Abstract
Background and Objectives
This study compared the potential impacts of the 2017 American College of Cardiology/American Heart Association (ACC/AHA) and the 2018 Korean Society of Hypertension (KSH) guidelines on prevalence of hypertension, recommended antihypertensive treatment, and achievement of target blood pressure (BP) in Korean population.
Methods
We analyzed the 2007–2017 Korea National Health and Nutrition Examination Survey data to calculate guideline-specific hypertension prevalence and treatment implications on 59,767 adults aged 20 years or older by sex and age.
Results
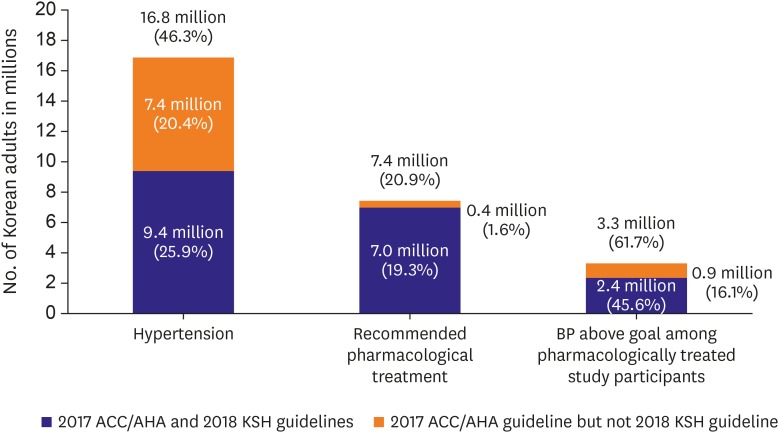
The prevalence of hypertension was markedly higher 46.3% by the ACC/AHA guideline due to the lowered BP cutoff than 25.9% by the KSH guideline; the increase was most pronounced in young adults. Yet, there was only a marginal 1.6% increase in the percentage of adults suggested pharmacological approach by the ACC/AHA guideline, but selectively in the older subgroups. Overall, 45.6% of Korean adults treated for hypertension failed to meet BP goal according to the KSH guideline; the underachievement extended to 61.7% of participants according to the ACC/AHA guideline.
Conclusions
The lowered BP threshold, 130/80 mmHg, by the 2017 ACC/AHA guideline, in conjuncture with 10-year risk calculation largely driven by age, would increase pharmacological treatment preferentially in very old individuals, while increasing prevalence and uncontrolled rate mostly in younger subgroups. Adoption of lower BP cutoff to the KSH guideline would require validated cardiovascular disease risk assessment tools accounting for risk distributions specific to Korean population.
Keywords: Hypertension, Blood pressure, Prevalence, Guideline, Cardiovascular diseases
INTRODUCTION
High blood pressure (BP) is a major yet modifiable risk factor for cardiovascular disease (CVD) worldwide.1) The 2017 American College of Cardiology/American Heart Association Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults (ACC/AHA guideline)2) has adopted lower BP criteria for hypertension, 130/80 mmHg, compared with the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC 7)'s3) previous 140/90 mmHg. On the other hand, the 2018 Korean Society of Hypertension (KSH) Guidelines for the Management of Hypertension (KSH guideline) stood by the diagnostic criteria of 140/90 mmHg,4) while recommending pharmacological treatment for individuals with prehypertension (130–139/80–89 mmHg) if at high risk for atherosclerotic cardiovascular diseases (ASCVD; Table 1).
Table 1. BP levels used to define hypertension, recommended antihypertensive medication, and treatment goal according to the 2017 ACC/AHA and 2018 KSH guidelines.
| Target population | 2017 ACC/AHA | 2018 KSH | |||
|---|---|---|---|---|---|
| Guideline definition of hypertension | |||||
| SBP (mmHg) | |||||
| All population | ≥130 | ≥140 | |||
| DBP (mmHg) | |||||
| All population | ≥80 | ≥90 | |||
| Guideline-recommended antihypertensive medication | |||||
| SBP (mmHg) | |||||
| General population | ≥140 | ≥140 | |||
| ≥60 yrs of age without diabetes or CKD | -* | ≥150 | |||
| Diabetes mellitus | ≥130 | ≥140 | |||
| Chronic kidney disease | ≥130 | -* | |||
| High cardiovascular disease risk | ≥130 | ≥130 | |||
| DBP (mmHg) | |||||
| General population | ≥90 | ≥90 | |||
| ≥60 yrs of age without diabetes or CKD | -* | ≥90 | |||
| Diabetes mellitus | ≥80 | ≥85 | |||
| Chronic kidney disease | ≥80 | -* | |||
| High cardiovascular disease risk‡ | ≥80 | ≥80 | |||
| Guideline treatment goal among those taking antihypertensive medication | |||||
| SBP (mmHg) | |||||
| General population | <130 | <140 | |||
| Age ≥65 yrs | <130 | <140 | |||
| Diabetes mellitus | <130 | ||||
| Uncomplicated | <140 | ||||
| Complicated† | <130 | ||||
| Chronic kidney disease | <130 | ||||
| Without albuminuria | <140 | ||||
| With albuminuria§ | <130 | ||||
| High cardiovascular disease risk‡ | -* | ≤130 | |||
| Cardiovascular disease | -* | ≤130 | |||
| Cerebrovascular disease | -* | ≤140 | |||
| DBP (mmHg) | |||||
| General population | <80 | <90 | |||
| Age≥65 yrs | -* | <90 | |||
| Diabetes mellitus | <80 | ||||
| Uncomplicated | <90 | ||||
| Complicated† | <80 | ||||
| Chronic kidney disease | <80 | ||||
| Without albuminuria | <90 | ||||
| With albuminuria§ | <80 | ||||
| High cardiovascular disease risk‡ | -* | ≤80 | |||
| Cardiovascular disease | -* | ≤80 | |||
| Cerebrovascular disease | -* | <90 | |||
For 2018 KSH guideline, 10-year predicted ASCVD risk ≥15% qualifies as high risk.
ACC = American College of Cardiology; AHA = American Heart Association; ASCVD = atherosclerotic cardiovascular disease; BP = blood pressure; DBP = diastolic blood pressure; KSH = Korean Society of Hypertension; SBP = systolic blood pressure.
*No specific BP threshold is provided in the guideline for this population. †Complicated by sub-clinical organ damage or cardiovascular diseases. ‡For 2017 ACC/AHA guideline, high cardiovascular disease risk is defined as a history of cardiovascular disease or 10-year predicted ASCVD risk ≥10% using the Pooled Cohort Equation. ‡High risk, elderly patients should be followed by elderly patients' criteria. §Including microalbuminuria.
Both contemporary BP guidelines were influenced by the benefit of intensive BP lowering in high-risk individuals, demonstrated by Systolic Blood Pressure Intervention Trial (SPRINT)5) as well as meta-analyses of trials.6) The identification of at-risk individuals is done by 10-year ASCVD risk prediction in the ACC/AHA guideline and by number of risk factors and target organ damage in the KSH guideline. Consequently, the recommendation for pharmacological treatment among adults with systolic blood pressure (SBP) 130–139/diastolic blood pressure (DBP) 80–89 mmHg as well as the BP goal would differ between the 2 guidelines. The objective of this study was to compare the prevalence of hypertension, the percentage recommended for pharmacological treatment, and the proportion with unmet BP goal according to the two aforementioned guidelines among Korean population by sex and age subgroups.
