Abstract
Central giant cell granuloma (CGCG) is a benign intraosseous lesion of the head and neck with potential for aggressive and locally destructive behaviour. Lesions of the maxilla tend to expand more than those of the mandible due to the thinner cortices and spongy tissue of this location. Surgical removal is the most common treatment; however, it may be disfiguring in aggressive cases, especially for lesions located in the maxilla. Alternative treatments, such as intralesional corticosteroid injections, have been performed with satisfactory results. We report a case of a 12-year-old female patient with a CGCG of the left maxilla that was treated with 40 doses of intralesional triamcinolone acetonide infiltrations combined with alendronate sodium and calcium carbonate. Clinical and imaging follow-up over 12 years demonstrates improvement in the patient’s condition.
Keywords: Corticosteroid, Granuloma, Giant cell, Injections, Intralesional, Triamcinolone acetonide
Introduction
Central giant cell granuloma (CGCG) is a rare, benign, intraosseous lesion of the head and neck region that has potential for aggressive and locally destructive behaviour [1, 2]. It typically presents as a painless, slow-growing lesion that may expand into surrounding tissues [3]. Due to the thinner cortical bone and spongy tissue of the maxilla, CGCGs in this location tend to expand more than lesions of the mandible [4]. Although the aetiology is known to be related to genetics and post-traumatic reparative processes, it is not clearly defined [2].
Radiographically, CGCGs appear as unilocular or multilocular radiolucent defects with well-defined margins and varying degrees of cortical expansion [1]. If small, they may resemble periapical granulomas or cysts. If large and multilocular, ameloblastoma and other multilocular entities share overlapping features. In addition, root resorption may also be observed [5].
Surgical removal is the most common treatment and can range from simple curettage to en bloc resection [3]. In aggressive cases, characterised by rapid progression and local invasion, surgical treatment may be disfiguring, especially for lesions located in the maxilla. Alternative treatment with intralesional corticosteroid injections has been performed with satisfactory results. These are used as definitive or pre-surgical treatments, aimed at reducing morbidity [6–8].
The present study reports a case of a young female patient with a CGCG of the left maxilla who was treated with intralesional infiltrations of triamcinolone combined with alendronate sodium and calcium carbonate and followed for a period of 12 years.
Clinical, Radiographic, and Histologic Findings
A 12-year-old female patient was referred for evaluation for a facial asymmetry and palatine and vestibular swelling. Intraoral examination revealed the swelling had a soft consistency and was covered by healthy-appearing gingiva and mucosa (Figs. 1, 2). A diagnosis of CGCG was considered. The patient was sent for additional tests to rule out other pathologies that present with similar features.
Fig. 1.

Extraoral photograph at the beginning of treatment
Fig. 2.

Intraoral photograph at the beginning of treatment
Radiographic and cone-bean computed tomography (CBCT) examinations revealed a unilocular radiolucent lesion of the left maxilla. The borders were well-defined and teeth 12 and 13 were involved (Figs. 3, 4).
Fig. 3.
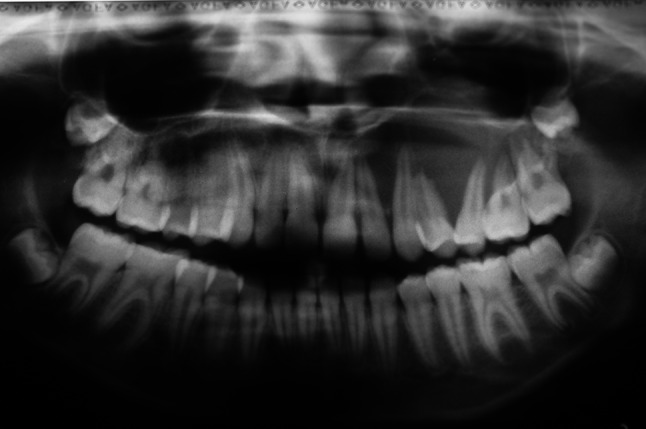
Pre-treatment panoramic radiograph
Fig. 4.
