Abstract
Endoscopic management of bile duct stones is now the standard of care, but challenges remain with difficult bile duct stones. There are some known factors associated with technically difficult bile duct stones, such as large size and surgically altered anatomy. Endoscopic mechanical lithotripsy is now the standard technique used to remove large bile duct stones, but the efficacy of endoscopic papil-lary large balloon dilatation (EPLBD) and cholangioscopy with intraductal lithotripsy has been increas-ingly reported. In patients with surgically altered anatomy, biliary access before stone removal can be technically difficult. Endotherapy using two new endoscopes is now utilized in clinical practice: enter-oscopy-assisted endoscopic retrograde cholangiopancreatography and endoscopic ultrasound-guided antegrade treatment. These new approaches can be combined with EPLBD and/or cholangioscopy to remove large bile duct stones from patients with surgically altered anatomy. Since various endoscopic procedures are now available, endoscopists should learn the indications, advantages and disad-vantages of each technique for better management of bile duct stones.
Keywords: Cholangioscope; Choleodcholithiasis; Cholangiopancreatography, endoscopic retrograde; Endosonography; Lithotripsy
INTRODUCTION
Bile duct stones (BDS) are one of the most common biliary tract diseases with a prevalence of 10% to 20% of symptomatic gallbladder stones.1 There are two types of BDS; primary de novo stones and secondary stones. Primary BDS arise within the intrahepatic and/or extrahepatic ducts and are common in Asian population. Meanwhile, secondary BDS migrate into the bile duct from the gallbladder, which are common in Western population. Although a natural history of asymptomatic BDS is not fully elucidated,2 BDS can cause various symptoms such as abdominal pain, obstructive jaundice, cholangitis and pancreatitis, which can be potentially fatal. Endoscopic retrograde cholangiopancreatography (ERCP) with endoscopic sphincterotomy (ES)3 is an established treatment for BDS with technical success rates of 85% to 90%. In the remaining 10% to 15%, additional techniques or devices are often necessary to manage those “difficult” BDS.4
WHAT ARE DIFFICULT BDS?
The reasons for difficulty include stone characteristics, the anatomy, patients’ conditions and endoscopists’ skills. There are some steps for endoscopic stone removal: access to the ampulla and biliary system, ampullary interventions and stone extraction. Endoscopists can encounter technical hurdles throughout those steps as shown in Table 1. The definition of difficult BDS can vary among endoscopists because difficult BDS for trainees is not always difficult for experts. However, large BDS5 and surgically altered anatomy6 are two major reasons for technical difficulty.
Table 1.
Factors Underlying Difficult Bile Duct Stones
| Category | Conditions | Reasons for difficulty |
|---|---|---|
| Patient characteristics | Unstable condition | Risk for adverse events |
| Coagulopathy | Risk for bleeding | |
| Anatomy | Surgically altered anatomy | Scope insertion, biliary cannulation |
| Periampullary diverticulum | Biliary cannulation | |
| Biliary stricture | Stone extraction | |
| Stone characteristics | Large stone | Need for lithotripsy |
| Impacted stone | Need for cholangioscopy | |
| Endoscopist | Less experienced | Less skills and knowledge |
In cases with large BDS, there are two recent approaches for stone extraction: endoscopic papillary large balloon dilatation (EPLBD)7 and intraductal lithotripsy under the guidance of per-oral cholangioscopy (POCS).8,9 On the other hand, biliary access is the major issue in cases with surgically altered anatomy. In the past, ERCP using a conventional duodenoscope or forward viewing scope was performed but the technical success rate was not satisfactory.6 In failed cases, salvage by percutaneous or surgical approach has been performed. Recently, two endoscopic approaches are increasingly utilized for management of BDS in surgically altered anatomy patients: enteroscopy-assisted ERCP10 and endoscopic ultrasound (EUS)-guided approach.11,12 Herein, these new modalities for difficult BDS are reviewed.
ENDOSCOPIC PAPILLARY LARGE BALLOON DILATATION
ES is the standard ampullary intervention for endoscopic management of BDS.3 While endoscopic papillary balloon dilation (EPBD) is an alternative to ES,13,14 it was reportedly associated with an increased risk of post-ERCP pancreatitis (PEP).15 The long-term outcomes such as recurrent BDS are reportedly superior to those of ES16 but EPBD is not widely used due to the increased risk of PEP. More recently, EPLBD, which was first described by Ersoz et al.17 in 2003, is increasingly utilized for difficult BDS. In EPLBD, the ampulla was dilated using a balloon >10 mm, which allows extraction of large BDS even without lithotripsy (Fig. 1). In a meta-analysis of EPLBD and ES,18 technical success rate was similar (98% in EPLBD and 95% in ES) but the use of mechanical lithotripsy (ML) was less often necessary after EPLBD. While ML was performed in 32% in ES, the rate of ML use was only 15% in EPLBD. Furthermore, EPLBD reduced adverse events (11% in EPLBD and 18% in ES), suggesting better safety and effectiveness of EPLBD for large BDS.
