Abstract
Background
When an emergency-care patient is diagnosed with an emerging infectious disease, hospitals in Korea may temporarily close their emergency departments (EDs) to prevent nosocomial transmission. Since February 2020, multiple, consecutive ED closures have occurred due to the coronavirus disease 2019 (COVID-19) crisis in Daegu. However, sudden ED closures are in contravention of laws for the provision of emergency medical care that enable the public to avail prompt, appropriate, and 24-hour emergency medical care. Therefore, this study ascertained the vulnerability of the ED at tertiary hospitals in Daegu with regard to the current standards. A revised triage and surveillance protocol has been proposed to tackle the current crisis.
Methods
This study was retrospectively conducted at 6 level 1 or 2 EDs in a metropolitan city where ED closure due to COVID-19 occurred from February 18 to March 26, 2020. The present status of ED closure and patient characteristics and findings from chest radiography and laboratory investigations were assessed. Based on the experience from repeated ED closures and the modified systems that are currently used in EDs, revised triage and surveillance protocols have been developed and proposed.
Results
During the study period, 6 level 1 or 2 emergency rooms included in the study were shut down 27 times for 769 hours. Thirty-one confirmed COVID-19 cases, of whom 7 died, were associated with the incidence of ED closure. Typical patient presentation with respiratory symptoms of COVID-19 was seen in less than 50% of patients, whereas abnormal findings on chest imaging investigations were detected in 93.5% of the study population. The chest radiography facility, resuscitation rooms, and triage area were moved to locations outside the ED, and a new surveillance protocol was applied to determine the factors warranting quarantine, including symptoms, chest radiographic findings, and exposure to a source of infection. The incidence of ED closures decreased after the implementation of the revised triage and surveillance protocols.
Conclusion
Triage screening by emergency physicians and surveillance protocols with an externally located chest imaging facility were effective in the early isolation of COVID-19 patients. In future outbreaks of emerging infectious diseases, efforts should be focused toward the provision of continued ED treatment with the implementation of revised triage and surveillance protocols.
Keywords: COVID-19 Crisis, Temporary ED Closure, Nosocomial Transmission, Revised Triage, Surveillance Protocol, Chest X-ray
Graphical Abstract
INTRODUCTION
In June 2015, an outbreak of the Middle East respiratory syndrome coronavirus (MERS-CoV) infection occurred in Korea. Subsequently, the high transmission efficiency of MERS-CoV was demonstrated through a single super-spreader, hospitalized for 3 days in the emergency department (ED) of a tertiary hospital, who caused 78 nosocomial transmissions, including among the medical staff.1,2,3 Following this incident, the Korean Centers for Disease Control and Prevention (KCDC) stipulated the implementation of a cohort isolation protocol for the ward or the entire hospital to prevent hospital transmission when a new infectious disease is confirmed in the hospital.4
The coronavirus disease 2019 (COVID-19) pandemic, also known as the coronavirus pandemic, is an ongoing pandemic caused by the severe acute respiratory syndrome coronavirus 2. The outbreak was identified in Wuhan, China, in December 2019. The World Health Organization (WHO) declared the outbreak a Public Health Emergency of International Concern on January 30, and a pandemic on March 11, 2020.
In Daegu Metropolitan City, since February 18, 2020, the number of patients with COVID-19 has increased rapidly after the infection was initially confirmed. At times, COVID-19 patients with atypical symptoms who present to the ED might not be initially identified for isolation during triage but may subsequently be confirmed COVID-19 positive. By February 18, 2020, with the increased number of confirmed cases in Daegu, many EDs were consecutively and repeatedly closed, and medical staff on duty and inpatients were quarantined. However, sudden ED closure goes against the laws that regulate the provision of emergency medical care, which enables the public to receive prompt, appropriate, and 24-hour emergency medical attention5; ED closures need to be carefully determined as they can seriously affect the treatment of severely ill patients, such as those with acute myocardial infarction, acute stroke, and major trauma.
