Abstract
Italy is one of the major COVID‐19 hotspots. To reduce the spread of the infections and the pressure on Italian healthcare systems, since March 10, 2020, Italy has been under a total lockdown, forcing people into home confinement. Here we present data from 1,310 people living in the Italian territory (M age = 23.91 ± 3.60 years, 880 females, 501 workers, 809 university students), who completed an online survey from March 24 to March 28, 2020. In the survey, we asked participants to think about their use of digital media before going to bed, their sleep pattern and their subjective experience of time in the previous week (March 17–23, which was the second week of the lockdown) and up to the first week of February (February 3–10, before any restriction in any Italian area). During the lockdown, people increased the usage of digital media near bedtime, but this change did not affect sleep habits. Nevertheless, during home confinement, sleep timing markedly changed, with people going to bed and waking up later, and spending more time in bed, but, paradoxically, also reporting a lower sleep quality. The increase in sleep difficulties was stronger for people with a higher level of depression, anxiety and stress symptomatology, and associated with the feeling of elongation of time. Considering that the lockdown is likely to continue for weeks, research data are urgently needed to support decision making, to build public awareness and to provide timely and supportive psychosocial interventions.
Keywords: bedtime, circadian rhythms, depression, home confinement, social isolation, time perception
1. INTRODUCTION
By March 9, 2020, more than 8,342 people in Italy had officially contracted COVID‐19 (Istituto Superiore di Sanità, 2020). To address this critical situation and to reduce the spread of the infections, the Italian Prime Minister Giuseppe Conte signed a series of decrees that imposed restrictions on the movement of individuals in the entire national territory from March 10 until May 3 (but these measures are likely to be extended). People are allowed to leave their homes for limited and documented purposes (e.g., shopping for basic necessities and to go to work [if this cannot be done from home]). Several activities have been temporarily closed, including schools, universities and shops selling non‐essential goods.
Although these measures and efforts are necessary for reducing pressure on Italian healthcare systems, there are reasons to be concerned because prolonged home confinement during a disease outbreak may affect people's physical and mental health (Wang et al., 2020; World Health Organization, 2020). Home confinement can reduce the level of physical activity and the exposure to daylight, and increase the level of stress due to social isolation (e.g., avoid social contact with family and friends) and the impossibility to engage in satisfying activity. These changes can impact the pace of the flow of time (Zakay, 2014), disrupt night‐time sleep (Altena et al., 2020) and increase the risk of mental health problems (Leigh‐Hunt et al., 2017). Sivertsen et al. (2019) have shown that young adults in a range between 18 and 35 years old tend to have a high and growing prevalence of sleep problems, and young adults make extensive use of social media devices that interact with daily activities, including sleep (Gradisar et al., 2013; Orzech, Grandner, Roane, & Carskadon, 2016). Social media platforms offer an opportunity to ameliorate social isolation, but the use of digital media near bedtime could have a broadly negative effect on sleep outcomes of young adults (Orzech et al., 2016).
We were interested in characterizing the change in digital media use before going to bed, in sleep quality and timing, and in the subjective experience of time passing, and their relationship with depression, anxiety and stress levels. To achieve this, we administered a cross‐sectional survey to non‐hospitalized Italian residents. In this survey we asked participants to think about the previous week (March 17–23, which was the second week of the lockdown) and the period prior to the first week of February (February 3–10, before any restriction in any Italian area).
2. METHODS
2.1. Participants
Participants completed an anonymous online survey, after reading the written consent form and explicitly agreeing to participate in the survey. The survey was shared via social media for a limited time window (from March 24 to 28, 2020), targeting people from 18 to 35 years old to obtain a homogenous sample of responders, because young adults (e.g., ages 18–35 years) are likely to be heavy digital users and they are especially at risk of sleep disturbance (Levenson, Shensa, Sidani, Colditz, & Primack, 2017; Sivertsen et al., 2019). There was no monetary or credit compensation for participating in the study. The study protocol was approved by the Ethics Committee of the Centre for Research and Psychological Intervention (CERIP) of the University of Messina and was conducted in accordance with the Declaration of Helsinki. A total of 1,342 participants completed the survey. From this sample, we excluded 26 participants who reported having been infected by COVID‐19, 17 participants with age >35 or <18 years and one outlier. The final sample consisted of 1,310 young adults living in the Italian territory. Data reported in this study were part of a wider research project designed with multiple purposes regarding the psychological impact of home confinement in Italy, and other data with different purposes will be presented elsewhere.