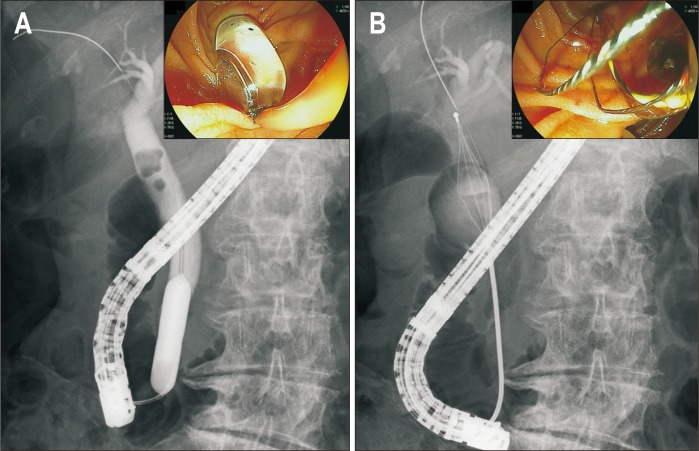
Fig. 1.
Endoscopic papillary large balloon dilation. (A) The ampulla was dilated with a large balloon. (B) A bile duct stone was extracted without lithotripsy.
Whether EPLBD should be preceded by ES or not is a matter of debate. EPLBD was originally preceded by ES but in a multicenter retrospective analysis,19 a large size ES was associated with bleeding with an odds ratio of 6.22. And a recent randomized controlled trial (RCT)20 showed similar efficacy and safety between EPLBD alone and EPLBD with ES. The adverse event rates were 6 % and 4% (p= 0.75) and PEP rates were 1 % and 3 % (p= 0.62) in EPLBD alone and EPLBD with ES. Complete stone removal was achieved in 92% and 88%, and the use of ML was necessary in 6.5% in EPLBD alone and 9.1% in EPLBD with ES (p=0.39).
Since the number of patients who were on antithrombotic agents is increasing rapidly in clinical practice, EPLBD without ES may be recommended in those patients on antithrombotic agents to avoid bleeding complications.21
While safety and efficacy of EPLBD have been proven, the diameter of balloon was limited to the size of distal bile duct. In addition, EPLBD is contraindicated in cases with distal biliary stricture due to the risk of perforation.19 Thus, if the size of BDS is larger than that of distal bile duct,22 lithotripsy is necessary for stone extraction even after EPLBD.
CHOLANGIOSCOPY-ASSISTED LITHOTRIPSY
ML is a standard method for lithotripsy in cases with large BDS. The technical success rate of ML is about 90%23,24 but ML can be technically challenging depending on the size and location of BDS. The technical success rate of ML was 67.6% in cases with stones >2.5 cm.23 An impacted stone was a risk factor for failed ML25 and a confluence stone is also technically challenging.
Extracorporeal shock wave lithotripsy (ESWL)26 is a treatment option but can be time consuming and needs a nasobiliary drainage tube placement, which causes discomfort to patients. Since the introduction of single-operator cholangioscopy, cholangioscope-assisted intraductal lithotripsy is increasingly utilized. POCS allows lithotripsy under direct visualization using electrohydraulic lithotripsy (EHL) and laser lithotripsy (Fig. 2).
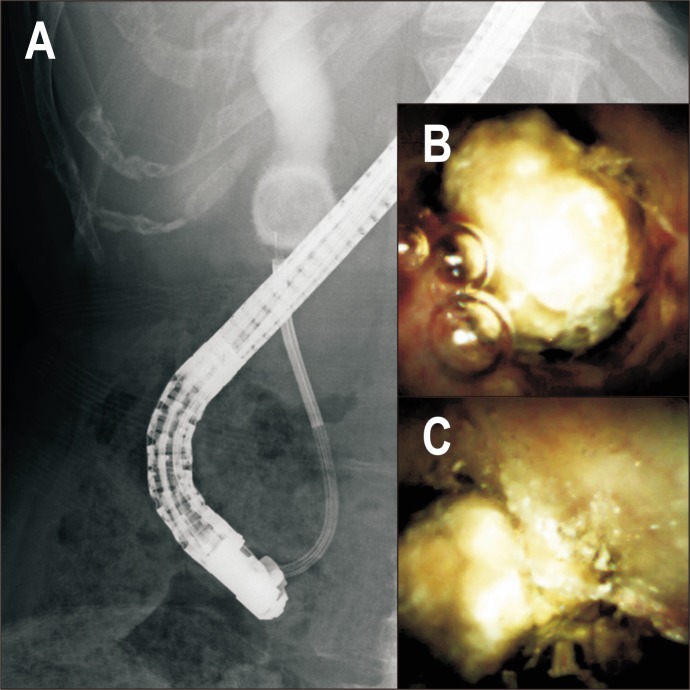
Fig. 2.
Per-oral cholangioscopy-assisted electrohydraulic lithotripsy (EHL). (A) A digital cholangioscope was inserted into the bile duct. (B) A large bile duct stone was visualized. (C) EHL was performed under direct visualization.
There are three types of cholangioscopy available now: dual-operator “mother-baby” cholangioscopy, single-operator “mother-baby” cholangioscopy and direct cholangioscopy (Table 2).
Table 2.
