Abstract
Myxoglobulosis is a rare histologic variant of mucocele that is characterized by transformation of mucin into eosinophilic globules. The globules frequently demonstrate a lamellar pattern and are surrounded by an inflammatory cell infiltrate. Myxoglobulosis has not yet been described in laryngeal mucosa. A 62 year old man presented for a check-up with hoarseness of 2 months duration. He was a current smoker and reported a 40 year habit. An asymmetrical swelling along the length of both vocal cords was consistent with a clinical diagnosis of Reinke’s edema. The histopathologic examination demonstrated bilateral pseudocyst formation within Reinke’s space. Extravasated mucin was present in the form of eosinophilic globules that filled the left Reinke’s space almost entirely and were also seen on the right side. The pseudocyst, mucinous globules, and accompanying inflammatory cells were characteristic of myxoglobulosis. The sequelae of nicotine abuse, including inflammation, increased mucous secretion, and a rasping cough, are considered to be the main etiological factors of laryngeal myxoglobulosis. The patient had no evidence of voice disorder at 18 month follow-up. This case report contributes to the recognition of an exceptionally rare histologic variant of laryngeal mucocele.
Keywords: Vocal cords, Hoarseness, Mucocele, Myxoglobulosis
Introduction
Oral mucoceles and salivary duct cysts (SDCs) are two common reactive lesions of the head and neck. Mucous extravasation phenomenon, another term for oral mucoceles, describes the inflammatory reaction to mucin spillage that usually results from a traumatized salivary duct [1]. In the head and neck, they occur in the oral cavity, paranasal sinuses, and lacrimal gland. Clinically, oral lesions present as painless, bluish swellings, and measure from 0.1 to 2 cm in diameter [4]. Mucous accumulation within the lumen of single organs, such as the appendix or gallbladder, is also termed a mucocele [3, 4].
Whereas mucoceles commonly affect the minor glands of the oral cavity, SDCs typically form in ducts of major salivary glands as a result of mucin accumulation due to distal obstruction [2–5]. The clinical differential diagnosis of mucoceles and SDCs is broad and may include lipoma, hemangioma, lymphangioma, benign or malignant salivary gland neoplasms, venous varix, lymphoepithelial cyst, soft tissue abscess, and pyogenic granuloma [2, 6, 7].
A rare histologic variant of mucocele, myxoglobulosis comprises 4–31% of all oral cavity mucoceles [5, 8–11]. Histologically, myxoglobulosis shows extravasation of mucin with characteristic eosinophilic globules. The globules have a lamellar structure, range in size from 88 to 416 µm in diameter, and are characteristically surrounded by an inflammatory cell infiltrate [5].To the best our knowledge, this case is the first report of laryngeal myxoglobulosis.
Case Report
A 62-year old male presented with a 2 month history of hoarseness without breathing difficulty. His past medical history was negative for surgical procedures in general anaesthesia, phono trauma, vocal load, or unfavourable microclimate at the work place. He provided a history of smoking 20 cigarettes per day for 40 years.
Indirect laryngoscopy showed asymmetrical edematous swelling along the lengths of both vocal cords consistent with a clinical diagnosis of Reinke’s edema. The patient underwent suspension microlaryngoscopy which showed pale, asymmetrically swollen vocal cords and narrowing of the airway. A biopsy of the mucosa of each vocal cord was taken and the greyish-white content of the left Reinke’s space was enucleated. Subsequently, the mucosa of both vocal cords was re-approximated.
Histologic examination of specimens from both vocal cords revealed focally atrophic and hyperplastic areas within the squamous epithelium. A low-grade squamous intraepithelial lesion was also identified. The subepithelial tissue was edematous with irregularly dispersed globules of mucin showing vaguely lamellar patterns. Globules of different diameters were surrounded or admixed with fibroblasts and scarce inflammatory cells. Minor salivary ducts or glands were not detected within the tissue specimens. The greyish-white content from the left Reinke’s space consisted entirely of narrowly packed globules, some lamellated, that ranged in size. Similarly, scare fibrous and inflammatory cells were present (Fig. 1a, b). The mucinous globules were highlighted with colloid iron staining (Fig. 2).
