---|---|---|
| <120 | and | <80 | Normal* | Normal | Optimal | Normal |
| 120–129 | and | <80 | Elevated | Elevated | Normal† | High normal |
| 130–139 | and/or | 80–89 | Prehypertension | Stage 1 | High normal‡ | Elevated |
| 140–159 | and/or | 90–99 | Grade I | Stage 2 | Grade 1 | Grade I |
| 160–179 | and/or | 100–109 | Grade II | Stage 2 | Grade 2 | Grade II |
| ≥180 | and/or | ≥110 | Grade II | Stage 2 | Grade 3 | Grade III |
BP category is defined according to seated clinic BP and by the highest level of BP, whether systolic or diastolic.
ACC = American College of Cardiology; AHA = American Heart Association; BP = blood pressure; DBP = diastolic blood pressure; ESC = European Society of Cardiology; ESH = European Society of Hypertension; JSH = Japanese Society of Hypertension; KSH = Korean Society of Hypertension; SBP = systolic blood pressure.
*BP threshold with minimal risk for cardiovascular events; †Normal BP category is defines as SBP 120–129 mmHg and/or DBP 80–84mmHg; ‡High normal BP category is defines as SBP 130–139 mmHg and/or DBP 85–89 mmHg.
Prehypertension (SBP 130–139 mmHg and/or DBP 80–89 mmHg) is only adopted in the Korean hypertension guidelines because it causes greater CV risks than normal BP category and can be used in parallel with prediabetes to express the need of preemptive life style changes. In addition, because DBP ranges between 80 and 85 mmHg are reported to be associated with CV risks especially in the Korean cohort study (n=1,234,435, age 30–95 years) including young subjects,14) DBP cut-off level of 85 mmHg became redundant and so it was removed in this updated KSH 2018 guidelines. Because the level of hypertension management is very poor in the young and middle-aged people, this approach that lowers DBP threshold to 80 mmHg for prehypertension enables to have more attention on hypertension when BP starts to elevate especially in younger individuals. Although prehypertension is an important public health challenge because it may develop hypertension and is associated with a high risk of CVD,15) it is still on debate whether prehypertension without diabetes, established CVDs or chronic kidney disease (CKD) should be treated with antihypertensive agents or not.16) More studies are needed to reveal better predictors of high-risk subpopulations with prehypertension,17) therefore risk-driven antihypertensive therapy was not adopted in prehypertension in KSH 2018 guidelines. Instead, increased BP load-driven antihypertensive therapy in addition to life style modification was supported when it was proved by out-of-office BP measurement such as ambulatory or home BP monitoring even in prehypertensive subjects.
Throughout middle and old age, usual BP is strongly and directly related to CV and overall mortality, without any evidence of a threshold down to at least 115/75 mmHg.18) Elevated BP category (SBP 120–129 mmHg and DBP <80 mmHg) is characterized with increased pulse pressure as well as elevated SBP and was adopted in both ACC/AHA and Korean hypertension guidelines, but elevated BP category in the Japanese guidelines seems to have more CV risks because BP level is much higher than other major guidelines.11) Since this is a new category with uncertain clinical implications, further studies are needed to identify the clinical significance in the future but primary care physicians and cardiologists should pay attention on the elevated BP group during follow-up in the clinic.
MASKED AND WHITE-COAT HYPERTENSIONS
Clinical clues to masked hypertension were provided as the BP range of prehypertension with the presence of metabolic syndrome, target organ damage, diabetes mellitus, CKD, and occupational stress, smoker, and younger male subjects. Basically, masked hypertension is supposed to neglected, only anticipation or high level of suspicion could lead to diagnosis and proper management of masked hypertension.
According to the Korean ambulatory BP monitoring registry (n=1,916), white-coat hypertension (WCH) was higher in untreated patient than in treated hypertensive patients19) suggesting WCH can be a challenge at the time of deciding to initiate antihypertensive medication in the untreated hypertensive subjects. Even though antihypertensive medication for WCH patients with high CV risk profiles may result in improved outcome, it is largely not adopted in KSH 2018 guidelines because evidence is not sufficient. But close follow-up for the new development of hypertension in WCH subjects is strongly recommended in the new Korean hypertension guidelines, similarly to other major guidelines.
TREATMENT INITIATION, OBVIOUSLY EXPANDED
In KSH 2018 guidelines, indications of antihypertensive medication were obviously expanded. Because there is no representative CV risk assessment system or CVD prediction model in Korea, count of risk factors is still recommended for rough estimation of CV risk. Presence of only 1 risk factor in hypertensives should start antihypertensive medication and life style modification simultaneously at the time of diagnosis of hypertension. In other words, the only exception for antihypertensive medication is the grade 1 hypertension patient without any risk factor at all.