This is the first study to evaluate multiple, consecutive, temporary ED closures caused by an emerging infectious disease. The present research study investigated the current status of ED closures, the characteristics of the causative patient, triage systems at each hospital, and nosocomial transmission. Furthermore, we aimed to propose a new COVID-19 surveillance protocol and a revised triage process for EDs to minimize their closure.
METHODS
Study setting, design, and subjects
Daegu Metropolitan City has 15 emergency medical centers that provide health services to a population of approximately 2.5 million individuals. Emergency medical centers are categorized by the level of care available on the basis of ED capacity and resource parameters, including the number of emergency physicians (EPs), nurses, equipment, and size of the department. Six level 1 and 2 EDs provide the highest level of emergency care services in the region and annually manage 230,000 severe emergency cases.6
We retrospectively analyzed the data from the COVID-19 cases that resulted in temporary closure of 2 level 1 and 4 level 2 EDs in Daegu between February 18 and March 25, 2020; the cutoff date for the study data collection was March 26, 2020. Moreover, we investigated the triage system, surveillance protocols, and use of personal protective equipment (PPE) against the COVID-19 crisis at these EDs. Based on the experience from repeated ED closures and the currently modified systems in EDs, we developed and proposed revised triage and surveillance protocols. COVID-19 was diagnosed on the basis of the WHO's interim guidance and the KCDC guidelines. A confirmed diagnosis of COVID-19 was defined as a positive result on high-throughput sequencing or real-time reverse transcriptase-polymerase chain reaction (RT-PCR) assay of nasopharyngeal swab specimens.
Data source and study variables
We obtained data from the 119 dispatch centers in the province on the date and duration of temporary ED closures. In addition, we extracted data, including clinical symptoms or signs, vital signs, recent exposure history, and laboratory findings on admission of patients with confirmed COVID-19 from electronic medical records. We determined the presence of a radiographic abnormality based on the report descriptions in the medical charts and a review of chest X-ray (CXR) findings by EPs. Data on triage systems from before and after the COVID-19 outbreak, nosocomial transmission that resulted in temporary ED closures, and the level of PPE use among healthcare professionals in the ED were investigated through EPs who worked in these EDs. Fever was defined as an axillary temperature of 37.5°C or higher. Exposure to a source of transmission was defined as travel within 14 days to a country which was reported to possess a COVID-19 risk by the KCDC, contact with a COVID-19 patient or a member of the Shincheonji sect.
Statistical analysis
Descriptive statistics are presented as medians with interquartile ranges (25th and 75th percentiles), and categorical variables are presented as numbers and percentages. All statistical tests were conducted in SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Ethics statement
The present study was reviewed and approved by the Institutional Review Board of Kyungpook National University Chilgok Hospital (2020-04-004). The requirement of informed consent was waived because of the retrospective nature of this study.
RESULTS
Temporary ED closure during the COVID-19 crisis in Daegu
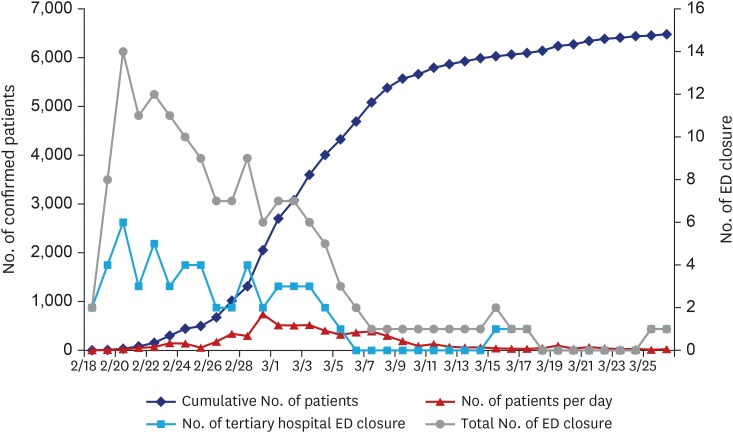
By March 26, 2020, there were 6,482 patients with confirmed COVID-19 since the first case was detected on February 18, 2020. Forty temporary ED closures took place in Daegu; these included closures at 27 level 1 and 2 and 13 level 3 EDs during the study period (Fig. 1). The median and total duration of temporary ED closures for level 1 and 2 EDs were 1,048.5 minutes and 769 hours, respectively (Table 1).
