Abstract
Objective:
We sought to test whether participation in an online group including IUD users influenced IUD-related knowledge, attitudes, and behavior among IUD non-users, as a proof-of-concept evaluation of information dissemination for less commonly used or novel contraceptives.
Study design:
We conducted a blinded, randomized controlled trial on the effect of online communication with IUD users within an online program called Birth Control Connect. Participants were women age 18–45 living in the United States who had never used an IUD. We invited participants randomized to the intervention to join two-week, nine-member discussion groups including four satisfied IUD users and five IUD non-users; we invited control participants to groups including nine IUD non-users. We performed chi-squared tests on IUD knowledge, information-seeking, informational support and use in immediate post-surveys, and t-tests comparing change in IUD attitudes and frequency of logins to discussion groups.
Results:
We invited 488 IUD non-users and enrolled them into 70 groups between October 2015 and April 2016. We found increased positive attitudes towards the IUD in the intervention arm (0.65-point increase between pre- and post-surveys, versus 0.05 mean change for control arm, p = 0.03 for hormonal IUD, with a trend in the same direction for the non-hormonal IUD). Informational support also increased, with 70.3% of intervention arm participants self-reporting that they gained a better idea of what the IUD would be like, compared to 51.3% in control arm (p < 0.01). Of intervention participants, 63.3% versus 51.3% of control participants reported gaining new information from their group (p = 0.03). There were no differences in correct responses to knowledge items or information-seeking between groups.
Conclusions:
Online exposure to IUD users increased positive attitudes toward the IUD and informational support for decision-making about the IUD among non-users.
Implications statement:
Online spaces provide a promising environment for the exchange of accurate, useful contraceptive information based on real user experiences. Interventions aiming to harness social communication through structured online conversations (e.g., on existing social media platforms) about user experiences with lesser-known contraceptive methods such as the IUD may be worthwhile.
Keywords: Contraception, IUD, Social, Communication, Internet, Online
1. Introduction
While attention has increasingly been paid to financial and logistical barriers to use of contraceptive methods, we do not have adequate understanding of how best to ensure that individuals receive information about contraceptive methods that enables them to make decisions that reflect their preferences [1]. While most previous educational efforts have focused on the clinical encounter or on formal educational environments [1], peers are influential sources of contraceptive information [2-6], and individuals often consider contraceptive information received from peers more trustworthy than from clinicians [7-13]. Social communication therefore has the potential to improve individuals’ knowledge of their contraceptive options through exposure to others’ lived experiences with specific methods. This sharing may inform method choice [6], and normalize use of specific methods and contraception in general.
Structured social communication interventions, in which users provide information about their lived experience of method use, has the potential to provide individuals making contraceptive decisions with information about methods in a factual and engaging manner. Given that peers are more likely to communicate negative experiences with contraceptive methods than positive experiences [4,6], ensuring communication with satisfied users about their lived experience can improve balance in the information and norms disseminated through social networks. This type of intervention may be particularly useful for information-gathering and decision-making for less commonly used methods that may be unknown to potential users.
The intrauterine device (IUD) serves as a useful case study for testing the proof-of-concept that social communication affects contraceptive knowledge, attitudes, and behaviors, given its relatively low use and the presence of documented knowledge-related barriers to use [14]. While use of intrauterine devices (IUDs) has recently increased in the United States, it remains relatively low compared with use of other contraceptive methods [15], and compared to other high-income countries such as those in Europe [16]. Studies suggest that informal social communication may be particularly influential in decision making about this method [6,10,17,18], with a preponderance of negative information – much of it second hand and from older relatives – reported through peer networks [6]. Women who had not used this method valued hearing about the experiences of prior users [6]. This is consistent with the Diffusion of Innovations theory [19,20], which suggests that for new or infrequently used interventions or technologies, early adopters have a role in diffusing information, practices, and norms within social networks [19]. Facilitating social communication between IUD users and non-users therefore has the potential to decrease barriers to use of this method among non-users.
In this study, we aimed to examine the effect of online exposure to satisfied IUD users on IUD-related behavior, knowledge, and attitudes among IUD non-users.
2. Methods and materials
We conducted a blinded, randomized trial on the effect of facilitated online communication with currently satisfied IUD users on IUD non-users. We designed an Internet community called Birth Control Connect, which consisted of closed online discussion groups of nine members each designed to support communication about contraception over a two-week period. Intervention groups included both IUD non-user participants and current IUD users, and control groups included only IUD non-users. We conducted surveys at baseline and follow-up. The institutional review board of University of Pennsylvania approved the study.
Clinicaltrials.gov trial number: #NCT02279043.
