Abstract
The lower than expected rates of children affected by coronavirus disease-2019 does not mean that there was no impact on children's health. Using data on pediatric healthcare visits before and after the breakout of coronavirus disease-2019 and historical data, we identified pediatric conditions that were most affected by the pandemic and epidemic control measures during the pandemic.
Abbreviations: COVID-19, Coronavirus disease-2019; CR, Change rate; DVN, Daily visiting number
The coronavirus disease-2019 (COVID-19) pandemic is a global health crisis. As of April 30, 2020, there were 3 090 445 cases confirmed globally, with 217 769 deaths based on the World Health Organization situation report.1 Children typically are more susceptible to infectious diseases. Unexpectedly, <1% of confirmed COVID-19 cases were in children <10 years of age in China.2 , 3 The lower than expected rates of children affected by COVID-19 does not mean that there is no impact on children's health.4, 5, 6
China's unprecedented systematic and proactive risk management has proven to be effective in containing and controlling COVID-19. Zhejiang Province was the first province to raise the public health emergency response to the highest level in the early days of the outbreak. Hangzhou, which is the capital of Zhejiang Province, rigorously enforced travel and social distancing restrictions, home quarantine, and infection prevention and control in the hospital. The impact of these epidemic control measures on children's physical and mental health is unknown.5 , 7 In this study, we analyzed pediatric visit data during the pandemic in Hangzhou to identify whether restrictions affected children's health.
Methods
From a governmental statistical report, about 12.2 million children (<14 years of age) resided in Hangzhou (a city with area of 34 585 km2 is the capital and most populous city of Zhejiang Province) at the end of 2018. We collected data from outpatient healthcare visits between January 1, 2020, and March 31, 2020, as well as historical data during the same period of 2019 from the Children's Hospital, Zhejiang University School of Medicine. This children's hospital, with >1900 beds, is the largest comprehensive pediatric medical center in Zhejiang Province and the Chinese National Clinical Research Centre of Child Health. We calculated the rate of each disease in all visiting before and after January 25, 2020, and using the change rate (CR; the rate in all visiting after outbreak/rate in all visiting before outbreak) and daily visiting number (DVN) before and after outbreak (DVNbefore and DVNafter) to