METHODS
Study population
This study analyzed data from the Korea National Health and Nutrition Examination Survey (KNHANES) conducted between 2007 and 2017. The KNHANES is an ongoing surveillance system in the Republic of Korea that assesses current health status and distributions of its risk factors. It collects detailed information on demographics, disease history, health behaviors, healthcare utilization, nutrition and provides detailed anthropometric, blood, and urinal profiles from on-site health examination.7) To produce unbiased cross-sectional estimates of the noninstitutionalized Korean population, it uses complex, multi-stage probability sample design. Sample weights are constructed to account for non-response and post-stratification, assuming the data within strata are missing at random.7) The details of the KNHANES is published elsewhere.7) In the present study, among 89,630 participants, 21,473 children/adolescents under the age of 20 were excluded. Then, 4,853 participants with missing BP measurements or information on antihypertensive medication intake were further excluded. Of the remaining 63,304 participants, 3,537 participants without measurement on key covariates required to calculate ASCVD risk score, including cigarette smoking, fasting glucose, physician diagnosis of diabetes mellitus (DM), and total and high-density lipoprotein cholesterols, were additionally excluded. Consequently, 59,767 participants (26,920 male and 36,384 female) were included in the final analyses.
Blood pressure measurement and definition of hypertension
BP was measured using a standard mercury sphygmomanometer (Baumanometer Wall Unit 33 [catalog No. 0850]; Baum Co., Inc., Copiague, NY, USA). Participants sat in a comfortable position after they had rested for at least five minutes and had refrained from smoking 30 minutes prior to the measurement. BP was measured on three consecutive occasions in a standardized environment, free of disturbances, at 1-minute intervals. To minimize variability and misclassification due to white coat hypertension, the average of the second and the third measurements was adopted for the data analysis.8) Using structured questionnaire, trained interviewee inquired participants regarding their previous physician diagnosis and treatment of hypertension. Participants currently using antihypertensive medication were classified as the treated group.
According to the 2017 ACC/AHA guideline, hypertension was defined as SBP ≥130 mmHg, DBP ≥80 mmHg, or current antihypertensive medication intake. Likewise, according to the 2018 KSH guideline, hypertension was defined as SBP ≥140 mmHg, DBP ≥90 mmHg, or current intake of antihypertensive medications. The guideline-specific prevalence of hypertension was calculated among all study participants combined and separately by sex and decile age groups. All presented statistics are weighted accordingly to account for contemporary Korean population structure.
Atherosclerotic cardiovascular diseases risk factors and predicted 10-year risk
Lifestyle factors, including current smoking status, and history of chronic diseases, including formal diagnosis by medical doctor and treatment status, were self-reported, guided by the standardized questionnaire. Quality of the survey and health examination was controlled by trained personnel using calibrated equipment and strictly adhering to standardized protocols. The health examination obtained participants' body weight and height to the nearest 0.1 kg and 0.1 cm, respectively, while wearing light clothing without shoes. Body mass index (BMI) was then calculated as the ratio of weight in kilograms to height in squared meters. Eight-hour fasting serum total and high-density lipoprotein cholesterols and glucose concentrations were enzymatically assessed via Hitachi Automatic Analyzer 7600 (Hitachi, Tokyo, Japan) in 2007 and COBAS 8000 C702 (Roche Diagnostics System, Rotkreuz, Switzerland) onwards. Then, presence of DM was defined as fasting plasma glucose ≥126 mg/dL, glycated hemoglobin level ≥6.5%, or taking glucose-lowering drugs.9) Dyslipidemia was defined as total cholesterol ≥240 mg/dL, low-density lipoprotein cholesterol ≥160 mg/dL, high-density lipoprotein cholesterol <40 mg/dL, triglyceride ≥200 mg/dL, or taking lipid-lowering drugs.10) Chronic kidney disease (CKD) was defined as glomerular filtration rate <60 mL/min/1.73 m2 estimated by the Chronic Kidney Disease-Epidemiology Collaboration equation.11),12) Predicted 10-year ASCVD risk scores were derived from the Korean Risk Prediction Model (KRPM)13) and, as a supplementary analysis, from the 2013 ACC/AHA Pooled Cohort Equation (PCE).14) Additionally, following the 2018 KSH guideline, CVD risk category was determined by the number of risk factors, including age, smoking, obesity, dyslipidemia, diabetes, family history of premature CVD, and subclinical organ damage.
Statistical analyses
General characteristics of the study population were reported as weighted frequency or mean and its corresponding 95% confidence interval (CI). We calculated the distribution of the population across 5 BP groups: SBP <120 and DBP <80 mmHg, SBP 120–129 and DBP <80 mmHg, SBP 130–139 or DBP 80–89 mmHg, SBP 140–159 or DBP 90–99 mmHg, and SBP ≥160 or DBP ≥100 mmHg—assigned to the higher category when SBP and DBP correspond to different groups. Participants taking antihypertensive medication were grouped separately. Then, we compared the differences in participant demographics and physiological characteristics across these groups. Next, we calculated the percentage and the number of Korean adults with hypertension and recommended for antihypertensive medication according to the ACC/AHA guideline, the KSH guideline, and the ACC/AHA guideline but not the KSH guideline—referred to as the “difference” of the two guidelines. Lastly, we calculated the percentage and the number of Korean adults treated for hypertension whose BP exceed the target, likewise by the two guidelines and their differences. These calculations were performed on the overall population and within subgroups defined by sex, age, and ASCVD risk categories based on the KRPM and the PCE. All statistical tests were 2-sided, and statistical significance was set at a p value <0.05. All analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Ethics approval and consent to participate
The KNHANES IV–VII were administered by the Korea Center for Disease Control and Prevention and approved by the Institutional Review Board (2007-02-CON-04-P, 2008-04EXP-01-C, 2009-01CON-03-2C, 2010-02CON-21-C, 2011-02CON-06-C, 2012-01EXP-01-2C, 2013-07CON-03-4C, 2013-12EXP-03-5C, 2015-01-02-6C). Each participant voluntarily participated and provided a signed written consent before participating in the study.
RESULTS
Participant characteristics
Table 2 presents general characteristics of the participants by BP classification according to the KSH guideline; the ACC/AHA guideline adopts identical BP classification, except shifting of the Korean criteria's prehypertension and stage 1 hypertension to stage 1 and 2 hypertension, respectively. Among participants currently untreated for hypertension, 48.5% (95% CI, 47.8-49.1) had SBP/DBP levels of <120/80 mmHg, 5.2% (95% CI, 5.0–5.5) had 120–129/<80 mmHg, 20.3% (95% CI, 19.9–20.8) had 130–139/80–89 mmHg, 8.7% (95% CI, 8.4–9.0) had 140–159/90–99 mmHg, and ≥160/100 mmHg 2.3% (95% CI, 2.1–2.5), respectively. Additionally, 15.0% (95% CI, 14.6–15.3) of the participants were currently taking antihypertensive medication.