2.1. Study setting and recruitment
We sought to recruit IUD non-users and users from across the US. Recruitment activities for IUD non-users and users took place between October 2015 and April 2016. We posted on social media and forum-based websites to recruit IUD non-user participants. Eligible participants were women between the ages of 18 to 45 who had ever been sexually active with men, desired pregnancy prevention, and had never used an IUD.
We recruited IUD users to serve as informational sources in the intervention arm. We used email flyers to recruit IUD users through professional and social networks with stated interests in reproductive health. Eligible IUD users were women age 18–45 who were satisfied with the IUD as a contraceptive method. Potential participants and IUD users first visited an eligibility screening page, and those who screened as eligible had the opportunity to give online consent.
We randomly selected IUD non-user participants and IUD users from the total pool of individuals who gave consent to enroll. We randomized IUD non-user participants to a group in the intervention arm, including five IUD non-users and four IUD users in each group, or a control arm group with nine IUD non-users and no IUD users. Research team members randomized IUD non-user participants using an electronic random number generator. Because the control arm required more non-user participants than the intervention arm to achieve an equal number of groups in each arm, the generator was programmed for 35.7% probability of assignment to the intervention arm and 64.3% probability of assignment to the control arm.
2.2. Study intervention
Birth Control Connect groups were dedicated to discussion of member experiences and perspectives related to contraception (see screenshot of dashboard in Fig. 1). Members were able to “See” other members, including their screen name and list of contraceptive methods they had ever used, ask questions, and respond to other members. Each business day during the two-week study period, the research team posted prompts to elicit discussion (e.g. “If you’re using a birth control method right now, how did you choose it?”). Table 4 includes a list of all conversation prompts. All group members received daily digest emails featuring the most recent topics in their group and encouraging them to engage with the group. The research team’s facilitation methods were identical between arms.
Fig. 1.
Screenshot of Birth Control Connect discussion group.
Table 4.
Conversation prompts included in Birth Control Connect User Groups.
| Intervention Day | Prompt posted to online user groups (both arms) |
|---|---|
| Day 1 | Bedsider video of young person communicating with Grandmother about contraception https://www.youtube.com/watch?v=COKYqgpc7dQ Introduction: You might not want to ask your Grandma all your burning questions – that’s what Birth Control Connect is for! Prompt 1: Since it’s our first day, introduce yourself and let us know what brings you to the community. When you’re done, you can ask your own question by clicking the purple button Prompt 2: If you’re using a birth control method right now, how did you choose it? |
| Day 2 | Prompt 3: Looking at your connections, what birth control methods are people using the most in this group? What do you think of these methods? |
| Day 3 | Prompt 4: What do you think about the side effects of birth control? |
| Day 4 | Prompt 5: What have you heard about the IUD? Have any questions about this method? Prompt 6: “If you’re using a birth control method right now, what do you like the most about your method?” |
| Day 5 | Prompt 7: The IUD is almost twice as popular among women age 15–45 today as it was 10 years ago. Why do you think more and more women are choosing to use an IUD? |
| Day 6 | Prompt 8: Some birth control methods take a little more brain power than others. Has it ever been hard for you to remember to use birth control? |
| Day 7 | Prompt 9: Condoms are great – they protect against pregnancy and sexually transmitted infections! Have you ever used condoms for birth control? What do you like or not like about them? Prompt 10: There are a lot of birth control options out there – which one do you think works the best to prevent pregnancy? |
| Day 8 | Video: Bedsider, “Guy's Guide to Birth Control: Intro” https://www.youtube.com/watch?v=W5foWuAlQN8&list=PLGg3x5v82SZw2TLWtjAif8tiLbLshgap9 Prompt 11: “Everyone can learn something new about birth control, even if they don’t use a method themselves. How much do your partner or partners know about your birth control method?” |
| Day 9 | Prompt 12: The birth control pill was the first hormonal birth control available - and is still the most commonly used. With all the other methods to choose from today, what do you think about taking a pill every day? |
| Day 10 | Prompt 13: If you’re using a birth control method right now, what’s the #1 thing you want other women to know about it? |
| Day 11 | Prompt 14: Some reversible forms of birth control last up to 10 years. If you’re using a method, how long does it last? Did that influence your decision to get it? Prompt 15: Sometimes mistakes happen. What would you do if you ever forgot to take the pill, wear your patch, or use a condom? |
| Day 12 | Prompt 16: When you think about how birth control fits into your life, how does the IUD compare to other methods? |
2.3. Outcomes and measures
We invited IUD non-user participants to complete surveys before and after the two-week study period. Participants received $10 via Paypal for the baseline survey and $15 for the post-survey. The primary outcome was initiation of IUD use by the end of the study period, measured by self-report in the post-survey. Secondary outcomes included: (1) IUD attitudes, using metrics described below; (2) IUD knowledge, including items related to method safety and effectiveness; (3) perceived informational support, including whether the intervention provided new information about IUDs, and whether or not participants learned what using an IUD would be like; and (4) other reported sources of IUD information accessed during the study period. Participants reported informational sources on the post-survey and we measured clicks to Bedsider.org, a contraceptive information resource hosted by Power to Decide. We also measured frequency of Birth Control Connect logins during the study period.