show changes of children's health during the pandemic under rigorous epidemic control measures. A CR of 1 means that the diseases do not change after the COVID-19 outbreak; a CR of <1 means the diseases were suppressed or inhibited during the pandemic; a CR of >1 means the diseases were stimulated or relative not inhibited during the pandemic. We use a CR of <0.5 to identify inhibited diseases and use a CR of >3 to identify stimulated diseases. We are using the DVN before the outbreak of >3 to filter inhibited diseases and total visiting number after outbreak of >120 to filter stimulated diseases to exclude the effects of rare sporadic diseases.
Results
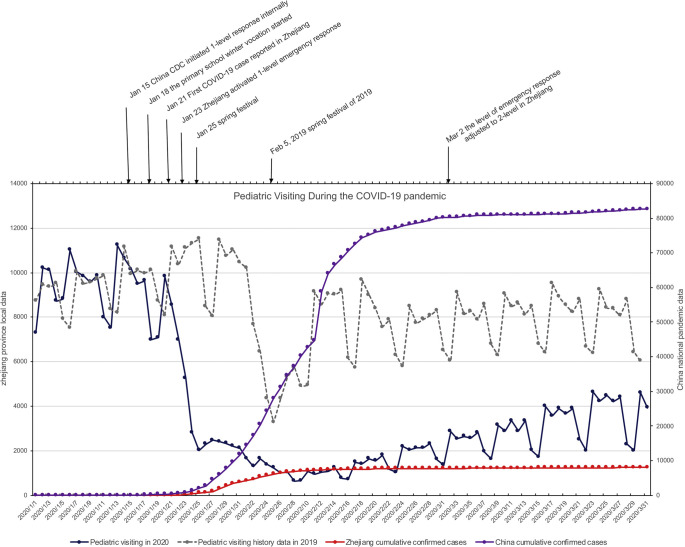
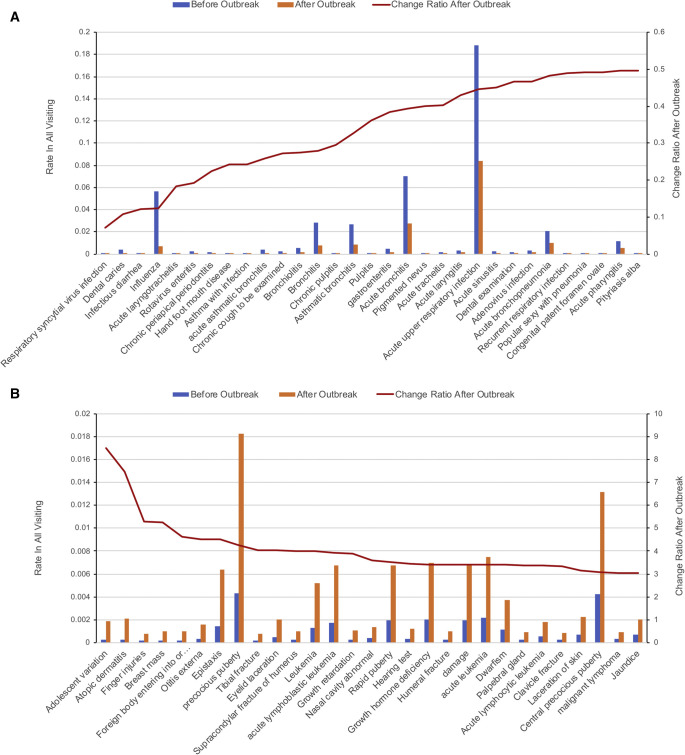
As shown in Figure 1 , the daily number of pediatric visits were similar to the historical data before the Chinese New Year (spring festival) on January 25, 2020. Coincident with COVID-19 restrictions, the daily number of pediatric visits after January 25, 2020, decreased to about only one-quarter compared with the historical data in 2019 owing to the measures, such as restriction of travel and social distancing, home quarantine, and infection prevention and control in the hospital, which suspended some services. Figure 2 shows the conditions for which visits were most changed. As shown in Figure 2, A, most decreases in visitations were for other infectious diseases such as respiratory syncytial virus infection (CR = 0.07, DVNbefore = 4.08, DVNafter = 0.08), influenza (CR = 0.12, DVNbefore = 494.38, DVNafter = 15.95), infectious diarrhea (CR = 0.12, DVNbefore = 9.00, DVNafter = 0.29), rotavirus enteritis (CR = 0.19, DVNbefore = 22.50, DVNafter = 1.14), and hand-foot-mouth disease (CR = 0.24, DVNbefore = 3.08, DVNafter = 0.20).
Figure 1.
The timeline of daily numbers of pediatric visits, cumulative confirmed cases of COVID-19 in the Zhejiang province and national response level in China during pandemic, and daily number of pediatric visits in the same period during 2019.
Figure 2.
Changes in children's healthcare visits during the COVID-19 pandemic in Hangzhou, China. A, Conditions with decreased rate of visits during the pandemic. B, Conditions with increased rate of visits during the pandemic.
Our elective dental visits were suspended after January 31; some visits for dental problems also decreased. Visits for the most common pediatric problems, such as acute upper respiratory infection (CR = 0.45, DVNbefore = 1642.46, DVNafter = 193.18) and acute bronchitis (CR = 0.39, DVNbefore = 610.04, DVNafter = 63.24) were inhibited substantially during the pandemic.