Table 2. Characteristics of the study participants by BP levels and antihypertensive medication usage according to the 2018 KSH guideline.
| Variables | SBP/DBP categories among participants untreated for hypertension (mmHg) | Taking antihypertensive medication (n=11,856) | |||||
|---|---|---|---|---|---|---|---|
| Normal BP (<120/80) (n=26,619) | Elevated BP (120–129/<80) (n=3,386) | Prehypertension (130–139/80–89) (n=11,299) | Stage 1 HTN (140–159/90–99) (n=5,238) | Stage 2 HTN (≥160/100) (n=1,369) | |||
| % of study population | 48.5 (47.8–49.1) | 5.2 (5.0–5.5) | 20.3 (19.9–20.8) | 8.7 (8.4–9.0) | 2.3 (2.1–2.5) | 15.0 (14.6–15.3) | |
| Sex | |||||||
| Male | 40.1 (39.5–40.8) | 54.7 (52.8–56.7) | 64.2 (63.2–65.2) | 66.9 (65.5–68.3) | 70.5 (67.8–73.2) | 47.6 (46.5–48.7) | |
| Female | 59.9 (59.2–60.5) | 45.3 (43.3–47.2) | 35.8 (34.8–36.8) | 33.1 (31.7–34.5) | 29.5 (26.8–32.2) | 52.4 (51.3–53.5) | |
| Age (year) | |||||||
| 20–29 | 26.5 (25.7–27.3) | 19.2 (17.2–21.3) | 15.6 (14.6–16.6) | 8.2 (7.1–9.4) | 4.3 (2.8–5.9) | 0.2 (0.1–0.4) | |
| 30–39 | 27.5 (26.7–28.3) | 13.5 (12.0–15.1) | 21.5 (20.5–22.5) | 16.4 (15.1–17.7) | 17.2 (14.7–19.8) | 1.8 (1.5–2.2) | |
| 40–49 | 23.4 (22.7–24.1) | 14.8 (13.3–16.3) | 26.0 (24.9–27.0) | 26.7 (25.2–28.2) | 30.7 (27.7–33.7) | 10.8 (9.9–11.6) | |
| 50–59 | 14.0 (13.5–14.5) | 18.9 (17.4–20.4) | 22.3 (21.4–23.3) | 25.6 (24.2–28.2) | 26.7 (23.9–29.5) | 26.1 (25.0–27.1) | |
| 60–69 | 5.7 (5.4–6.0) | 18.0 (16.6–19.4) | 9.4 (8.8–9.9) | 12.9 (11.9–13.8) | 11.2 (9.6–12.7) | 30.0 (29.0–31.0) | |
| 70–79 | 2.5 (2.3–2.7) | 12.8 (11.6–14.0) | 4.4 (4.0–4.8) | 8.1 (7.4–8.8) | 7.5 (6.2–8.9) | 25.0 (24.1–25.9) | |
| 80+ | 0.4 (0.3–0.5) | 2.6 (2.1–3.2) | 0.9 (0.7–1.0) | 2.2 (1.8–2.5) | 2.3 (1.5–3.2) | 6.1 (5.6–6.6) | |
| Household income | |||||||
| Low | 10.4 (9.8–11.0) | 21.0 (19.4–22.7) | 12.4 (11.6–13.2) | 17.4 (16.1–18.6) | 17.9 (15.5–20.3) | 31.5 (30.3–32.7) | |
| Middle-low | 24.7 (23.9–25.6) | 26.6 (24.6–28.6) | 24.9 (23.8–26.0) | 25.5 (24.0–27.0) | 24.4 (21.7–27.0) | 25.8 (24.8–26.9) | |
| Middle-high | 31.9 (31.0–32.8) | 28.2 (26.2–30.2) | 30.3 (29.2–31.5) | 29.5 (27.9–31.1) | 31.3 (28.3–34.3) | 21.2 (20.2–22.2) | |
| High | 33.0 (31.9–34.0) | 24.1 (22.3–26.0) | 32.4 (31.1–33.7) | 27.6 (26.0–29.3) | 26.5 (23.6–29.3) | 21.4 (20.3–22.6) | |
| Smoking status | |||||||
| Non-smoker | 60.9 (60.2–61.6) | 54.5 (52.3–56.6) | 45.4 (44.3–46.5) | 42.5 (40.9–44.1) | 37.0 (34.1–39.9) | 55.9 (54.8–57.0) | |
| Previous smoker | 12.1 (11.6–12.6) | 16.3 (14.7–17.9) | 17.9 (17.0–18.8) | 18.1 (16.8–19.4) | 22.0 (19.2–24.9) | 21.6 (20.6–22.5) | |
| Current smoker | 27.0 (26.3–27.7) | 29.2 (27.2–31.3) | 36.7 (35.6–37.9) | 39.4 (37.8–41.1) | 41.0 (38.0–43.9) | 22.5 (21.5–23.5) | |
| BMI (kg/m2) | 22.7 (22.7–22.8) | 24.0 (23.9–24.2) | 24.4 (24.3–24.5) | 25.1 (24.9–25.2) | 25.5 (25.3–25.8) | 25.3 (25.2–25.4) | |
| Total cholesterol (mg/dL) | 183.8 (183.3–184.3) | 190.6 (189.–192.1) | 196.0 (195.2–196.8) | 200.0 (198.7–201.3) | 203.6 (201.4–205.8) | 187.0 (186.1–187.8) | |
| HDL-C (mg/dL) | 51.7 (51.6–51.9) | 49.4 (48.9–49.9) | 49.1 (48.9–49.4) | 48.5 (48.1–48.9) | 48.2 (47.5–48.9) | 46.9 (46.6–47.1) | |
| Triglyceride (mg/dL) | 110.9 (109.7–112.2) | 137.8 (133.1–142.5) | 158.0 (154.5–161.5) | 178.0 (172–183.6) | 194.4 (184.6–204.3) | 160.2 (157.5–163.0) | |
| Lipid-lowering agent | 1.9 (1.8–2.1) | 5.5 (4.7–6.4) | 2.8 (2.5–3.2) | 2.9 (2.4–3.4) | 1.7 (0.9–2.4) | 24.4 (23.4–25.3) | |
| Fasting glucose (mg/dL) | 93.1 (92.8–93.3) | 100.4 (99.4–101.3) | 99.0 (98.5–99.6) | 102.0 (101.2–102.8) | 104.9 (103.0–106.9) | 109.4 (108.8–110.1) | |
| Diabetes mellitus | 3.8 (3.6–4.1) | 11.5 (10.3–12.8) | 7.8 (7.2–.8.3) | 10.1 (9.1–2.9) | 10.7 (8.7–12.7) | 27.7 (26.6–28.7) | |
| GFR (mL/min/1.73m2) | 101.8 (101.4–102.1) | 94.6 (93.9–95.4) | 96.3 (95.9–96.7) | 93.2 (92.6–93.7) | 91.8 (90.8–92.8) | 81.9 (81.5–82.3) | |
| CKD | 0.7 (0.6–0.8) | 2.5 (1.9–3.0) | 1.0 (0.8–1.2) | 2.4 (2.0–2.9) | 2.9 (1.9–3.8) | 11.1 (10.4–11.8) | |
| History of CVD | 2.4 (2.1–2.7) | 6.9 (5.7–8.2) | 4.3 (3.7–4.9) | 4.7 (3.8–5.6) | 2.7 (1.6–3.8) | 21.3 (20.1–22.5) | |
| Number of ASCVD risk factors according to the KSH guideline | |||||||
| 0 | 40.4 (39.6–41.1) | 19.2 (17.4–20.9) | 18.4 (17.5–19.3) | 10.3 (9.3–11.3) | 7.7 (6.0–9.5) | 5.0 (4.5–5.5) | |
