Abstract
Background
Pregnancy in women with epilepsy (WWE) is known to have a higher risk for fetal development complications, which may include congenital malformations. Unfortunately, information pertaining to pregnancy in WWE is difficult to obtain because there are considerable ethical issues preventing these studies from being conducted on pregnant women. Therefore, this study investigated the pregnancies of Korean WWE in a tertiary epilepsy center to observe data resulting from the outcome of the pregnancies.
Methods
This was a retrospective study of 48 pregnant WWE who were treated at the regional tertiary epilepsy center. All records of hospital visits before and after the period of pregnancy were analyzed to obtain information about the seizures as well as pregnancy-related outcomes, including the status of the newborns' conditions.
Results
The subject group consisted of 31 (63.3%) with partial epilepsy, 6 (12.5%) with generalized epilepsy, and 11 (22.9%) with unclassified epilepsy. There were 27 subjects who took one antiepileptic drug (AED), and 12 who took two AEDs. The most commonly used drug was lamotrigine (29.8%). Of the 48 WWE involved in the study, 31 underwent caesarian sections and 17 opted for natural birth. Thirty-nine (81.3%) delivered at full-term, but 9 (18.7%) delivered at preterm. Compared to full-term infants, pre-mature infants showed lower birth weight, smaller head circumference, shorter height, and lower 1-minute Apgar scores, but seizure frequencies of the mothers did not differ.
Conclusion
In WWE, epilepsy classification, number of AEDs taken, and frequency of seizures are not significantly correlated with delivery and fetal condition. This data could be used as a clinical reference for physicians to provide useful information to WWE if they are concerned about their pregnancies.
Keywords: Pregnancy, Epilepsy, Antiepileptic Drugs
Graphical Abstract
INTRODUCTION
Women with epilepsy (WWE) who are pregnant have reported various effects related to either the epilepsy itself or as a result of taking antiepileptic drugs (AEDs).1 Taking an AED during pregnancy may make some WWE anxious in addition to arousing the misconception that epilepsy is a hereditary disease. This can lead to WWE hesitating to follow through with a pregnancy.
The European Registry of Antiepileptic Drugs and Pregnancy reported 33.4% of WWE experienced seizures during pregnancy. Seizure frequency was increased in 15.8% of these women, reduced in 12.0%, and unchanged in 70.5%.2 The reasons for seizure recurrence during pregnancy are multifactorial. Some causes include decreased use of prescribed AEDs due to fear of harming the baby, physical changes such as hormonal fluctuations, and higher estrogen-to-progesterone ratio. Sleep deprivation and psychosocial stress may also contribute to seizure recurrence.3
In East Asia, many people hold traditional beliefs and stigmas against certain health conditions, with epilepsy being one of these conditions. These beliefs, often rooted in non-academic reasoning, can cause issues with providing patients proper education and treatment of their condition. Without a concerted effort to provide accurate medical information regarding this subject matter, these issues will continue to be unresolved. Unfortunately, information is difficult to obtain when there are considerable ethical issues preventing these studies from being conducted on pregnant women. Additionally, the small amount of information that exists on this matter involves tests conducted on Caucasian subjects, and does not take ethnic diversity into account. Therefore, there is growing interest in the role of ethnicity on pregnancy outcomes in WWE.4 This study investigated the pregnancies of Korean WWE in a tertiary epilepsy center to observe data resulting from the outcome of the pregnancies.
METHODS
All pregnancies of the WWE in this study were retrospectively reviewed using electronic medical records from August 2015 to March 2018 at a regional tertiary epilepsy center. Upon using the keywords “pregnancy” and “epilepsy” in a collection of 51 consecutive WWE pregnancy records, 48 of the cases were enrolled in the study. Of the 51 cases that were initially examined, 2 were excluded due to unknown information regarding the full term of the pregnancies and 1 was a terminated pregnancy due to the mother's anxieties about the possible effects of AEDs on the fetus. Seizure frequency was categorized by the research team as A (completely seizure free or only auras), B (1 to 3 seizure days ± auras per year), C (4 to 12 seizure days ± auras per year), and D (> 12 seizure days ± auras per year).