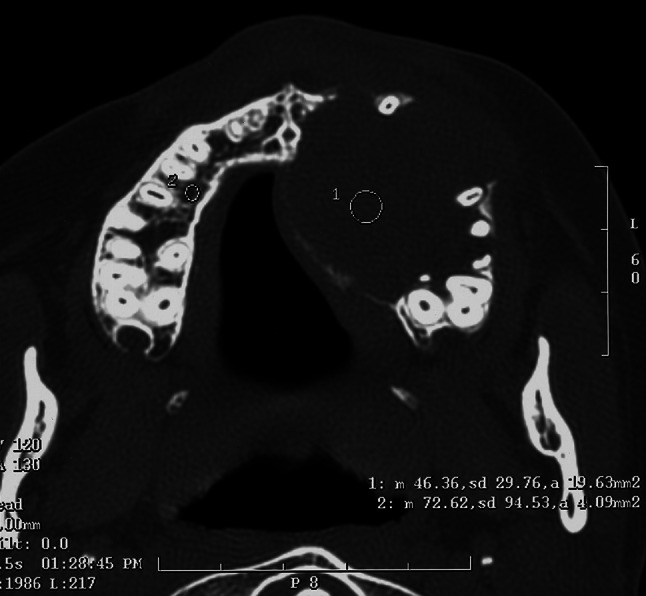
Pre-treatment axial image from the computed tomography scan
Histopathologic examination revealed multinucleated giant cells surrounded by abundant connective tissue (Fig. 5a, b). Hemosiderin pigment and areas of haemorrhage were observed (Fig. 5b).
Fig. 5.
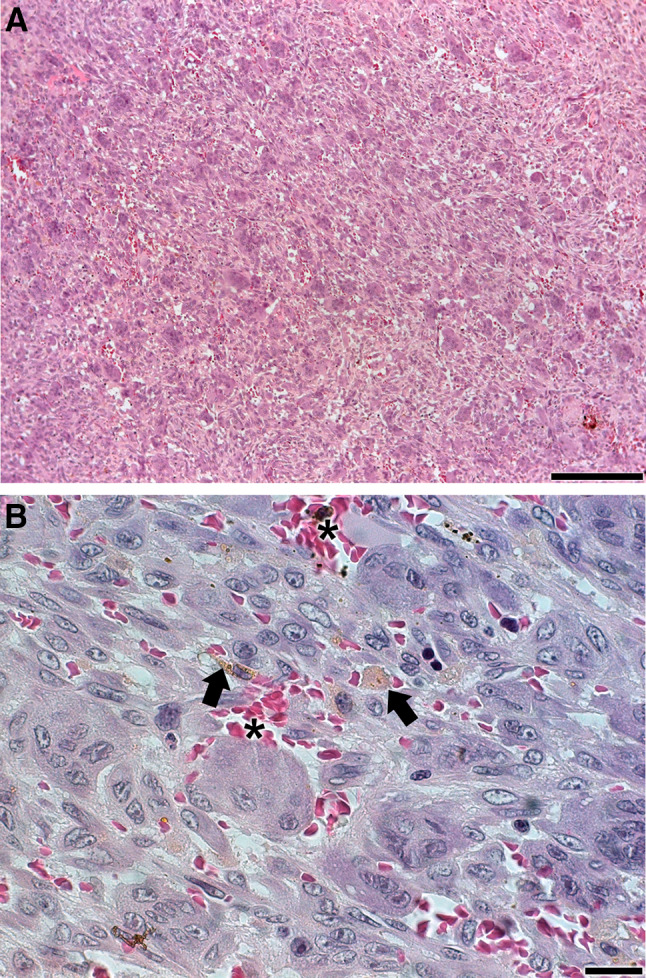
a, b Incisional biopsy shows characteristic histopathologic features of central giant cell granuloma. Multinucleated giant cells are separated by interstitial fibrous connective tissue bands. Hemosiderin pigment (arrows) and areas of haemorrhage (asterisks) were present (stained with H&E). Scale bars: a, 200 µm and b, 20 µm
As CGCGs have a similar microscopic presentation to Brown tumours associated with hyperparathyroidism, the patient underwent tests to determine her serum ionised calcium (normal range 1.12–1.32 mEq/L), alkaline phosphatase (normal range 5.8–11.6 ug/L) and parathyroid hormone (normal range 12–72 pg/mL) levels and was found to have values of 1.39 mEq/L, 407.5 ug/L and 59.7 pg/mL, respectively. The change in alkaline phosphatase concentration indicated an increase in osteoblastic activity promoted by the lesion. Thus, these findings excluded a diagnosis of hyperparathyroidism.