| 1–2 | 47.5 (46.8–48.2) | 54.5 (52.4–56.5) | 56.5 (55.4–57.6) | 55.7 (54.1–57.3) | 53.3 (50.1–56.5) | 43.7 (42.6–44.8) | |
| ≥3 | 12.1 (11.6–12.6) | 26.4 (24.7–28.1) | 25.1 (24.1–26.1) | 34.0 (32.5–35.5) | 38.9 (35.9–42.0) | 51.3 (50.1–52.4) | |
| Predicted 10-year ASCVD risk according to the Korean Risk Prediction Model* | |||||||
| <5% | 94.6 (94.2–95.1) | 80.1 (77.7–82.4) | 87.0 (85.8–88.1) | 74.0 (72.6–75.4) | 60.4 (57.3–63.6) | 22.2 (20.5–23.9) | |
| ≥5% and <10% | 3.2 (2.9–3.6) | 8.8 (7.0–10.6) | 8.3 (7.4–9.2) | 14.7 (13.5–15.9) | 22.4 (19.6–25.2) | 25.9 (24.4–27.4) | |
| ≥10% and <20% | 1.5 (1.3–1.7) | 7.3 (6.0–8.5) | 3.5 (3.0–4.0) | 7.4 (6.6–8.1) | 11.9 (10.0–13.9) | 25.8 (24.4–27.2) | |
| ≥20% | 0.6 (0.5–0.7) | 3.8 (2.9–4.8) | 1.2 (1.0–1.5) | 3.9 (3.4–4.4) | 5.2 (4.1–6.3) | 26.2 (24.7–27.6) | |
Values are presented as weighted % or mean (95% confidence interval). The study participants were grouped into the higher category of SBP and DBP. For example, if a person had an isolated elevation of SBP (150/80 mmHg), they were allocated in stage 1 hypertension group.
ASCVD = atherosclerotic cardiovascular disease; BMI = body mass index; BP = blood pressure; CKD = chronic kidney disease; CVD = cardiovascular disease; DBP = diastolic blood pressure; HTN = hypertension; GFR = glomerular filtration rate; HDL-C = high-density lipoprotein cholesterol; KSH = Korean Society of Hypertension; SBP = systolic blood pressure.
*High risk defined as a 10-year predicted ASCVD risk ≥10% or history of CVD. Predicted 10-year ASCVD risk was calculated among adults without a history of CVD.
Overall, participants classified into higher BP category were older with higher proportion of male sex. They also had higher BMI, cholesterol and fasting glucose levels, and more reduced kidney function. In the context of health-related lifestyle, they were more likely to be current smoker and drinker yet less likely to fulfill sufficient physical activity. Altogether, participants with higher BP accompanied greater number of ASCVD risk factors designated by the KSH guideline. In parallel, they were also more likely to embody high-risk 10-year ASCVD risk level according to the KRPM (2.1% in <120/80 mmHg; 11.1% in 120–129/<80 mmHg; 4.7% in 130–139/80–89 mmHg; 11.3% in 140–159/90–99 mmHg; 17.1% in ≥160/100 mmHg), with the exception observed between elevated BP and prehypertension groups. Substituting the KRPM with the PCE yielded parallel result.
Prevalence of hypertension
In a nationally representative dataset from the Republic of Korea, we found that 18,463 participants, representing 9.4 million people nationally, or 25.9% (95% CI, 25.4–26.5) of the population, would qualify as hypertension on the basis of KSH guideline definitions (Table 3 and Figure 1). The numbers are markedly higher when applying the ACC/AHA guideline, where additional 11,299 people, representing 16.8 million or 46.3% (95% CI, 45.6–46.9) of the population, would be classified as having hypertension with the use of lowered BP thresholds. Therefore, 7.4 million adults aged above 20 years would be additionally classified as having hypertension on the basis of the ACC/AHA guidelines, translating to a 20.4% (95% CI, 20.1–20.8) relative increase. The prevalence of hypertension based on the ACC/AHA guideline was consistently higher within all sex, age, and ASCVD risk. Compared with participants labeled as hypertension by the KSH guideline, those additionally given hypertension status by the ACC/AHA guideline were younger, with the most prominent increase contributed by the age group 40–49 years (23.9%, 95% CI, 23.4–24.3) and male sex (26.1% vs. 14.6% in female sex). They were most likely to possess only one to 2 ASCVD risk factors (22.9%) by the KSH guideline; analogously, they embodied near-minimal predicted 10-year ASCVD risk by the KRPM (21.7% in <5% category). Application of the PCE did not significantly change the direction nor the magnitude of the result (Supplementary Table 1 and Supplementary Figure 1).
Table 3. Percentage of study participants, meeting the definition for hypertension and recommended antihypertensive medication according to the 2017 ACC/AHA and the 2018 KSH guidelines.