All records of hospital visits before and after the period of pregnancy were analyzed to obtain information about the seizures as well as pregnancy-related outcomes, including the status of the newborns' conditions.
Descriptive statistics and frequency analysis were performed to determine the pregnant WWE and newborn characteristics. In order to compare data aspects such as gestational period, number of AEDs taken, birth weight, and demographic characteristics, the Kolmogorov-Smirnov method was used and did not indicate sample normality. Thus, non-parametric Mann-Whitney tests, as well as χ2 tests and Fisher's exact tests, were used. The Kruskal-Wallis test was used for comparing seizure frequency categories. Data analysis was performed using SPSS version 25.0, and P < 0.05 was considered statistically significant.
Ethics statement
The study protocol was reviewed and approved by the Institutional Review Board of the Dongsan Medical Center (approval No. 2018-05-036). Informed consent was waived because of the study's retrospective design.
RESULTS
The enrolled subjects included 48 Korean WWE with 49 babies, which included one set of twins. The average age of the WWE at the time of pregnancy was 33.13 ± 4.34 years and body mass index (BMI) was 21.77 ± 4.12 upon initial visit. The final pre-birth visit average BMI was 26.91 ± 4.31 (Table 1).
Table 1. Baseline characteristic of pregnancy in WWE (n = 48).
| Characteristics | Values | |
|---|---|---|
| Age, yr | 33.13 ± 4.34 | |
| BMI at the first visit | 21.77 ± 4.12 | |
| BMI at the delivery | 26.91 ± 4.31 | |
| High-risk pregnancy, exclude epilepsy, yes | 14 (29.2) | |
| Pregnancy of old age | 2 (14.3) | |
| Placenta previa | 2 (14.3) | |
| Incompetent internal os of cervix | 2 (14.3) | |
| Intrauterine growth restriction | 3 (21.4) | |
| Pre-eclampsia | 1 (7.1) | |
| Preterm labor | 1 (7.1) | |
| Gestational DM | 2 (14.3) | |
| Twin | 1 (7.1) | |
| Methods of pregnancy | ||
| Normal pregnancy | 44 (91.7) | |
| In vitro fertilization | 2 (4.2) | |
| Ovulation induction | 2 (4.2) | |
| Pregnancy time | ||
| First | 19 (39.6) | |
| Second | 19 (39.6) | |
| Third | 6 (12.5) | |
| Forth | 3 (6.3) | |
| Fifth | 1 (2.1) | |
Values are presented as mean ± standard deviation or number (%).
WWE = women with epilepsy, BMI = body mass index, DM = diabetes mellitus.
High-risk pregnancy was evident in 14 (29.2%) patients. There were 3 cases of developmental delays in the uterus, 2 gestational diabetes, 2 placenta previa, 2 cervical incompetence, 2 mothers over the age of 35, 1 preeclampsia, 1 twin pregnancy, and 1 premature labor pains. Pregnancy occurred naturally in 44 (91.7%) patients, 2 (4.2%) through in vitro fertilization, and 2 (4.2%) with stimulated ovulation. The number of times the subjects experienced pregnancy ranged from 1 to 5. Of the total subjects, 19 (39.6%) were experiencing their first pregnancy and 19 (39.6%) their second pregnancy.
