Abstract
Depression and anxiety are common among people who have experienced an acute coronary event (e.g., heart attack). Multidisciplinary cardiac rehabilitation programs often focus on reducing risk factors associated with future cardiac events, however, mental health interventions are not routinely available. Given known difficulties with access to mental health treatment, the present study sought to explore the efficacy and acceptability of an Internet-delivered cognitive behavioural therapy program (Cardiac Wellbeing Course) among participants who experienced an acute coronary event. The five-lesson course was delivered over eight weeks and was provided with brief weekly contact, via telephone and secure email with a guide. Participants were randomized to the Cardiac Wellbeing Course (n = 25) or waiting-list control group (n = 28). Symptoms were assessed at pre-treatment, post-treatment, and four-week follow-up. Completion rates (84%) and satisfaction ratings (95%) were high. Statistically significant between-group improvements were observed for the treatment group on primary measures of general anxiety (Cohen's d = 1.62; 67% reduction), depression (Cohen's d = 1.09; 61% reduction), and physical activity levels (Cohen's d = 0.27; 70% increase). Statistically significant improvements were also observed on secondary measures of distress (Cohen's d = 0.98; 51% reduction), cardiac anxiety (Cohen's d = 0.92; 34% reduction), and mental-health quality of life (Cohen's d = 0.23; 24% improvement). The changes were maintained at four-week follow-up. The current findings add to the existing literature and highlight the potential of Internet-delivered cognitive behavioural therapy programs among participants who have experienced an acute coronary event.
Keywords: Depression, Anxiety, Internet-delivered, Cognitive behaviour therapy, Transdiagnostic, Cardiac
Highlights
-
•
Randomized controlled trial of Internet-delivered therapy for a cardiac population
-
•
Large improvements in anxiety and depression (d = 1.62, 1.09) compared to controls
-
•
Improvements in activity levels and heart-focused anxiety also observed
-
•
High completion rates (84%) and satisfaction ratings (95%) of course
-
•
Future research should examine integration of the course in healthcare settings.
1. Introduction
Cardiovascular disease (CVD) affects approximately 1.3 million Canadians and is the second leading cause of death in Canada, after cancer (Public Health Agency of Canada, 2018). In CVD, excess burden is placed on the heart which can lead to an acute coronary event (ACE) such as unstable angina (i.e., insufficient blood flow to the heart causing chest pain) or myocardial infarction (i.e., heart attack). Depression and anxiety are estimated to affect 20% of individuals who have experienced an ACE (Kuhl et al., 2006; Mampuya, 2012).
Prolonged exposure to depression and anxiety have been identified as important to the development and prognosis of CVD (Huether and Mccance, 2012), although the link between psychological treatment and cardiac outcomes remains unclear. A large review of outcomes in coronary heart disease studies did not find a reduction in mortality associated with psychological treatments (Richards et al., 2017). However, supplementing treatment of physical symptoms with psychological treatment has been demonstrated to reduce patient mortality among men, with the most effective trials being offered shortly after a cardiac event (i.e., two months; Linden et al., 2007). Additionally, a large reduction in adverse clinical events at follow-up were observed when cardiac rehabilitation patients received psychological interventions for stress compared to cardiac rehabilitation without a psychological component (18% vs. 33%, respectively; Blumenthal et al., 2016).
Providing psychological treatment to people with CVD is hypothesized to enhance cardiac recovery in other ways (Compare et al., 2011; Panaite et al., 2015). For example, the presence of depression and anxiety are associated with lower exercise, higher fatigue, and lower quality of life among people with CVD (Mampuya, 2012). Depressive symptoms are also associated with poor attendance and compliance with cardiac rehabilitation programs (Caulin-Glaser et al., 2007). Treating depression and anxiety using cognitive behavioural therapy (CBT) has been shown to increase quality of life, in addition to reducing symptoms among people with CVD (Reavell et al., 2018). Furthermore, the authors of a global review of cardiac rehabilitation guidelines reported consensus among major public health agencies regarding the importance of assessing and addressing psychological symptoms such as depression after a cardiac event (Mehra et al., 2019). A scientific statement made by the American Heart Association also echoes this sentiment and recommends that psychological interventions for depression and anxiety be considered an integral part of cardiac rehabilitation programs (Leon et al., 2005).
Despite the high prevalence of anxiety and depression among people with CVD, mental health interventions are not routinely available following an ACE, even among people who attend cardiac rehabilitation programs (Messerli-Burgy et al., 2012). Additional barriers exist, such as stigma associated with seeking mental health care, focus on physical health following cardiac events, and lack of access to efficient evidence-based psychological treatments (Mampuya, 2012). Without effective tools to manage contributory factors in CVD (e.g., depression and anxiety), excess strain is placed on the health care system (Blumenthal et al., 2016).
One strategy for increasing access to timely psychological care are Internet-delivered cognitive behavioural therapy (ICBT) interventions (Andersson and Titov, 2014). In ICBT, structured therapeutic content is typically provided to participants, which is often divided into weekly lessons and delivered over the Internet. There are several reviews that support the efficacy of ICBT as a treatment for a variety of psychological disorders, with large effect sizes reported for disorder-specific programs (Andersson et al., 2019; Andrews et al., 2018). Additionally, reviews have been conducted for ICBT programs which treat depression and anxiety among people with somatic conditions with favourable results (Mehta et al., 2018; van Beugen et al., 2014). ICBT programs which treat multiple conditions in the same protocol (e.g., depression and/or anxiety), often referred to as transdiagnostic ICBT, produce results comparable to disorder-specific ICBT programs (Pasarelu et al., 2017).