Comparison of Three Cholangioscopy Systems
| Variable | Dual-operator “mother-baby” cholan-gioscopy | Single-operator “mother-baby” cholangioscopy | Direct cholangioscopy |
|---|---|---|---|
| Endoscopists | Two | Single | Single |
| Need for additional processor | Yes | Yes | No |
| Steering | 2 Directions | 4 Directions | 2–4 Directions |
| Scope diameter, mm | 3.3–3.5 | 3.6 | 5–6 |
| Working channel diameter, mm | 1.2 | 1.2 | 2 |
| Dedicated irrigation channel | No | Yes | No |
| Image quality | Very good | Good | Very good |
| Image enhanced endoscopy | Yes | No | Yes |
| Technical ease for biliary access | Yes | Yes | No |
| Maneuverability | Good | Very good | Needs expertise |
| Cost | High | High | Low |
In a RCT of laser lithotripsy under endoscopic or percutaneous cholangioscope and ESWL,27 the rate of stone clearance was significantly higher in laser lithotripsy (97%) than in ESWL (73%). Comparison of EHL and laser lithotripsy is summarized in Table 3. A recent systematic review28 also demonstrated that laser lithotripsy had a higher complete ductal clearance rate (95.1 %) than EHL (88.4 %) and ESWL (84.5 %, p<0.001). Meanwhile, the adverse event rate was significantly higher in EHL (13.8 %) than in ESWL (8.4 %) or laser lithotripsy (9.6 %, p= 0.04). Thus, laser lithotripsy provides better clinical outcomes in large BDS but it may depend on the local expertise and availability of each technique. In a recent multicenter, international, retrospective analysis of digital cholangioscopy for difficult BDS, technical success and adverse event rates were comparable: 96.7% versus 99% (p=0.31) and 3.3% versus 5.0% (p=0.54) in EHL and laser lithotripsy groups. However, the procedure time was significantly longer in EHL group (73.9 minutes vs 49.9 minutes, p<0.001).9
Table 3.
Comparison of EHL and Laser Lithotripsy for the Removal of Difficult Bile Duct Stones
| Complete duct clearance rate28 | Complication rate28 | Advantages | Disadvantages | |
|---|---|---|---|---|
| EHL | 88.4 | 13.8 | A small generator, inexpensive | Risk of bleeding and perforation |
| Laser | 95.1 | 9.6 | Less traumatic | A large machine, expensive |
EHL, electrohydraulic lithotripsy.
There are two recent RCTs comparing POCS-assisted lithotripsy and the standard technique.29,30 Buxbaum et al.29 compared POCS-assisted lithotripsy and the conventional technique including ML and EPLBD for BDS >1 cm. Complete stone removal rates were 93% in POCS-assisted lithotripsy and 67% in the conventional treatment without significant differences in the rates of adverse events (9.5% and 11.1%). However, the procedure time was significantly longer in POCS-assisted lithotripsy group (120.7 and 81.2 minutes). Another RCT by Angsuwatcharakon et al.30 compared POCS-guided laser lithotripsy and ML after failed EPLBD. Complete stone removal rates in a single session were 100% and 63% with comparable adverse events (6% and 13%) in the POCS group and the ML group. In this study, the procedure time was not significantly different (66 and 83 minutes) and the fluoroscopy time was significantly shorter (11 and 21 minutes) in the POCS group. Cost of POCS should also be discussed in the era of medical cost effectiveness, given the high price of a single-use digital cholangioscope. In the cost-effective analysis by Deprez et al.,31 however, the use of cholangioscope for difficult BDS would decrease the number of procedures by 28% and the cost by 11%, respectively. In summary, POCS-assisted lithotripsy can be a standard of care in terms of safety, efficacy and cost effectiveness for large BDS.
ENTEROSCOPY-ASSISTED ERCP
Endoscopic management of BDS in patients with surgically altered anatomy is still technically demanding.6 In cases with Billroth II reconstruction or Roux-en-Y reconstruction, scope insertion can be difficult or impossible in some cases, and even after scope insertion both biliary cannulation and stone extraction pose technical hurdles to endoscopists. Recent development of enteroscopes dedicated for therapeutic ERCP allows easy scope insertion and the use of various ERCP devices (Fig. 3).32-34
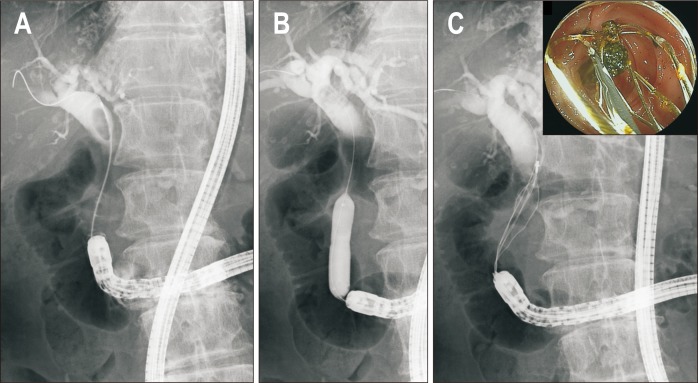
Fig. 3.
Enteroscopy-assisted endoscopic retrograde cholangiopancreatography. (A) Cholangiogram revealed bile duct stones. (B) Endoscopic papillary large balloon dilation was performed. (C) Bile duct stones were extracted with a basket catheter.
In cases with surgically altered anatomy, the size of BDS is often too large for stone extraction without lithotripsy. Various techniques described above can be applied in this setting. Single-session and overall complete stone removal rates in surgically altered anatomy patients are reportedly 66.7% to 100% and 96.7% to 100%, respectively, using EPLBD.6 ML can be performed using recently developed enteroscopes33,34 with short scope length and a large channel but the size of BDS is limited to <2–3 cm for successful lithotripsy by ML. Furthermore, the insertion and manipulation of a stiff ML device is often technically challenging during enteroscopy-assisted ERCP.