2.2. Measures
2.2.1. Sleep quality
Perceived sleep quality in the previous week (March 17–23, the second week of the lockdown) and prior to the first week of February (February 3–10, before any restriction in any Italian area) was assessed using the Italian version of the Pittsburg Sleep Quality Index (PSQI; Curcio et al., 2013). Scores higher than 5 indicate poor sleep. From the PSQI we also derived information about how many hours they spent in bed (TIB; hr), at what time participants went to bed to sleep (bedtime) and at what time participants woke up in the morning (wake time).
2.2.2. Digital media use near bedtime
The use of digital media was assessed by asking participants to report their frequency of digital media activity choices in the 2 hr before bedtime in the previous week and prior to the first week of February. We selected 10 digital media activities based on the work of Orzech et al. (2016), such as computer work, Email/instant messaging, social networking sites, videogames, surfing the internet, video calls/calls on phones, watching online videos, reading e‐books, watching TV/DVDs, and watching TV series. Response options ranged from “never” to “every day” and were transformed into weighted responses to estimate total digital media use per week (range, 0–70), as previously done by Orzech et al. (2016).
2.2.3. Experience of time
An ad‐hoc questionnaire was created to assess the ability of participants to keep track of physical time (Time Track, three items referring to difficulties in remembering the day of the week, remembering the day of the month and keeping track of the time of day), to assess the subjective experience of time (Time Expansion, two items referring to the feeling of boredom and that time is passing slowly) and to assess the regularity of daily routines (Schedule, two items referring to maintaining routines such as meal times and bedtimes).
2.2.4. Stress, depression and general anxiety
The short‐form version of the Depression Anxiety Stress Scales (DASS‐21) was used to assess stress, depression and general anxiety (Bottesi et al., 2015). Scores from each subscale were summed up and multiplied by two to suit the original 42 items. The cut‐offs for moderate symptomatology for depression, anxiety and stress are ≥14, ≥10 and ≥19, respectively (Lovibond & Lovibond, 1996).
3. RESULTS
Of the 1,310 participants (M age = 23.91 ± 3.60 years), 501 were workers (M age = 26.0 ± 4.06 years, 315 F) and 809 were university students (M age = 22.6 ± 2.53 years, 565 F). One‐fourth (24.2%) of the entire sample reported moderate to extremely severe symptoms of depression, 32.6% of the sample reported moderate to extremely severe symptoms of anxiety, and 50.12% of the sample reported moderate to extremely severe symptoms of stress (Figure 1a).
Figure 1.
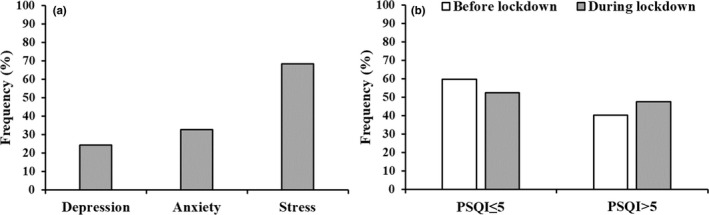
(a) Frequency of participants reporting moderate symptoms of depression, anxiety and stress as derived by the Depression Anxiety Stress Scales (DASS)‐21 scores. (b) Frequency of participants with a Pittsburg Sleep Quality Index (PSQI) score ≤ 5 and > 5 before and during the lockdown
Under the restriction, our sample increased the frequency of digital media use in the 2 hr before going to bed from ~27 activities a week before the restriction to ~31 activities under lockdown (F1,1,308 = 113.37, p < .0001, ηp 2 = .08).