Scintigraphy was requested to rule out the hypothesis of a giant cell tumour which affect the long bones of the body, including the femur and tibia. The examination revealed only the bone lesion only in the left maxillary region. It displayed osteoblastic characteristics interspersed with osteolytic areas and/or necrosis. There was no scintigraphic evidence of bone lesions in other regions of the skeleton, ruling out a giant cell tumour.
Diagnosis
The clinical, radiographic, and histologic features together supported the diagnosis of central giant cell granuloma.
Treatment
The initial treatment considered was complete enucleation of the lesion. This would likely require the removal of all involved teeth. As an alternative, corticosteroid infiltration injections were chosen for the patient.
The infiltrations began on March 8, 2006 at the site of the vestibular mucosa. Each infiltration consisted of 2 mL of triamcinolone actinide (20 mg/mL) combined with 3.6 mL of 2% mepivacaine with epinephrine at a ratio of 1:200,000. The total dose of triamcinolone acetonide was 40 mg for each infiltration. After 14 sessions, there was an improvement in the patient’s condition as indicated by a firmer consistency of the vestibular region on palpation. With this success, infiltration via a palatal approach was then performed. After five more sessions, there was resistance to penetration of the needle in the vestibular region and infiltration was only possible in by palatal approach. At this point, the patient began taking antiresorptive medication (70 mg of alendronate sodium) and calcium carbonate once a week. This medication was continued for three and a half years. No episodes of infection occurred during or after treatment.
After 2 years, infiltration with 3% mepivacaine commenced because the patient reported tachycardia attributed to the epinephrine. The dosage was 2 mL of triamcinolone acetonide (20 mg/mL) with 3.6 mL of 3% mepivacaine.
The treatment was carried out from 2006 to 2012 with a total of 40 doses of corticosteroid. Radiographically, there was a reduction in size of the lesion as well as a change from an osteolytic calcification pattern to normal radiopacity. Some areas showed bony sclerosis. The patient is currently undergoing clinical and imaging follow-up and shows continued improvement. No functional or aesthetic impairment was experienced (Figs. 6, 7, 8, 9).
Fig. 6.

Extraoral photograph at follow-up
Fig. 7.

Intraoral photograph at follow-up
Fig. 8.

Panoramic radiograph at follow-up
Fig. 9.
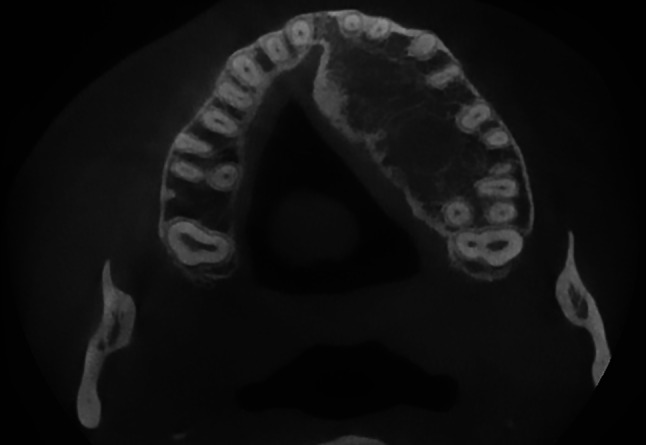
Axial image from the computed tomography scan at 12 year follow-up
Discussion
Although benign, CGCG can be aggressive and locally destructive. When located in the maxilla, it can expand into surrounding tissues, as was observed in the present case [1–3]. To provide a better prognosis and avoid surgery, a therapeutic alternative based on intralesional corticosteroids, as previously reported in the literature, was the treatment of choice for this patient.
