Dear Editor,
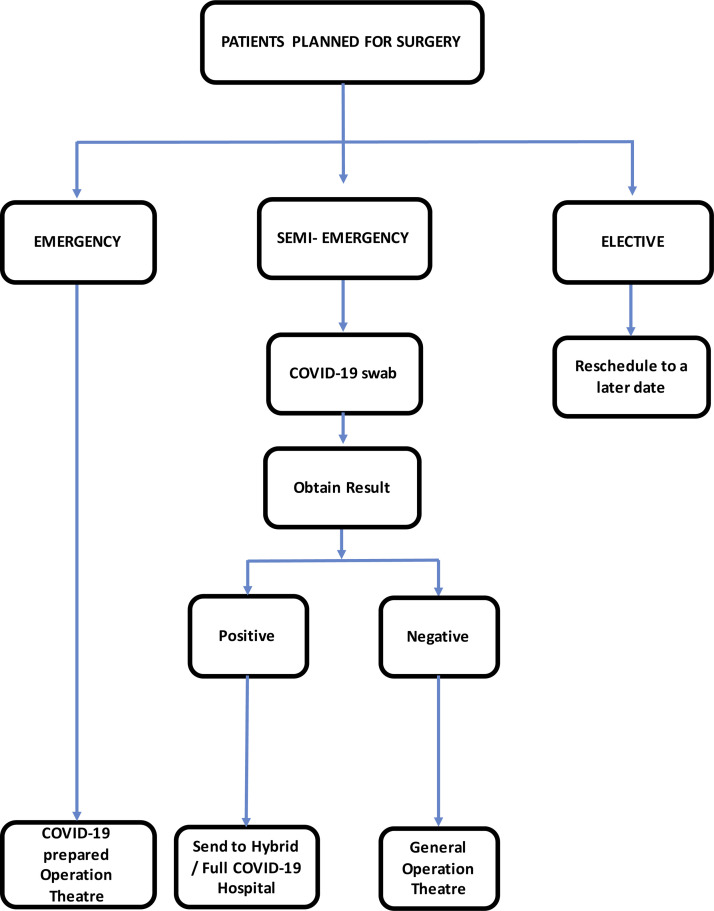
Since December 2019, the outbreak of coronavirus disease 2019 (COVID-19) has become a global public health threat [1]. On 28 February 2020, World Health Organisation (WHO) upgraded their assessment of the risk of spread and the risk of the impact of COVID-19 to very high. At the time of preparing this manuscript, the Malaysian Ministry of Health (MOH) reported 6353 confirmed cases and a total of 105 death cases in Malaysia [2]. Globally, the number of confirmed cases by the WHO has reached 3,435,894 in 212 countries [3]. The MOH had identified designated Covid-19 hospitals and prepared guidelines on the Management of Emergency Surgeries during the COVID-19 pandemic. 2 Hospitals were categorized into three groups; (1) Full COVID-19 hospitals, (2) Hybrid COVID-19 hospitals and (3) Non-COVID-19 hospitals. All COVID-19 burns were managed at Full COVID-19 or Hybrid COVID-19 hospitals. Non-burn COVID-19 patients were managed in Non-COVID-19 and Hybrid COVID-19 hospitals (Fig. 1 ).
Fig. 1.
Flow chart for burns surgery during COVID-19 pandemic.
During this unprecedented crisis, we implemented certain changes in the management of burns in Malaysia to ensure the health system would be able to handle the anticipated surge in demand for hospital beds and acute care facilities with the progress of the pandemic. All new burn patients presented to the hospital underwent mandatory screening using a standardized questionnaire (Table 1 ). If any of these questions were positive, the patients were referred to the Infectious Disease team for the COVID-19 risk assessment. Indications for the COVID-19 real-time reverse transcription polymerase chain reaction (rRT-PCR) test are as follows but not limited to, the following.
-
1
All burns patients requiring surgery.
-
2
All burns patients with an identified risk for COVID-19 from the questionnaire
-
3
All burns patients presenting with respiratory symptoms
Table 1.