Fig. 1.
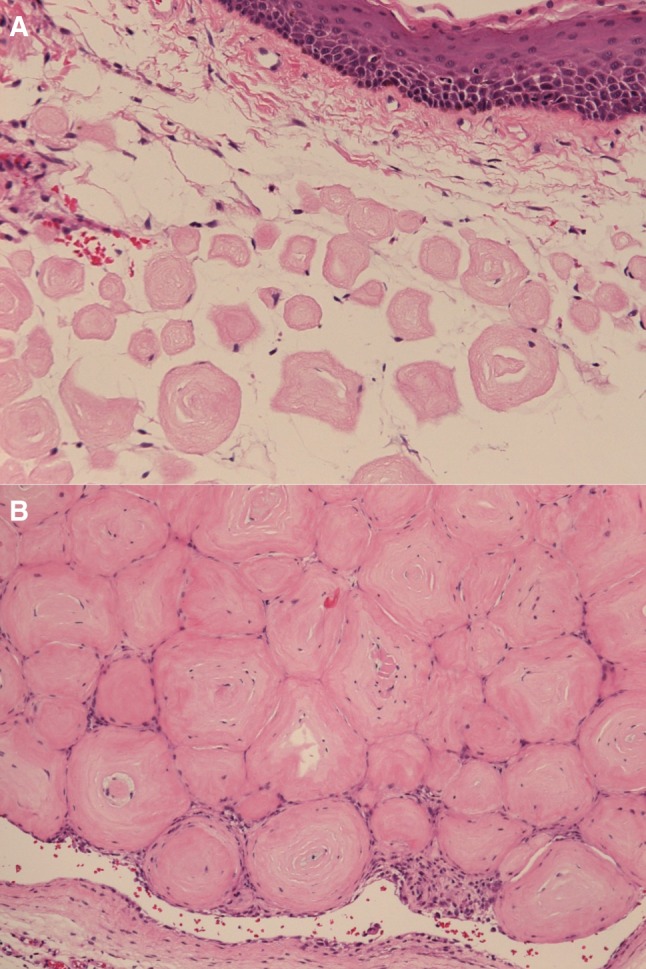
Myxoglobulosis of the vocal cord. a Biopsy from the right vocal cord. Pink globules of varying sized are dispersed within the edematous lamina propria. b Biopsy from the left vocal cord. Reinke’s space was filled with closely packed eosinophilic globules, some of which show lamellar internal structure
Fig. 2.
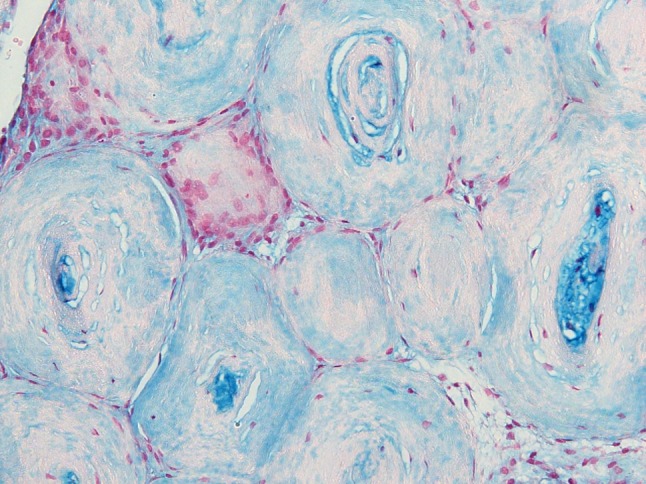
Colloid iron staining shows abundant mucin within the globules
After the surgery, the patient was followed for 18 months. The first visit was 1 month after the surgery, followed by visits at 8, 12, and 18 months. At every visit, the patient assessed his voice as normal and did not report any deterioration of voice quality. There were no residual or new swellings or mucosal changes of the vocal cords. The videostroboscopic examination showed complete glottal closure and symmetric vibration of the vocal cords. The stroboscopic findings did not deteriorate during the observed period.