Fig. 1. Number of COVID-19-confirmed patients and ED closures during the COVID-19 crisis in Daegu Metropolitan City.
COVID-19 = coronavirus disease 2019, ED = emergency department.
Table 1. Clinical characteristics of the study patients.
| Variables | All patients (n = 31) | ||
|---|---|---|---|
| Sex | |||
| Male | 16 (51.6) | ||
| Female | 15 (48.4) | ||
| Age, yr | 75 (64–80) | ||
| < 40 | 3 (9.7) | ||
| 40–59 | 4 (12.9) | ||
| ≥ 60 | 24 (77.4) | ||
| Coexisting disorders | |||
| Diabetes mellitus | 10 (32.3) | ||
| Heart disease | 1 (3.2) | ||
| Hypertension | 16 (51.6) | ||
| Stroke | 1 (3.2) | ||
| Cancer | 3 (9.7) | ||
| Signs and symptoms | |||
| Dyspnea | 15 (48.4) | ||
| Fever | 14 (45.2) | ||
| Cough | 9 (29.0) | ||
| Sputum | 5 (16.1) | ||
| Headache | 2 (6.5) | ||
| Myalgia | 5 (16.1) | ||
| Nausea or vomiting | 2 (6.5) | ||
| Diarrhea | 2 (6.5) | ||
| Cardiac arrest | 2 (6.5) | ||
| Exposure to source of transmission within the past 14 days | 6 (19.4) | ||
| Fever on ED admission | |||
| Temperature, °C | 37.1 (36.6–37.8) | ||
| < 37.5 | 17 (54.8) | ||
| 37.5–38.5 | 12 (38.7) | ||
| ≥ 38.5 | 2 (6.5) | ||
| Vital signs on ED admission | |||
| Systolic blood pressure, mmHg | 130 (110–146) | ||
| Oxygen saturation measured with a pulse oximeter | 96 (90.5–99) | ||
| Heart rate, /min | 80 (74–94) | ||
| Respiratory rate, /min | 20 (20–21) | ||
| Time from ED admission to isolation, min | 403 (89–1,711) | ||
| Time from ED admission to diagnosis, min | 432 (304–1,326) | ||
| Time from ED admission to chest X-ray, min | 54 (30–125) | ||
| Duration of ED shutdown, min | 1,048.5 (465–2,734) | ||
Data are presented as median (interquartile range) or number (%).
ED = emergency department.
Characteristics of patients who caused temporary ED closure
Of the 31 patients identified to have caused ED closure, 77.4% were aged 60 or older. The commonest symptom was dyspnea (48.4%), followed by fever on admission (45.2%), and cough (29.0%). Six patients who were exposed to a transmission source had attended a Shincheonji religious meeting, or had a history of contact with the Shincheonji sect. The median duration from emergency room (ER) admission to isolation and ED admission to COVID-19 diagnosis by RT-PCR was 403 and 432 minutes, respectively (Table 1).
Radiographic abnormalities in chest imaging were observed in 29 patients (93.5%). The commonest patterns on chest radiography were ground-glass opacity (48.4%) and consolidation (41.9%). The median white blood cell count was 6.13 × 103/mm3, and the level of C-reactive protein was elevated (median, 7.3 mg/L; ref., < 0.5 mg/dL). Of the 31 patients included in this study, 7 had died by the specified study cutoff date (Table 2).
Table 2. Radiologic and laboratory findings of the study patients.
| Variables | All patients (n = 31) | ||
|---|---|---|---|
| Chest X-ray findings | |||
| Normal | 2 (6.5) | ||
| Abnormal | 29 (93.5) | ||
| Ground-glass opacity | 15 (48.4) | ||
| Consolidation | 13 (41.9) | ||
| Patch/nodular | 1 (3.2) | ||
| Laboratory findings | |||
| White cell count, per mm3 | 6,130 (3,800–8,530) | ||
| Hemoglobin, g/dL | 12.4 (11–13.8) | ||
| Platelet count, per mm3 | 177,000 (135,000–241,500) | ||
| Erythrocyte sedimentation rate, mm/hr | 53.5 (29.5–77) | ||
| C-reactive protein, mg/dL | 7.3 (2.1–14.6) | ||
| Clinical outcomes at data cutoff | |||
| Recovery | 9 (29.0) | ||
| Active | 15 (48.4) | ||
| Death | 7 (22.6) | ||
Data are presented as median (interquartile range) or number (%).