ICBT programs developed specifically for cardiac conditions have also been studied but results have been mixed regarding the efficacy of such interventions. For example, some researchers have reported important and statistically-significant change among participants corresponding with small to large effect sizes (Glozier et al., 2013; Johansson et al., 2019) which indicates the potential efficacy of such programs. Another study demonstrated a statistically non-significant between group effect, however, a statistically-significant change corresponding to a medium effect size was observed among intervention participants (Lundgren et al., 2016). On the other hand, results from some studies have failed to demonstrate statistically significant between-group change, which have been explained as the result of using an active control group (Lundgren et al., 2016) and recruitment and attrition problems (Habibovic et al., 2014; Norlund et al., 2018).
Given the importance of providing rehabilitation to people after experiencing an ACE, there remains a need for further development and testing of alternative models of treatment, such as transdiagnostic approaches and adapting existing Internet-delivered programs which have been previously established as efficacious. To date, no published transdiagnostic ICBT studies have been developed and tested among Canadians who have experienced an ACE. To address this need, the current study used a randomized controlled trial (RCT) design to examine the efficacy of a transdiagnostic ICBT course initially developed to target depression and anxiety (Cardiac Wellbeing Course) for adults who have experienced an ACE (i.e., myocardial infarction or unstable angina) compared to a waiting-list control group. To assess for acceptability, data regarding completion rates, participant satisfaction, and negative effects of treatment were gathered. It was hypothesized that participants who received the 8-week intervention would report: (1) significant improvements on measures of depression, general anxiety, and activity levels relative to the control group, (2) significant improvements on secondary measures of cardiac anxiety, distress, and quality of life relative to the control group; and (3) a negligible amount of negative effects and a high level of satisfaction with the course.
2. Method
2.1. Design and ethics
The study used an open, two-arm, RCT design in which participants were randomly assigned to receive 1) transdiagnostic ICBT, or 2) an eight-week waiting-list which served as a control for the influence of time on symptom change between the two groups. Outcomes were assessed at pre-treatment, post-treatment, and four-week post-treatment follow-up. All measures were completed online. The current trial received institutional research ethics board approval and was registered (ISRCTN#18912772).
2.2. Participant recruitment, screening, and randomization
According to a preliminary power analysis, a total of 70 participants (35 in each group) were required to participate in the current study. However, difficulties in recruitment resulted in conducting a secondary power analysis which assumed large (rather than medium) effects based on similar ICBT programs (Reinholt and Krogh, 2014; Titov et al., 2011). As such, a total of 16 participants per group was calculated as sufficient (one-tailed test, power at 90%, and alpha at 0.05) to detect large between group effects (f = 0.50).
Recruitment occurred across 10 provinces in Canada through social media, print and television media, national cardiac groups, private and public rehabilitation centres, private employee assistance companies, and in waiting rooms of physician clinics, walk-in clinics, and pharmacies. Recruitment also involved brief speaking arrangements to address members of the public, public groups, and delivering webinars to nursing and health professional staff at cardiac rehabilitation centres. Recruitment consisted of educating organizations about ICBT and providing the web address of the study website where prospective participants could register.
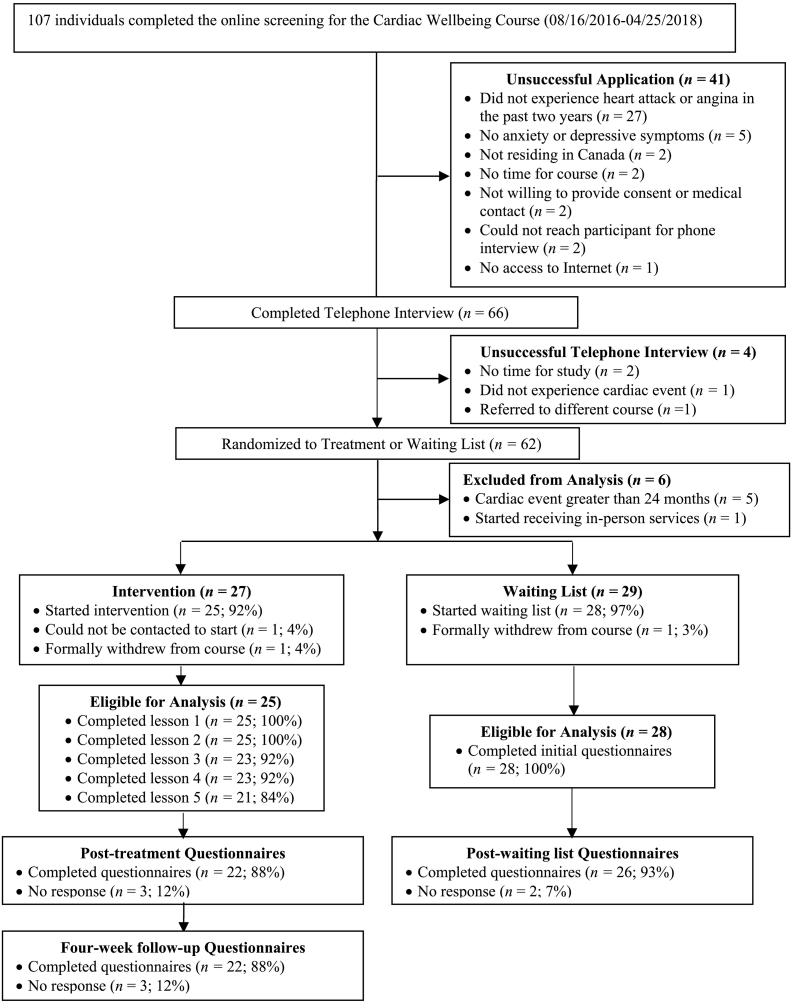
A total of 107 individuals applied for the Cardiac Wellbeing Course, of which, 56 met inclusion criteria. Participants were eligible for the current study if they 1) experienced an ACE (i.e., myocardial infarction or unstable angina) within the last 24 months, 2) were over the age of 18, 3) endorsed symptoms of depression and/or anxiety, and 4) had access to the Internet. The time frame of 24 months was chosen in line with a large ICBT protocol among cardiac patients (Norlund et al., 2015) and to ensure that participants' concerns were related to a recent cardiac event. Participation in the intervention was not restricted by requiring minimum depression or anxiety symptom levels, which is consistent with previous trials of the Wellbeing Course where patients with subthreshold symptoms have been found to benefit from treatment (Hadjistavropoulos et al., 2016; Hadjistavropoulos et al., 2017). As such, participants who met all other inclusion criteria and self-identified as requiring assistance with managing depression and/or anxiety symptoms primarily related to their ACE were included in this study. Participants were excluded from the study if they 1) had an acute health threatening disease (e.g., cancer), 2) severe psychiatric illness (e.g., psychosis), 3) suicidal thoughts or plans, or 4) had an unstable heart condition. Participants received no remuneration for their participation in the study. The flow of participants in this study is presented in Fig. 1.