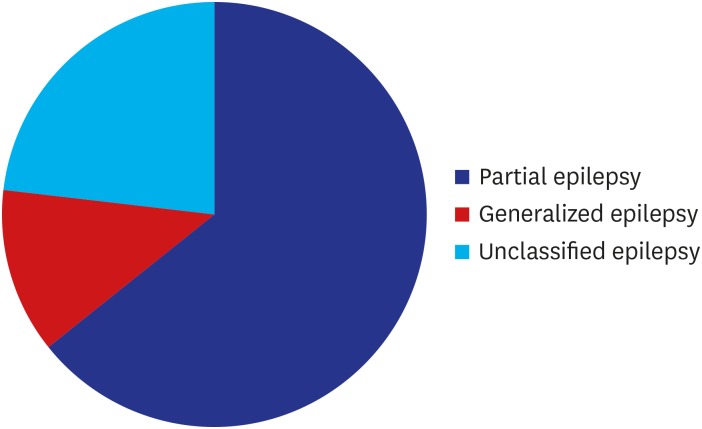
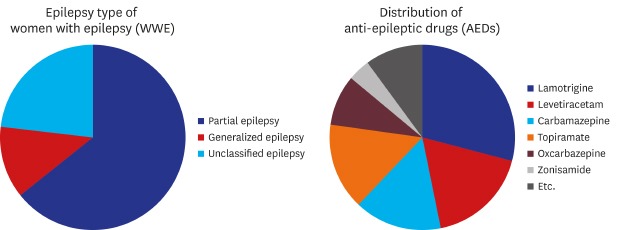
The WWE consisted of 31 (63.3%) with partial epilepsy, 6 (12.5%) with generalized epilepsy, and 11 (22.9%) with unclassified epilepsy (Fig. 1). One subject (2.1%) had a family history of epilepsy. For seizure frequency before pregnancy, 29 (60.4%) were in category A, 8 (16.7%) in B, and 11 (22.9%) in C and D combined.
Fig. 1. Epilepsy type of women with epilepsy.
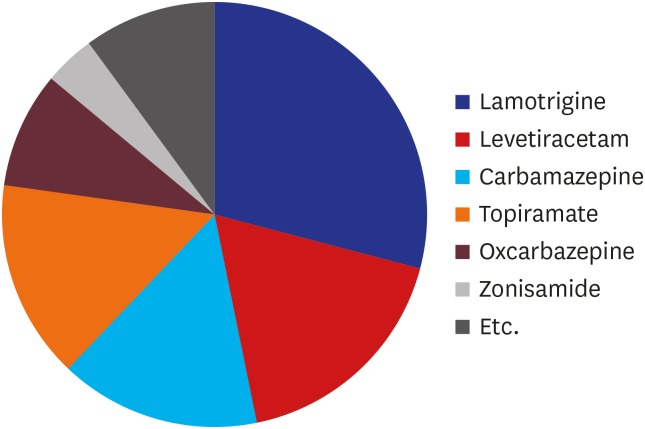
There were abnormal electroencephalography findings in 35 (72.9%) of the 48 subjects. Among 33 subjects with available magnetic resonance imaging (MRI) information, 17 (51.5%) showed MRI abnormalities. During pregnancy, 27 (56.3%) of the subjects took one AED, 12 (25.0%) took two AEDs, 6 (12.5%) took three AEDs, 2 (4.2%) took four AEDs, and 1 (2.1%) took no AEDs. Among the 47 WWE taking AEDs, 23 (48.9%) took lamotrigine in doses of 25–550 mg, 14 (29.8%) levetiracetam 250–2,000 mg, 12 (25.5%) carbamazepine 200–900 mg, 12 (25.5%) topiramate 50–400 mg, and 7 (14.9%) oxcarbazepine 600–1,200 mg. Other drugs taken included zonisamide, phenytoin, clonazepam, gabapentin, valproate, and pregabalin (Fig. 2).
Fig. 2. Distribution of antiepileptic drugs.
Among 48 patients, the method of delivery included 31 (64.6%) caesarian sections (CS) and 17 (35.4%) natural births (Table 2). Of the 31 CS patients, 14 had already undergone CS in a previous pregnancy due to breech, cephalopelvic disproportion (CPD), pain, seizure, induction failure, or gestational hypertension. Additionally, there were 5 cases of CPD, 2 premature rupture of membranes (PROM), 2 placenta previa partialis, 2 extreme pain, 2 mothers > 35 years old, 1 fetal heart rate deceleration, 1 uterine myoma, 1 gestational diabetes mellitus (GDM), and 1 preeclampsia. None of the mothers chose CS because of epilepsy prevalence, even if the frequency of seizures worsened during pregnancy. Of the total subject population, 28 (58.3%) did not have any children while they were pregnant.