In a case sharing a maxillary location in a female patient of a similar age, Wendt et al. treated with intralesional injections of triamcinolone acetonide for a period of 11 weeks [9]. After 6 years of follow-up, the clinical and radiographic findings demonstrated success of this treatment for their patient.
Osterne et al. performed a meta-analysis with studies that treated CGCG with intralesional infiltrations of corticosteroids [6]. Based on favourable results for 41 evaluated patients, these authors suggested that this treatment should be considered a first choice for CGCG. Other authors report similar findings of complete remission without evidence of recurrence for CGCGs treated with intralesional infiltration of triamcinolone [7, 10]. Based on these collective outcomes, it may be concluded that the administration of intralesional corticosteroid injections are an effective alternative treatment for CGCG, especially in children.
Intralesional corticosteroid infiltration may be used alone or in combination with other treatments such as bisphosphonates, calcitonin, denosumab, or surgery [11, 12]. An immunohistochemical study provided persuasive evidence that CGCG of the jawbones is positive for glucocorticoid and/or calcitonin receptors [13]. This finding supports the therapeutic use of intralesional steroids and calcitonin in aggressive cases. Naidu et al. successfully treated a CGCG patient with intralesional injections of triamcinolone and denosumab [12]. Bisphosphonates and denosumab have similar antiresorptive effects. Bisphosphonates, such as alendronate, are known to prevent or restore bone loss caused by glucocorticoids by inhibiting osteoclast-mediated bone resorption [14–16].
Our research group performed a combined treatment with triamcinolone acetonide and alendronate sodium for another CGCG patient with similarly a favourable outcome [17]. After 2 years of treatment, the bony architecture was near normal and only minimal radiolucency was present around the root apices of the involved teeth. Both the cortical and the drilling areas were treated. The patient has been followed up for 11 years without relapses or sequelae.
The advantages of choosing intralesional corticosteroids instead of surgical removal include a lower cost, avoidance of compromising vital structures, and the possibility to combine this treatment with surgery, if necessary, after regression of the lesion [18]. Nevertheless, the use of intralesional corticosteroids in combination with bisphosphonates also carries risks. The most notable of these is the development of medication-related osteonecrosis of the jaw after dentoalveolar surgery [19].
Sarinho and Melo highlighted that children or adolescents who require corticosteroid therapy should also be provided care and guidance related to bone health and calcium intake [20]. The combination of alendronate and calcium is used to treat osteoporosis induced by corticosteroids [16]. Rudge et al. concluded that once-weekly oral alendronate is well tolerated, effective at suppressing bone resorption, and may improve volumetric bone density in children with chronic illness taking glucocorticoids [21]. Importantly, it does not affect bone growth [21]. The effects of bisphosphonates on bone remodelling, however, may interfere with dental exfoliation and eruption processes and cause eruption delay [22].
In the present case, the corticosteroid treatment was provided in association with alendronate sodium and calcium carbonate to promote bone formation and achieve a better prognosis. There was no alteration in the bone growth process or of dental eruption.
Maintenance dosages are not needed at this point for lesional control. Reports of CGCG treatments with corticosteroid infiltration in the literature are of shorter duration and generally long-term control is achieved [23].
To date, there is no delineation of the lesion identified to fully verify complete resolution of this case. A surgical procedure, if made, would be restricted to osteoplasty in the palatal process of the maxilla. An incisional biopsy to verify the presence of characteristic giant cells was considered; however, this procedure is being postponed because of the risk of osteonecrosis [19]. While osteonecrosis is more common in the mandible, the time of use (3½ years) and concomitant use of corticosteroids raise the risk for our patient. Currently, she does not show interest in performing this procedure and instead prefers periodic monitoring with CT scans.