| Variables | 2017 ACC/AHA guideline | 2018 KSH guideline | 2017 ACC/AHA but not 2018 KSH | ||||
|---|---|---|---|---|---|---|---|
| Hypertension | Recommended antihypertensive medication | Hypertension | Recommended antihypertensive medication | Hypertension | Recommended antihypertensive medication | ||
| Overall | 46.3 (45.6, 46.9) | 20.9 (20.4, 21.4) | 25.9 (25.4, 26.5) | 19.3 (18.8, 19.7) | 20.4 (20.1, 20.8) | 1.6 (0.9, 3.0) | |
| Age group (year) | |||||||
| 20–29 | 22.5 (21.3, 23.8) | 4.9 (4.3, 5.5) | 4.8 (4.2, 5.4) | 4.7 (4.1, 5.3) | 17.7 (17.1, 18.0) | 0.2 (0.0, 0.5) | |
| 30–39 | 31.6 (30.5, 32.7) | 10.2 (9.5, 10.9) | 10.3 (9.6, 11.0) | 9.8 (9.1, 10.4) | 21.3 (21.0, 21.8) | 0.4 (0.0, 1.0) | |
| 40–49 | 45.0 (43.9, 46.1) | 18.8 (17.9, 19.7) | 21.1 (20.2, 22.0) | 17.8 (16.9, 18.6) | 23.9 (23.4, 24.3) | 1.0 (0.2, 1.4) | |
| 50–59 | 59.1 (58.1, 60.2) | 26.4 (25.4, 27.4) | 35.3 (34.3, 36.4) | 24.4 (23.4, 25.4) | 23.8 (23.4, 24.1) | 2.0 (1.2, 3.0) | |
| 60–69 | 67.8 (66.7, 69.0) | 37.6 (36.4, 38.8) | 51.1 (49.9, 52.3) | 32.3 (31.1, 33.5) | 16.7 (16.2, 17.4) | 5.3 (4.8, 5.9) | |
| 70–79 | 74.6 (73.4, 75.8) | 48.7 (47.2, 50.2) | 62.6 (61.2, 63.9) | 45.7 (44.2, 47.1) | 12.0 (11.8, 12.1) | 3.0 (2.4, 3.8) | |
| 80+ | 79.8 (77.4, 82.2) | 52.9 (49.9, 55.9) | 69.7 (66.8, 72.5) | 49.4 (46.3, 52.4) | 10.1 (9.6, 10.5) | 3.5 (2.4, 4.2) | |
| Sex | |||||||
| Male | 55.3 (54.4, 56.1) | 24.9 (24.2, 25.6) | 29.2 (28.4, 29.9) | 23.2 (22.5, 23.9) | 26.1 (25.7, 26.5) | 1.7 (1.3, 2.1) | |
| Female | 37.3 (36.5, 38.0) | 16.9 (16.4, 17.4) | 22.7 (22.1, 23.3) | 15.4 (14.9, 15.9) | 14.6 (14.2, 15.0) | 1.5 (0.9, 2.1) | |
| Number of ASCVD risk factors* | |||||||
| 0 | 21.3 (20.4, 22.2) | 5.4 (5.0, 5.8) | 7.0 (6.5, 7.5) | 5.8 (5.4, 6.3) | 14.3 (14.0, 14.5) | −0.4 (−0.7, −0.1) | |
| 1–2 | 48.1 (47.3, 49.0) | 20.6 (20.0, 21.2) | 25.2 (24.5, 25.8) | 19.1 (18.5, 19.7) | 22.9 (22.4, 23.2) | 1.5 (1.1, 2.0) | |
| ≥3 | 69.6 (68.6, 70.5) | 38.0 (37.0, 39.0) | 48.2 (47.1, 49.2) | 33.9 (33.0, 34.9) | 21.4 (20.8, 22.0) | 4.1 (3.8, 4.5) | |
| Predicted 10-year ASCVD risk† | |||||||
| <5% | 37.4 (36.7, 38.1) | 12.9 (12.5, 13.3) | 15.7 (15.3, 16.2) | 11.9 (11.5, 12.3) | 21.7 (21.3, 22.1) | 1.0 (0.3, 1.5) | |
| ≥5% and <10% | 71.7 (70.5, 72.9) | 39.9 (38.2, 41.5) | 52.5 (51.1, 53.8) | 36.5 (35.1, 37.9) | 19.2 (18.8, 19.7) | 3.4 (2.8, 4.1) | |
| ≥10% and <20% | 79.4 (78.2, 80.6) | 55.1 (53.5, 56.7) | 65.0 (63.6, 66.5) | 48.2 (46.6, 49.7) | 14.4 (14.1, 14.8) | 6.9 (6.5, 7.2) | |
| ≥20% | 92.1 (91.1, 93.1) | 58.8 (57.2, 60.5) | 85.1 (83.8, 86.5) | 62.7 (60.9, 64.5) | 7.0 (6.6, 7.6) | −3.9 (−5.0, −3.2) | |
| History of CVD | |||||||
| Yes | 37.3 (36.5, 38.0) | 54.8 (52.4, 57.2) | 22.7 (22.1, 23.3) | 41.8 (39.3, 44.3) | 14.6 (14.1, 15.2) | 13.0 (15.4, 12.0) | |
| No | 55.3 (54.4, 56.1) | 18.6 (17.9, 19.2) | 29.2 (28.4, 29.9) | 15.0 (14.4, 15.6) | 26.1 (25.7, 26.7) | 3.6 (2.5, 5.1) | |
Values are presented as weighted % (95% confidence interval).
ACC/AHA = American College of Cardiology/American Heart Association; ASCVD = atherosclerotic cardiovascular disease; CVD = cardiovascular disease; KSH = Korean Society of Hypertension.
*Number of ASCVD risk factors are based on the 2018 KSH guideline. †Predicted 10-year ASCVD risk is derived from the Korean Risk Prediction Model.
Figure 1. Number and percent of participants with hypertension, recommendation for pharmacological antihypertensive treatment, and BP above goal among study participants according to the 2017 ACC/AHA and the 2018 KSH guidelines. Treatment recommendation based on the KRPM.
ACC/AHA = American College of Cardiology/American Heart Association; BP = blood pressure; KRPM = Korean Risk Prediction Model; KSH = Korean Society of Hypertension.
Eligibility for antihypertensive treatment
In Korea, of the 9.4 million people with hypertension according to KSH criteria, 15.0% (95% CI, 14.6–15.3) were currently receiving one or more antihypertensive drugs, whereas 19.3% (95% CI, 18.8–19.7) were recommended antihypertensive medication in addition to lifestyle modifications (Table 3 and Figure 1). Similarly, by the ACC/AHA guideline, 20.9% (95% CI, 20.4–21.4) were recommended for antihypertensive medication, a mere 1.6% (95% CI, 0.9–3.0) addendum by the Korean guideline, relatively miniscule to 20.4% increase in prevalence. Those recommended for antihypertensive medication by the ACC/AHA guideline but not the KSH guideline primarily originated from older subgroups, with the most distinguished contribution from age 60 to 69 years by 5.3% (95% CI, 4.8–5.9); in contrast, almost no additional participants were recommended for pharmacological intervention in younger subgroups (age 20 to 29 years, 0.2%; age 30 to 39 years, 0.4%). Moreover, participants recommended for antihypertensive medication only by the ACC/AHA guideline had a higher mean number of ASCVD risk factors defined by the KSH guideline and the highest proportion with 10-year ASCVD risk between 10% to 20% by the KRPM. Yet, despite the 7.0% increase in hypertension prevalence with the lowered BP cutoff, 3.9% less participants with predicted 10-year ASCVD risk equivalent to or higher than 20% were recommended antihypertensive medication by the ACC/AHA guideline than by the KSH guideline. Additional 13.0% of the participants whom reported affirmative to previous cardiovascular morbidity were recommended by the ACC/AHA but not by the KSH guidelines. No sex differences were observed.