Fig. 1.
Participant flow for the Cardiac Wellbeing Course.
All interested potential participants were directed to the study website (www.onlinetherapyuser.ca) where they were assessed for program eligibility using an Internet-delivered screening questionnaire after providing informed consent. The questionnaire assessed basic study eligibility and gathered information regarding background, cardiac history, and severity of depression and anxiety symptoms. An application programming interface connected to an online randomizer (www.random.org) was integrated with the online assessment software, such that participant randomization occurred automatically at the point of application and was reviewed only after participants were successfully admitted to the study. Participants were randomized to the intervention or an eight-week waiting-list control condition using a 1:1 ratio and a simple randomization sequence. Participants assigned to the waiting-list control group had the opportunity to receive the intervention once the eight-week waiting period was over.
Following completion of the online screening questionnaire, a telephone interview was conducted by the primary researcher or research assistant to ensure program eligibility and to enroll participants in the intervention. During the telephone interview, details were gathered to ensure program eligibility as per inclusion and exclusion criteria (e.g., acute health condition, severe psychiatric diagnosis) and to assess for risk of suicidality. The interview was also used to ensure participants fully understood the nature of the treatment and study requirements. Following the successful completion of the telephone interview, participants randomized to the intervention were able to start the program immediately. Conversely, participants assigned to the waiting-list control group were provided with a unique username and password to a version of the website containing outcome measures only (i.e., no therapeutic material). Participants allocated to the waiting-list condition were offered access to the Cardiac Wellbeing Course once their eight-week waiting period had elapsed.
2.3. Intervention
The treatment program was entitled the Cardiac Wellbeing Course, which was modified and adapted from an existing ICBT program (Wellbeing Course) originally developed at the eCentreClinic, Macquarie University, Australia (Titov et al., 2015). The Wellbeing Course is an eight-week online transdiagnostic course that consists of lesson content delivered in slideshow format, lesson summaries combined with recommendations for practicing lesson skills, and additional resources on topics not covered in the lessons (e.g., managing sleep difficulties, effective communication). The course also contains vignettes (i.e., patient stories) illustrating the skills emphasized in each lesson and documents (i.e., frequently asked questions) with answers to common questions about how to apply the course material. All materials are intended to be presented online. In addition to reviewing the modules and completing homework exercises, participants receive standardized automated emails each week notifying them of new content, reinforcing completion of course materials, and reminding them about content they have not accessed.
To develop the Cardiac Wellbeing Course, modifications were made to the original Wellbeing Course, including: 1) minor modifications to the slide content to increase the relevance of the intervention to people who have experienced an ACE, 2) creation of two new vignettes reflecting people who had experienced an ACE and were also struggling with depression and anxiety; and 3) creation of a supplemental resource introducing techniques to cope with fear related to uncertainty of a future cardiac event. Material used to modify the slide content was based on information typically found in educational pamphlets by cardiac health groups (e.g., Heart and Stroke Foundation) and provided participants with information regarding the recurrence of cardiovascular events. This material appeared in early lessons of the course. The patient vignettes created for the course replaced ones from the original Wellbeing Course and were available for every lesson. Special attention was placed on illustrating common struggles with depression and/or anxiety after a cardiac event, both cognitively and behaviorally (e.g., limiting physical activity and socialization in response to low mood or fears of physical activity). Inspiration for the patient vignettes was taken from firsthand accounts of experiencing a cardiac event which were publicly available on cardiac websites (e.g., Heart and Stroke Foundation). The supplemental resource was based on cognitive-behavioural and mindfulness techniques used in the treatment of chronic health conditions (Kabat-Zinn, 2013) and focused on changing cognitions and behaviour in order to increase coping with fear and uncertainty of future cardiac recurrence. Materials developed for the Cardiac Wellbeing Course were reviewed by several reviewers (e.g., lay audience with CVD, researchers with ICBT experience and experience in health psychology) who gave qualitative and informal feedback prior to the launch of the trial.
2.4. Guided support
Following the protocol used in the Wellbeing Course (Titov et al., 2015), contact with participants occurred via secure messaging and telephone. Participants received support from the primary researcher who was trained in the provision of online therapy and who acted as program guide throughout the study. A registered social worker also trained in the provision of online therapy provided treatment to one participant during the study when the primary researcher was unavailable to act as a program guide. As participants worked through each lesson, they were able to send a message to their guide, who was responsible for communicating with participants on a weekly basis through the secure messaging system. Participants were also given the choice to receive brief weekly telephone calls instead of online messages if preferred. Weekly contact was confined to approximately 10 min per phone call or email, unless clinically indicated. The aim of support in the Cardiac Wellbeing Course was to summarize course content, answer questions, reinforce progress and encourage skills practice, normalize challenges of treatment, and obtain feedback about the course. All telephone contact with participants was noted for record-keeping purposes and the guides acted under the supervision of a registered psychologist.