Developing revised triage and ED surveillance protocol response to the COVID-19 outbreak in Daegu
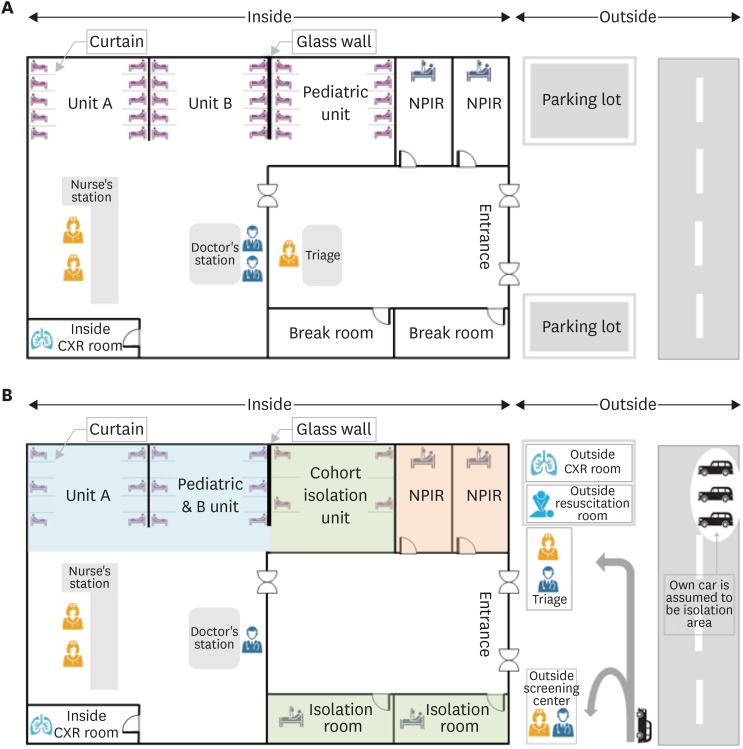
Following temporary ED closures, 6 hospitals in Daegu defined different isolation spaces depending on the prevailing circumstances at the hospital, although all 6 hospitals adopted similar modified triage protocols. Prior to ED admission, patients were examined and triaged by EPs and nurses, and the ED space was remodeled to accommodate chest radiography. The observation area for general or critically ill emergency care patients and that for patients with suspected COVID-19, fever, or respiratory symptoms were operated separately. After temporary ED closure, healthcare professionals in all hospitals wore level D PPE and worked in the designated triage areas (Fig. 2).
Fig. 2. Structural and functional changes in the emergency department after the coronavirus disease outbreak. (A) Original triage. (B) Revised triage. Unit A: treatment of moderately to severely ill patients. The gap between the sick beds is readjusted to 2.5 m or more. Unit B: treatment of mildly ill patients. The gap between the sick beds is readjusted to 2.5 m or more. When the room is full, the patient's car is assumed to be an isolation area and medical treatment is initiated for the patient in the vehicle until the NPIR is empty.
NPIR = negative-pressure isolation room, CXR = chest X-ray.