For clinician's view point, the definition of the risk factors in hypertension patient is very important because it is critical to decide the timing of antihypertensive medication. As defined in ESC/ESH guidelines, they are defined by the risk exposed by hypertension plus combined condition to increased CV events or death. Because of baseline risk conferred by hypertension, the threshold of the additional risk factor regarding blood glucose level or lipid level were lower than individual diagnostic criteria for hypercholesterolemia or diabetes.8)
In addition, with the exceptions of age more than 80 or frail patient, all elderly hypertensive patients are indicated for antihypertensive medication because age over 65 itself was shown to be strong risk factor in a Korean cohort study.20),21)
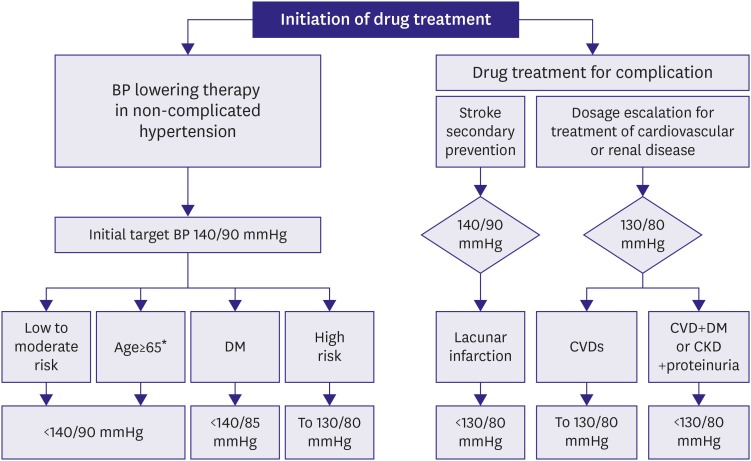
TARGET BLOOD PRESSURES, WHAT EVIDENCES TELL
In KSH 2018 guidelines, two clinical pathways were introduced for hypertensive patients taking antihypertensive medication (Figure 2). In addition to non-complicated patient who start antihypertensive medication when BP is 140/90 mmHg or higher, all other hypertensive patients combined or complicated clinical CVD or renal disease should be started with angiotensin converting enzyme inhibitor for coronary artery disease, heart failure (HF), or albuminuria, beta blocker for coronary artery diseases or HF, calcium channel blocker for variant angina, and/or diuretics for HF according to the disease specific guidelines when those drugs are tolerated regardless of the presence of hypertension or not. Some patients need maximal tolerable dose of specific drug if BP, heart rate and side effects are acceptable. In this case, the target BP indicates the maximal BP allowed during the titration of those drugs.
Figure 2. Clinical algorithm to achieve target BP according to the presence of complicated diseases or patient risk profiles. In complicated patients, one or more antihypertensive medications are already initiated regardless of level of BP according to the standard treatment guidelines so that further titration can be decided by recommended target BP.
BP = blood pressure; CKD = chronic kidney disease; CVD = cardiovascular disease; DM = diabetes mellitus.
*BP lowering drug treatment and lifestyle modifications are recommended for frail elderly patients or very old patients (≥80 years) when SBP is ≥160 mmHg.
Because of the recommended clinical algorithm, it is important to recognize that there are also two kinds of patients population even in meta-analyses cited in major international hypertension guidelines. One is usual hypertension population in whom antihypertensive medication was initiated only when BP level reach the hypertension threshold. The other is complicated population who take antihypertensive medication not because they are hypertensive patient but because some classes of antihypertensive medication are proved to be essential for treatment of the complications. Most of recent guidelines are heavily influenced by meta-analyses.22) In some meta-analyses, studies enrolling patients already taking antihypertensive medication because of complications were included for analyses.23) Therefore, it is very hard to know how much proportion of those population are really hypertensive or normotensive. Moreover, usually in treated normotensive patient or HF patient, it is very easy to achieve BP less than 130 mmHg. In this regards, in terms of target BP, the evidence extracted from the achieved BP in those complicated populations should be differently interpreted from the evidence from the achieved BP in strict hypertensive populations. Another issue regarding the meta-analyses of hypertension treatment is how to interpret the influence of SPRINT.4),23) Because the corresponding clinic BP level to 120 mmHg by automated office BP measurement is speculated to be, at least, above 130 mmHg, it seems to be safe not to include SPRINT as it is.24)
When further lowering target BP, as shown in SPRINT and Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial, harmful side effects should be considered. In the recent meta-analyses excluding the study for complicated patient but including SPRINT and ACCORD trial, relative risk reduction by BP lowering below 130 mmHg could be statistically significant only when SRINT was included.23) At the same time, absolute risk reduction per standardized BP reduction of 10/5 mmHg in SBP/DBP was decreased down to a half when the initial BP levels was 150 mmHg vs. 130 mmHg.