We used attitudinal scales previously developed to assess respondents’ overall attitudes towards a range of contraceptive methods, both for themselves and for others their age [21]. For each method they reported having heard of, we asked participants to respond on a scale from 0 (“terrible method”) to 10 (“great method”) to the following questions: “Overall, how would you rate each of the following as a birth control method for yourself (even if you’ve never used it)?” and “Overall, how would you rate each of the following as a birth control method for women your age, in general?”, with “women your age” serving as a proxy for peers in general [22]. We derived knowledge items from the National Survey of Reproductive and Contraceptive Knowledge [22]. We asked knowledge items on safety and effectiveness, as well as informational support items, on a 5-point Likert scale where 1 = Strongly disagree and 5 = Strongly agree. We chose scale response options for these items instead of correct-incorrect because, while these are knowledge constructs, “safe” and “effective” are relative terms which may range in meaning to participants. We dichotomized responses as 4 or 5, versus 1, 2, or 3.
2.4. Statistical analysis
We calculated the sample size as 270 IUD non-users and 90 IUD users, populating 20 groups in each arm. This calculation accounted for an unbalanced sample, due to more IUD non-user participants in each group in the control arm than the intervention arm. We calculated that with this sample size, we would have a detectable standard effect size of approximately 0.4 for continuous outcomes and 0.2 for binary outcomes, which is small to medium according to generally accepted standard effect size standards [23] and thus acceptable for a proof-of-concept study.
We analyzed outcomes for participants in the arm to which they had been randomized. We performed bivariate analyses for all outcomes at the individual participant level. We conducted regression analyses adjusting for cluster effects by discussion group for those outcomes with significant results in bivariate analyses.
We assessed bivariate comparisons using chi-squared tests for dichotomous behavior, knowledge, informational support, and information-seeking outcomes; t-tests of change in continuous attitude outcomes; and t-test of number of group logins. We excluded participants who did not complete a post-survey in analyses using post-survey data. In analyzing attitude changes, we excluded participants who did not complete both a baseline and post-survey, as well as those who had not heard of the IUD at baseline. Among those who had never heard of the IUD at baseline, we compared rates of learning about the IUD and post-survey attitudes between arms. We performed mixed effects linear and logistic regressions adjusting for cluster effects by online discussion group assignment for those outcomes with a significant difference in bivariate tests. We performed an attritional analysis using chi-squared tests to assess for differences in follow-up by age, race/ethnicity, parity, or study condition. We performed all analyses with Stata 14 software.
3. Results
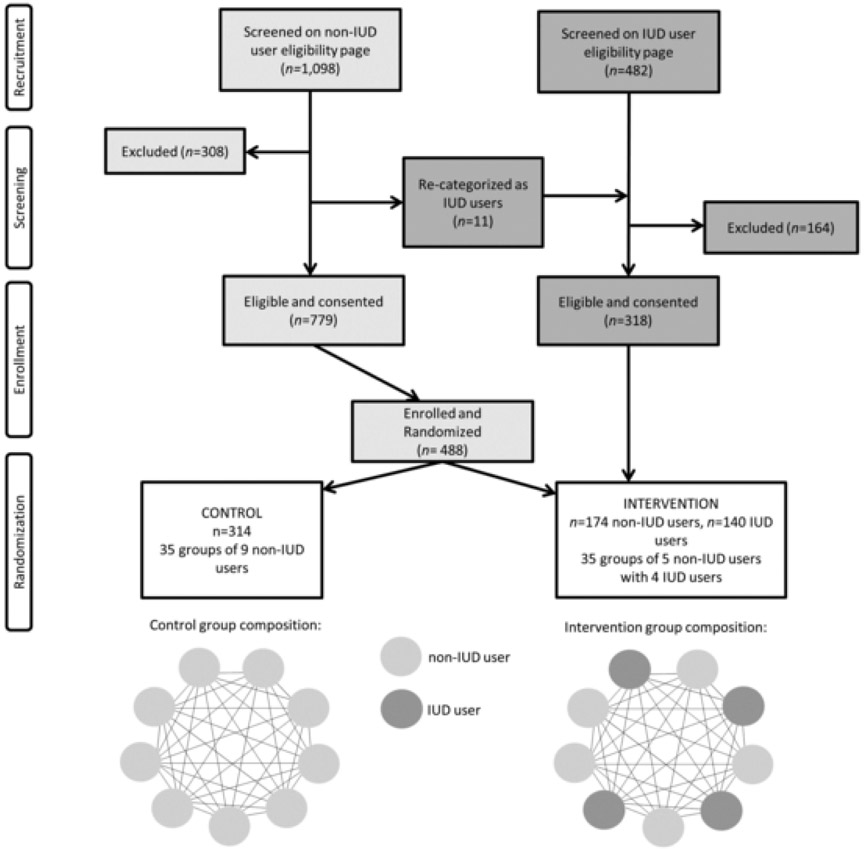
A total of 1,580 women submitted responses on the eligibility screening page (see Fig. 2). Of 779 eligible and consented women, we randomly selected 490 to participate. Post-randomization, we excluded two participants because they reported IUD use in the baseline survey after screening eligible as IUD non-users. We recruited beyond our sample size calculation to obtain a more racially/ethnically diverse sample, as early recruitment yielded a sample of predominantly White participants.