Looking at changes in sleep habits, we observed a significant increase of the PSQI score under the restriction (F1,1,308 = 67.47, p < .0001, ηp 2 = .05), with no difference between students and workers (all ps > .187, Figure 2a). The proportion of poor sleepers (i.e., PSQI > 5) increased from 40.5% to 52.4% (χ2 1 = 84.50, p < .0001; log odds ratio = 1.070 [CI = 0.84–1.30]; Figure 1b). Sleep timing changed dramatically, with all participants going to bed later under restrictions (F1,1,308 = 384.1, p < .0001, ηp 2 = .22; Figure 2b). On average, bedtime was delayed by ~41 min in both workers and students. The restrictions had an even stronger effect on wake time (F1,1,308 = 535.29, p < .0001, ηp 2 = .29), in particular in workers (F1,1,308 = 22.25, p < .0001, ηp 2 = .02; Figure 2c), who started to wake up about 1 hr and 13 min later than usual, whereas students delayed their wake time by ~45 min. The later wake time resulted in a generally longer TIB under restrictions (F1,1,308 = 51.08, p < .0001, ηp 2 = .04), which was mainly driven by workers (F1,1,308 = 25.60, p < .0001, ηp 2 = .02; Figure 2d), who spent ~26 min more in bed than before the restrictions (change for students: ~5 min).
Figure 2.
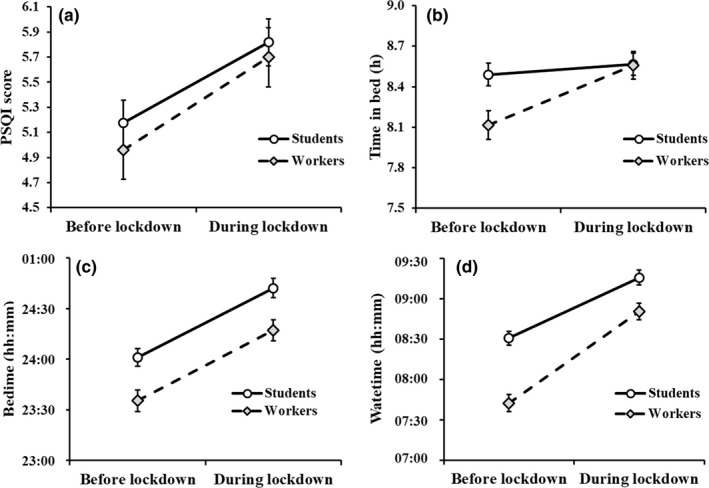
Changes in (a) Pittsburg Sleep Quality Index (PSQI) total score, (b) time in bed, (c) bedtime and (d) wake time as a function of the presence of the lockdown and the status (worker or student) of the participants. Error bars represent confidence intervals
Regarding the experience of time, the lockdown induced a significant increased difficulty in keeping track of time (F1,1,308 = 596.41, p < .0001, ηp 2 = .31), with people experiencing confusion about what day of the week, day of the month and time of the day it was, about six times in the week, compared to three times before lockdown. Also, they experienced an expansion of time during the lockdown (F1,1,308 = 188.05, p < .0001, ηp 2 = 0.13), with people increasingly feeling a sense of boredom, and they felt stuck in time about five times in the week compared to 3.5 times before lockdown.
We observed that the change in sleep quality (PSQI global score) was stronger in participants with a high DASS‐21 score (i.e., participants with higher symptoms of depression, anxiety and stress; r = .27, p<.001), in particular in students (Figure 3a). Interestingly, the increase in subjective elongation of time was moderately associated with poorer sleep quality (r = .33, p < .001), in particular in workers (see Figure 3b), but mildly associated with the increased use of digital media (r = .15, p < .001). Lastly, the increase in digital media use before going to bed mildly affected sleep habits; that is, sleep latency (r = .10, p < .001), bedtime (r = .09, p = .001) and wake time (r = .13, p < .001), but not sleep quality (r = .04, p = .166).
Figure 3.