In KSH 2018 guidelines, the objectives of antihypertensive treatment are to reduce the overall risk of occurrence, progression and recurrence of heart, brain, kidney and vascular complications and to prevent mortality. Based on the evidence from meta-analyses not including SPRINT study,25) the goal of BP control should be managed below 140/90 mmHg in general patients, and some hypertensive patients with diabetes, proteinuria, high-risk category can control their BP below 130/80 mmHg. Target BPs in the new Korean hypertension guideline takes the most conservative and safest stance and it is similar to 2018 European hypertension guidelines in terms of target BPs.
PHARMACOLOGICAL TREATMENT, NEW TRENDS
Recently published Korean hypertension guidelines typically recommends thiazide-like diuretics such as chlorthalidone or indapamide and also initial combination therapy is recommended when required BP lowering is >20/10 mmHg in SBP/DBP to achieve target BP goals. Needless to say, these recommendations underscore straightforward BP lowering to the target levels, however for such intensive strategy, safety issues always should be kept in mind. Because lowering BP thresholds depends not only on the level of BP but also on the patient's characteristics, 2018 Korean hypertension guidelines recommended that it needs much caution when BP is lowered below 110/70 mmHg in the elderly, diabetes patients, multiple coronary artery diseases without revascularization therapy, and severe left ventricular hypertrophy.
COMPARISON WITH MAJOR GLOBAL GUIDELINES
There are several differences between KSH 2018 guidelines and the foreign major guidelines because of the difference in the scope of the guidelines, difference in the health care system, and availability of the clinical evidences (Table 2). For example, for earlier intervention, lowering thresholds for hypertension diagnosis could be the simplest approach as shown in ACC/AHA 2017 guideline.5) This change also means to make an intervention for the younger subjects who more likely to think that they do not have any health problem. But in Korea, because of quite lower absolute risk for most of the subjects in the hypertensive BP range, lowering diagnostic threshold to 130/80 mmHg could result in serious epidemiological distortion and wide spread inertia for hypertension as a diagnostic entity. Such changes should be supported by cost-effective healthcare system for life style modification which is not available in Korea yet.
Table 2. Comparison of office BP targets in major hypertension guidelines.
| Category | KSH 2018 | ACC/AHA 2017 | ESC/ESH 2018 | JSH 2019 | |
|---|---|---|---|---|---|
| General population | <140/90 | <130/80 | <130/80 | <130/80 | |
| Elderly (≥65 years of age)* | <140/90 | <130 (SBP) | <140/80 | <140/90 (≥75 years) | |
| Diabetes mellitus | <140/85 | <130/80 | <130/80 | <130/80 | |
| Chronic kidney disease | Proteinuria (−) | <140/90 | <130/80 | <140/80 | <140/90§ |
| Proteinuria (+) | <130/80 | <130/80 | |||
| Cardiovascular disease | Coronary artery disease | <130/80 | <130/80 | <130/80 | <130/80 |
| Heart failure | <130/80 | <130/80 | <130/80† | <130 (SBP) | |
| Cerebrovascular disease‡ | Stroke/TIA | <140/90 | <130/80 | <130/80 | <130/80 |
| Lacunar | <130/80 | ||||
ACC = American College of Cardiology; AHA = American Heart Association; BP = blood pressure; ESC = European Society of Cardiology; ESH = European Society of Hypertension; JSH = Japanese Society of Hypertension; KSH = Korean Society of Hypertension; SBP = systolic blood pressure; TIA = transient ischemic attack.
*Office BP thresholds for treatment in very old patients (≥80 years) or frail elderly hypertensives when BP is ≥160/90 mmHg in both KSH and ESH guidelines, whereas BP level to initiate treatment is SBP ≥130 and ≥140/90 mmHg in ACC/AHA and JSH guidelines, respectively; †Outcome for patients with heart failure is poor if BP values are low, which suggests that it may be wise to avoid actively lowering BP to <120/70 mmHg, especially in heart failure with reduced ejection fraction; ‡Recommended BP goals for the secondary stroke prevention. ESH guideline suggests an SBP target range of 120–130 mmHg should be considered in all hypertensive patients with ischemic stroke or TIA; §JSH guideline recommends a target BP <140/90mmHg in patients with cerebrovascular disease in whom bilateral carotid artery stenosis and/or cerebral main artery occlusion is present or has not yet been evaluated.