Fig. 2.
Recruitment, screening, enrollment, and randomization of IUD non-user study participants to intervention and control Birth Control Connect groups [Consolidated Standards of Reporting Trials (CONSORT) diagram].
Of 488 IUD non-users enrolled, we assigned 174 to the intervention arm and invited them to 35 groups with five IUD non-users and four IUD users each. In the control arm, we assigned 314 IUD non-users to 35 groups of nine IUD non-users each. Seventy-one percent of participants completed both baseline and post-survey. In chi-squared tests, neither baseline characteristics nor arm assignment were associated with completion of both surveys. Table 1 presents the demographic characteristics of participating IUD non-users. IUD non-user participants had a mean age of 25.1 years (standard deviation (SD) 4.60). The majority of participants were White (61.7%), and a majority of participants reported using the contraceptive pill at baseline (54.6%). There were no significant differences in demographics by arm.
Table 1.
Birth Control Connect online participant characteristics at baseline, by study arm.
| Characteristic* | Intervention [Online discussion groups with IUD users] (n = 174), % |
Control [Online discussion groups with no IUD users] (n = 314), % |
|---|---|---|
| Age group | ||
| 18–24 | 51.7 | 50.6 |
| 25–34 | 45.4 | 43.6 |
| 35–45 | 2.9 | 5.4 |
| Missing | 0 | 0.3 |
| Race/ethnicity | ||
| Asian | 6.9 | 7.6 |
| Black/African American | 12.6 | 12.1 |
| Hispanic/Latina | 6.3 | 11.5 |
| White | 66.7 | 58.9 |
| Other | 5.2 | 5.7 |
| Missing | 2.3 | 4.1 |
| Number of children | ||
| 0 children | 88.5 | 89.8 |
| ≥1 child | 11.5 | 9.9 |
| Missing | 0 | 0.3 |
| Number of pregnancies** | ||
| 0 pregnancies | 47.1 | 50.6 |
| ≥1 pregnancy | 12.1 | 9.2 |
| Missing | 40.8 | 40.1 |
| Birth control method used at baseline (may report more than one) | ||
| Pill | 54.6 | 54.6 |
| Patch | 1.2 | 3.5 |
| Ring | 5.8 | 4.2 |
| Shot | 6.9 | 3.8 |
| Arm implant | 9.8 | 9.2 |
| Condoms | 36.8 | 35.0 |
| Withdrawal | 21.3 | 22.3 |
| Female sterilization | 2.3 | 1.3 |
| Male sterilization | 1.2 | 2.2 |
| Other | 1.2 | 1.9 |
| None | 4.0 | 5.1 |
| Birth control methods ever used | ||
| Pill | 82.2 | 79.0 |
| Patch | 11.5 | 10.2 |
| Ring | 12.1 | 12.4 |
| Shot | 10.9 | 15.3 |
| Arm implant | 4.0 | 4.5 |
| Condoms | 78.2 | 80.3 |
| Withdrawal | 52.9 | 55.1 |
| Female sterilization | 0 | 0.3 |
| Male sterilization | 0 | 0.3 |
| Other | 0 | 0.3 |
| Parental education | ||
| High school graduate or less | 17.8 | 16.2 |
| Some college or 4-year college graduate | 32.2 | 38.9 |
| More than 4-year college graduate | 23.6 | 16.9 |
| Missing | 26.4 | 28.0 |
| Geographic region | ||
| Northeast (Connecticut, Maine, Massachusetts, | 32.2 | 21 |
| New Hampshire, Rhode Island, Vermont, New Jersey, New York, and Pennsylvania) | ||
| Midwest (Illinois, Indiana, Michigan, Ohio, | 18.4 | 17.5 |
| Wisconsin, Iowa, Kansas, Minnesota, Missouri, Nebraska, North Dakota, and South Dakota) | ||
| South: (Delaware, Florida, Georgia, Maryland, North Carolina, South Carolina, Virginia, District of Columbia, West Virginia, Alabama, Kentucky, Mississippi, Tennessee, Arkansas, Louisiana, Oklahoma, Texas) | 24.1 | 37.6 |
| West (Arizona, Colorado, Idaho, Montana, Nevada, New Mexico, Utah, Wyoming, (Alaska, California, Hawaii, Oregon, and Washington) | 25.3 | 25.3 |
| Unknown state | 0 | 1 |
No differences in characteristics were significantly different by study arm.