This case highlights the possibility of not submitting a young patient, in this case 12 years old, to an extensive surgery that would involve the entire left hemi-maxilla region. Although there is still a palatal mass, the vestibular and extraoral view of the patient no longer shows increased volume. Bone formation by intralesional corticosteroid applications is an important outcome of the treatment to date, as the entire extension of the lesion was initially reabsorbed. Considering the aforementioned factors, the conservative treatment used in this case was sufficient to achieve significant bone formation while avoiding compromise to maxillofacial function and aesthetics.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
7/14/2021
A Correction to this paper has been published: 10.1007/s12105-021-01357-x
Contributor Information
Raíssa Pinheiro de Mendonça, Email: raissa.rpm@hotmail.com.
Geovanni Pereira Mitre, Email: geovannimitre@gmail.com.
Flavio Henrique Real, Email: flavio.real@hotmail.com.
Maria Sueli da Silva Kataoka, Email: sukataoka@yahoo.com.br.
Sérgio de Melo Alves Júnior, Email: sergiomalves@gmail.com.
Newton Guerreiro Da Silva Júnior, Email: ngsj47@gmail.com.
João de Jesus Viana Pinheiro, Email: radface@hotmail.com, Email: joaopinheiro@ufpa.br.
References
- 1.El-Naggar AK, Chan JKC, Grandis JR, Takata T, Slootweg PJ, editors. World Health Organization classification of head and neck tumours. Lyon: IARC Press; 2017. p. 256. [Google Scholar]
- 2.Garg P, Jain J, De N, Chatterjee K. A central giant cell granuloma in posterior part of maxilla: a case report. Int J Surg Case Rep. 2017;30:222–225. doi: 10.1016/j.ijscr.2016.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jerkins D, Malotky M, Miremadi R, Dole M. Central giant cell granuloma of the mandible requiring multiple treatment modalities: a case report. J Oral Maxillofac Surg. 2016;74(8):1596–1607. doi: 10.1016/j.joms.2016.02.019. [DOI] [PubMed] [Google Scholar]
- 4.Rawashdeh MA, Bataineh AB, Al-Khateeb T. Long-term clinical and radiological outcomes of surgical management of central giant cell granuloma of the maxilla. Int J Oral Maxillofac Surg. 2006;35(1):60–66. doi: 10.1016/j.ijom.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 5.de Lange J, van den Akker HP. Clinical and radiological features of central giant-cell lesions of the jaw. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:464–470. doi: 10.1016/j.tripleo.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 6.Osterne RL, Araújo PM, de Souza-Carvalho AC, Cavalcante RB, Sant’Ana E, Nongueira RL. Intralesional corticosteroid injections in the treatment of central giant cell lesions of the jaws: a meta-analytic study. Med Oral Patol Oral Cir Bucal. 2013;18(2):e226–e232. doi: 10.4317/medoral.18345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dolanmaz D, Esen A, Mihmanlı A, Işık K. Management of central giant cell granuloma of the jaws with intralesional steroid injection and review of the literature. Oral Maxillofac Surg. 2016;20(2):203–209. doi: 10.1007/s10006-015-0530-5. [DOI] [PubMed] [Google Scholar]
- 8.de Oliveira JP, Olivete F, de Oliveira ND, et al. Combination therapies for the treatment of recurrent central giant cell lesion in the maxilla: a case report. J Med Case Rep. 2017;11(1):74. doi: 10.1186/s13256-016-1173-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wendt FP, Torriani MA, Gomes AP, de Araujo LM, Torriani DD. Intralesional corticosteroid injection for central giant cell granuloma: an alternative treatment for children. J Dent Child. 2009;76(3):229–232. [PubMed] [Google Scholar]
