Abstract
Purpose
COVID-19 profoundly affected the United States, with New York City rapidly becoming the epicenter of the disease. Patients with cancer represent a vulnerable population in this pandemic, with data suggesting a higher risk for severe events and unfavorable outcomes. Timely identification of COVID-19 in patients with cancer has been thwarted by the limited availability of outpatient testing for SARS-CoV-2. Chest computed tomography (CT) plays a major role in the identification of COVID-19 pneumonia, with radiologic hallmarks including bilateral, peripheral ground-glass opacities (GGOs) and consolidation. Patients with cancer undergoing radiation therapy (RT) commonly have daily cone beam computed tomography (CBCT) obtained for image-guided RT, and such imaging frequently includes the chest.
Methods and Materials
We retrospectively reviewed the CBCT scans of an initially asymptomatic patient undergoing image-guided RT for breast cancer who developed COVID-19 symptoms during the second week of RT. Lung windows of daily CBCT scans were reviewed with diagnostic radiology to survey for changes consistent with COVID-19. Diagnostic CT scans at the time of recovery were obtained and compared with the CBCTs.
Results
Five consecutive CBCT scans were retrospectively reviewed. Bilateral, peripheral GGOs were noted on the fourth and fifth CBCT scans in the 2 days before symptom onset. CBCT on the day of RT resumption demonstrated substantial worsening of the GGO compared with scans obtained during the asymptomatic phase. Diagnostic CTs demonstrated bilateral, peripheral GGOs and mediastinal lymphadenopathy, findings suggesting COVID-19 pneumonitis. Repeat diagnostic CT 3 days later showed improved pulmonary findings, and the patient resumed RT without incident.
Conclusions
Familiarity with typical CT changes of COVID-19 pneumonitis may allow for early detection in cancer patients undergoing CBCT for RT treatment. Prompt review of the lung windows is recommended to identify such changes, with the hope that presymptomatic diagnosis leads to expedited patient management, improved outcomes, and a reduction of inadvertent COVID-19 dissemination.
Introduction
Since the initial cases of COVID-19 were reported in December 2019 in Wuhan, China,1 the SARS-CoV-2 virus disseminated internationally, rapidly reaching pandemic proportions. The United States has reported the largest number of cases worldwide, and New York City has become the epicenter of the crisis.2 In the face of COVID-19, patients with cancer represent a particularly vulnerable population, with data suggesting a higher risk for severe events such as intensive care unit (ICU) admission, ventilator requirement, or death compared with the general population.3,4 There is a wide variation in clinical presentation, with up to 80% of patients estimated to be asymptomatic5 and the remainder experiencing symptoms ranging from transient fever, dry cough, and dyspnea to respiratory failure, multiorgan failure, and death.6 Rare symptoms including anosmia and ageusia, in addition to gastrointestinal symptoms, have also been described.7,8 Adverse outcomes and death are more common in the elderly and those with comorbidities, with a fatality rate ranging from 4% to 11%.9
There have been several reports documenting the pulmonary imaging abnormalities associated with COVID-19, including in the setting of subclinical disease.10, 11, 12, 13 A study from China reported on temporal patterns of SARS-CoV-2 pneumonia on computed tomography (CT); the most common CT patterns in such patients were ground-glass opacities (GGOs), air bronchograms, crazy-paving patterns, and thickening of the adjacent pleura.10 Cone beam computed tomography (CBCT) is a medical imaging technique capturing cone-shaped x-ray beam images that are reconstructed to form a 3-dimensional axial representation of the patient.14 CBCT is one of many image-guided radiation therapy (RT) tools used for the verification of patient setup to ensure accurate RT delivery.15 In patients undergoing breast or thoracic RT, the lungs are encompassed in the daily CBCT, allowing the unique opportunity to monitor lung findings over several weeks. Typically, bone and soft tissue windows are used to allow for anatomic matching on specified structures for RT targeting. However, timely review of lung windows on CBCT may afford the opportunity to assess for lung changes indicative of asymptomatic SARS-CoV-2 infection.
Patients undergoing RT must present to a health care facility for treatment because delay, interruption, or premature termination of RT are associated with suboptimal oncologic outcomes.16, 17, 18, 19 Unfortunately, daily travel to a health care facility increases the risk of exposure to SARS-CoV-2, and, in the case of asymptomatic patients, inadvertent dissemination of the virus to other patients, health care professionals, and administrative staff. Rapid recognition of COVID-associated lung abnormalities on routine daily CBCTs may allow for early clinical assessment and the prompt initiation of appropriate precautions and/or treatment for these patients. The purpose of this case report is to describe an initially asymptomatic patient in our radiation oncology clinic who was noted to have imaging changes consistent with SARS-CoV-2 pulmonary changes on CBCT before the onset of symptoms.