Table 2. Obstetric history in WWE (n = 48).
| Variables | Values | |||
|---|---|---|---|---|
| Delivery type | ||||
| Vaginal delivery, yes | 17 (35.4) | |||
| Caesarean section, yes | 31 (64.6) | |||
| Past experience | 14 (45.2) | |||
| CPD | 5 (16.1) | |||
| PROM | 2 (6.5) | |||
| Placenta previa patialis | 2 (6.5) | |||
| Pain | 2 (6.5) | |||
| Elderly pregnancy, age ≥ 35 | 2 (6.5) | |||
| Etc. | 4 (12.9) | |||
| Gestational age, wk | 37.81 ± 2.12 | |||
| Full term delivery, yes | 39 (81.3); 38.62 ± 0.99 | |||
| Vaginal delivery, yes | 15 (38.5) | |||
| Caesarean section, yes | 24 (61.5) | |||
| Preterm birth, yes | 9 (18.7); 34.33 ± 2.24 | |||
| Vaginal delivery, yes | 2 (22.2) | |||
| Caesarean section, yes | 7 (77.8) | |||
| Obstetric history | ||||
| No. of children = 0 (n = 28) | ||||
| Preterm labor, yes | 3 (10.7) | |||
| Abortion, yes | 6 (21.4) | |||
| One/two | 5 (17.9)/1 (3.6) | |||
| No. of children = 1 (n = 16) | ||||
| Full term delivery | 15 (93.8) | |||
| Preterm labor | 1 (6.3) | |||
| Abortion | 4 (25.0) | |||
| One/two | 3 (18.8)/1 (6.3) | |||
| No. of children = 2 (n = 2) | ||||
| Full term delivery | 2 (100.0) | |||
| No. of children = 3 (n = 2) | ||||
| Full term delivery | 2 (100.0) | |||
Values are presented as mean ± standard deviation or number (%).
WWE = women with epilepsy, CPD = cephalopelvic disproportion, PROM = premature rupture of membranes.
The mean gestational age was 37.81 ± 2.12 weeks. Full-term delivery occurred in 39 (81.3%) subjects with a 38.6 ± 1.0-week gestational age. Preterm labor occurred in 9 (18.7%) subjects with a mean of 34.3 ± 2.2 weeks. Compared to full-term infants, pre-mature infants showed lower birth weight, smaller head circumference, shorter height, and lower 1-minute Apgar scores, but seizure frequencies of the mothers did not differ (Table 3).
Table 3. Characteristics according to pregnancy duration.
| Variables | Full term delivery, 37–40 wk (n = 38) | Preterm birth, ≤ 36 wk (n = 10) | P value | |
|---|---|---|---|---|
| Age, yr | 32.85 ± 4.53 | 34.33 ± 3.28 | 0.390 | |
| BMI | ||||
| First visit | 21.49 ± 3.36 | 22.98 ± 6.64 | 0.621 | |
| Delivery | 26.92 ± 3.61 | 26.86 ± 6.87 | 0.775 | |
| No. of AEDs | 1.49 ± 0.79 | 2.11 ± 1.17 | 0.173 | |
| Delivery type | 0.459 | |||
| Vaginal delivery | 15 (39.5) | 2 (20.0) | ||
| C-sec | 23 (60.5) | 8 (80.0) | ||
| EEG, abnormal (F = 38, P = 10, n = 48) | 29 (76.3) | 6 (60.0) | 0.687 | |
| MRI, abnormal (F = 25, P = 8, n = 33) | 13 (52.0) | 4 (50.0) | 0.148 | |
| Seizure severity (n = 48) | 0.117 | |||
| A | 25 (65.8) | 2 (25.0) | ||
| B | 5 (13.2) | 3 (37.5) | ||
| C | 1 (2.6) | 0 (0.0) | ||
| D | 7 (18.4) | 3 (37.5) | ||
| Fetal | ||||
| Sex, male | 16 (80.0) | 4 (20.0) | 1.000 | |
| Height (n = 48) | 50.28 ± 2.31 | 44.45 ± 4.91 | < 0.001a | |
| Weight | 3,171.28 ± 453.03 | 1,916.00 ± 834.54 | < 0.001a | |
| Head circumference (n = 46) | 34.05 ± 1.69 | 30.19 ± 3.37 | 0.002a | |
| Apgar score | ||||
| 1 min (n = 46) | 7.68 ± 0.53 | 6.63 ± 0.92 | 0.007a | |
| 5 min (n = 46) | 8.95 ± 0.23 | 8.25 ± 0.89 | 0.108 | |
Values are presented as mean ± standard deviation or number (%).