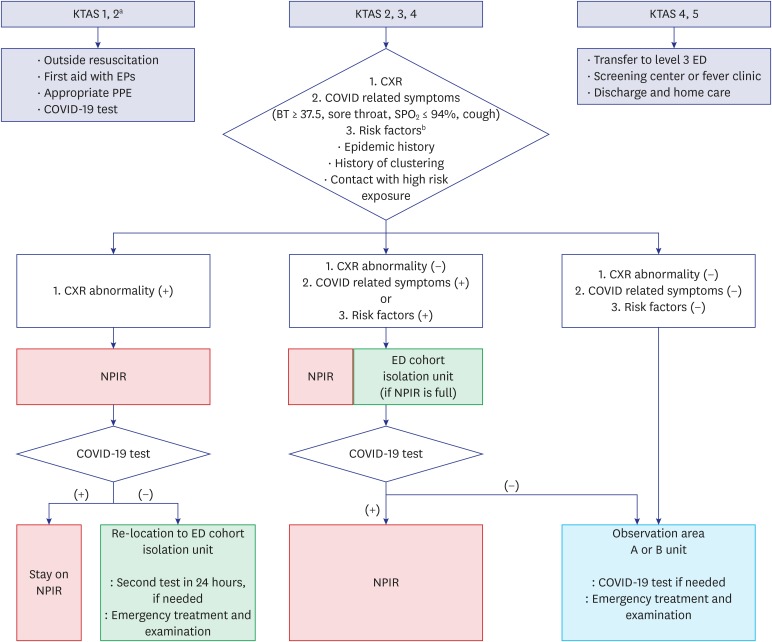
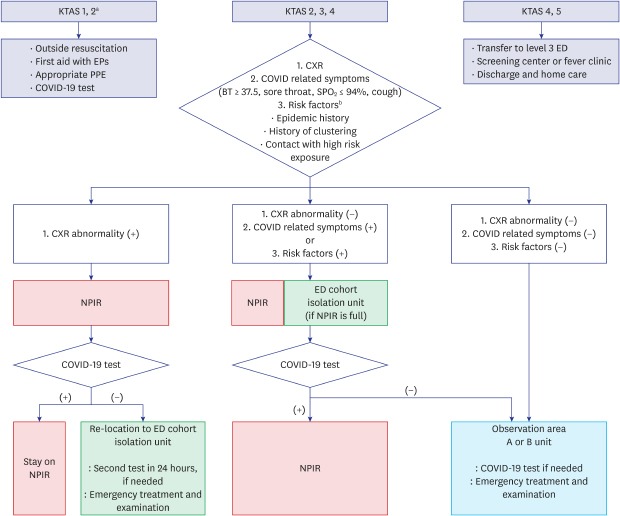
Based on these experiences, we suggest new ED surveillance protocols as a response to the COVID-19 crisis: 1) The Korean Triage and Acuity Scale (KTAS) levels 1 and 2 life-threatening patients or emergency cases were to be treated as done previously; but, healthcare professionals should use appropriate PPE and use negative pressure carts to move all patients; 2) In the case of urgent patients, KTAS levels 2, 3, and 4, patients were to be assigned and treated according to their symptoms, CXR findings, and exposure to the source of transmission; 3) In the case of non-urgent patients with KTAS levels 4 or 5, it is necessary to guide outpatients to local clinics, or level 3 EDs to reduce the patient load in the ED (Fig. 3). Following the institution of the revised triage system and surveillance protocol in the 6 EDs, only 3 temporary ED closures took place (Fig. 1).
Fig. 3. The coronavirus disease surveillance protocol in the ED.
KTAS = Korean Triage and Acuity Scale, EP = emergency physician, PPE = personal protective equipment, COVID-19 = coronavirus disease 2019, NPIR = negative-pressure isolation room, CXR = chest X-ray, ED = emergency department, BT = body temperature.
aKTAS: 1, immediate resuscitation; 2, very urgent; 3, urgent; 4, standard; and 5, non-urgent; bRisk factors: epidemic history, history of clustering, contact with high risk exposure.
DISCUSSION
This is the first study on the present situation, causes, and improvement plans with regard to temporary ED closures consequent to an emerging infectious disease. In Korea, rarely the KCDC has ordered the shutdown of hospitals on confirmation of a positive case of an emerging infectious disease in the hospital or the community. Hospital closure and isolation appears to have played a useful role in preventing an emerging infectious disease, both in-hospital and amongst the local community.7,8 However, temporary ED closure is being variably implemented by each hospital, depending on the situation, in the absence of clear guidelines from the KCDC or local governmental authorities. ED closure has many effects, such as disruption of emergency care provision to other severely ill emergency patients. However, ED closures have not been sufficiently deliberated, and further discussions and clearer standard guidelines are needed.