Case
The patient is a postmenopausal woman who received a diagnosis of pathologic T2N0M0, moderately differentiated invasive ductal carcinoma of the right breast that was estrogen receptor–positive, progesterone receptor–positive, and human epidermal growth factor receptor 2–negative. The patient was treated with lumpectomy and sentinel-lymph node biopsy, to be followed by adjuvant hypofractionated whole-breast RT (4256 cGy in 16 fractions) and hormone therapy, as per multidisciplinary tumor board recommendations. At the time of CT simulation, the patient did not report fever or respiratory symptoms, and her lung parenchyma on the CT simulation was normal. Approximately 2 weeks later, in March 2020, RT was initiated, and the patient remained asymptomatic. The patient was treated on our Varian Halcyon unit, using daily kilo-voltage (kV) CBCTs for patient setup. During the first week of treatment, no radiographic pulmonary abnormalities were noted on daily review of the CBCT soft tissue windows.
The patient presented on Monday morning for her sixth fraction of RT, and upon COVID-19 verbal screening at the entrance to the cancer center, she reported a 2-day history of fatigue and fever, with a peak temperature of 101°F. She had no other complaints and denied respiratory symptoms. Her vital signs were within normal limits, and her oxygen saturation was at her baseline of 95% to 98% on room air. Lung auscultation revealed good air entry bilaterally with no adventitious sounds. Owing to the limited access of SARS-CoV-2 testing in New York City, outpatient testing was not available, and the patient’s symptoms were not severe enough to warrant referral to the emergency room. As per departmental guidelines based on CDC recommendations,20 the patient’s RT was held until she became afebrile without antipyretics for at least 72 hours and at least 7 days from symptom onset.
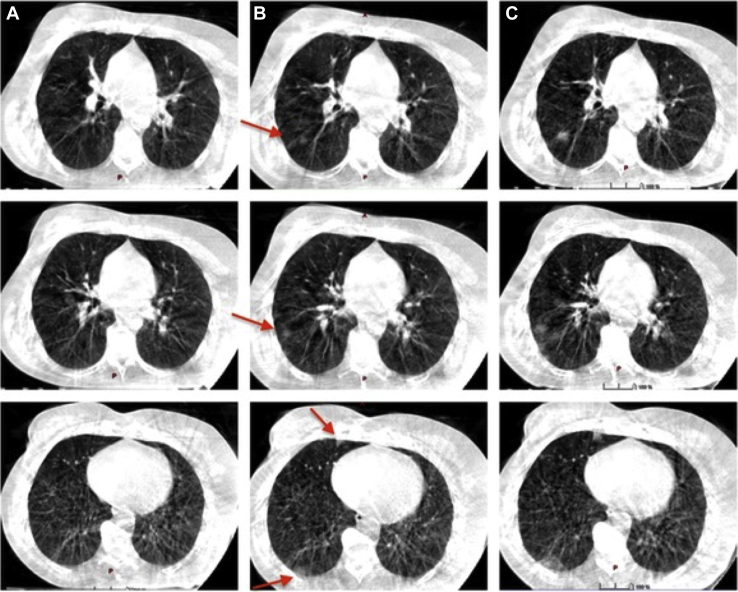
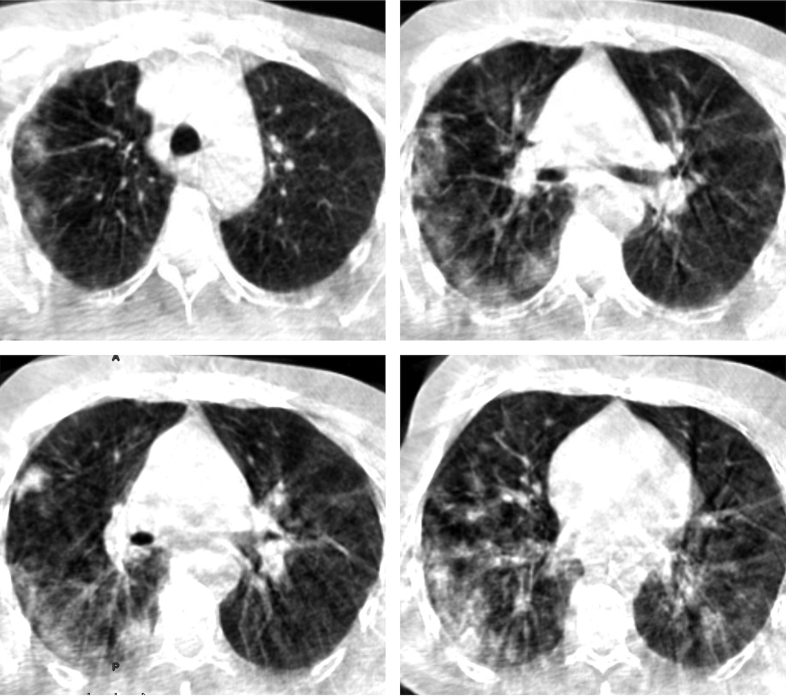
The patient’s 5 CBCT scans from the first week of RT were reviewed retrospectively, and peripheral, predominantly right lower lobe GGOs were noted on the CBCT obtained at the fourth and fifth fractions in the 2 days before her symptom onset (Fig 1). The patient was monitored daily via telemedicine. She remained febrile with fatigue and anorexia. On the fourth day after symptom onset, she reported a mild, transient dry cough, dysgeusia (“everything tastes salty”), and dysosmia (“smelling coffee all day”). The patient defervesced on the eighth day after symptom onset, and she was no longer symptomatic. On the 11th day after symptom onset, the patient met our departmental criteria for resuming RT with the appropriate precautions for COVID-recovered patients. CBCT that day showed substantial worsening of the GGO bilaterally (Fig 2). The case was reviewed with diagnostic radiology and infectious disease; given the severity of the radiologic findings and the unknown consequence of RT in a patient recovering from probable SARS-CoV-2 pneumonia, it was decided to hold RT again and obtain serial diagnostic imaging to monitor the progression of lung disease.