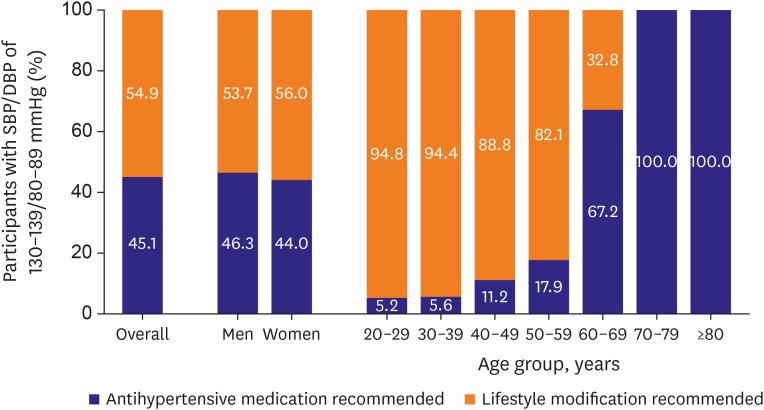
Figure 2 characterizes 45.1% of the participants with SBP/DBP of 130 to 139/80 to 89 mmHg, whom were recommended antihypertensive medication only by the ACC/AHA guideline. These individuals are recommended for antihypertensive medication, because they are qualified as stage 1 hypertension by the ACC/AHA guideline, has history of CVD, a 10-year predicted ASCVD risk equal to or exceeding 10% according to KRPM, DM, or CKD; or are ≥65 years of age with SBP between 130 and 139 mmHg. The proportion of recommended individuals exponentially increased with older age. Adherence to the PCE yielded similar results, where additional 1.6% of participants of age 20 to 29 years were recommended treatment but reaching the entirety by the seventh decade (Supplementary Figure 2).
Figure 2. Percentage of participants with SBP of 130–139 mmHg or DBP of 80–89 mmHg recommended for antihypertensive medication according to the 2017 ACC/AHA guideline. A 10-year predicted risk for ASCVD is based on the KRPM.
ACC/AHA = American College of Cardiology/American Heart Association; ASCVD = atherosclerotic cardiovascular disease; DBP = diastolic blood pressure; KNHANES = Korean National Health and Nutrition Examination Survey; KRPM = Korean Risk Prediction Model; SBP = systolic blood pressure.
Blood pressure above target
Among Korean adults taking antihypertensive medication, 45.6% (95% CI, 44.4–46.8) had not achieved target BP according to the KSH guideline compared with 61.7% (95% CI, 60.5–62.9) with above-goal BP according to the ACC/AHA guideline (Table 4 and Figure 1). This translates to overall 16.1% additional participants with unmet goal BP by the American guideline, thereby in need of treatment intensification. By the Korean guideline, the youngest subgroup had the lowest proportion of unachieved BP (36.2% in age 20 to 29 years), which incrementally escalated to 50.3% by age 70 to 79 years. However, with the lowering of target BP from 140 mmHg by the KSH guideline to 130 mmHg for general population and different subgroup-specific target BPs by the ACC/AHA guideline, older participants, in contrast, were more likely to attain target BP. The difference in proportion of the participants with unattained BP goal by the 2 guidelines was most pronounced among young adults, especially in age group 30 to 39 (38.4%). Once again, not much sex differences were observed within each guideline in regard to target BP attainment; adopting the ACC/AHA guideline included additional 17.9% male and 14.5% female participants with unmet BP goal than adhering to the KSH guideline. Participants with BP above goal according to the ACC/AHA guideline but not to the KSH guideline had relatively low to moderate number (0 to 2) and level (highest in <5% group) of ASCVD risk by both algorithms (Table 4 and Supplementary Table 2).
Table 4. Percentage of study participants taking antihypertensive medication with BP above treatment goals recommended by the 2017 ACC/AHA and the 2018 KSH guidelines.
| Variables | BP above goal according to | 2017 ACC/AHA but not 2018 KSH | ||
|---|---|---|---|---|
| 2017 ACC/AHA guideline | 2018 KSH guideline | |||
| Overall | 61.7 (60.5–62.9) | 45.6 (44.4–46.8) | 16.1 (15.2–16.8) | |
| Age group (year) | ||||
| 20–29 | 63.1 (26.0–100.0) | 36.2 (5.7–66.7) | 26.9 (26.5–27.4) | |
| 30–39 | 84.5 (78.4–90.6) | 46.1 (37.1–55.2) | 38.4 (38.1–38.8) | |
| 40–49 | 74.9 (71.5–78.4) | 42.1 (38.2–46.0) | 32.8 (32.2–33.3) | |
| 50–59 | 69.1 (66.8–71.4) | 42.4 (40.0–44.9) | 26.7 (26.1–27.1) | |
| 60–69 | 56.6 (54.7–58.5) | 45.1 (43.2–47.1) | 11.5 (11.2–12.0) | |
| 70–79 | 54.7 (52.7–56.8) | 50.3 (48.3–52.3) | 4.4 (3.9–5.0) | |
| 80+ | 53.8 (49.8–57.8) | 48.6 (44.5–52.6) | 5.2 (5.0–5.5) | |
| Sex | ||||
| Male | 63.5 (61.8–65.2) | 45.6 (43.8–47.3) | 17.9 (17.5–18.6) | |
| Female | 60.1 (58.6–61.6) | 45.6 (44.1–47.1) | 14.5 (14.2–14.8) | |
| Number of ASCVD risk factors* | ||||
| 0 | 58.6 (53.8–63.5) | 35.2 (30.3–40.1) | 23.4 (23.0–23.8) | |
| 1–2 | 61.7 (60.0–63.5) | 38.3 (36.5–40.0) | 23.4 (23.1–23.8) | |
| ≥3 | 62.3 (60.7–63.9) | 49.0 (47.3–50.6) | 13.3 (12.7–13.8) | |
| Predicted 10-year ASCVD risk† | ||||
| <5% | 65.2 (62.4–67.9) | 28.7 (26.0–31.4) | 36.5 (36.3–36.8) | |
| ≥5% and <10% | 65.2 (62.8–67.5) | 40.5 (38.0–43.0) | 24.7 (24.3–25.0) | |
| ≥10% and <20% | 57.3 (55.3–59.2) | 50.5 (48.5–52.4) | 6.8 (6.1–7.5) | |
| ≥20% | 61.1 (59.2–63.0) | 57.2 (55.2–59.1) | 3.9 (3.7–4.3) | |
| History of CVD | ||||
| Yes | 57.7 (55.9–59.5) | 36.8 (35.1–38.5) | 20.9 (20.0–21.6) | |
| No | 60.0 (57.1–63.0) | 58.5 (55.5–61.5) | 1.5 (0.9–1.9) | |
Values are presented as weighted % (95% confidence interval).
ACC/AHA = American College of Cardiology/American Heart Association; ASCVD = atherosclerotic cardiovascular disease; BP = blood pressure; CVD = cardiovascular diseases; KSH = Korean Society of Hypertension.
*Number of ASCVD risk factors are based on the 2018 KSH guideline. †Predicted 10-year ASCVD risk is derived from the Korean Risk Prediction Model.