2.5. Measures1
Initial eligibility and background information was gathered by an online screening questionnaire upon application to the study. Participants randomized to the waiting-list control group completed a set of initial baseline questionnaires (i.e., primary and secondary measures) which were then re-administered once the eight-week waiting period had ended. Participants randomized to the intervention completed primary and secondary measures upon starting the course and at the end of the eight-week course. Intervention participants also completed primary measures at the beginning of every lesson of the course and at post-treatment were asked treatment satisfaction questions. Intervention participants were surveyed again at four-week follow-up and completed the primary measures as well as a measure of cardiac anxiety and distress. Participants randomized to the waiting-list control group did not complete follow-up measures.
2.5.1. Primary measures
2.5.1.1. General anxiety
The Generalized Anxiety Disorder 7-Item Scale (GAD-7; Spitzer et al., 2006) was used to measure anxiety levels among participants. The GAD-7 is a seven-item measure which asks participants to rate the frequency of common symptoms of anxiety over the past two weeks using a scale that ranges from 0 (not at all) to 3 (nearly every day). The GAD-7 has excellent internal consistency (Cronbach's α = 0.92) and strong criterion validity (Spitzer et al., 2006). A total score of ≥10 has been identified as an acceptable cut-off score indicative of clinical levels of anxiety (Kroenke et al., 2010). Preliminary research has demonstrated that the GAD-7 possesses good psychometric properties in a sample of participants with CVD and can act as an effective screening tool for anxiety (Lehmann et al., 2018). Cronbach's α in the current study ranged from 0.85 (pre-treatment) to 0.90 (post-treatment).
2.5.1.2. Depression
The Patient Health Questionnaire 9-item scale (PHQ-9; Kroenke et al., 2001) was used to measure symptoms of depression among participants. The PHQ-9 is a nine-item measure of the symptoms and severity of major depressive disorder. Each item is rated on a scale from 0 (not at all) to 3 (nearly every day). The PHQ-9 has been recommended as a brief screening tool among cardiac patients and a total score ≥10 has been identified as an acceptable cut-off score indicative of major depressive disorder among patients with coronary artery disease (McManus et al., 2005). The PHQ-9 also has excellent internal consistency among cardiac patients (Cronbach's α = 0.90; Stafford et al., 2007). Cronbach's α in the current study ranged from 0.85 (pre-treatment) to 0.90 (post-treatment).
2.5.1.3. Physical activity
The Godin Leisure-time Exercise Questionnaire (GLTEQ; Godin and Shephard, 1985) was used to measure physical activity among participants. The GLETQ asks participants to indicate how many 15-min periods per week of various types of exercise they engaged in during the previous 7-day period (i.e., strenuous, moderate, and mild; examples provided). A summary score indicating total leisure activity is calculated by multiplying the number of participant-identified 15-min periods of exercise by weights of 9, 5, and 3, respectively, to create an overall score with higher scores reflective of greater physical activity levels. Previous examinations of the GLTEQ indicate that it can adequately discriminate between physically active and inactive respondents (Amireault and Godin, 2015). Additionally, the GLTEQ is used in research among patients with multiple sclerosis and in studies of physical activity among CVD populations (Rodgers et al., 2013; Sikes et al., 2018; Tokgözoðlu et al., 2016).
2.5.2. Secondary measures
2.5.2.1. Cardiac anxiety
The Cardiac Anxiety Questionnaire (CAQ; Eifert et al., 2000) is an 18-item measure that was used to assess symptoms of heart-focused anxiety. Participants are asked to rate the frequency of activity avoidance, worry, and fear related to their heart using a scale that ranges from 0 (never) to 4 (always). Mean scores for the CAQ are created for three subscales (i.e., heart-related fear, avoidance, attention to symptoms) as well as a mean total score, with higher scores indicating higher levels of cardiac anxiety. The CAQ has good reliability in medical settings (Cronbach's α = 0.83; Eifert et al., 2000) and has also demonstrated adequate reliability in an examination of ICBT for heart failure patients (Cronbach's α = 0.85 and 0.87; Lundgren et al., 2016). A single cut-off score has not been proposed for the CAQ. Cronbach's α in this study for the CAQ-total score ranged from 0.83 (pre-treatment) to 0.90 (post-treatment); avoidance subscale 0.90 and 0.84; attention subscale 0.75 and 0.76; and fear subscale 0.64 and 0.85.
2.5.2.2. Distress
The Depression, Anxiety, and Stress Scale (DASS-21; Lovibond and Lovibond, 1995) was used to measure symptoms of distress among participants. The DASS-21 is a 21-item measure that that consists of three subscales (i.e., depression, anxiety, stress), each item of which is rated on a scale that ranges from 0 (never) to 3 (almost always). A total score was created by summing all items, which can be used as an indicator of distress (Henry and Crawford, 2005; Osman et al., 2012). Additionally, subscale scores for depression, anxiety, and stress were also calculated by summing seven corresponding items from the DASS-21. The DASS-21 has good internal consistency (Cronbach's α for total score = 0.97, depression = 0.95, anxiety = 0.90, and stress = 0.93) and concurrent validity (Crawford and Henry, 2003). Preliminary research has demonstrated that the DASS-21 possesses good psychometric properties in a sample of CVD patients attending cardiac rehabilitation (Komasi et al., 2018). Cronbach's α in this study for the DASS-21-total score ranged from 0.89 (pre-treatment) to 0.91 (post-treatment); depression subscale 0.90 and 0.92; anxiety subscale 0.74 and 0.67; and stress subscale 0.80 and 0.86.