Figure 1.
(A) Baseline CBCT. (B) CBCT at fourth fraction. (C) CBCT at fifth fraction. Serial CBCT scans demonstrate increasing peripheral ground-glass opacities, predominantly in the lower right lobe (red arrows). Abbreviation: CBCT = cone beam computed tomography.
Figure 2.
Selected images from cone beam computed tomography scan obtained on the 11th day after symptom onset, after the patient had a complete clinical recovery and was eligible to resume radiation therapy based on departmental guidelines. The cone beam computed tomography scan demonstrates worsening peripheral ground-glass opacities with greater bilateral involvement.
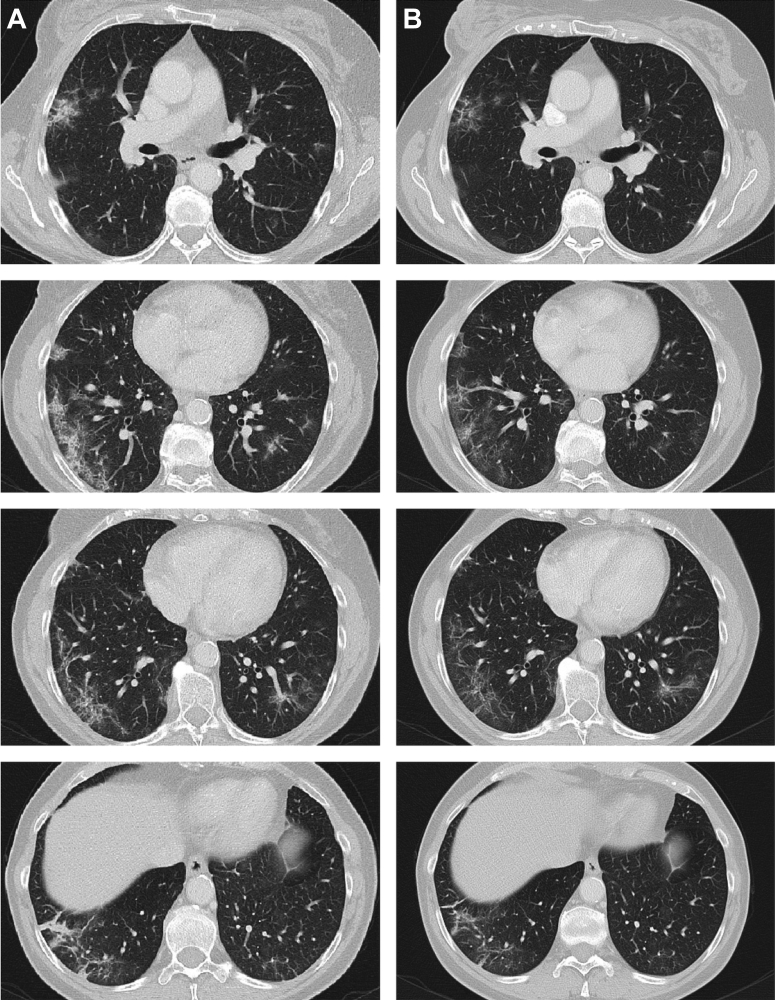
The patient underwent diagnostic CT of the chest on the 13th day after symptom onset, demonstrating bilateral, peripheral GGOs most prominent on the right side and lymph nodes in the pretracheal space and an aortopulmonary window measuring up to 1.2 cm (Fig 3, column A). Diagnostic impression was consistent with a viral pneumonitis, including COVID-19 pneumonia. Comparison made with CBCT scans from 2 days prior showed stable to improved pulmonary findings. Repeat diagnostic CT of the chest was performed on the 16th day after symptom onset, demonstrating improvement in bilateral, peripheral GGOs with decreased lymphadenopathy, suggesting an amelioration (Fig 3, column B). The patient resumed RT and remained asymptomatic with continued improvement in her pulmonary GGOs on subsequent CBCT scans.
Figure 3.
Left panel: diagnostic computed tomography scan obtained the 13th day after symptom onset demonstrating bilateral peripheral ground-glass opacities, more prominent on the right side. Right panel: diagnostic computed tomography scan obtained the 16th day after symptom onset, with improvement and diminished volume of ground-glass opacities.
Discussion
COVID-19 infection disproportionately affects patients with underlying comorbidities, including cancer.21 Given that patients with cancer require frequent medical visits to treatment facilities, the risk of inadvertent dissemination of COVID-19 poses a serious threat to this vulnerable patient population. Adding to this challenge is the covert nature of the SARS-CoV-2 virus, with rates of asymptomatic infection being reported as high as 80%. Up to 50% of asymptomatic patients can have radiographic abnormalities before the onset of symptoms.22 Radiographic imaging findings are important in the diagnosis and treatment of this disease. In patients with cancer receiving CBCT as part of their RT, review of lung windows to screen for COVID-19 changes could lead to early detection of the infection in asymptomatic patients.