Discussion
Mucocele, also known as mucous extravasation phenomenon, is a frequent reactive lesion of minor salivary glands in the head and neck region, especially the oral cavity [1, 4, 9, 11]. Li et al. first reported a histologic variant of a lower lip mucocele called myxoglobulosis. They described globular structures that lack epithelial tissue and contain eosinophilic, lamellated, amorphous, or fibrillary material [12]. Accounts of oral myxoglobulosis were confirmed in further publications [3–5, 9, 10]. The reported frequency varies from 2.9–31% of oral mucoceles [4, 9, 11]. To the best of our knowledge, this is the first report of laryngeal myxoglobulosis.
The etiopathogenesis of laryngeal myxoglobulosis is unknown; however, we theorize it is related to morphologic specificities of Reinke’s space, excess production of mucin, and coughing. Reinke’s space of the vocal cords lies between the vocal ligament and squamous epithelium. As it contains few capillaries or lymphatics, poor lymphatic drainage may contribute to the collection of edematous and mucinous fluid. Contrary to the supraglottis, the number of seromucinous glands is low in the glottic region [13]. While this does not favour mucocele development, a long history of heavy smoking is known to cause hypersecrection of mucous [14]. Additionally, increased muscular activity during phonation or coughing can cause damage to rare ducts of small salivary glands and extravasation of mucin. In a study of patients with hyperkinetic voice patterns, 65% had epidermoid cysts and 35% retention cysts of the vocal cords [15].
The globules characteristic of myxoglobulosis raise questions regarding the variations of mucin quality or inflammatory microenvironment that contribute to their formation. In mucoceles of the lower lip, a pseudocyst comprising extravasated mucinous material, muciphages, neutrophilic leucocytes, and surrounding granulation tissue will form within a few days after ductal damage. Ide et al. theorized that granulation tissue projections from the pseudocystic wall detach into the lumen and degenerate to form the globules of myxoglobulosis [16]. Other authors speculate the amount of extravasated mucin exceeds the phagocytic capacity of macrophages and the remainder forms into the globules [9]. A histologically similar lesion of the lower lip was described as a collagenous spherulosis in an oral mucosa cyst by Henry et al. [17]. They proposed that collagen deposition, possibly produced by myoepithelial cells of salivary gland, formed in rounded eosinophilic globules under special circumstances.
Conclusion
Myxoglobulosis is a rare histologic variant of mucocele. In the head and neck, it is most frequent in the oral mucosa. This case demonstrates this entity can occur also in the mucosa of the vocal cords and may resemble Reinke’s edema clinically. Due to the exceptional rarity and unusual histologic features, we believe that myxoglobulosis deserves to be recognised as a special variant of oral and laryngeal mucoceles.
Acknowledgements
The first author would like to express her gratitude to Professor Irena Hočevar Boltežar for her support and expertise during follow-up of patient and in preparation of manuscript.
Funding
None.