The findings of this study confirmed that it is important to quickly design and implement revised triage and ER surveillance protocols that are suitably individualized with regard to the characteristics of infectious diseases in order to prevent the entry of patients with emerging infectious diseases into the ED. When severely ill patients with various symptoms visit the ED, the original triage protocol has limitations in effectively classifying patients with emerging infectious diseases, such as COVID-19.9 In the original ED triage protocol, the classification of severity and determination of the care ranking and isolation of patients for treatment are undertaken by nurses. The severity is graded on the basis of chief complaints or vital signs. In the present study, it is shown that the original ED triage protocol was ineffective in the identification and isolation of COVID-19 patients with nonspecific symptoms.
In some cases, ED closures occurred because of suspected COVID-19 patients without confirmed RT-PCR results. It is possible that the explosive increase in the number of confirmed patients and recurrent ED closures may have resulted in overreactions by medical staff.
In general, many patients with COVID-19 presented with respiratory complaints, such as fever, sore throat, shortness of breath (SpO2 ≤ 94%) and cough.10,11 In the present study, which was mainly focused on level 1 and 2 EDs, the patients showed many atypical symptoms, and CXRs showed abnormal findings in most patients (29/31); therefore, it was of great importance to check chest images of all patients who visited the ED for signs or risk factors.12 Based on these findings, the revised triage and ED surveillance protocols were devised at level 1 and 2 EDs in Daegu that experienced repeated closures.
In the revised triage, EPs presided over and classified patients together with nurses. The KTAS level 1 and 2 life-threatening patients or emergency cases were treated as previously; but emergency workers were required to use appropriate PPE and use negative pressure carts to move all patients. For KTAS levels 2, 3, and 4, modified methods were used. In the revised triage, if the chest imaging showed abnormal findings or the patient had respiratory symptoms or risk factors, he/she was moved to a negative-pressure isolation room (NPIR). In cases with even mild suspicion of fever of unknown origin or COVID-19, it was recommended to move the patient to a temporary isolation area in the ER with readjusted bed gap and curtain (or wall) separation (ER cohort isolation). When the room was full, the patient's car was used as an isolation area and medical treatment was initiated for the patient in the vehicle until the NPIR was empty. Patients without any possibility of having COVID-19 infection entered the observation zone (Figs. 2 and 3). In the case of mildly ill patients, KTAS levels 4 or 5, it was necessary to guide them to local clinics to reduce patient load in the ED and reduce the number of ED beds and to increase the physical distance between sick beds. Furthermore, the authors of this report conducted cardiopulmonary resuscitation of patients with out-of-hospital cardiac arrests outside the ED (Fig. 2). In 2015, massive hospital transmissions had occurred because of a MERS super spreader in the ER.1,2,3 Since then, the Korean ED environment has been improved, such as through the installation of a ventilation system, expansion of the ER space, and bigger bed gaps, and through educating guardians to use appropriate PPE, such as masks. Due to these changes, it is assumed that no hospital transmission in the ED occurred this time.
Incidentally, as stated in Article 5-2 of the Act on Emergency Medical Care (immunity for good faith in emergency), EPs have a certain freedom from liability because of the characteristics of their work. This confers minimal legal protection that permits doctors to exercise conscientious discretion when treating patients, but the same needs to be expanded and applied in the management of emerging infectious diseases. In the event of a second transmission, the current method wherein the doctor or hospital takes full responsibility and faces blame can lead to the refusal of medical services to certain patients. In fact, a private clinic did not even undertake examinations in cases of MERS and COVID-19, which led to an influx of patients at the tertiary hospital. Even if an unavoidable secondary transmission occurs, it is necessary to establish a provision that confers legal immunity to emergency medical personnel.
This study has some limitations. First, the revised triage and ED surveillance protocol cannot be applied to all hospitals, based on the status of hospital facilities, equipment, and personnel. Second, some patients have an extended latent period and, therefore a possibility of future hospital transmissions exist. Moreover, given the high false negative rate of the COVID-19 test kit, the test results of patients may vary in terms of accuracy. Third, the revised triage and ED surveillance protocols devised in this study are based on clinical experience with COVID-19, and a customized revised triage protocol may be required for other emerging infectious diseases.