BMI = body mass index, AED = antiepileptic drug, EEG = electroencephalography, MRI = magnetic resonance imaging.
aStatistical significance (P < 0.05).
A total of 49 babies were born which included one set of twins. There were 20 (40.8%) male and 29 (59.2%) female infants. The birth weight was 2,915.10 ± 744.54 g including 10 (20.4%) infants who were reported as underweight and 7 born prematurely. There was no significant difference in body weight at birth according to the type of maternal AED. The average cephalic presentation was observed as 33.38 ± 2.51, and 12 (26.1%) infants were smaller than the natural cephalic presentation, 5 of whom were premature. The mean Apgar score at one minute was 7.50 ± 0.72 and at five minutes was 8.83 ± 0.49. In the Apgar one-minute score, 1 infant scored 5 and 3 infants scored 6. These 4 infants required intensive care. However, their Apgar five-minute score was normal. There were no abnormalities in the infants.
Seizure frequency changes during pregnancy were evaluated compared to the 10 months prior to pregnancy (Table 4). The observation divided the subjects into 3 groups which were 9 (18.8%) patients with worse seizure frequency, 23 (47.9%) patients with unchanged frequency, and 16 (33.3%) with improved frequency. There was no specific trimester during which the seizures were aggravated. In the 5 subjects who experienced worsening seizures (placed in category D), 3 increased their dosage of lamotrigine, which was their prescribed AED. The other 2 subjects experienced worsening seizures due to improper medication adherence and sleep deprivation. In this case, we educated the patients on the proper way to administer their prescribed medication and suggested lifestyle modification to correct their sleep issues. Among these groups, there were no differences in pregnancy outcomes. In the worsened seizure frequency group, 2 patients underwent natural childbirth and 7 opted for CS. Among the 7 CS patients, there were 4 cases of repeated CS, 1 fetal HR deceleration, 1 placenta previa partialis, and 1 PROM. The unchanged seizure frequency group had 8 natural births and 15 CSs. Among those 15, there were 7 cases of repeated CS, 4 CPD, 1 uterine myoma, 1 early contraction pain, 1 preeclampsia, and 1 placenta previa partialis. In the improved seizure frequency group, there were 7 natural births and 9 CSs. Of those 9, there were 3 cases of repeated CS, 2 mothers > 35 years old, 1 PROM, 1 CPD, 1 GDM, and 1 early contraction pain. When comparing the groups according to seizure frequency during pregnancy, there were no differences in pregnancy outcomes. When comparing the groups according to fetal body weight, there were no differences in clinical characteristics of epilepsy (Table 5).
Table 4. Seizure frequency changing during pregnancy (n = 48).