Screening questionnaire for COVID-19.
| 1. Are you suffering from any fever or acute respiratory infection (sudden onset of respiratory infection with at least one of the following symptoms: shortness of breath, cough or sore throat)? |
| 2. Have you travelled to / resided in a foreign country within the last 14 days? |
| 3. Have you been in close contact with a person suspected or confirmed to have the COVID-19 infection? (close contact: having cared for, lived with, of had direct contact with the respiratory secretions or body fluids) |
| 4. Have you attended or have been in close contact with anyone who has attended gatherings or events associated with a known COVID-19 outbreak? |
| 5. Have you been in close contact with someone who is under the Home Quarantine Order or someone suspected of COVID-19 infection in the past 14 days? |
Management of burn patients were divided into three categories; 1. Emergency, 2. Semi-emergency, and 3. Elective. All elective procedures were rescheduled until the current situation improves. Emergency cases such as burns with compartment syndrome were performed in the COVID-19 prepared operating theatre with personal protective equipment (PPE) and enhanced airborne precaution. This group of patients was managed as COVID-19 positive until test results became available. Patients for semi-emergency surgery were subjected to COVID-19 rRT-PCR testing. Patients with positive results were transferred to a COVID-19 designated hospital (hybrid or full COVID hospital) with negative pressure transport and standard precautions. Patients with negative results were managed in the general operation theatre. Minor burns and uncomplicated wounds in stable patients were managed as an outpatient. Wherever possible, wound management in patients with minor burns was decentralized to the nearest primary health care facility to minimize exposure risk for both patients and health care workers. The usage of telemedicine for referrals and consultation was emphasized during this pandemic period. Consultations were conveyed immediately with accuracy from a primary or secondary health care facility to a covering Burn Unit. Patients received professional diagnosis and treatment without delay. Telemedicine also allowed the sharing of expert opinion and management protocols. Communication via this method avoids in-person interaction, which contributes to the prevention of disease transmission.
As a precaution, mitigation strategies were drawn up and implemented. The burns management team was divided into functional independent teams. Direct meetings between the teams were kept to a minimum and discussions held via video conferencing, ensuring the continuity of care if one team is exposed to the COVID-19 virus. All health care personnel involved in burns management were made to undergo compulsory training on the handling of PPE. This training and assessment were conducted by the hospital Occupational Health and Safety Department. Quality control of surgery and risk assessment of exposure to health care personnel were vital decision-making points. Only emergency and semi-emergency cases were performed during the outbreak period. The senior-most member of the team carried the burden of decision making and surgeries. Appropriate decision making with the best surgical option reduced operating time, operative complications, and improved outcome.
Implementation of these strategies has helped us to prevent COVID-19 infection among the doctors and nurses in our department. Up to now, we have zero confirmed cases of transmission of this disease to health care workers from treating COVID-19 positive patients nationwide [4]. This pandemic has drastically changed the way we handle burn patients. Emphasis on patient and health care workers' safety is the utmost priority. It is imperative that we learn from this experience and formulate guidelines that can be adhered to for future pandemics. As long as a vaccine is not available, we need to be constantly prepared for any surge in new cases. Adherence to the new norm is mandatory for us to succeed in this pandemic.
Acknowledgements
This short communication has obtained the permission to publish by the Director-General of Health, Ministry of Health, Malaysia.
References
- 1.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y. Early transmission dynamics in Wuhan, China, of novel coronavirus–In#Fected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ministry of Health Malaysia . Ministry of Health Malaysia; Putrajaya: 2020. Guidelines COVID-19 management in malaysia No. 5/2020 (updated on 25 March 2020)http://www.moh.gov.my/index.php/pages/view/2019-ncov-wuhan-guidelines Available from: [Google Scholar]
- 3.World Health Organization. 2020. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200504-covid-19-sitrep-105.pdf?sfvrsn=4cdda8af_2.
- 4.Ministry of Health Malaysia . Ministry of Health Malaysia; 2020. Press conference by Datuk Dr Noor Hisham Abdullah, director general of health.http://www.moh.gov.my/index.php/pages/view/2274 Available from: [Google Scholar]