Studies have described the radiographic characteristics of distinct groups of patients and temporal changes associated with disease progression.10 The imaging features of this viral pneumonia are diverse, typically ranging from normal appearance to diffuse changes in the lungs; patients with multiple comorbidities are more likely to have bilateral and diffuse disease.10 Overall, there is a slight predilection for the lower right lobe. The extent of disease on CT increases gradually from the subclinical period throughout the first 3 weeks, then decreases thereafter,10 but radiographic changes may continue to evolve beyond 26 days of symptoms.10,12 Asymptomatic patients are more likely to have unilateral, multifocal GGOs. After symptom onset, bilateral and diffuse GGOs are predominant. In the progressive stage, GGOs are relatively decreased in frequency, with a transition to consolidation and mixed-pattern development. As the disease peaks, GGOs decrease further, and peak lung involvement is characterized by increasing crazy-paving patterns and reticulation, along with bronchiolectasis and thickening of the adjacent pleura. The resolving stage demonstrates decreasing consolidation and absence of crazy-paving patterns after the first 2 to 3 weeks of disease.11, 12, 13,23, 24, 25 Our patient’s radiographic changes were generally consistent with the aforementioned findings; during the subclinical period, GGOs were predominantly located in the peripheral right lower lobe and progressed in the symptomatic stage to become more diffuse and bilateral. Based on our patient’s available imaging, her CT lung abnormalities appeared to peak in severity approximately 11 days after symptom onset, followed by gradual resolution of GGOs as demonstrated in her diagnostic CT scans (Fig 3).
Radiographic evolution of the disease typically mirrors the clinical course, with time to medical ventilation and ICU admission paralleling the severity of CT findings.26 Timely detection has been shown to be associated with improved clinical outcomes and prognosis.27 One retrospective series demonstrated as many as 75% of patients with negative reverse transcription polymerase chain reaction (RT-PCR) COVID-19 testing had positive CT findings; some patients continued to test negative on repeat RT-PCR before eventually testing positive, indicating CT findings may have greater sensitivity than RT-PCR. Interestingly, 40% of patients had improvement in CT findings before serial RT-PCR results converting from positive to negative,13 suggesting RT-PCR results lag behind radiographic findings.