| Variables | Worse (n = 9, 18.8%) | Same (n = 23, 47.9%) | Improve (n = 16, 33.3%) | P value | |
|---|---|---|---|---|---|
| Age, yr | 32.00 ± 3.08 | 33.91 ± 3.70 | 32.63 ± 5.74 | 0.276 | |
| BMI | |||||
| First visit | 22.41 ± 6.06 | 21.76 ± 2.91 | 21.43 ± 4.56 | 0.787 | |
| Delivery | 27.35 ± 3.82 | 26.95 ± 3.83 | 26.61 ± 5.36 | 0.990 | |
| No. of AEDs | 1.78 ± 0.83 | 1.4 ± 0.89 | 1.5 ± 0.73 | 0.374 | |
| Delivery type | 0.544 | ||||
| Vaginal delivery | 2 (22.22) | 8 (34.78) | 7 (43.75) | ||
| C-sec | 7 (77.78) | 15 (65.21) | 9 (56.25) | ||
| Gestational period, wk | 37.44 ± 1.74 | 37.87 ± 2.07 | 37.94 ± 2.46 | 0.452 | |
| EEG, abnormal (W = 9, S = 23, I = 16, n = 48) | 7 (77.8) | 15 (65.2) | 13 (81.3) | 0.631 | |
| MRI, abnormal (W = 5, S = 16, I = 12, n = 33) | 3 (60.0) | 10 (62.5) | 3 (25.0) | 0.454 | |
| Seizure severity (n = 48) | 0.011a | ||||
| A | 1 (12.5) | 18 (81.8) | 8 (50.0) | ||
| B | 1 (12.5) | 2 (9.1) | 4 (25.0) | ||
| C | 0 (0.0) | 0 (0.0) | 1 (6.3) | ||
| D | 5 (62.5) | 2 (9.1) | 3 (18.8) | ||
| Baby | |||||
| Sex, male | 2 (10.0) | 11 (55.0) | 7 (35.0) | 0.409 | |
| Height | 49.56 ± 4.67 | 48.43 ± 4.08 | 49.79 ± 2.68 | 0.516 | |
| Weight | 2,757.78 ± 744.91 | 2,883.75 ± 776.12 | 3,050.63 ± 697.10 | 0.466 | |
| Head circumference | 34.06 ± 1.52 | 33.19 ± 2.99 | 33.32 ± 2.02 | 0.759 | |
| Apgar score | |||||
| 1 min (n = 46) | 7.57 ± 0.53 | 7.50 ± 0.83 | 7.47 ± 0.62 | 0.688 | |
| 5 min (n = 46) | 8.86 ± 0.38 | 8.83 ± 0.48 | 8.80 ± 0.54 | 0.883 | |
Values are presented as mean ± standard deviation or number (%).
BMI = body mass index, AED = antiepileptic drug, EEG = electroencephalography, MRI = magnetic resonance imaging.
aStatistical significance (P < 0.05).
Table 5. Characteristics according to fetal weight (n = 49).
| Variables | Underweight (n = 10) | Normal weight (n = 39) | P value | |
|---|---|---|---|---|
| Age, yr | 35.00 ± 3.06 | 32.64 ± 4.46 | 0.116 | |
| EEG, abnormal (U = 9, N = 39, n = 48) | 5 (55.6) | 30 (76.9) | 0.228 | |
| MRI, abnormal (U = 9, N = 25, n = 34) | 7 (77.8) | 11 (44.0) | 0.064 | |
| Seizure severity | 0.182 | |||
| A | 4 (44.4) | 23 (60.5) | ||
| B | 1 (11.1) | 7 (18.4) | ||
| C | 0 (0.0) | 1 (2.6) | ||
| D | 4 (44.4) | 7 (18.4) | ||
| Epilepsy type (n = 49) | 0.402 | |||
| Partial epilepsy | 6 (60.0) | 26 (66.7) | ||
| Generalized epilepsy | 0 (0.0) | 6 (15.4) | ||
| Unclassified epilepsy | 4 (40.0) | 7 (17.9) | ||
| No. of AEDs | 1.60 ± 1.26 | 1.56 ± 0.82 | 0.723 | |
| Seizure frequency before pregnancy | 1.10 ± 1.52 | 0.84 ± 1.44 | 0.573 | |
| Seizure frequency during pregnancy | 1.22 ± 2.95 | 0.67 ± 1.24 | 0.897 | |
| First visit BMI | 20.12 ± 8.85 | 21.63 ± 3.77 | 0.951 | |
| Delivery BMI | 23.89 ± 10.46 | 27.00 ± 3.71 | 0.855 | |
| Gestational period, wk | 34.50 ± 3.17 | 38.46 ± 1.21 | < 0.001a | |
| Delivery type | 0.174 | |||
| Vaginal delivery | 2 (20.0) | 15 (38.5) | ||
| C-sec | 8 (80.0) | 24 (61.5) | ||
Values are presented as mean ± standard deviation or number (%).
BMI = body mass index, AED = antiepileptic drug, EEG = electroencephalography, MRI = magnetic resonance imaging.
aStatistical significance (P < 0.05).