2.5.2.3. Quality of life
The Short Form Health Survey 12-Item version 2 (SF-12; Ware Jr. et al., 1996) was used as a general measure of health-related quality of life among two domains: physical health functioning and mental health functioning. Scores on each scale range from 0 to 100, with higher scores indicating greater health. The SF-12 has good internal consistency (physical health, Cronbach's α = 0.89; mental health, Cronbach's α = 0.86). An examination of the SF-12 in a sample of patients with coronary heart disease indicated that the measure replicated well and similar responsiveness to change was observed compared to a longer version of the measure (Müller-Nordhorn et al., 2004). Cronbach's α in the current study ranged from 0.77 (pre-treatment) to 0.78 (post-treatment) for the physical health functioning scale and 0.76 and 0.80 for the mental health functioning scale.
2.6. Treatment satisfaction and negative effects
Following past ICBT research (e.g., Titov et al., 2015), participants who received the intervention indicated whether they would recommend the intervention to a friend and whether completing the course was worth their time (yes/no). Participants were also asked if they experienced any unwanted negative effects associated with receiving treatment (yes/no), and responding yes to this question were prompted to provide details (Rozental et al., 2014).
2.7. Intervention use
For participants who received the intervention, several activities were recorded for the purposes of describing engagement with the program. The number of logins to the program was captured as well as the number of days which participants accessed the service. The number of lessons completed by participants was also captured as a means of describing program completion. The number of emails sent by participants to their guide as well as the number of emails and phone calls received from their guide was recorded as a means of describing program engagement.
2.8. Analytic plan
SPSS version 23 was used to conduct all statistical analyses. Descriptive statistics were used to describe participant background, intervention use, and treatment satisfaction. Group differences on demographic variables were assessed using binomial regressions and general linear models analysis. The alpha significance level for these analyses was adjusted from 0.05 to 0.01 as a partial control for the number of analyses conducted.
Consistent with previous research (Dear et al., 2015b; Hadjistavropoulos et al., 2016), generalized estimation equation (GEE) models were used to examine changes in symptoms over time while also accounting for within-subject variance (Hardin and Hilbe, 2013; Hubbard et al., 2010). An interchangeable working correlation with robust error estimation was used and was chosen for model parsimony. The distribution of each dependent variable was examined prior to the analyses and each GEE model specified a gamma with log link response scale to address skewness within the dependent variables.
To address missing values and consistent with previous research (Dear et al., 2015a), replacement values were generated for all dependent variables (National Research Council, 2010) at post-treatment and four-week follow-up using participants' baseline scores for each measure as a covariate. Participants who did not start the waitlist or the intervention were not included in the analysis. Among participants who received the intervention, 12% (n = 3) of data was missing at post-treatment and four-week follow-up compared to 7% (n = 2) of missing data at post-treatment for participants randomized to the waitlist. An exploration of demographic and symptom variables predicting missing values was conducted to determine suitability of a missing at random assumption (MAR; Karin et al., 2018; Little et al., 2014). The missing values analyses were statistically non-significant, indicating that a MAR assumption would be suitable, and which allowed imputation of missing cases.
To compare outcomes between the intervention and waitlist-control groups, GEE analyses were conducted for the primary measures (i.e., GAD-7, PHQ-9, GLTEQ) and secondary measures (i.e., CAQ, DASS-21, SF-12) among participants from pre-treatment to post-treatment. To provide additional clinical information, effect sizes (Cohen's d) and 95% confidence intervals were calculated for within and between effects based on pooled standard deviations which were calculated for the estimated standard errors. Additionally, the number of participants reporting reliable symptom improvement and recovery were calculated for the GAD-7 and PHQ-9. Following past research (Jacobson and Truax, 1991; Richards and Borglin, 2011), participants were determined to have met criteria for reliable improvement if they scored above the clinical cut-off scores at pre-treatment (i.e., ≥10 on the GAD-7 or PHQ-9) and their symptoms improved by an amount greater than potential measurement error (3.53 or 5.20 respectively; as reported by Gyani et al., 2013). Reliable recovery was determined to have occurred if participants scored above the clinical cut-off scores at pre-treatment, if they made reliable improvement, and if they scored below the clinical cut-off scores at post-treatment.
Treatment satisfaction was evaluated using descriptive statistics to report the means, standard deviations, and ranges for participant ratings of treatment satisfaction and negative effects questions. Additional information from program use variables were also reported (i.e., range and frequency of logins, days access, lessons completed, messages sent, messages received, and phone calls received) as an indicator of program engagement.
3. Results
3.1. Baseline information
Demographic information is presented in Table 1. Statistically significant group differences were not observed for background variables. Similarly, no statistically significant group differences were observed for cardiac-related variables.
Table 1.