Patients undergoing therapeutic radiation typically undergo radiographic confirmation of setup before treatment delivery. Modalities include KV port films using 2-dimensional x-ray and/or CBCT scans.15,28 Traditionally, patients treated with breast-tangent RT do not undergo daily image-guided radiation therapy, but rather weekly portal imaging. The Varian Halcyon 2.0 platform uses KV CBCT and iterative CBCT imaging for improved soft tissue definition.29 Patients with thoracic and breast malignancies undergoing treatment on the Halcyon receive CBCT for setup verification, which opportunely encompasses the lungs. Pulmonary infiltrates potentially indicative of infection with SARS-CoV-2 may be identifiable on routine daily CBCT scans, which would not otherwise have been appreciable with KV orthogonal imaging or weekly portal imaging. Given the relatively high proportion of patients with breast cancer treated in most radiation oncology departments, Halcyon’s daily KV CBCT imaging presents a unique opportunity for lung evaluation during the COVID-19 pandemic. Suppli et al have reported on early pulmonary findings discovered on retrospective review of daily CBCT scans done in a patient with lung cancer admitted to the ICU during RT who ultimately died of COVID-19 infection.30
In our institution, this case prompted the initiation of a protocol for the prospective review of thoracic CBCT scans in patients undergoing RT in an effort to detect pulmonary changes suggestive of COVID-19 pneumonitis. With the limited access to SARS-CoV-2 testing in NYC and the risk of false-negative RT-PCR despite abnormal CT chest findings, the utility of a laboratory test in identifying asymptomatic or suspected infected patients with cancer may be impractical. Given that imaging characteristics have been shown to correlate with clinical severity and progression of disease, the combination of clinical and laboratory findings and acquaintance with typical radiographic COVID-19-related changes may facilitate the prompt diagnosis of these patients, leading to immediate quarantine and/or treatment and decreased risk of unintended dissemination.
Conclusions
COVID-19 has affected the United States on a level not seen since the influenza pandemic of 1918, and NYC rapidly became the epicenter of the pandemic. Due to the high prevalence of asymptomatic patients and the limited availability of outpatient SARS-CoV-2 testing, a combination of screening for symptoms, clinical acumen, and use of available technology is necessary for the prompt identification and management of these patients. As many patients with cancer undergo routine CBCT during RT, familiarity with COVID-19-related lung changes may lead to earlier detection, diagnosis, and treatment while decreasing inadvertent dissemination among this vulnerable patient population.
Footnotes
Sources of support: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosures: The authors certify they have no affiliations with or involvement in any organization or entity with any financial interest, or non-financial interest in the subject matter or materials discussed in this editorial.
Data sharing: Research data are not available at this time.
References
- 1.Rothan H.A., Byrareddy S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:102433. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization Coronavirus disease (COVID-2019) situation reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports Available at:
- 3.Xia Y., Jin R., Zhao J., Li W., Shen H. Risk of COVID-19 for patients with cancer. Lancet Oncol. 2020;21 doi: 10.1016/S1470-2045(20)30150-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang L, Zhu F, Xie L, et al. Clinical characteristics of COVID-19-infected cancer patients: A retrospective case study in three hospitals within Wuhan, China [e-pub ahead of print]. Ann Oncol.https://doi.org/10.1016/j.annonc.2020.03.296. Accessed May 15, 2020. [DOI] [PMC free article] [PubMed]
- 5.Heneghan C., Brassey J., Jefferson T. COVID-19: What proportion are asymptomatic? https://www.cebm.net/covid-19/covid-19-what-proportion-are-asymptomatic/ Available at:
- 6.Adhikari S.P., Meng S., Wu Y.J. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: A scoping review. Infect Dis Poverty. 2020;9:29. doi: 10.1186/s40249-020-00646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gautier J.F., Ravussin Y. A new symptom of COVID-19: Loss of taste and smell. Obesity (Silver Spring) 2020;28:848. doi: 10.1002/oby.22809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tian Y., Rong L., Nian W., He Y. Review article: Gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther. 2020;51:843–851. doi: 10.1111/apt.15731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singhal T. A review of coronavirus disease-2019 (COVID-19) Indian J Pediatr. 2020;87:281–286. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shi H., Han X., Jiang N. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: A descriptive study. Lancet Infect Dis. 2020;20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bernheim A., Mei X., Huang M. Chest CT findings in coronavirus disease-19 (COVID-19): Relationship to duration of infection. Radiology. 2020 doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pan F., Ye T., Sun P. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology. 2020 doi: 10.1148/radiol.2020200370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ai T., Yang Z., Hou H. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases. Radiology. 2020 doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scarfe W.C., Farman A.G. What is cone-beam CT and how does it work? Dent Clin North Am. 2008;52:707–730. doi: 10.1016/j.cden.2008.05.005. v. [DOI] [PubMed] [Google Scholar]
- 15.Yan H., Zhen X., Cerviño L., Jiang S.B., Jia X. Progressive cone beam CT dose control in image-guided radiation therapy. Med Phys. 2013;40 doi: 10.1118/1.4804215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bese N.S., Sut P.A., Ober A. The effect of treatment interruptions in the postoperative irradiation of breast cancer. Oncology. 2005;69:214–223. doi: 10.1159/000087909. [DOI] [PubMed] [Google Scholar]
- 17.Chen M., Jiang G.L., Fu X.L. The impact of overall treatment time on outcomes in radiation therapy for non-small cell lung cancer. Lung Cancer. 2000;28:11–19. doi: 10.1016/s0169-5002(99)00113-0. [DOI] [PubMed] [Google Scholar]
- 18.Dong Y., Zaorsky N.G., Li T. Effects of interruptions of external beam radiation therapy on outcomes in patients with prostate cancer. J Med Imaging Radiat Oncol. 2018;62:116–121. doi: 10.1111/1754-9485.12675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gonzalez Ferreira J.A., Jaén Olasolo J., Azinovic I., Jeremic B. Effect of radiotherapy delay in overall treatment time on local control and survival in head and neck cancer: Review of the literature. Rep Pract Oncol Radiother. 2015;20:328–339. doi: 10.1016/j.rpor.2015.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention Discontinuation of isolation for persons with COVID-19 not in healthcare settings (interim guidance) https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-in-home-patients.html Available at:
- 21.Jordan R.E., Adab P., Cheng K.K. Covid-19: Risk factors for severe disease and death. BMJ. 2020;368:m1198. doi: 10.1136/bmj.m1198. [DOI] [PubMed] [Google Scholar]
- 22.Inui S., Fujikawa A., Jitsu M. Chest CT findings in cases from the cruise ship “Diamond Princess” with coronavirus disease 2019 (COVID-19) Radiol Cardiothorac Imaging. 2020;2 doi: 10.1148/ryct.2020200110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chung M., Bernheim A., Mei X. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. 2020;295:202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lei J., Li J., Li X., Qi X. CT imaging of the 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295:18. doi: 10.1148/radiol.2020200236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ng M.-Y., Lee E.Y.P., Yang J. Imaging profile of the COVID-19 infection: Radiologic findings and literature review. Radiol Cardiothorac Imaging. 2020;2 doi: 10.1148/ryct.2020200034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang G., Gong T., Wang G. Timely diagnosis and treatment shortens the time to resolution of coronavirus disease (COVID-19) pneumonia and lowers the highest and last CT scores from sequential chest CT. AJR Am J Roentgenol. 2020:1–7. doi: 10.2214/AJR.20.23078. [DOI] [PubMed] [Google Scholar]
- 28.Sterzing F., Engenhart-Cabillic R., Flentje M., Debus J. Image-guided radiotherapy: A new dimension in radiation oncology. Dtsch Arztebl Int. 2011;108:274–280. doi: 10.3238/arztebl.2011.0274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cai B., Laugeman E., Mazur T.R. Characterization of a prototype rapid kilovoltage x-ray image guidance system designed for a ring shape radiation therapy unit. Med Phys. 2019;46:1355–1370. doi: 10.1002/mp.13396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Suppli MH, Riisgaard de Blanck S, Elgaard T, Josipovic M, Pøhl M. Early appearance of coronavirus disease 2019 associated pulmonary infiltrates during daily radiotherapy imaging for lung cancer [e-pub ahead of print]. J Thorac Oncol. https://doi.org/10.1016/j.jtho.2020.04.004. Accessed May 15, 2020. [DOI] [PMC free article] [PubMed]