Regarding target BP, there is a little difference in nuance between below 130 mmHg (<130 mmHg) and to 130 mmHg or less (≤130 mmHg). If it is concerned around 140 mmHg, there could be no argue against the rounding them to <140 mmHg. But when BP lowered below 140 mmHg, the risk of adverse event increases gradually.26) Strictly speaking, such description or discrepancy itself suggests that actual sweet spot for target BP could be about 130 mmHg.
NON-ADHERENCE PROBLEM, NOT YET READY
In ACC/AHA 2017 guidelines, systematic team-based approach was recommended with grade I and level of evidence A. However, team-based approach is time and cost demanding and it needs high quality human interaction. Patient centered counselling needs soft skills or new interviewing style not only for a physician but also supportive team members. But this recommendation does not necessarily mean that such infrastructures are established in United States well enough for systematic team-based approach to be included in the ACC/AHA hypertension guidelines.
In addition, in European hypertension guidelines, strategies to improving adherence are also much updated and they are based on the patient centered approaches or motivational strategies. But there are few information about how much these recommendations can be implemented.
Considering healthcare system in Korea, team-based approach or patient centered counselling could pose tremendous burden for revision of the current system, largely not patient centered yet. Therefore, these approaches could not be recommended in the new Korean hypertension guidelines. Because untreated patients especially in young age comprise the major unmet needs in overall hypertension management in Korea, physician needs to be able to handle the unique situational awareness and practical reasoning of young asymptomatic hypertension patients to motivate the behavioral changes.
CONCLUSION
In general, recently revised Korean hypertension guidelines are in line with major global hypertension guidelines in terms of earlier and intensive control of hypertension. But because of relatively smaller benefit-to-risk ratio in Korean population when the BP threshold for treatment is lowered, the KSH 2018 guideline recommendations are relatively conservative until more evidences are accumulated. In addition to more intensive therapy for patient taking antihypertensive medication already, more practically, new hypertensives should be identified by using out-of-office BP measurement and more hypertensive patient should be adherent to antihypertensive treatment by patient centered approaches.
May Measurement Month campaign led by International Society of Hypertension is a global initiative to increase awareness of high BP and to enhance better hypertension control and it was launched in Korea from 2019 to screen unawareness of high BP and to identify untreated or poorly controlled hypertensive patients. For the evidence-based optimal management of hypertension, most of all, Korean specific risk assessment system and prediction modeling to identify high risk hypertensives should be established as soon as possible. Smart digital healthcare and precision medicine revolutionized by the omics data and state-of-the art technologies will provide a remarkable progress in the management of hypertension in the future.
Footnotes
Funding: This research was supported by a fund (2018-ER6303-00) by Research of Korea Centers for Disease Control and Prevention.
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Shin J, Cho MC.
- Data curation: Shin J.
- Investigation: Shin J.
- Project administration: Cho MC.
- Resources: Cho MC.
- Supervision: Cho MC.
- Validation: Cho MC.
- Visualization: Shin J, Cho MC.
- Writing - original draft: Shin J.
- Writing - review & editing: Cho MC.