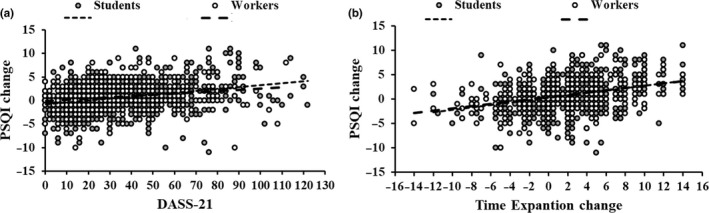
Change in Pittsburg Sleep Quality Index (PSQI) global score (before lockdown scores minus during lockdown scores) as a function of (a) Depression Anxiety Stress Scales (DASS)‐21 total score and (b) time expansion change in students and workers
4. DISCUSSION
In this cross‐sectional study, we investigated the impact of the Italian restriction measures on individuals' daily habits, such as sleep–wake rhythms, digital media use and the experience of time. As expected, during the lockdown people increased the usage of digital media near bedtime. However, this change in digital media use did not affect sleep habits. Nevertheless, already in the second week of the lockdown (March 17–23), sleep–wake rhythms markedly changed, with people going to bed and waking up later, and spending more time in bed, but, paradoxically, also reporting a lower sleep quality. The decrease in sleep quality was stronger for people with a higher level of depression, anxiety and stress symptomatology and also associated with an increased feeling of expansion of time.
Although this is a partial snapshot of the current Italian situation and does not consider adults older than 35 years and children and adolescents, our data seem to confirm the evidence already observed in quarantined individuals (Brooks et al., 2020), showing that people in lockdown are experiencing negative psychosocial changes, which have an impact on well‐being (e.g., sleep disturbances, depression and anxiety). As stated by a task force of the European CBT‐I Academy (Altena et al., 2020), during total lockdown individuals' sleep habits are challenged by several factors (i.e., reduced exposure to sunlight, reduced physical activity and psychological distress. We also think that the lack of social zeitgebers, such as regular work schedules and social activities, as well as changes in living conditions (e.g., moving to parents' house), are strongly affecting sleep habits under restrictions. Of note, our data were collected before the passage to the daylight‐saving time (March 29), which may further exacerbate sleep and mood problems in people living under social restrictions.
Considering that the lockdown is likely to continue for some weeks, there is a pressing need to monitor the psycho‐physiological well‐being of the population and to gather research data to develop evidence‐driven strategies to reduce adverse psychological impacts caused by these unprecedented changes in people's daily lives (Brooks et al., 2020; Lazzerini & Putoto, 2020). We are aware of several initiatives in Italy and worldwide to collect these data, which are urgently needed to support decision making, to build public awareness, and to provide timely and supportive psychosocial interventions (Lazzerini & Putoto, 2020).
CONFLICT OF INTEREST
This is not an industry‐supported study. None of the authors have potential conflicts of interest to be disclosed. All the authors have seen and approved the manuscript.
AUTHOR CONTRIBUTIONS
All authors developed the study concept, contributed to the study design, data collection and data analysis, interpreted the data, drafted the manuscript and approved the final version for submission.
ACKNOWLEDGEMENTS
The present work was carried out within the scope of the research program “Dipartimenti di Eccellenza” from MIUR to the Department of General Psychology.
Cellini N, Canale N, Mioni G, Costa S. Changes in sleep pattern, sense of time and digital media use during COVID‐19 lockdown in Italy. J Sleep Res. 2020;29:e13074. 10.1111/jsr.13074
Funding information
This work is supported by the University of Padova under the STARS Grants programme to NC.