POCS is not readily available in patients with surgically altered anatomy but some technical tips35-40 have been reported to perform POCS in this setting; direct insertion of enteroscopes into the bile duct, insertion of ultra-slim endoscope or cholangioscope into the bile duct with a help of the overtube of enteroscopes. Although POCS-guided lithotripsy is useful in patients with surgically altered anatomy, the procedure should be performed using CO2 insufflation to decrease the risk of air embolism. Intraabdominal pressure is often high with retained gas or CO2 after enteroscope insertion and additional insufflation in the bile duct may increase the risk of embolism, though its incidence is not fully elucidated.
EUS-GUIDED STONE MANAGEMENT
EUS-guided biliary interventions are increasingly utilized after failed or difficult ERCP.11,12 EUS-guided rendezvous (EUS-RV)41 and EUS-guided antegrade (EUS-AG) treatment are two major techniques used for endoscopic management of BDS. EUS-RV is useful in cases with accessible ampulla but failed biliary cannulation42 and subsequent procedure after biliary access is similar to the conventional ERCP. On the other hand, EUS-AG is a technique useful for inaccessible ampulla, especially in those with surgically altered anatomy.43-45
In EUS-AG stone treatment, biliary access is achieved from the stomach or jejunum under EUS-guidance. After guidewire passage through the ampulla into the duodenum, the ampulla is dilated using a balloon. Finally, BDS is antegradely pushed out using a stone extraction balloon (Fig. 4). In a multicenter retrospective study,46 its technical success rate was 72% with its adverse event rate of 17%. The major reason for technical failure was failed puncture of the intrahepatic bile duct, which is often minimally dilated in this setting. However, guidewire passage and stone extraction through the ampulla can be a reason for technical failure, too. To overcome these technical hurdles, approach to difficult BDS such as large balloon dilation and intraductal lithotripsy, which are discussed above, can be applied to EUS-AG.
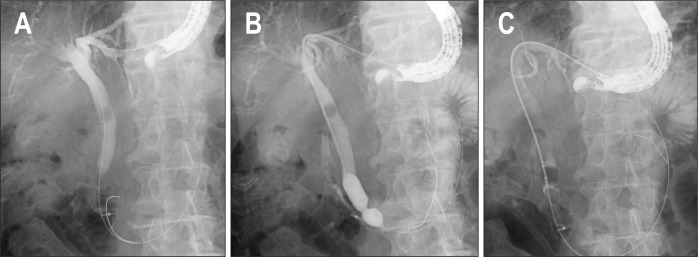
Fig. 4.
Endoscopic ultrasound-guided antegrade stone treatment. (A) Biliary access was achieved under endoscopic ultrasound guidance. (B) The ampulla was dilated with a balloon. (C) Bile duct stones were extracted in an antegrade manner using a balloon catheter.
During EUS-AG stone treatment, ES is technically impossible and the ampullary intervention is limited to papillary balloon dilatation. In cases with a large distal common bile duct (CBD), large balloon dilatation can be performed to enhance stone extraction. However, the balloon size is limited to the size of distal CBD and intraductal lithotripsy is necessary in cases with BDS larger than the size of distal CBD but the use of multiple devices with a prolonged procedure time can increase the risk of bile leak. To prevent bile leak, a two-step approach allows safe use of ML and cholangioscopy in EUS-AG stone treatment.47 In this two-step approach, only EUS-hepaticogastrostomy (EUS-HGS) or EUS-hepaticojejunostomy (EUS-HJS) is created in the first session, which can be completed in a short time and the risk of bile leak is small because there is no need to pass the guidewire through the ampulla or to extract BDS after the ampullary intervention. In the second session, HGS or HJS fistula is matured and stone extraction devices can be introduced through the mature fistula without a risk of bile leak. Although there have been no reports on the exact duration necessary for mature fistula creation but in general the second session can be safely performed 2 to 4 weeks after the first session. Intraductal lithotripsy can be performed using ML or POCS-guided lithotripsy, which was increasingly reported in recent papers.48-50 The mature fistula can be readily dilated using a bougie dilator or a balloon dilator before device insertion, depending on the size of devices used for lithotripsy. While ML can be introduced into the bile duct through the fistula over the guidewire easily, dilation up to 10-F is necessary if digital cholangioscopy-assisted lithotripsy is necessary after EUS-HGS or EUS-HJS using a plastic stent. Alternatively, a large bore fully-covered metal stent can also be utilized both to prevent bile leak and to allow easy access to the biliary system. The devices used for lithotripsy during EUS-guided approach are similar to ERCP approach: ML, ESWL and cholangioscopy-assisted laser lithotripsy and EHL.51
While most EUS-BD procedures were initially performed for unresectable malignant biliary obstruction, advanced EUS-guided management of benign biliary diseases including complex BDS has been increasingly reported (Table 4). Hosmer et al.48 reported a single center experience of nine cases with Roux-en-Y anatomy with the technical success rate of stone extraction was 100%. Balloon dilation of the ampulla ≥10 mm was performed in 89% and cholangioscopy-assisted EHL was performed in 44%. James et al.49 reported EUS-guided hepaticoenterostomy as a portal to allow definitive antegrade treatment of benign biliary diseases including eight cases with BDS. Stone clearance was successful in 100% with a combined balloon dilation and cholangioscopy. Mukai et al.50 also reported EUS-guided treatment of 37 cases with benign biliary diseases. They applied two-stage interventions when a complex procedure was expected such as in cases with BDS ≥15 mm or with tight biliary stricture. POCS-assisted lithotripsy was utilized in 13 BDS cases with a technical success rate of 100%. We can select the lithotripsy technique depending on characteristics of patients and BDS but there are no comparative studies of lithotripsy in EUS-guided approach. Thus, the technique can be selected according to the local expertise or preferences.