As shown in Figure 2, B, there also were conditions for which visits rate increased by more than 3-fold during this period. The number of patient visits for problems related to adolescent development, such as adolescent abnormality not otherwise specified (CR = 8.48, DVNbefore = 1.96, DVNafter = 4.38), breast mass (CR = 5.24, DVNbefore = 1.62, DVNafter = 2.24), precocious puberty (CR = 4.26, DVNbefore = 37.38, DVNafter = 41.95), and rapid puberty (CR = 3.51, DVNbefore = 16.79, DVNafter = 15.52) unexpectedly increased. Visits for pediatric skin problems, such as atopic dermatitis (CR = 7.46, DVNbefore = 2.46, DVNafter = 4.83), papular urticaria (CR = 2.94, DVNbefore = 4.67, DVNafter = 3.62), eczema (CR = 2.75, DVNbefore = 58.96, DVNafter = 42.67), and otitis externa (CR = 4.52, DVNbefore = 3.00, DVNafter = 3.58) also increased. The number of injuries also rose significantly, especially indoor injuries such as finger injuries (CR = 5.30, DVNbefore = 1.33, DVNafter = 1.86), foreign body entering into or through eye or natural orifice (CR = 4.62, DVNbefore = 1.92, DVNafter = 2.33), tibial fracture (CR = 4.04, DVNbefore = 1.75, DVNafter = 1.86), eyelid laceration (CR = 4.03, DVNbefore = 4.33, DVNafter = 4.61), and supracondylar fracture of humerus (CR = 4.00, DVNbefore = 2.13, DVNafter = 2.24). Some cases of epistaxis (CR = 4.51, DVNbefore = 12.29, DVNafter = 14.61) also were due to injuries. After January 25, 2020, there were 19 electrical injuries seen, compared with only 6 in the first 3 months in 2019.
Discussion
A pandemic like COVID-19 may have a relatively small impact on children owing to severe acute respiratory syndrome coronavirus 2 compared with adults. We show a substantial impact of quarantine measures on children's health for which concern and preparation are required.
Measures such as restriction of travel and social distancing, home quarantine, and infection prevention and control in the hospital, which necessitated suspending some services, likely were causes for both decrease in visits for some conditions and increase in visits for other conditions. As expected, most visits for common infectious diseases decreased. The potential explanation for increased visits by adolescents may be weight gain owing to longtime home quarantine and lack of exercise during this period. The high rate of atopic dermatitis and related skin conditions may be related to the lack of sunlight exposure and decreased vitamin D levels during the longtime home quarantine.
An increased number of visits for injury indicate that prevention should be put at a higher priority during the pandemic. Parents should be advised to the check safety of home play areas and ensure children's exposure to natural sunlight if possible when they are under home quarantine. They should especially be aware of eating behaviors and developmental changes in adolescents. Besides these issues, there may be long-term health problems, especially mental health issues, that deserve concern and follow-up.8
A limitation of this study is that rates of disease were measured using total visits and changes may be relative rather than actual. However, relative rates show willingness of patients or parents or both to visit for certain conditions. The outpatient daily visit number before outbreak was 8734.58 and the corresponding number during the outbreak was 2267.79 (CR = 0.26). This indicated that the relative rate after outbreak onset would be about 3.85 times if the DVN do not change. There also are some conditions such as leukemia (CR = 3.98, DVNbefore = 11.38, DVNafter = 11.94), for which change can be explained partially by cultural factors , eg, the choice of families to avoid side effects of difficult treatments before spring festival.
Footnotes
H.L. was supported by the National Natural Science Foundation of China (81871456) and National Key R&D Program of China (2016YFC0901905). J.F. was supported by Zhejiang University special scientific research fund for COVID-19 prevention and control. The authors declare no conflicts of interest.
References
- 1.World Health Organization (WHO) WHO; Geneva: 2020. Coronavirus disease (COVID-2019) situation reports. [Google Scholar]
- 2.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 3.Castagnoli R., Votto M., Licari A., Brambilla I., Bruno R., Perlini S. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.1467. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Cruz A.T., Zeichner S.L. COVID-19 in children: initial characterization of the pediatric disease. Pediatrics. 2020:e20200834. doi: 10.1542/peds.2020-0834. [DOI] [PubMed] [Google Scholar]
- 5.Golberstein E., Wen H., Miller B.F. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.1456. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 6.Humphreys K.L., Myint M.T., Zeanah C.H. Increased Risk for Family Violence During the COVID-19 Pandemic. Pediatrics. 2020:e20200982. doi: 10.1542/peds.2020-0982. [DOI] [PubMed] [Google Scholar]
- 7.Xie X., Xue Q., Zhou Y., Zhu K., Liu Q., Zhang J. mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.1619. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jiao W.Y., Wang L.N., Liu J., Fang S.F., Jiao F.Y., Pettoello-Mantovani M. Behavioral and Emotional Disorders in Children during the COVID-19 Epidemic. J Pediatr. 2020;221 doi: 10.1016/j.jpeds.2020.03.013. 264-6.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]