DISCUSSION
We documented and compared the implications in adopting the 2 contemporary BP guidelines in Korean population. Specifically, we assessed the sex- and age-specific impact on prevalence of hypertension, recommendation for antihypertensive medication, and BP goals with antihypertensive drug treatment. Overall, the prevalence of hypertension was markedly higher by the ACC/AHA guideline due to the lowered BP cutoff than by the KSH guideline. Yet, when incorporating age, predicted 10-year ASCVD risk, comorbidity/target organ damage alongside, there was only a marginal (1.6%) increase in the percentage of adults who are suggested pharmacological approach only by the ACC/AHA guideline. On the other hand, among treated participants, 16.1% would not meet BP goal according to the ACC/AHA guideline These findings also concur with the pattern of increased hypertension prevalence when ACC/AHA guideline is applied on US population.15)
The ACC/AHA guideline's shift to lowered BP cutoff was supported by rigorous systematic evidence from prospective epidemiologic studies and randomized trials; they demonstrated that even mildly elevated BP would increase risk for adverse cardiac outcomes, and lowering of SBP below 130 mmHg would reduce CVD risk.16),17),18) A previous meta-analysis showed that lowering of usual SBP or DBP was associated with graded reduction in risk for all stroke and cerebral heart disease mortality without definite lower threshold.16) A recent Korean study also confirmed that SBP 130–139/DBP 80–89 mmHg was associated with significantly higher CVD risk compared to SBP <120/DBP<80 mmHg across the entire lifespan of age 20–94 years.19)
However, despite the substantial increase in prevalence by the ACC/AHA guideline, the increase in candidate for antihypertensive medications is relatively miniscule. The lowered BP cutoff by the ACC/AHA guideline therefore underscores the emphasis of early preventive measures and lifestyle modifications, especially for young adults, in whom lifestyle modification is central to high BP management and cardiovascular health promotion.20) After cumulative high BP exposure, BP reduction later in life may not completely restore CVD risks to ideal levels in these individuals.21)
On the other hand, for older individuals, treatment of SBP 130–139/DBP 80–89 mmHg according to the ACC/AHA guideline would almost always result in pharmacological treatment, as the 10-year risk function is largely age-driven. However, it is clinically challenging to attain intensive BP control without concerns for extremely low DBP and the associated risk of myocardial hypoperfusion and mortality.18) Furthermore, upon population aging in Korea, the number of very old individuals exhibiting frailty and multimorbidity would rapidly increase.22) Treatment intensification and sustainment may be complicated in the presence of high risks for adverse events including syncope and falls.23) Given the shortage of trials that have included older patients with poor functional status, the benefit-to-risk ratio of aggressive antihypertensive treatment should be carefully weighed via an individualized approach.
It is important to note that the risk factor profiles and the absolute CVD risks largely differ by ethnicity. A multiethnic study has illustrated heterogeneous distributions of unfavorable BP, lipid, and glucose levels, and smoking status among diverse countries, resulting in variations in the burden of CVD attributable to risk factor clusters.24) Moreover, the 10-year ASCVD risk rarely exceeds 10% before the sixth decade of life in Koreans.19) Such low overall 10-year risk challenges us to yield adequate risk threshold for therapeutic decisions. A longer-term and population-specific estimation of ASCVD risk may be needed to identify high-risk patients at earlier age for individualized risk-based clinical decisions and doctor-patient communications.25)
Lastly, the public health implications of the new guidelines should be discussed at both individual and population levels. By the ACC/AHA guideline, approximately 7.4 million adults would now be burdened with the risk of psychological morbidity or social stigma26) due to the label of hypertension. Beyond, with additional 0.4 million adults newly requiring pharmacological intervention and 1 million existing patients requiring more aggressive treatment, such expansion of treatment scope and intensity may substantially increase disease burden and health expenditure.27) The cost-effectiveness of lowering BP cutoff in Korea should be further studied in detail. Moreover, previous findings suggest considerable racial and socioeconomic disparities in the management of hypertension.28) The differences in population structure, social environmental factors, and healthcare systems should be considered when applying the ACC/AHA guideline to Korean population.
Our study is distinguished in several ways. To the extent of our knowledge, this is the first study to comprehensively examine and to compare the potential impacts of the recent guidelines embodying different BP diagnostic and treatment criteria on Korean population. Our results delineate how additional hypertension diagnosis by the ACC/AHA guideline would theoretically affect the treatment expectations as well as substantiality of resources needed to be deployed for such new inclusions. With the usage of KNHANES, the study results can be generalized and extrapolated to establish framework for anteceding BP guidelines and healthcare policies in Korea.
Despite the timely clinical implications and robustness of the dataset, our study also has limitations. The key variables are collected from single-occasion measurements and self-report. Despite standardized protocols and calibrated tools used, data collection processes are subjected to measurement error and recall bias. One particular area of concern is misclassification of hypertension status due to white coat hypertension. Confirmatory studies using repeated and sporadic measurements from both clinic and ambulatory settings would yield more stable representation of BP levels. Moreover, our study is based on Korean adults aged 20 or above; the findings may have limited generalizability to children/adolescents or to populations of different structure, healthcare system, individual biology, and lifestyle.
In conclusion, the adoption of the 2017 ACC/AHA guideline would yield only modest percentage increase overall in Korean adults recommended for antihypertensive medication but selectively in older individuals. Furthermore, over 61% of treated individuals would have BP above target and thereby be laden with more intensive antihypertensive drug therapy in adherence to the ACC/AHA guideline. While randomized trials and observational studies generally support intensive BP control, lowering the definition of hypertension requires a framework of individualized CVD risk prediction accounting for the risk distribution among Korean population. Future studies should also address cost-effectiveness and social implications of incorporating lower BP criteria in Korea. Although the new BP cutoff was not adopted to the 2018 KSH guideline, inclination towards lower population BP, with emphasis on early lifestyle modifications, would eventually lead to more timely and proactive CVD prevention in Korea.
ACKNOWLEDGMENTS
We are grateful to all participants of Korea National Health and Nutrition Examination Survey (KNHANES). We also appreciate the contributions of physicians, medical technicians, interviewers, and the expert committees for organizing and publishing of KNAHNES data.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Cho SMJ, Lee H, Kim HC
- Data curation: Cho SMJ, Lee H.
- Formal analysis: Cho SMJ, Lee H.
- Investigation: Cho SMJ, Lee H.
- Methodology: Cho SMJ, Lee H, Kim HC.
- Resources: Cho SMJ, Lee H.
- Software: Cho SMJ, Lee H.
- Supervision: Kim HC.
- Validation: Cho SMJ, Lee H.
- Visualization: Cho SMJ, Lee H.
- Writing - original draft: Cho SMJ, Lee H.
- Writing - review & editing: Cho SMJ, Lee H, Kim HC.
SUPPLEMENTARY MATERIALS
Percentage of study participants, meeting the definition for hypertension and recommended antihypertensive medication according to the 2017 ACC/AHA and the 2018 KSH guidelines
Percentage of study participants taking antihypertensive medication with BP above treatment goals recommended by the 2017 ACC/AHA and the 2018 KSH guidelines
Number and percent of participants with hypertension, recommendation for pharmacological antihypertensive treatment, and BP above goal among study participants according to the 2017 ACC/AHA and the 2018 KSH guidelines. Treatment recommendation based on the Pooled Cohort Equation.