Missingness is relatively high for number of pregnancies and parental education because study follow-up survey assessed these variables, and were thus not available for participants lost to follow-up. The pregnancy question was optional.
Overall, we screened 482 IUD users; 318 were eligible, and of these, we randomly selected 140 to enroll in the intervention group arm with four IUD users in each of the 35 groups. The mean age of IUD users was 26.9 years old (SD 4.85). We recruited IUD users from 35 different US states. Of the 140 IUD users, 93 reported hormonal IUD use, 32 reported nonhormonal IUD use, and 15 did not specify.
Participants had an average of 7.90 logins during the study period (SD 6.89), with number of logins ranging from 0-63. There were 59 participants (12.1%) who never logged in. As none of these 59 participants completed a post-survey, we did not include their data in outcome analyses of survey data. Number of logins and percentage of participants who never logged in were not differential by arm.
On enrollment, participants in both arms gave IUDs a mean rating between 5 and 7 on a scale of 0–10 as a method for themselves, and between 7 and 8 as a method for women their age (Table 3). Participants reported greater increases in positive attitude regarding IUDs in the intervention group compared to the control group. This increase was statistically significant for rating of the hormonal IUD for women their age (+0.65 in intervention arm, +0.05 in control arm, p = 0.03). The increase approached statistical significance for the non-hormonal IUD for women their age (+0.50 in intervention group, +0.04 in control, p = 0.08).
Table 3.
Changes in Birth Control Connect online participant attitudes about the hormonal and non-hormonal IUD in pre- and post-surveys* by study arm.
| Mean participant rating of hormonal IUD… |
Intervention group [Online discussion groups with IUD users](n = 119) |
Control group [Online discussion groups with no IUD users](n = 211) |
p-value of t-test of mean difference between arms |
||||
|---|---|---|---|---|---|---|---|
| Pre-survey | Post-survey | Mean difference | Pre-survey | Post-survey | Mean difference | ||
| … as a contraceptive method for self | 6.17 | 6.69 | 0.50 | 6.52 | 6.74 | 0.16 | 0.28 |
| … as a contraceptive method for women of same age | 7.66 | 8.30 | 0.65 | 7.87 | 7.92 | 0.05 | 0.03 |
| Mean participant rating of non- hormonal IUD… |
Intervention group (n = 114) | Control group (n = 207) | |||||
| … as a contraceptive method for self | 5.91 | 6.08 | 0.22 | 6.24 | 6.33 | 0.04 | 0.58 |
| … as a contraceptive method for women of same age | 7.54 | 8.02 | 0.50 | 7.53 | 7.49 | 0.00 | 0.08 |
Included Data is only for those participants who completed both baseline and post-surveys, and who reported having heard of the hormonal or non-hormonal IUD in both surveys. More participants reported having heard of the hormonal IUD in both surveys than of the non-hormonal IUD, resulting in the difference in sample sizes for ratings of each type.
There were no significant differences by arm in IUD-related knowledge at follow-up (Table 2). The majority of participants in both arms agreed or strongly agreed that the IUD is safe and very effective at preventing pregnancy. More intervention participants correctly responded that the IUD is more effective than the contraceptive pill in preventing pregnancy, approaching statistical significance (56.2% versus 46.5%, p = 0.08).
Table 2.