- 10.da Rosa MRP, de Sá JL, Martins VB, de Oliveira MV. Central giant cells lesion: report of a conservative management. Eur J Dent. 2018;12(2):305–310. doi: 10.4103/ejd.ejd_402_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schreuder WH, van den Berg H, Westermann AM, Peacock ZS, de Lange J. Pharmacological and surgical therapy for the central giant cell granuloma: a long-term retrospective cohort study. J Craniomaxillofac Surg. 2017;45(2):232–243. doi: 10.1016/j.jcms.2016.11.011. [DOI] [PubMed] [Google Scholar]
- 12.Naidu A, Malmquist MP, Denham CA, Schow SR. Management of central giant cell granuloma with subcutaneous denosumab therapy. J Oral Maxillofac Surg. 2014;72(12):2469–2484. doi: 10.1016/j.joms.2014.06.456. [DOI] [PubMed] [Google Scholar]
- 13.Vered M, Buchner A, Dayan D. Immunohistochemical expression of glucocorticoid and calcitonin receptors as a tool for selecting therapeutic approach in central giant cell granuloma of the jawbones. Int J Oral Maxillofac Surg. 2006;35(8):756–760. doi: 10.1016/j.ijom.2006.02.014. [DOI] [PubMed] [Google Scholar]
- 14.Ananchenko G, Novakovic J, Tikhomirova A. Alendronate sodium. Profiles Drug Subst Excip Relat Methodol. 2013;38:1–33. doi: 10.1016/B978-0-12-407691-4.00001-0. [DOI] [PubMed] [Google Scholar]
- 15.Sambrook PN, Kotowicz M, Nash P, et al. Prevention and treatment of glucocorticoid-induced osteoporosis: a comparison of calcitriol, vitamin D plus calcium, and alendronate plus calcium. J Bone Miner Res. 2003;18(5):919–924. doi: 10.1359/jbmr.2003.18.5.919. [DOI] [PubMed] [Google Scholar]
- 16.Papapoulos SE. The role of bisphosphonates in the prevention and treatment of osteoporosis. Am J Med. 1993;95(5A):48S–52S. doi: 10.1016/0002-9343(93)90383-Z. [DOI] [PubMed] [Google Scholar]
- 17.da Silva NG, Carreira AS, Pedreira EN, Tuji FM, Ortega KL, de Jesus Viana Pinheiro J. Treatment of central giant cell lesions using bisphosphonates with intralesional corticosteroid injections. Head Face Med. 2012;8:23. doi: 10.1186/1746-160X-8-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kurtz M, Mesa M, Alberto P. Treatment of a central giant cell lesion of the mandible with intralesional glucocorticosteroids. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:636–637. doi: 10.1067/moe.2001.115721. [DOI] [PubMed] [Google Scholar]
- 19.Ruggiero SL, Dodson TB, Fantasia J, et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw: 2014 update. J Oral Maxillofac Surg. 2014;72(10):1938–1956. doi: 10.1016/j.joms.2014.04.031. [DOI] [PubMed] [Google Scholar]
- 20.Sarinho ESC, Melo VMPP. Glucocorticoid-induced bone disease: mechanisms and importance in pediatric practice. Rev Paul Pediatr. 2017;35(2):207–215. doi: 10.1590/1984-0462;2017/;35;2;00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rudge S, Hailwood S, Horne A, Lucas J, Wu F, Cundy T. Effects of once-weekly oral alendronate on bone in children on glucocorticoid treatment. Rheumatology. 2005;44(6):813–818. doi: 10.1093/rheumatology/keh538. [DOI] [PubMed] [Google Scholar]
- 22.Hernandez M, Phulpin B, Mansuy L, Droz D. Use of new targeted cancer therapies in children: effects on dental development and risk of jaw osteonecrosis: a review. J Oral Pathol Med. 2017;46(5):321–326. doi: 10.1111/jop.12516. [DOI] [PubMed] [Google Scholar]
- 23.Nogueira RL, Teixeira RC, Cavalcante RB, Ribeiro RA, Rabenhosrt SH. Intralesional injection of triamcinolone hexacetonide as an alternative treatment for central giant-cell granuloma in 21 cases. Int J Oral Maxillofac Surg. 2010;39(12):1204–1210. doi: 10.1016/j.ijom.2010.06.015. [DOI] [PubMed] [Google Scholar]