Participant characteristics and program engagement by group.
| Variable | All participants (n = 53) |
Intervention (n = 25) |
Waiting-list group (n = 28) |
Statistical significance | |||
|---|---|---|---|---|---|---|---|
| N | % | n | % | n | % | ||
| Participant pre-treatment characteristics | |||||||
| Age | |||||||
| Mean (SD) | 58.08 (9.59) | – | 56.72 (11.90) | – | 59.29 (6.93) | – | F1,51 = 0.94; p = 0.34 |
| Range | 36–85 | – | 36–85 | – | 47–72 | – | |
| Gender | |||||||
| Female | 31 | 58.5 | 12 | 48.0 | 19 | 67.9 | Wald's χ2 = 2.11; p = 0.15 |
| Male | 22 | 41.5 | 13 | 52.0 | 9 | 32.1 | |
| Marital status | |||||||
| Single/never married | 6 | 11.3 | 2 | 8.0 | 4 | 14.3 | Wald's χ2 = 0.69; p = 0.71 |
| Married/common law | 42 | 79.2 | 21 | 84.0 | 21 | 75.0 | |
| Separated/divorced/widowed | 5 | 9.4 | 2 | 8.0 | 3 | 10.7 | |
| Children | |||||||
| Yes | 46 | 86.8 | 23 | 92.0 | 23 | 82.1 | Wald's χ2 = 1.07; p = 0.30 |
| No | 7 | 13.2 | 2 | 8.0 | 5 | 17.9 | |
| Education | |||||||
| Less than high school | 4 | 7.5 | 4 | 16.0 | 0 | – | Wald's χ2 = 0.25; p = 0.97 |
| High school diploma | 8 | 15.1 | 4 | 16.0 | 4 | 14.3 | |
| Post high school certificate/diploma | 16 | 30.2 | 7 | 28.0 | 9 | 32.1 | |
| University education | 25 | 47.2 | 10 | 40.0 | 15 | 53.6 | |
| Employment status | |||||||
| Employed part-time/full time | 27 | 50.9 | 14 | 56.0 | 13 | 46.4 | Wald's χ2 = 1.36; p = 0.71 |
| Unemployed | 3 | 5.7 | 2 | 8.0 | 1 | 3.6 | |
| Homemaker | 2 | 3.8 | 1 | 4.0 | 1 | 3.6 | |
| Student, retired, or disability | 21 | 39.6 | 8 | 32.0 | 13 | 46.4 | |
| Ethnicity | |||||||
| Caucasian | 50 | 94.3 | 23 | 92.0 | 27 | 96.4 | Wald's χ2 = 0.01; p = 0.99 |
| Indigenous | 1 | 1.9 | 1 | 4.0 | 0 | – | |
| Other | 2 | 3.8 | 1 | 4.0 | 1 | 3.6 | |
| Location | |||||||
| Large city (over 200,000) | 23 | 43.4 | 9 | 36.0 | 14 | 50.0 | Wald's χ2 = 2.10; p = 0.35 |
| Small city | 12 | 22.6 | 5 | 20.0 | 7 | 25.0 | |
| Small rural location | 18 | 34.0 | 11 | 44.0 | 7 | 25.0 | |
| Physical health characteristics | |||||||
| Cardiac condition | |||||||
| Myocardial infarction | 39 | 73.6 | 19 | 76.0 | 20 | 71.4 | Wald's χ2 = 0.14; p = 0.71 |
| Unstable angina | 14 | 26.4 | 6 | 24.0 | 8 | 28.6 | |
| Months since acute coronary event | |||||||
| Mean | 5.58 (6.87) | – | 5.36 (6.89) | – | 5.79 (6.97) | – | Wald's χ2 = 0.05; p = 0.82 |
| Range | <1–23 | – | <1–23 | – | <1–23 | – | |
| Cardiac rehabilitation | |||||||
| Currently attending | 29 | 54.7 | 10 | 40.0 | 19 | 67.9 | Wald's χ2 = 4.02; p = 0.05 |
| Attended in past | 18 | 34.0 | 7 | 28.0 | 11 | 39.3 | Wald's χ2 = 0.75; p = 0.39 |
| Psychological component included in rehab | 5 | 9.4 | 2 | 8.0 | 3 | 10.7 | Wald's χ2 = 0.11; p = 0.74 |
| Mental health characteristics | |||||||
| Sought some form of mental health treatment in the past | 22 | 41.5 | 10 | 40.0 | 12 | 42.9 | Wald's χ2 = 0.04; p = 0.83 |
| Infrequent use of some form of mental health treatment | 7 | 13.2 | 3 | 12.0 | 4 | 14.3 | Wald's χ2 = 0.06; p = 0.81 |
| Taking psychotropic medications | 10 | 18.9 | 6 | 24.0 | 4 | 14.3 | Wald's χ2 = 0.80; p = 0.37 |
| Pre-treatment GAD-7 ≥ 10 | 24 | 45.3 | 13 | 52.0 | 11 | 39.3 | Wald's χ2 = 0.86; p = 0.36 |
| Pre-treatment PHQ-9 ≥ 10 | 31 | 58.5 | 17 | 68.0 | 14 | 50.0 | Wald's χ2 = 1.74; p = 0.19 |
| Above clinical cut-off on GAD-7 or PHQ-9 | 33 | 62.3 | 19 | 76.0 | 14 | 50.0 | Wald's χ2 = 3.67; p = 0.06 |
Note. GAD-7 = Generalized Anxiety Disorder 7-item scale; PHQ-9 = Patient Health Questionnaire 9-item scale.
3.2. Primary measures
The means, standard deviations, percentage reductions, and Cohen's d effect sizes for the primary measures are presented in Table 2.
Table 2.