Birth Control Connect post-participation survey responses of IUD knowledge, informational support, information seeking, and use, by study arm.
| Intervention [Online discussion groups with IUD users] (n = 128), |
Control [Online discussion groups with no IUD users] (n = 226), |
||
|---|---|---|---|
| Outcome | % | % | p-value |
| Knowledge Agree or strongly agree that the IUD is safe | 80.5 | 76.1 | 0.34 |
| Agree or strongly agree that the IUD is very effective at preventing pregnancy | 89.8 | 89.8 | 0.99 |
| Correctly responded that the IUD is more effective than the | 56.3 | 46.5 | 0.08 |
| pill at preventing pregnancy Informational support Agree or strongly agree that people on the Birth Control Connect group gave them information about the IUD they didn’t have before | 63.3 | 51.3 | 0.03 |
| Agree or strongly agree that people on Birth Control Connect gave them a better idea of what it would be like to have an IUD | 70.3 | 51.3 | <0.01 |
| Information seeking Reported looking for online information about the IUD | 46.1 | 45.6 | 0.93 |
| (outside Birth Control Connect) in past two weeks Reported consulting a healthcare provider about the | 7.8 | 6.7 | 0.68 |
| IUD in the past two weeks Reported talking to other women they know about the IUD in the past two weeks | 43.8 | 38.5 | 0.33 |
| IUD use (hormonal or non-hormonal) | 1.6 | 1.8 | 0.89 |
In both arms, 4.7% of participants reported not having heard of the hormonal IUD at baseline, and slightly higher percentages reported not having heard of the non-hormonal IUD (8.8% of intervention participants vs. 5.7% of control participants [difference not significant]). The majority of participants unfamiliar with these methods reported knowing about them in the post-survey. This did not differ significantly by arm (data not shown).
More participants in the intervention arm agreed or strongly agreed that their group gave them new information about the IUD (63.3% versus 51.3%, p = 0.03). More participants in the intervention arm agreed or strongly agreed that the group helped them learn what it would be like to have an IUD (70.3% versus 51.3%, p < 0.001). There were no significant differences in participant reports of seeking additional online information about IUDs, consulting with a healthcare provider about the IUD, or communicating with other peers about the IUD during the study period. Overall, 29.9% of participants clicked on links to Bedsider.org during the study period. This did not differ significantly by study arm.
At the end of the two-week study period, there were no significant differences in IUD use by arm (1.6% in the intervention arm vs. 1.8% in the control arm, p = 0.89).
4. Discussion
Patients of reproductive age increasingly consult online websites, message boards, and social media as sources of health information [24-29]. Internet-based communication can help to disseminate information about relatively lesser-known contraceptive methods, such as the IUD, through interaction between method users and non-users. Other studies have explored online educational didactic programs and assessed social media’s influence on birth control choices [30]. In this study, we applied the approach of actively facilitating online social communication about the lived experience of contraceptive use, using IUDs as a case study. The feasibility and acceptability of this intervention was supported by its relatively high uptake, with a mean number of 7.9 logins. This intervention may therefore serve as a model for future interventions in populations in which information and norms about specific methods are barriers to individuals being able to consider use of these methods.
Participants reported improved attitudes about the IUD, and that they received new information after interacting online with satisfied IUD users over a two-week period. These effects can reduce barriers to use of the IUD for individuals for whom this method is compatible with their values and preferences. While we had originally chosen IUD uptake as our primary outcome because it aligned with the Diffusion of Innovations Theory’s emphasis on innovation uptake, increasing attention to the preference-sensitive nature of contraceptive decision making has made clear the limitations of any outcome focused on uptake of a specific method [31]. Attention to outcomes related to normative attitudes and information support is in fact more consistent with a patient-centered approach focusing on people’s ability to consider the full range of contraceptive options that may be acceptable to them.
Our findings have implications beyond the IUD, in demonstrating how social communication can help to disseminate information about lesser-known methods (with relevance to future contraceptive innovations) and thus expand awareness about the number of contraceptive options. Interventions to encourage experience-sharing with lesser-known methods may take place in familiar and accessible online spaces. For example, hashtags, “tweetorials” or “Tweetups” on Twitter or “Ask Me Anything” threads on Reddit are familiar user formats that can be used to help structure user-based conversation around personal method experiences. Future research can leverage existing social media modalities to assess engagement and impact of interventions to disseminate peer-based information.
Online social communication interventions for contraceptive education have the added benefit of occurring outside of the clinical environment, in which embedded power dynamics between patient and provider can enable directive contraceptive counseling practices [32,33]. Patients have reported feeling pressure from providers following implementation of clinical education interventions targeting long-acting reversible contraception (LARC) use [34]. Online information sharing can help more people obtain and weigh contraceptive information on their own terms, potentially providing a counterbalance to directive method-based counseling received in a healthcare setting. It is imperative that all forms of contraceptive education remain non-directive and serve to avail individuals of information about all of their contraceptive options. Future interventions can build upon our findings to design online peer-based communications that foster conversation about the full range of options – particularly as more options emerge – to allow for access to methods that are most aligned with individual values and preferences.