Table 4.
EUS-Guided Management of Bile Duct Stones in Patients with Surgically Altered Anatomy
| Author | Year | Study design | No. | Reconstruction | Procedures | Technical success, % | Reasons for failure | Adverse events, % |
|---|---|---|---|---|---|---|---|---|
| Weilert et al.43 | 2011 | Single left, retrospective | 6 | 6 R-Y | EUS-AG | 67 | 2 Failed device insertions | 16 |
| Iwashita et al.44 | 2013 | Single left, retrospective | 4 | 3 R-Y, 1 child | EUS-AG | 100 | - | 25 (1 mild pain) |
| Itoi et al.45 | 2014 | Single left, retrospective | 5 | 2 R-Y, 2 B-II, 1 JI | EUS-AG | 60 | 2 Failed stone extractions | 0 |
| Iwashita et al.46 | 2016 | Multileft, retrospective | 29 | 19 R-Y, 4 child, 3 B-II, 2 JI,1 HJS | EUS-AG | 72 | 6 Failed puncture, 1 failed guidewire insertion, 1 failed stone extraction | 17 (2 pain, 1 bile peritonitis, 1 cholecystitis, 1 elevated CRP) |
| Hosmer et al.48 | 2018 | Single left, retrospective | 9 | 9 R-Y | EUS-HGS followed by stone extraction | 100 | - | 11 (1 cholangitis) |
| James et al.49,* | 2018 | Single left, retrospective | 20* | 15 R-Y, 2 B-II, 3 Whipple | EUS-HGS/HJS followed by stone extraction or balloon dilation/stent | 100 | - | 15 (1 pain, 1 pancreatitis, 1 cholangitis) |
| Mukai et al.50,* | 2019 | Single left, retrospective | 37† | 26 R-Y, 2 B-II, 6 Whipple, 2 HD | EUS-AG, EUS-HGS/HJS followed by stone extraction or balloon dilation/stent | 91.9 | 3 Failed hepatoenteric tract creation | 8.1 (3 bile peritonitis) |
EUS, endoscopic ultrasound; R-Y, Roux-en-Y; AG, antegrade; B-II, Billroth II; JI, jejunal interposition; HJS, hepaticojejunostomy; CRP, C-reactive protein; HGS, hepaticogastrostomy; HD, hepaticoduodenostomy.
Included 8 bile duct stones, 11 benign biliary strictures and 1 bile leak; †Included 11 common bile duct stones, 5 intrahepatic bile duct stones, 10 anastomotic strictures and 11 anastomotic strictures complicated by stones.
There are some advantages and disadvantages for EUS- and enteroscopy-assisted stone management in cases with surgically altered anatomy (Table 5). While enterosocpy-assisted ERCP utilizes the physiological biliary access and has a low risk of bile leak, scope insertion can be technically difficult or even impossible depending on the anatomy. On the other hand, in EUS-guided approach, there is no need for deep scope insertion but the approach is limited to the left intrahepatic bile duct. Sometimes, biliary dilation is minimal and the puncture of the bile duct can be technically difficult. In addition, the risk of bile leak does exist in EUS-guided approach. Treatment algorithm for BDS should be established in cases with surgically altered anatomy. Currently, enteroscopy-assisted ERCP is often the first approach. After failed enteroscopy-assisted ERCP, EUS-guided approach can be a salvage technique if biliary access to the left intrahepatic bile duct is acceptable. When the right intrahepatic bile duct approach is necessary, percutaneous transhepatic biliary drainage should be selected. We previously proposed this algorithm in our review52 and clinical outcomes of this algorithm should be confirmed in prospective studies. Finally, both enteroscopy-assisted ERCP and EUS-AG stone treatment need expertise as well as dedicated devices, and we recommend those procedures should be performed by experts in high volume centers.
Table 5.
Comparisons of Enteroscopy-Assisted and Endoscopic Ultrasound-Guided Stone Management
| Advantages | Disadvantages | |
|---|---|---|
| Enteroscopy-assisted procedure | No bile leak | Difficult scope insertion |
| Physiological route | Can be time consuming | |
| Endoscopic ultrasound-guided procedure | Short scope insertion time | Risk of bile leak |
| Combined with a cholangioscope | No dedicated devices |
SUMMARY
Endoscopic management of BDS has been established as a standard of care but there still exist difficult BDS in clinical practice. Some emerging techniques and devices such as EPLBD, cholangioscope, enteroscopy-assisted ERCP and EUS-AG are increasingly utilized with reportedly high technical success rates and acceptable adverse event rates. Endoscopists should learn the indications, advantages and disadvantages of each technique for better management of difficult BDS. Treatment algorithm for difficult BDS according to the stone characteristics and the patient anatomy is to be further established in the future.