Percentage of participants with SBP of 130–139 mmHg or DBP of 80–89 mmHg recommended for antihypertensive medication according to the 2017 ACC/AHA guideline. A 10-year predicted risk for ASCVD is based on the Pooled Cohort Equation.
References
- 1.GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1923–1994. doi: 10.1016/S0140-6736(18)32225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 3.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–115. doi: 10.1161/HYP.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 4.Cho SMJ, Lee HK, Kim HC, et al. Differences in prevalence of hypertension subtypes according to the 2018 Korean Society of Hypertension and 2017 American College of Cardiology/American Heart Association guidelines: The Korean National Health and Nutrition Examination Survey, 2007–2017 (KNHANES IV–VII) Clin Hypertens. 2019;25:26. doi: 10.1186/s40885-019-0129-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Williamson JD, Supiano MA, Applegate WB, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016;315:2673–2682. doi: 10.1001/jama.2016.7050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–967. doi: 10.1016/S0140-6736(15)01225-8. [DOI] [PubMed] [Google Scholar]
- 7.Kweon S, Kim Y, Jang MJ, et al. Data resource profile: the Korea national Health and Nutrition Examination Survey (KNHANES) Int J Epidemiol. 2014;43:69–77. doi: 10.1093/ije/dyt228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chadachan VM, Ye MT, Tay JC, Subramaniam K, Setia S. Understanding short-term blood-pressure-variability phenotypes: from concept to clinical practice. Int J Gen Med. 2018;11:241–254. doi: 10.2147/IJGM.S164903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim MK, Ko SH, Kim BY, et al. 2019 Clinical practice guidelines for type 2 diabetes mellitus in Korea. Diabetes Metab J. 2019;43:398–406. doi: 10.4093/dmj.2019.0137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rhee EJ, Kim HC, Kim JH, et al. 2018 Guidelines for the management of dyslipidemia. Korean J Intern Med. 2019;34:723–771. doi: 10.3904/kjim.2019.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kidney Disease: Improving Global Outcomes (KDIGO) Hepatitis C Work Group. KDIGO 2018 clinical practice guideline for the prevention, diagnosis, evaluation, and treatment of hepatitis C in chronic kidney disease. Kidney Int Suppl (2011) 2018;8:91–165. doi: 10.1016/j.kisu.2018.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jung KJ, Jang Y, Oh DJ, et al. The ACC/AHA 2013 pooled cohort equations compared to a Korean Risk Prediction Model for atherosclerotic cardiovascular disease. Atherosclerosis. 2015;242:367–375. doi: 10.1016/j.atherosclerosis.2015.07.033. [DOI] [PubMed] [Google Scholar]
- 14.Goff DC, Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American college of cardiology/American heart association task force on practice guidelines. Circulation. 2014;129:S49–73. doi: 10.1161/01.cir.0000437741.48606.98. [DOI] [PubMed] [Google Scholar]
- 15.Muntner P, Carey RM, Gidding S, et al. Potential US population impact of the 2017 ACC/AHA high blood pressure guideline. Circulation. 2018;137:109–118. doi: 10.1161/CIRCULATIONAHA.117.032582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 17.Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people. Lancet. 2014;383:1899–1911. doi: 10.1016/S0140-6736(14)60685-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Böhm M, Schumacher H, Teo KK, et al. Achieved blood pressure and cardiovascular outcomes in high-risk patients: results from ONTARGET and TRANSCEND trials. Lancet. 2017;389:2226–2237. doi: 10.1016/S0140-6736(17)30754-7. [DOI] [PubMed] [Google Scholar]
- 19.Lee H, Cho SM, Park JH, Park S, Kim HC. 2017 ACC/AHA blood pressure classification and cardiovascular disease in 15 million adults of age 20–94 years. J Clin Med. 2019;8:1832. doi: 10.3390/jcm8111832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang MH, Kang SY, Lee JA, et al. The effect of lifestyle changes on blood pressure control among hypertensive patients. Korean J Fam Med. 2017;38:173–180. doi: 10.4082/kjfm.2017.38.4.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu K, Colangelo LA, Daviglus ML, et al. Can antihypertensive treatment restore the risk of cardiovascular disease to ideal levels?: the Coronary Artery Risk Development in Young Adults (CARDIA) Study and the Multi-Ethnic Study of Atherosclerosis (MESA) J Am Heart Assoc. 2015;4:e002275. doi: 10.1161/JAHA.115.002275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chon D, Lee Y, Kim J, Lee KE. The association between frequency of social contact and frailty in older people: Korean Frailty and Aging Cohort Study (KFACS) J Korean Med Sci. 2018;33:e332. doi: 10.3346/jkms.2018.33.e332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Benetos A, Petrovic M, Strandberg T. Hypertension management in older and frail older patients. Circ Res. 2019;124:1045–1060. doi: 10.1161/CIRCRESAHA.118.313236. [DOI] [PubMed] [Google Scholar]
- 24.Peters SAE, Wang X, Lam TH, et al. Clustering of risk factors and the risk of incident cardiovascular disease in Asian and Caucasian populations: results from the Asia Pacific Cohort Studies Collaboration. BMJ Open. 2018;8:e019335. doi: 10.1136/bmjopen-2017-019335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dorresteijn JA, Kaasenbrood L, Cook NR, et al. How to translate clinical trial results into gain in healthy life expectancy for individual patients. BMJ. 2016;352:i1548. doi: 10.1136/bmj.i1548. [DOI] [PubMed] [Google Scholar]
- 26.Panza GA, Puhl RM, Taylor BA, Zaleski AL, Livingston J, Pescatello LS. Links between discrimination and cardiovascular health among socially stigmatized groups: a systematic review. PLoS One. 2019;14:e0217623. doi: 10.1371/journal.pone.0217623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee JY, Jo MW, Yoo WS, Kim HJ, Eun SJ. Evidence of a broken healthcare delivery system in Korea: unnecessary hospital outpatient utilization among patients with a single chronic disease without complications. J Korean Med Sci. 2014;29:1590–1596. doi: 10.3346/jkms.2014.29.12.1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee H, Park JH, Floyd JS, Park S, Kim HC. Combined effect of income and medication adherence on mortality in newly treated hypertension: nationwide study of 16 million person-years. J Am Heart Assoc. 2019;8:e013148. doi: 10.1161/JAHA.119.013148. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Percentage of study participants, meeting the definition for hypertension and recommended antihypertensive medication according to the 2017 ACC/AHA and the 2018 KSH guidelines
Percentage of study participants taking antihypertensive medication with BP above treatment goals recommended by the 2017 ACC/AHA and the 2018 KSH guidelines
Number and percent of participants with hypertension, recommendation for pharmacological antihypertensive treatment, and BP above goal among study participants according to the 2017 ACC/AHA and the 2018 KSH guidelines. Treatment recommendation based on the Pooled Cohort Equation.
Percentage of participants with SBP of 130–139 mmHg or DBP of 80–89 mmHg recommended for antihypertensive medication according to the 2017 ACC/AHA guideline. A 10-year predicted risk for ASCVD is based on the Pooled Cohort Equation.