References
- 1.Shin J, Park JB, Kim KI, et al. 2013 Korean Society of Hypertension guidelines for the management of hypertension: part I-epidemiology and diagnosis of hypertension. Clin Hypertens. 2015;21:1. doi: 10.1186/s40885-014-0012-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shin J, Park JB, Kim KI, et al. 2013 Korean Society of Hypertension guidelines for the management of hypertension. Part II-treatments of hypertension. Clin Hypertens. 2015;21:2. doi: 10.1186/s40885-014-0013-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shin J, Park JB, Kim KI, et al. 2013 Korean Society of Hypertension guidelines for the management of hypertension: part III-hypertension in special situations. Clin Hypertens. 2015;21:3. doi: 10.1186/s40885-014-0014-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.SPRINT Research Group. Wright JT, Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Circulation. 2018;138:e484–e594. doi: 10.1161/CIR.0000000000000596. [DOI] [PubMed] [Google Scholar]
- 6.Nerenberg KA, Zarnke KB, Leung AA, et al. Hypertension Canada's 2018 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults and children. Can J Cardiol. 2018;34:506–525. doi: 10.1016/j.cjca.2018.02.022. [DOI] [PubMed] [Google Scholar]
- 7.Kim HC, Ihm SH, Kim GH, et al. 2018 Korean Society of Hypertension guidelines for the management of hypertension: part I-epidemiology of hypertension. Clin Hypertens. 2019;25:16. doi: 10.1186/s40885-019-0121-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee HY, Shin J, Kim GH, et al. 2018 Korean Society of Hypertension guidelines for the management of hypertension: part II-diagnosis and treatment of hypertension. Clin Hypertens. 2019;25:20. doi: 10.1186/s40885-019-0124-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim KI, Ihm SH, Kim GH, et al. 2018 Korean Society of Hypertension guidelines for the management of hypertension: part III-hypertension in special situations. Clin Hypertens. 2019;25:19. doi: 10.1186/s40885-019-0123-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 11.Umemura S, Arima H, Arima S, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2019) Hypertens Res. 2019;42:1235–1481. doi: 10.1038/s41440-019-0284-9. [DOI] [PubMed] [Google Scholar]
- 12.Korean Society Hypertension (KSH); Hypertension Epidemiology Research Working Group. Kim HC, Cho MC. Korea hypertension fact sheet 2018. Clin Hypertens. 2018;24:13. doi: 10.1186/s40885-018-0098-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams B, Mancia G, Spiering W, et al. 2018 Practice guidelines for the management of arterial hypertension of the ESH/ESC: task force for the management of arterial hypertension. J Hypertens. 2018;36:2284–2309. doi: 10.1097/HJH.0000000000001961. [DOI] [PubMed] [Google Scholar]
- 14.Kimm H, Mok Y, Lee SJ, Lee S, Back JH, Jee SH. The J-curve between diastolic blood pressure and risk of all-cause and cardiovascular death. Korean Circ J. 2018;48:36–47. doi: 10.4070/kcj.2017.0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang Y, Wang S, Cai X, et al. Prehypertension and incidence of cardiovascular disease: a meta-analysis. BMC Med. 2013;11:177. doi: 10.1186/1741-7015-11-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martin JF, Martin LN, Cipullo JP. Pharmacologic treatment for prehypertension: to treat or not to treat? Recent Patents Cardiovasc Drug Discov. 2009;4:133–141. doi: 10.2174/157489009788452904. [DOI] [PubMed] [Google Scholar]
- 17.Pimenta E, Oparil S. Prehypertension: epidemiology, consequences and treatment. Nat Rev Nephrol. 2010;6:21–30. doi: 10.1038/nrneph.2009.191. [DOI] [PubMed] [Google Scholar]
- 18.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 19.Shin J, Park SH, Kim JH, et al. Discordance between ambulatory versus clinic blood pressure according to global cardiovascular risk group. Korean J Intern Med. 2015;30:610–619. doi: 10.3904/kjim.2015.30.5.610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jung KJ, Jang Y, Oh DJ, et al. The ACC/AHA 2013 pooled cohort equations compared to a Korean risk prediction model for atherosclerotic cardiovascular disease. Atherosclerosis. 2015;242:367–375. doi: 10.1016/j.atherosclerosis.2015.07.033. [DOI] [PubMed] [Google Scholar]
- 21.Lee JH, Kim KI, Cho MC. Current status and therapeutic considerations of hypertension in the elderly. Korean J Intern Med. 2019;34:687–695. doi: 10.3904/kjim.2019.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–967. doi: 10.1016/S0140-6736(15)01225-8. [DOI] [PubMed] [Google Scholar]
- 23.Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension: 7. Effects of more vs. less intensive blood pressure lowering and different achieved blood pressure levels - updated overview and meta-analyses of randomized trials. J Hypertens. 2016;34:613–622. doi: 10.1097/HJH.0000000000000881. [DOI] [PubMed] [Google Scholar]
- 24.Kjeldsen SE, Mancia G. The un-observed automated office blood pressure measurement technique used in the SPRINT study points to a standard target office systolic blood pressure <140 mmHg. Curr Hypertens Rep. 2017;19:3. doi: 10.1007/s11906-017-0700-y. [DOI] [PubMed] [Google Scholar]
- 25.Xie X, Atkins E, Lv J, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016;387:435–443. doi: 10.1016/S0140-6736(15)00805-3. [DOI] [PubMed] [Google Scholar]
- 26.Bangalore S, Toklu B, Gianos E, et al. Optimal systolic blood pressure target after SPRINT: insights from a network meta-analysis of randomized trials. Am J Med. 2017;130:707–719.e8. doi: 10.1016/j.amjmed.2017.01.004. [DOI] [PubMed] [Google Scholar]