Footnotes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Iranmanesh P, Frossard JL, Mugnier-Konrad B, et al. Initial cholecystectomy vs sequential common duct endoscopic assessment and subsequent cholecystectomy for suspected gallstone migration: a randomized clinical trial. JAMA. 2014;312:137–144. doi: 10.1001/jama.2014.7587. [DOI] [PubMed] [Google Scholar]
- 2.Johnson AG, Hosking SW. Appraisal of the management of bile duct stones. Br J Surg. 1987;74:555–560. doi: 10.1002/bjs.1800740703. [DOI] [PubMed] [Google Scholar]
- 3.Ryozawa S, Itoi T, Katanuma A, et al. Japan Gastroenterological Endoscopy Society guidelines for en-doscopic sphincterotomy. Dig Endosc. 2018;30:149–173. doi: 10.1111/den.13001. [DOI] [PubMed] [Google Scholar]
- 4.Yasuda I, Itoi T. Recent advances in endoscopic management of difficult bile duct stones. Dig Endosc. 2013;25:376–385. doi: 10.1111/den.12118. [DOI] [PubMed] [Google Scholar]
- 5.Doshi B, Yasuda I, Ryozawa S, Lee GH. Current endoscopic strategies for managing large bile duct stones. Dig Endosc. 2018;30:59–66. doi: 10.1111/den.13019. [DOI] [PubMed] [Google Scholar]
- 6.Nakai Y, Kogure H, Yamada A, Isayama H, Koike K. Endoscopic management of bile duct stones in patients with surgically altered anatomy. Dig Endosc. 2018;30:67–74. doi: 10.1111/den.13022. [DOI] [PubMed] [Google Scholar]
- 7.Itoi T, Ryozawa S, Katanuma A, et al. Japan Gastroenterological Endoscopy Society guidelines for en-doscopic papillary large balloon dilation. Dig Endosc. 2018;30:293–309. doi: 10.1111/den.13029. [DOI] [PubMed] [Google Scholar]
- 8.Ogura T, Imanishi M, Kurisu Y, et al. Prospective evaluation of digital single-operator cholangioscope for diagnostic and therapeutic procedures (with videos) Dig Endosc. 2017;29:782–789. doi: 10.1111/den.12878. [DOI] [PubMed] [Google Scholar]
- 9.Brewer Gutierrez OI, Bekkali NLH, Raijman I, et al. Efficacy and safety of digital single-operator chol-angioscopy for difficult biliary stones. Clin Gastroenterol Hepatol. 2018;16:918–926. doi: 10.1016/j.cgh.2017.10.017. [DOI] [PubMed] [Google Scholar]
- 10.Tsujino T, Yamada A, Isayama H, et al. Experiences of biliary interventions using short double-balloon enteroscopy in patients with Roux-en-Y anastomosis or hepaticojejunostomy. Dig Endosc. 2010;22:211–216. doi: 10.1111/j.1443-1661.2010.00985.x. [DOI] [PubMed] [Google Scholar]
- 11.Dhir V, Isayama H, Itoi T, et al. Endoscopic ultrasonography-guided biliary and pancreatic duct inter-ventions. Dig Endosc. 2017;29:472–485. doi: 10.1111/den.12818. [DOI] [PubMed] [Google Scholar]
- 12.Minaga K, Kitano M. Recent advances in endoscopic ultrasound-guided biliary drainage. Dig Endosc. 2018;30:38–47. doi: 10.1111/den.12910. [DOI] [PubMed] [Google Scholar]
- 13.Komatsu Y, Kawabe T, Toda N, et al. Endoscopic papillary balloon dilation for the management of common bile duct stones: experience of 226 cases. Endoscopy. 1998;30:12–17. doi: 10.1055/s-2007-993721. [DOI] [PubMed] [Google Scholar]
- 14.Tsujino T, Kawabe T, Komatsu Y, et al. Endoscopic papillary balloon dilation for bile duct stone: im-mediate and long-term outcomes in 1000 patients. Clin Gastroenterol Hepatol. 2007;5:130–137. doi: 10.1016/j.cgh.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 15.Fujita N, Maguchi H, Komatsu Y, et al. Endoscopic sphincterotomy and endoscopic papillary balloon dilatation for bile duct stones: a prospective randomized controlled multicenter trial. Gastrointest Endosc. 2003;57:151–155. doi: 10.1067/mge.2003.56. [DOI] [PubMed] [Google Scholar]
- 16.Yasuda I, Fujita N, Maguchi H, et al. Long-term outcomes after endoscopic sphincterotomy versus endoscopic papillary balloon dilation for bile duct stones. Gastrointest Endosc. 2010;72:1185–1191. doi: 10.1016/j.gie.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 17.Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003;57:156–159. doi: 10.1067/mge.2003.52. [DOI] [PubMed] [Google Scholar]
- 18.Madhoun MF, Wani S, Hong S, Tierney WM, Maple JT. Endoscopic papillary large balloon dilation re-duces the need for mechanical lithotripsy in patients with large bile duct stones: a systematic review and meta-analysis. Diagn Ther Endosc. 2014;2014:309618. doi: 10.1155/2014/309618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park SJ, Kim JH, Hwang JC, et al. Factors predictive of adverse events following endoscopic papillary large balloon dilation: results from a multicenter series. Dig Dis Sci. 2013;58:1100–1109. doi: 10.1007/s10620-012-2494-8. [DOI] [PubMed] [Google Scholar]