Compliance with ethical standards
Conflict of interest
All the authors declared that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bezerra TM, Monteiro BV, Henriques ÁC, de Vasconcelos Carvalho M, Nonaka CF, da Costa Miguel MC. Epidemiological survey of mucus extravasation phenomenon at an oral pathology referral center during a 43 year period. Braz J Otorhinolaryngol. 2016;82(5):536–542. doi: 10.1016/j.bjorl.2015.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stojanov IJ, Malik UA, Woo SB. Intraoral salivary duct cyst: clinical and histopathologic features of 177 cases. Head Neck Pathol. 2017;11:469–476. doi: 10.1007/s12105-017-0810-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schulman JM, Jordan RC. Oral mucus extravasation phenomenon with myxoglobulosis. J Cutan Pathol. 2014;41(10):767–770. doi: 10.1111/cup.12392. [DOI] [PubMed] [Google Scholar]
- 4.de Brito Monteiro BV, Bezerra TM, da Silveira ÉJ, Nonaka CF, da Costa Miguel MC. Histopathological review of 667 cases of oral mucoceles with emphasis on uncommon histopathological variations. Ann Diagn Pathol. 2016;21:44–46. doi: 10.1016/j.anndiagpath.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 5.Paremala K, Radhika MB, Thambiah LJ. Myxoglobulosis of lower lip: Report of two cases. J Oral Maxillofac Pathol. 2011;15(2):232–235. doi: 10.4103/0973-029X.84512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.More CB, Bhavsar K, Varma S, Tailor M. Oral mucocele: a clinical and histopathological study. J Oral Maxillofac Pathol. 2014;18(Suppl 1):S72–S77. doi: 10.4103/0973-029X.141370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thompson LD. Mucocele: retention and extravasation types. Ear Nose Throat J. 2013;92(3):106–108. doi: 10.1177/014556131309200307. [DOI] [PubMed] [Google Scholar]
- 8.Probstein JG, Lasar GN. Mucocele of the appendix with mixoglobulosis. Ann Surg. 1948;127:171–176. doi: 10.1097/00000658-194801000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Conceição JG, Gurgel CA, Ramos EA, De Aquino Xavier FC, Schlaepfer-Sales CB, Cangussu MC, et al. Oral mucoceles: a clinical, histopathological and immunohistochemical study. Acta Histochem. 2014;116(1):40–47. doi: 10.1016/j.acthis.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 10.Chi AC, Lambert PR, 3rd, Richardson MS, Neville BW. Oral mucoceles: a clinicopathologic review of 1,824 cases, including unusual variants. J Oral Maxillofac Surg. 2011;69(4):1086–1093. doi: 10.1016/j.joms.2010.02.052. [DOI] [PubMed] [Google Scholar]
- 11.Shah KA. Myxoglobulosis in oral extravasation mucocele: an entity? Histopathology. 2002;43:291–296. doi: 10.1046/j.1365-2559.2003.01688.x. [DOI] [PubMed] [Google Scholar]
- 12.Li TJ, Kitano M, Yoshida A, Iwashige Y, Yamashita S. Myxoglobulosis in an extravasation mucocele of the lower lip. J Oral Pathol Med. 1997;26(7):342–344. doi: 10.1111/j.1600-0714.1997.tb00227.x. [DOI] [PubMed] [Google Scholar]
- 13.Milles SE. Larynx and pharynx. In: Milles SE, editor. Histology for pathologists. 4. Philadelphia: Wolters Kluwer; 2012. pp. 461–475. [Google Scholar]
- 14.Yu H, Li Q, Kolosov VP, Perelman JM, Zhou X. Regulation of cigarette smoke-induced mucin expression by neuregulin1β/ErbB3 signalling in human airway epithelial cells. Basic Clin Pharmacol Toxicol. 2011;109(1):63–72. doi: 10.1111/j.1742-7843.2011.00686.x. [DOI] [PubMed] [Google Scholar]
- 15.Milutinović Z, Vasiljević J. Contribution to the understanding of the etiology of vocal fold cysts: a functional and histologic study. Laryngoscope. 1992;102(5):568–571. doi: 10.1288/00005537-199205000-00017. [DOI] [PubMed] [Google Scholar]
- 16.Ide F, Kikuchi K, Kusama K. Is papillary synovial metaplasia-like change a hitherto undescribed histologic pattern of lip mucoceles? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(6):800–801. doi: 10.1016/j.tripleo.2010.01.035. [DOI] [PubMed] [Google Scholar]
- 17.Henry CR, Nace M, Helm KF. Collagenous spherulosis in an oral mucous cyst. J Cutan Pathol. 2008;35(4):428–430. doi: 10.1111/j.1600-0560.2007.00824.x. [DOI] [PubMed] [Google Scholar]