Means, standard deviations, and effect sizes (Cohen's d) for primary and secondary outcomes by group.
| Estimated marginal means |
Percentage changes from pre-treatment |
Within-group effect sizes from pre-treatment |
Between-group effect size |
|||||
|---|---|---|---|---|---|---|---|---|
| Pre-treatment | Post-treatment | 4-Week follow-up | To post-treatment | To 4-week follow-up | To post-treatment | To 4-week follow-up | At post-treatment | |
| Primary outcomes | ||||||||
| GAD-7 | ||||||||
| ICBT | 9.76 (4.48) | 3.23 (2.77) | 2.87 (1.99) | 67 [52,77] | 71 [60,78] | 1.75 [1.10,2.41] | 1.98 [1.31,2.66] | 1.62 [1.00,2.24] |
| WLC | 8.75 (4.09) | 9.02 (4.15) | – | -3 [−24,15] | – | −0.06 [−0.59,0.46] | – | |
| GLTEQ | ||||||||
| ICBT | 20.08 (17.98) | 34.13 (20.48) | 49.59 (26.06) | 70 [25,115] | 147 [90,204] | 0.73 [0.16,1.30] | 1.32 [0.71,1.93] | 0.27 [−0.27,0.81] |
| WLC | 30.11 (16.70) | 29.58 (13.24) | – | −2 [−20,16] | – | −0.04 [−0.56,0.49] | – | |
| PHQ-9 | ||||||||
| ICBT | 11.00 (4.11) | 4.32 (2.45) | 4.00 (2.29) | 61 [50,69] | 64 [53,72] | 1.97 [1.30,2.65] | 2.10 [1.41,2.79] | 1.09 [0.51,1.66] |
| WLC | 9.18 (4.99) | 8.72 (5.07) | – | 5 [−21,25] | – | 0.09 [−0.43,0.61] | – | |
| Secondary outcomes | ||||||||
| CAQ-Total | ||||||||
| ICBT | 1.73 (0.51) | 1.14 (0.44) | 0.80 (0.45) | 34 [22,44] | 54 [41,64] | 1.24 [0.63,1.84] | 1.94 [1.26,2.61] | 0.92 [0.36,1.49] |
| WLC | 1.79 (0.51) | 1.64 (0.61) | – | 9 [−6,22] | – | 0.29 [−0.24,0.81] | – | |
| CAQ-Attention | ||||||||
| ICBT | 1.34 (0.67) | 0.91 (0.62) | 0.55 (0.57) | 32 [8,50] | 59 [35,74] | 0.66 [0.10,1.23] | 1.26 [0.65,1.87] | 0.95 [0.38,1.51] |
| WLC | 1.73 (0.66) | 1.51 (0.65) | – | 13 [−4,27] | – | 0.33 [−0.19,0.86] | – | |
| CAQ-Avoidance | ||||||||
| ICBT | 2.10 (0.83) | 1.42 (0.68) | 1.12 (0.84) | 33 [17,45] | 47 [26,62] | 0.90 [0.32,1.48] | 1.18 [0.57,1.78] | 0.28 [−0.27,0.82] |
| WLC | 1.56 (0.75) | 1.60 (0.63) | – | −2 [−20,13] | – | −0.05 [−0.58,0.47] | – | |
| CAQ-Fear | ||||||||
| ICBT | 1.76 (0.57) | 1.12 (0.56) | 0.75 (0.47) | 36 [21,49] | 58 [44,68] | 1.12 [0.53,1.72] | 1.93 [1.26,2.60] | 0.94 [0.37,1.51] |
| WLC | 1.98 (0.55) | 1.74 (0.73) | – | 12 [−4,26] | – | 0.38 [−0.15,0.90] | – | |
| DASS-21-Total | ||||||||
| ICBT | 22.60 (8.10) | 11.03 (5.22) | 9.40 (5.32) | 51 [41,61] | 58 [48,69] | 1.70 [1.05,2.35] | 1.93 [1.26,2.60] | 0.98 [0.41,1.55] |
| WLC | 20.22 (9.43) | 18.03 (8.53) | – | 11 [−6,28] | – | 0.24 [−0.28,0.77] | – | |
| DASS-21-Depression | ||||||||
| ICBT | 7.36 (3.67) | 3.45 (2.47) | 2.77 (2.46) | 53 [36,66] | 62 [44,74] | 1.25 [0.64,1.86] | 1.47 [0.84,2.09] | 0.55 [0.00,1.10] |
| WLC | 5.97 (4.11) | 5.39 (4.22) | – | 10[−24,34] | – | 0.14 [−0.39,0.66] | – | |
| DASS-21-Anxiety | ||||||||
| ICBT | 7.00 (3.76) | 3.36 (2.14) | 2.72 (2.22) | 52 [37,64] | 61 [45,73] | 1.19 [0.59,1.79] | 1.39 [0.77,2.01] | 0.67 [0.12,1.23] |
| WLC | 6.43 (3.43) | 5.10 (2.91) | – | 21 [0,37] | – | 0.42 [−0.11,0.95] | – | |
| DASS-21-Stress | ||||||||
| ICBT | 8.24 (3.36) | 4.20 (2.37) | 4.01 (2.42) | 49 [36,62] | 51 [38,64] | 1.39 [0.77,2.01] | 1.44 [0.82,2.07] | 1.26 [0.67,1.85] |
| WLC | 7.82 (3.30) | 7.53 (2.87) | – | 4 [−11,19] | – | 0.09 [−0.43,0.62] | – | |
| SF-12-Mental | ||||||||
| ICBT | 38.06 (6.19) | 47.34 (8.27) | – | 24 [15,34] | – | 1.27 [0.66,1.88] | – | 0.23 [−0.33,0.79] |
| WLC | 42.24 (8.98) | 45.41 (8.46) | – | 8 [−1,16] | – | 0.36 [−0.18,0.91] | – | |
| SF-12-Physical | ||||||||
| ICBT | 39.44 (8.62) | 44.95 (7.98) | – | 14 [5,23] | – | 0.66 [0.09,1.23] | – | −0.17 [−0.73,0.39] |
| WLC | 43.66 (8.34) | 46.20 (6.66) | – | 6 [−1,13] | – | 0.33 [−0.21,0.88] | – | |
Note. CAQ = Cardiac Anxiety Questionnaire; DASS-21 = Depression, Anxiety, and Stress 21-item Scale; GAD-7 = Generalized Anxiety Disorder 7-item scale; GLTEQ = Godin Leisure-Time Exercise Questionnaire; PHQ-9 = Patient Health Questionnaire 9-item scale; SF-12 = Short Form 12-item Health Survey; ICBT = Internet-delivered cognitive behavioural therapy; WLC = waiting-list control. Standard deviations are shown in rounded parentheses for the estimated means; 95% confidence intervals are shown in square parentheses for the percentage changes and effect sizes.