In conclusion, when an outbreak of an emerging infectious disease occurs, it is important to use revised triage and surveillance protocols that are matched to the characteristics of the causative agent. Emergency treatment should be continued in tandem with thorough use of PPE and improved safety of the ED treatment environment, rather than resorting to ED closure. If inevitable, ED closures need to be implemented through clear and systematic guidelines issued by the national and local governments and hospitals.
ACKNOWLEDGMENTS
We thank all ED healthcare professionals and the 119 emergency medical technicians who are helping in the fight against COVID-19. We also thank Kwang Sung Lee for the support rendered for data collection at the National Medical Center.
Footnotes
Funding: This study was supported by a research grant from Daegu Medical Association COVID-19 Scientific Committee (2020).
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Kim JK, Lee DE, Chung HS.
- Data curation: Kim JK, Lee DE, Chung HS, Yeo IH, Kim C, Park J, Seo KS.
- Formal analysis: Lee DE, Chung HS.
- Investigation: Kim JK, Lee DE, Chung HS, Park SY, Kim JH, Lee SH, Kim G, Cheon JJ, Kim YH.
- Methodology: Kim JK, Lee DE, Chung HS.
- Writing - original draft: Kim JK, Lee DE, Chung HS.
- Writing - review & editing: Kim JK, Lee DE, Chung HS.
References
- 1.Korea Centers for Disease Control and Prevention. Middle East respiratory syndrome coronavirus outbreak in the Republic of Korea, 2015. Osong Public Health Res Perspect. 2015;6(4):269–278. doi: 10.1016/j.phrp.2015.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oh MD, Park WB, Park SW, Choe PG, Bang JH, Song KH, et al. Middle East respiratory syndrome: what we learned from the 2015 outbreak in the Republic of Korea. Korean J Intern Med. 2018;33(2):233–246. doi: 10.3904/kjim.2018.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kang CK, Song KH, Choe PG, Park WB, Bang JH, Kim ES, et al. Clinical and epidemiologic characteristics of spreaders of Middle East respiratory syndrome coronavirus during the 2015 outbreak in Korea. J Korean Med Sci. 2017;32(5):744–749. doi: 10.3346/jkms.2017.32.5.744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim JY, Song JY, Yoon YK, Choi SH, Song YG, Kim SR, et al. Middle East Respiratory syndrome infection control and prevention guideline for healthcare facilities. Infect Chemother. 2015;47(4):278–302. doi: 10.3947/ic.2015.47.4.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Law Information Center. Emergency medical service act. [Updated 2020]. [Accessed April 1, 2020]. http://www.law.go.kr/lsInfoP.do?lsiSeq=215835&efYd=20200324#0000.
- 6.National Emergency Medical Center. Emergency medical statistics yearbook. [Updated 2019]. [Accessed March 28, 2020]. https://www.e-gen.or.kr/nemc/statistics_annual_report.do.
- 7.Lee H, Heo JW, Kim SW, Lee J, Choi JH. A lesson from temporary closing of a single university-affiliated hospital owing to in-hospital transmission of coronavirus disease 2019. J Korean Med Sci. 2020;35(13):e145. doi: 10.3346/jkms.2020.35.e145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yoo JH, Hong ST. The outbreak cases with the novel coronavirus suggest upgraded quarantine and isolation in Korea. J Korean Med Sci. 2020;35(5):e62. doi: 10.3346/jkms.2020.35.e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang J, Zhou L, Yang Y, Peng W, Wang W, Chen X. Therapeutic and triage strategies for 2019 novel coronavirus disease in fever clinics. Lancet Respir Med. 2020;8(3):e11–2. doi: 10.1016/S2213-2600(20)30071-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55(3):105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yoon SH, Lee KH, Kim JY, Lee YK, Ko H, Kim KH, et al. Chest radiographic and CT findings of the 2019 novel coronavirus disease (COVID-19): analysis of nine patients treated in Korea. Korean J Radiol. 2020;21(4):494–500. doi: 10.3348/kjr.2020.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]