DISCUSSION
This study showed that high-risk pregnancy rates were lower in WWE compared to the general rate of pregnant Korean women. According to a review from the National Institute of Health Insurance Service, 39.7%–42.8% of all pregnant women were identified as high-risk pregnancies,5 but only 29.2% of WWE in our study were identified as high-risk pregnancies. These results are presumed because our study did not evaluate all women of childbearing potential with epilepsy. Additionally, WWE tend to avoid pregnancy due to stigma and fear of AED-related malformation, which further affects the accuracy of these statistics. Finally, this study did not take into account women who have previously experienced a terminated pregnancy or premature birth who may be hesitant to attempt pregnancy again.
Of the total subject population, more than three-quarters were taking either one or two AEDs. The most common AED was lamotrigine, followed by levetiracetam. Lamotrigine with Topiramate and lamotrigine with levetiracetam were the most common combinations of AEDs used by WWE during pregnancy. These particular AEDs are considered to hold a much lower risk of major congenital malformation compared to alternatives such as valproate, phenobarbital and phenytoin, so it does not come as a surprise that they were the most commonly used AEDs by the WWE in this study.6,7,8
He et al.4 reported a higher rate of CS in WWE compared to the general rate of pregnant women in China. The data from this Korean study also reports a higher rate of CS (64.6%) compared to natural birth (35.4%) in pregnant WWE. Women who had already undergone natural birth in a previous pregnancy were more likely to opt for natural birth again over CS. The proportion of high-risk pregnancies in WWE was lower, despite the higher CS rate compared to the general rate of pregnant women in Korea.5
Newborn babies who reached full gestational age made up 81.3% of the total, and even the premature babies showed a normal 5-minute Apgar score. Seizure frequency was not significantly correlated with preterm delivery. The number of AEDs taken by pregnant WWE was not associated with pregnancy, delivery, or the condition of the baby at birth. Additionally, epilepsy classification and seizure frequency were not significantly correlated with fetal weight. Also, according to the Apgar score results, the fetal health was not different in full-term births compared to preterm births.
Several studies have measured seizure frequency during pregnancy in WWE. In one study, 154 pregnancies were evaluated. Seizure frequency was unchanged in 54% of these pregnancies, decreased in 14%, and increased in 32% compared to pre-pregnancy seizure frequency.9 Another study recruited 78 pregnant subjects with 72% showing unchanged seizure frequency, 14% decreased frequency, and 14% increased frequency compared to the pre-pregnancy baseline.10 These results were similar to our study, in which more than half of the WWE had no change in the seizure frequency during their pregnancies. In this study there was no trimester during which seizures were particularly aggravated. Thus, there may be other factors involved in seizure aggravation aside from changing body weight or drug concentration.
Crump et al.11 reported that preterm birth was strongly associated with epilepsy in Swedish adults by the national cohort study, although AED prescriptions carried a relatively weaker association and preterm birth was independent of fetal growth. Several studies also suggested that more specific pregnancy planning can result in better seizure control during pregnancy and improved neonatal outcomes including congenital malformations.12,13 Although, our study did not evaluate the development of preterm babies born to WWE, it seems that epilepsy itself has a minimal effect on preterm birth and fetal health.
This study has several limitations, primarily related to the uniqueness of the study and the resulting lack of existing information on the subject. This study was a retrospective and single center study with a relatively small sample. However, there are currently no studies on pregnancy and childbirth in WWE in Korea, so referential information is scarce. Also, the authors are unable to evaluate the developmental results of children of WWE after birth. These limitations make it difficult to confirm the results of this study on a long-term basis. However, the authors suggest that this initial evaluation of the association between pregnancy and WWE in Korea is necessary to promote further research that confirms and expands on the results of this study.
In conclusion, this study shows that epilepsy classifications, the number of AEDs, and the frequency of seizures is not significantly correlated with delivery and fetal condition. The majority of the WWE in this study did not experience an increase in seizure frequency during their pregnancy. Although there are some limitations to the data collected, there was no indication that epilepsy has any significant negative effect on pregnancy. Thus, our data may be used to ease the fears of WWE who are hesitant to become pregnant or follow through with their pregnancy.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Cho YW.