- 20.Park JS, Jeong S, Lee DK, et al. Comparison of endoscopic papillary large balloon dilation with or without endoscopic sphincterotomy for the treatment of large bile duct stones. Endoscopy. 2019;51:125–132. doi: 10.1055/a-0639-5147. [DOI] [PubMed] [Google Scholar]
- 21.Hakuta R, Kogure H, Nakai Y, et al. Endoscopic papillary large balloon dilation without sphincteroto-my for users of antithrombotic agents: a multicenter retrospective study. Dig Endosc. 2019;31:316–322. doi: 10.1111/den.13326. [DOI] [PubMed] [Google Scholar]
- 22.Fujita Y, Iwasaki A, Sato T, et al. Feasibility of endoscopic papillary large balloon dilation in patients with difficult bile duct stones without dilatation of the lower part of the extrahepatic bile duct. Gut Liver. 2017;11:149–155. doi: 10.5009/gnl15634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schneider MU, Matek W, Bauer R, Domschke W. Mechanical lithotripsy of bile duct stones in 209 pa-tients--effect of technical advances. Endoscopy. 1988;20:248–253. doi: 10.1055/s-2007-1018186. [DOI] [PubMed] [Google Scholar]
- 24.Chang WH, Chu CH, Wang TE, Chen MJ, Lin CC. Outcome of simple use of mechanical lithotripsy of difficult common bile duct stones. World J Gastroenterol. 2005;11:593–596. doi: 10.3748/wjg.v11.i4.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Garg PK, Tandon RK, Ahuja V, Makharia GK, Batra Y. Predictors of unsuccessful mechanical lithotripsy and endoscopic clearance of large bile duct stones. Gastrointest Endosc. 2004;59:601–605. doi: 10.1016/S0016-5107(04)00295-0. [DOI] [PubMed] [Google Scholar]
- 26.Tandan M, Reddy DN. Extracorporeal shock wave lithotripsy for pancreatic and large common bile duct stones. World J Gastroenterol. 2011;17:4365–4371. doi: 10.3748/wjg.v17.i39.4365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Neuhaus H, Zillinger C, Born P, et al. Randomized study of intracorporeal laser lithotripsy versus ex-tracorporeal shock-wave lithotripsy for difficult bile duct stones. Gastrointest Endosc. 1998;47:327–334. doi: 10.1016/S0016-5107(98)70214-7. [DOI] [PubMed] [Google Scholar]
- 28.Veld JV, van Huijgevoort NCM, Boermeester MA, et al. A systematic review of advanced endoscopy-assisted lithotripsy for retained biliary tract stones: laser, electrohydraulic or extracorporeal shock wave. Endoscopy. 2018;50:896–909. doi: 10.1055/a-0637-8806. [DOI] [PubMed] [Google Scholar]
- 29.Buxbaum J, Sahakian A, Ko C, et al. Randomized trial of cholangioscopy-guided laser lithotrip-sy versus conventional therapy for large bile duct stones (with videos) Gastrointest Endosc. 2018;87:1050–1060. doi: 10.1016/j.gie.2017.08.021. [DOI] [PubMed] [Google Scholar]
- 30.Angsuwatcharakon P, Kulpatcharapong S, Ridtitid W, et al. Digital cholangioscopy-guided laser versus mechanical lithotripsy for large bile duct stone removal after failed papillary large-balloon dilation: a randomized study. Endoscopy. 2019;51:1066–1073. doi: 10.1055/a-0848-8373. [DOI] [PubMed] [Google Scholar]
- 31.Deprez PH, Garces Duran R, Moreels T, et al. The economic impact of using single-operator cholangi-oscopy for the treatment of difficult bile duct stones and diagnosis of indeterminate bile duct stric-tures. Endoscopy. 2018;50:109–118. doi: 10.1055/s-0043-121268. [DOI] [PubMed] [Google Scholar]
- 32.Moreels TG. Update in enteroscopy: new devices and new indications. Dig Endosc. 2018;30:174–181. doi: 10.1111/den.12920. [DOI] [PubMed] [Google Scholar]
- 33.Tanisaka Y, Ryozawa S, Mizuide M, et al. Usefulness of the “newly designed” short-type single-balloon enteroscope for ERCP in patients with Roux-en-Y gastrectomy: a pilot study. Endosc Int Open. 2018;6:E1417–E1422. doi: 10.1055/a-0754-2290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yamada A, Kogure H, Nakai Y, et al. Performance of a new short-type double-balloon endoscope with advanced force transmission and adaptive bending for pancreaticobiliary intervention in patients with surgically altered anatomy: a propensity-matched analysis. Dig Endosc. 2019;31:86–93. doi: 10.1111/den.13261. [DOI] [PubMed] [Google Scholar]
- 35.Itoi T, Sofuni A, Itokawa F, et al. Diagnostic and therapeutic peroral direct cholangioscopy in patients with altered GI anatomy (with videos) Gastrointest Endosc. 2012;75:441–449. doi: 10.1016/j.gie.2011.09.038. [DOI] [PubMed] [Google Scholar]