In doing this work, it will be essential to carefully consider how social communication interventions themselves have the potential to be designed and applied in problematic manners. As an example, at the time of developing our intervention, we decided to include only satisfied users (as opposed to both satisfied and unsatisfied users). We made this decision based on the documented prevalence of negative social communication about IUDs, our previous findings of non-IUD users’ desire for information from users about their experiences, the reliance on unscripted and organic communication within the intervention groups, and the short time frame and lack of intensive nature of the intervention. In retrospect, we recognize this approach has the potential to overemphasize positive aspects of use of IUDs, and we would recommend similar studies include a more representative range of experiences. In general, those designing future interventions should carefully consider how aspects of design such as this has the potential to support individuals’ ability to make autonomous decisions about their contraceptive choices, or in fact to interfere with this ability.
Limitations of our study include that, despite attempts to obtain a racially/ethnically diverse sample, the majority of the study population (61.7%) was White, resulting in lower generalizability of findings. More attention to recruiting Hispanic/Latina participants, as well as a Spanish-language Birth Control Connect groups, would have improved recruitment. The study period was only two weeks long for the sake of feasibility, but contraceptive decision-making is often a longer-term process, and acting on the decision to use an IUD in particular can take several weeks due to access-related barriers. This short time frame may also underlie our finding of changes in attitudes about the IUD for “women your age,” without a similar change in attitude about the method for the woman herself, as it may require less time to shift general normative attitudes than attitudes regarding one’s own method use. We did not assess intention to change methods, which may have been a more sensitive measure of impact during the two-week period. We enrolled a wide age range of women ages 18–40, comprising different developmental stages and not conforming to typical online peer interaction; however, this design also allowed for participant access to a diverse range of user experience; this may have a benefit for information-seekers as compared with typical peer communication within similar age groups. Finally, we had loss to follow up of 29%, although baseline characteristics and study arm did not predict loss to follow up. While unmeasured factors may have influenced attrition, we hypothesize that risk of biased results due to attrition is relatively low.
In conclusion, online social communication can impact contraceptive attitudes and have potential to affect contraceptive knowledge and behavior through enhancing the ability to consider the full range of method options. Future work should expand current online modes of peer communication to spread high-quality information and support autonomous decision making.
Acknowledgments
This work was supported by the William and Flora Hewlett Foundation [Grant #2014-9716], Menlo Park, CA.
Footnotes
Declaration of interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- [1].Pazol K, Zapata LB, Dehlendorf C, Malcolm NM, Rosmarin RB, Frederiksen BN Impact of contraceptive education on knowledge and decision making: an updated systematic review. Am J Prev Med 2018;55(5):703–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Madhavan S, Adams A, Simon D Women’s networks and the social world of fertility behavior. Int Perspect Sex Reprod Health 2003;58–68. [DOI] [PubMed] [Google Scholar]
- [3].Gayen K, Raeside R Social networks and contraception practice of women in rural Bangladesh. Soc Sci Med 2010;71(9):1584–1592. [DOI] [PubMed] [Google Scholar]
- [4].Rutenberg N, Watkins SC The buzz outside the clinics: conversations and contraception in Nyanza Province. Kenya Stud Fam Plann 1997;290–307. [PubMed] [Google Scholar]
- [5].Valente TW, Saba WP Campaign exposure and interpersonal communication as factors in contraceptive use in Bolivia. J Health Commun 2001;6(4):303–322. [DOI] [PubMed] [Google Scholar]
- [6].Anderson N, Steinauer J, Valente T, Koblentz J, Dehlendorf C Women’s social communication about IUDs: a qualitative analysis. Perspect Sex Reprod Health 2014;46(3):141–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Gilliam ML, Warden M, Goldstein C, Tapia B Concerns about contraceptive side effects among young Latinas: a focus-group approach. Contraception 2004;70(4):299–305. [DOI] [PubMed] [Google Scholar]
- [8].Gilliam ML, Davis SD, Neustadt AB, Levey EJ Contraceptive attitudes among inner-city African American female adolescents: barriers to effective hormonal contraceptive use. J Pediatr Adolesc Gynecol 2009;22(2):97–104. [DOI] [PubMed] [Google Scholar]
- [9].Guendelman S, Denny C, Mauldon J, Chetkovich C Perceptions of hormonal contraceptive safety and side effects among low-income Latina and non-Latina women. Matern Child Health J 2000;4(4): 233–239. [DOI] [PubMed] [Google Scholar]