- Data curation: Bae JG.
- Formal analysis: Jeon JY.
- Investigation: Kim KT, Bae JG, Cho YW.
- Methodology: Kim KT, Bae JG.
- Validation: Cho YW.
- Writing - original draft: Jeon JY, Cho YW.
- Writing - review & editing: Jeon JY, Cho YW.
References
- 1.Barrett C, Richens A. Epilepsy and pregnancy: report of an Epilepsy Research Foundation Workshop. Epilepsy Res. 2003;52(3):147–187. doi: 10.1016/s0920-1211(02)00237-1. [DOI] [PubMed] [Google Scholar]
- 2.Battino D, Tomson T, Bonizzoni E, Craig J, Lindhout D, Sabers A, et al. Seizure control and treatment changes in pregnancy: observations from the EURAP epilepsy pregnancy registry. Epilepsia. 2013;54(9):1621–1627. doi: 10.1111/epi.12302. [DOI] [PubMed] [Google Scholar]
- 3.Vélez-Ruiz NJ, Pennell PB. Issues for women with epilepsy. Neurol Clin. 2016;34(2):411–425. doi: 10.1016/j.ncl.2015.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.He S, Zhu H, Qiu X, Zhu X, Peng A, Duan J, et al. Pregnancy outcome in women with epilepsy in Western China: a prospective hospital based study. Epilepsy Behav. 2017;74:10–14. doi: 10.1016/j.yebeh.2017.05.034. [DOI] [PubMed] [Google Scholar]
- 5.Kim HY, Moon CS. Integrated care center for high risk pregnancy and neonate - an analysis of process and problems in obstetrics. Korean J Perinatol. 2014;25(3):140–152. [Google Scholar]
- 6.Hernández-Díaz S, Smith CR, Shen A, Mittendorf R, Hauser WA, Yerby M, et al. Comparative safety of antiepileptic drugs during pregnancy. Neurology. 2012;78(21):1692–1699. doi: 10.1212/WNL.0b013e3182574f39. [DOI] [PubMed] [Google Scholar]
- 7.Stephen LJ, Harden C, Tomson T, Brodie MJ. Management of epilepsy in women. Lancet Neurol. 2019;18(5):481–491. doi: 10.1016/S1474-4422(18)30495-2. [DOI] [PubMed] [Google Scholar]
- 8.Menon S, Siewe Fodjo JN, Weckhuysen S, Bhwana D, Njamnshi AK, Dekker M, et al. Women with epilepsy in sub-Saharan Africa: a review of the reproductive health challenges and perspectives for management. Seizure. 2019;71:312–317. doi: 10.1016/j.seizure.2019.08.016. [DOI] [PubMed] [Google Scholar]
- 9.Bardy AH. Incidence of seizures during pregnancy, labor and puerperium in epileptic women: a prospective study. Acta Neurol Scand. 1987;75(5):356–360. doi: 10.1111/j.1600-0404.1987.tb05459.x. [DOI] [PubMed] [Google Scholar]
- 10.Gjerde IO, Strandjord RE, Ulstein M. The course of epilepsy during pregnancy: a study of 78 cases. Acta Neurol Scand. 1988;78(3):198–205. doi: 10.1111/j.1600-0404.1988.tb03646.x. [DOI] [PubMed] [Google Scholar]
- 11.Crump C, Sundquist K, Winkleby MA, Sundquist J. Preterm birth and risk of epilepsy in Swedish adults. Neurology. 2011;77(14):1376–1382. doi: 10.1212/WNL.0b013e318231528f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abe K, Hamada H, Yamada T, Obata-Yasuoka M, Minakami H, Yoshikawa H. Impact of planning of pregnancy in women with epilepsy on seizure control during pregnancy and on maternal and neonatal outcomes. Seizure. 2014;23(2):112–116. doi: 10.1016/j.seizure.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 13.Watila MM, Beida O, Kwari S, Nyandaiti NW, Nyandaiti YW. Seizure occurrence, pregnancy outcome among women with active convulsive epilepsy: one year prospective study. Seizure. 2015;26:7–11. doi: 10.1016/j.seizure.2015.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]