- 36.Koshitani T, Matsuda S, Takai K, et al. Direct cholangioscopy combined with double-balloon enter-oscope-assisted endoscopic retrograde cholangiopancreatography. World J Gastroenterol. 2012;18:3765–3769. doi: 10.3748/wjg.v18.i28.3765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hakuta R, Kogure H, Isayama H, et al. Electrohydraulic lithotripsy of large bile duct stones under di-rect cholangioscopy with a double-balloon endoscope. Endoscopy. 2015;47:E519–E520. doi: 10.1055/s-0034-1392669. [DOI] [PubMed] [Google Scholar]
- 38.Sato T, Kogure H, Nakai Y, Isayama H, Koike K. Electrohydraulic lithotripsy under double-balloon en-doscope-assisted direct cholangioscopy for treatment of choledocholithiasis in a patient with Roux-en-Y gastrectomy. VideoGIE. 2018;3:113–114. doi: 10.1016/j.vgie.2017.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hakuta R, Kogure H, Nakai Y, et al. Successful endoscopic lithotripsy using a new digital cholangio-scope through an overtube placed by an enteroscope. Endoscopy. 2018;50:E269–E271. doi: 10.1055/a-0640-2817. [DOI] [PubMed] [Google Scholar]
- 40.Tonozuka R, Itoi T, Sofuni A, et al. Novel peroral direct digital cholangioscopy-assisted lithotripsy us-ing a monorail technique through the overtube in patients with surgically altered anatomy (with vid-eo) Dig Endosc. 2019;31:203–208. doi: 10.1111/den.13310. [DOI] [PubMed] [Google Scholar]
- 41.Mallery S, Matlock J, Freeman ML. EUS-guided rendezvous drainage of obstructed biliary and pan-creatic ducts: report of 6 cases. Gastrointest Endosc. 2004;59:100–107. doi: 10.1016/S0016-5107(03)02300-9. [DOI] [PubMed] [Google Scholar]
- 42.Tsuchiya T, Itoi T, Sofuni A, Tonozuka R, Mukai S. Endoscopic ultrasonography-guided rendezvous technique. Dig Endosc. 2016;28:96–101. doi: 10.1111/den.12611. [DOI] [PubMed] [Google Scholar]
- 43.Weilert F, Binmoeller KF, Marson F, Bhat Y, Shah JN. Endoscopic ultrasound-guided anterograde treatment of biliary stones following gastric bypass. Endoscopy. 2011;43:1105–1108. doi: 10.1055/s-0030-1256961. [DOI] [PubMed] [Google Scholar]
- 44.Iwashita T, Yasuda I, Doi S, et al. Endoscopic ultrasound-guided antegrade treatments for biliary dis-orders in patients with surgically altered anatomy. Dig Dis Sci. 2013;58:2417–2422. doi: 10.1007/s10620-013-2645-6. [DOI] [PubMed] [Google Scholar]
- 45.Itoi T, Sofuni A, Tsuchiya T, Ijima M, Iwashita T. Endoscopic ultrasonography-guided transhepatic an-tegrade stone removal in patients with surgically altered anatomy: case series and technical review (with videos) J Hepatobiliary Pancreat Sci. 2014;21:E86–E93. doi: 10.1002/jhbp.165. [DOI] [PubMed] [Google Scholar]
- 46.Iwashita T, Nakai Y, Hara K, Isayama H, Itoi T, Park DH. Endoscopic ultrasound-guided antegrade treatment of bile duct stone in patients with surgically altered anatomy: a multicenter retrospective cohort study. J Hepatobiliary Pancreat Sci. 2016;23:227–233. doi: 10.1002/jhbp.329. [DOI] [PubMed] [Google Scholar]
- 47.Nakai Y, Isayama H, Koike K. Two-step endoscopic ultrasonography-guided antegrade treatment of a difficult bile duct stone in a surgically altered anatomy patient. Dig Endosc. 2018;30:125–127. doi: 10.1111/den.12965. [DOI] [PubMed] [Google Scholar]
- 48.Hosmer A, Abdelfatah MM, Law R, Baron TH. Endoscopic ultrasound-guided hepaticogastrostomy and antegrade clearance of biliary lithiasis in patients with surgically-altered anatomy. Endosc Int Open. 2018;6:E127–E130. doi: 10.1055/s-0043-123188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.James TW, Fan YC, Baron TH. EUS-guided hepaticoenterostomy as a portal to allow definitive ante-grade treatment of benign biliary diseases in patients with surgically altered anatomy. Gastrointest Endosc. 2018;88:547–554. doi: 10.1016/j.gie.2018.04.2353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mukai S, Itoi T, Sofuni A, et al. EUS-guided antegrade intervention for benign biliary diseases in pa-tients with surgically altered anatomy (with videos) Gastrointest Endosc. 2019;89:399–407. doi: 10.1016/j.gie.2018.07.030. [DOI] [PubMed] [Google Scholar]
- 51.Kamiyama R, Ogura T, Okuda A, et al. Electrohydraulic lithotripsy for difficult bile duct stones under endoscopic retrograde cholangiopancreatography and peroral transluminal cholangioscopy guidance. Gut Liver. 2018;12:457–462. doi: 10.5009/gnl17352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nakai Y, Kogure H, Isayama H, Koike K. Endoscopic ultrasound-guided biliary drainage for benign bil-iary diseases. Clin Endosc. 2019;52:212–219. doi: 10.5946/ce.2018.188. [DOI] [PMC free article] [PubMed] [Google Scholar]