REFERENCES
- Altena, E. , Baglioni, C. , Espie, C. A. , Ellis, J. , Gavriloff, D. , Holzinger, B. , … Riemann, D. (2020). Dealing with sleep problems during home confinement due to the COVID‐19 outbreak: Practical recommendations from a task force of the European CBT‐I Academy. Journal of Sleep Research. 10.1111/jsr.13052 [DOI] [PubMed] [Google Scholar]
- Bottesi, G. , Ghisi, M. , Altoè, G. , Conforti, E. , Melli, G. , & Sica, C. (2015). The Italian version of the Depression Anxiety Stress Scales‐21: Factor structure and psychometric properties on community and clinical samples. Comprehensive Psychiatry, 60, 170–181. 10.1016/j.comppsych.2015.04.005 [DOI] [PubMed] [Google Scholar]
- Brooks, S. K. , Webster, R. K. , Smith, L. E. , Woodland, L. , Wessely, S. , Greenberg, N. , & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet, 395(10227), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curcio, G. , Tempesta, D. , Scarlata, S. , Marzano, C. , Moroni, F. , Rossini, P. M. , … De Gennaro, L. (2013). Validity of the Italian version of the Pittsburgh sleep quality index (PSQI). Neurological Sciences, 34(4), 511–519. 10.1007/s10072-012-1085-y [DOI] [PubMed] [Google Scholar]
- Gradisar, M. , Wolfson, A. R. , Harvey, A. G. , Hale, L. , Rosenberg, R. , & Czeisler, C. A. (2013). The sleep and technology use of Americans: Findings from the National Sleep Foundation's 2011 sleep in America poll. Journal of Clinical Sleep Medicine, 9(12), 1291–1299. 10.5664/jcsm.3272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Istituto Superiore di Sanità . (2020, March 9, 2020). Comunicato stampa N°19/2020. Studio ISS. Un paziente su cinque positivo al coronavirus ha tra 19 e 50 anni. Retrieved from https://www.iss.it/comunicati‐stampa1 [Google Scholar]
- Lazzerini, M. , & Putoto, G. (2020). COVID‐19 in Italy: Momentous decisions and many uncertainties. Lancet Global Health, 8(5), e641–e642. 10.1016/S2214-109X(20)30110-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh‐Hunt, N. , Bagguley, D. , Bash, K. , Turner, V. , Turnbull, S. , Valtorta, N. , & Caan, W. (2017). An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health, 152, 157–171. 10.1016/j.puhe.2017.07.035 [DOI] [PubMed] [Google Scholar]
- Levenson, J. C. , Shensa, A. , Sidani, J. E. , Colditz, J. B. , & Primack, B. A. (2017). Social media use before bed and sleep disturbance among young adults in the United States: A nationally representative study. Sleep, 40(9). 10.1093/sleep/zsx113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond, S. H. , & Lovibond, P. F. (1996). Manual for the depression anxiety stress scales. Sydney, NSW: Psychology Foundation of Australia. [Google Scholar]
- Orzech, K. M. , Grandner, M. A. , Roane, B. M. , & Carskadon, M. A. (2016). Digital media use in the 2 h before bedtime is associated with sleep variables in university students. Computers in Human Behavior, 55, 43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sivertsen, B. , Vedaa, Ø. , Harvey, A. G. , Glozier, N. , Pallesen, S. , Aarø, L. E. , … Hysing, M. (2019). Sleep patterns and insomnia in young adults: A national survey of Norwegian university students. Journal of Sleep Research, 28(2), e12790. 10.1111/jsr.12790 [DOI] [PubMed] [Google Scholar]
- Wang, C. , Pan, R. , Wan, X. , Tan, Y. , Xu, L. , Ho, C. S. , & Ho, R. C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID‐19) epidemic among the general population in china. International Journal of Environmental Research and Public Health, 17(5), 1729. 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2020). Mental health and psychosocial considerations during the COVID‐19 outbreak. (No. WHO/2019‐nCoV/MentalHealth/2020.1). Retrieved from https://apps.who.int/iris/bitstream/handle/10665/331490/WHO‐2019‐nCoV‐MentalHealth‐2020.1‐eng.pdf?sequence=1&isAllowed=y [Google Scholar]
- Zakay, D. (2014). Psychological time as information: The case of boredom. Frontiers in Psychology, 5, 917. [DOI] [PMC free article] [PubMed] [Google Scholar]