- [10].Yee L, Simon M The role of the social network in contraceptive decision-making among young, African American and Latina women. J Adolesc Health 2010;47(4):374–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Sucato GS, Bhatt SK, Murray PJ, Ott MA Transdermal contraception as a model for adolescent use of new methods. J Adolesc Health 2011;49(4):357–362. [DOI] [PubMed] [Google Scholar]
- [12].Raine TR, Gard JC, Boyer CB, et al. Contraceptive decision-making in sexual relationships: young men’s experiences, attitudes and values. Cult Health Sex 2010;12(4):373–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Landry DJ, Camelo TM Young unmarried men and women discuss men’s role in contraceptive practice. Perspect Sex Reprod Health 1994;26(5):222–227. [Google Scholar]
- [14].Kaye K, Suellentrop K, Sloup C The fog zone: how misperceptions, magical thinking, and ambivalence put young adults at risk for unplanned pregnancy. Washington, DC: The National Campaign to Prevent Teen and Unplanned Pregnancy; 2009. [Google Scholar]
- [15].Kavanaugh ML, Jerman J Contraceptive method use in the United States: trends and characteristics between 2008, 2012 and 2014. Contraception 2018;97(1): 14–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Hubacher D, Kavanaugh M Historical record-setting trends in IUD use in the United States. Contraception 2018;98(6):467–470. [DOI] [PubMed] [Google Scholar]
- [17].Brown MK, Auerswald C, Eyre SL, Deardorff J, Dehlendorf C Identifying counseling needs of nulliparous adolescent intrauterine contraceptive users: a qualitative approach. J Adolesc Health 2013;52(3):293–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Hoopes AJ, Gilmore K, Cady J, Akers AY, Ahrens KR A qualitative study of factors that influence contraceptive choice among adolescent school-based health center patients. J Pediatr Adolesc Gynecol 2016;29(3):259–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Rogers EM The diffusion of innovation. 5th ed. New York: Free Press; 2003. [Google Scholar]
- [20].Valente TW, Rogers EM The origins and development of the diffusion of innovations paradigm as an example of scientific growth. J Sci Commun 1995;16(3):242–273. [DOI] [PubMed] [Google Scholar]
- [21].Dehlendorf C, Fitzpatrick J, Fox E, et al. Cluster randomized trial of a patient-centered contraceptive decision support tool, My Birth Control. Am J Obstet Gynecol 2019;220(6):565. e1–e12. [DOI] [PubMed] [Google Scholar]
- [22].Guttmacher Institute. National survey of reproductive and contraceptive knowledge. Survey of young adults 2009. (the fog zone). https://www.guttmacher.org/sites/default/files/dataset_documents/ns-questionnaire2009.pdf. Accessed 13 Oct 2019.
- [23].Cohen J Statistical power analysis for the behavioral sciences. Routledge; 2013. [Google Scholar]
- [24].Hawn C Take two aspirin and tweet me in the morning: how Twitter, Facebook, and other social media are reshaping health care. Health Aff (Millwood) 2009;28(2):361–368. [DOI] [PubMed] [Google Scholar]
- [25].Yang Q Are social networking sites making health behavior change interventions more effective? A meta-analytic review. J Health Commun 2017;22(3): 223–233. [DOI] [PubMed] [Google Scholar]
- [26].Lefebvre RC, Bornkessel AS Digital social networks and health. Circulation 2013;127(17):1829–1836. [DOI] [PubMed] [Google Scholar]
- [27].Myneni S, Fujimoto K, Cobb N, Cohen T Content-driven analysis of an online community for smoking cessation: integration of qualitative techniques, automated text analysis, and affiliation networks. Am J Public Health 2015;105(6):1206–1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Graham AL, Zhao K, Papandonatos GD, et al. A prospective examination of online social network dynamics and smoking cessation. PLoS ONE 2017;12(8):e0183655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Robbins R, Niederdeppe J How online peer-to-peer conversation shapes the effects of a message about healthy sleep. Prev Sci 2017;18(2):141–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Jawad A, Jawad I, Alwan N Interventions using social networking sites to promote contraception in women of reproductive age. Cochrane Database Syst Rev 2019;3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Dehlendorf C, Reed R, Fox E, Seidman D, Hall C, Steinauer J Ensuring our research reflects our values: the role of family planning research in advancing reproductive autonomy. Contraception 2018;98(1):4–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Gomez AM, Wapman M Under (implicit) pressure: young Black and Latina women’s perceptions of contraceptive care. Contraception 2017;96(4):221–226. [DOI] [PubMed] [Google Scholar]
- [33].Gomez AM, Fuentes L, Allina A Women or LARC first? Reproductive autonomy and the promotion of long-acting reversible contraceptive methods. Perspect Sex Reprod Health 2014;46(3): 171–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Mann ES, White AL, Rogers PL, Gomez AM Patients’ experiences with South Carolina’s immediate postpartum Long-acting reversible contraception Medicaid policy. Contraception 2019;100(2):165–171. [DOI] [PubMed] [Google Scholar]
- [35].Humes KR, Jones NA, Ramirez RR. Overview of race and Hispanic origin: 2010. US Census Bureau; 2011. [Google Scholar]