3.2.1. General anxiety
The GEE analyses revealed a statistically significant Time effect (Wald's χ2 = 51.46, p < 0.001) and a statistically significant Time by Group interaction (Wald's χ2 = 27.49, p < 0.001) for symptoms of general anxiety. Planned contrasts revealed statistically significant reductions from pre-to post-treatment among the treatment group but not for the control group (p < 0.001, p = 0.71; respectively). Differences between post-treatment and four-week follow-up scores for the treatment group were statistically non-significant (p = 0.50), indicating maintenance of treatment gains.
3.2.2. Depression
The GEE analyses revealed a statistically significant Time effect (Wald's χ2 = 56.13, p < 0.001) and statistically significant Time by Group interaction (Wald's χ2 = 28.20, p < 0.001) for symptoms of depression. Planned contrasts revealed statistically significant reductions from pre-to post-treatment among the treatment group but not for the control group (p < 0.001, p = 0.57; respectively). Differences between post-treatment and four-week follow-up scores for the treatment group were statistically non-significant (p = 0.55), indicating maintenance of treatment gains.
3.2.3. Physical activity
The GEE analyses revealed a statistically significant Time effect (Wald's χ2 = 25.56, p < 0.001) and statistically significant Time by Group interaction (Wald's χ2 = 7.21, p = 0.01) for physical activity levels. Planned contrasts revealed statistically significant reductions from pre-to post-treatment among the treatment group but not for the control group (p < 0.01, p = 0.86; respectively). A statistically significant difference was observed among the treatment group between post-treatment and four-week follow-up (p = 0.01), indicating further symptom reductions.
3.3. Secondary measures
The means, standard deviations, percentage reductions, and Cohen's d effect sizes for the secondary measures are presented in Table 2.
3.3.1. Distress
GEE analyses revealed statistically significant Time effects for distress (i.e., DASS-21-total score; Wald's χ2 = 54.79, p < 0.001) and statistically significant Time by Group interactions were also observed (Wald's χ2 = 16.65, p < 0.001). Similar results were observed for the subscales of the distress measure, the details of which appear in Table 2. Planned contrasts revealed statistically significant pre-to post-treatment reductions for the treatment group for distress but not for the control group (p < 0.001, p = 0.16; respectively). Notably, there was a shift in scores among participants in the waiting-list control group indicating some improvement in scores for the anxiety subscale of the distress measure (p = 0.01). At four-week follow-up, statistically significant differences were observed from post-treatment for distress (p = 0.03), indicating further symptom reductions.
3.3.2. Cardiac anxiety
Statistically significant Time effects were observed for overall cardiac anxiety (i.e., CAQ-total score; Wald's χ2 = 36.76, p < 0.001) as well as the attention subscale (Wald's χ2 = 21.83, p < 0.001), avoidance subscale (Wald's χ2 = 13.83, p = 0.001), and fear subscale (Wald's χ2 = 42.29, p < 0.001). Statistically significant Time by Group interactions were observed for overall cardiac anxiety (Wald's χ2 = 7.78, p = 0.01), the avoidance subscale (Wald's χ2 = 7.62, p = 0.01), and fear subscale (Wald's χ2 = 6.88, p = 0.01). Time by Group interactions were statistically non-significant for the attention subscale of the cardiac anxiety measure (Wald's χ2 = 2.42, p = 0.12). Planned contrasts revealed statistically significant reductions from pre-to post-treatment for overall cardiac anxiety, the fear subscale, and avoidance subscale for the treatment group but not for the control group (all Ps < .001, p range: 0.07 to 0.83; respectively). At four-week follow-up, statistically significant differences were observed from post-treatment for overall cardiac anxiety (p < 0.001), the fear subscale (p = 0.001), and avoidance subscale (p = 0.01), indicating further symptom reductions.
3.3.3. Quality of life
Statistically significant Time effects were observed for mental health quality of life (Wald's χ2 = 21.75, p < 0.001), and physical health quality of life (Wald's χ2 = 11.10, p = 0.001). Statistically significant Time by Group interactions were observed for mental health quality of life (Wald's χ2 = 5.23, p = 0.02) but were statistically non-significant for physical health quality of life (Wald's χ2 = 1.51, p = 0.22). Planned contrasts revealed statistically significant reductions for mental health quality of life from pre-to post-treatment among the treatment group but not for the control group (p < 0.001, p = 0.07; respectively).
3.4. Clinical significance
Percentage change as well as within- and between-group effect sizes from the GEE models are shown in Table 2. For the treatment group, significant percentage improvements were observed for the primary and secondary measures from pre- to post-treatment (range: 61% to 70% and 14% to 53%, respectively) compared to very minimal percentage improvements for the waiting-list control group (range: −3% to 5% and −2% to 13%, respectively) from pre- to post-treatment, with the exception of the anxiety subscale of the distress measure (21% change). For the treatment group relative to the waiting-list control group at post-treatment, large between-group effect sizes (Cohen's d) were observed for the measures of general anxiety, depression, distress, the stress subscale of the distress measure, overall cardiac anxiety, the attention subscale of the cardiac anxiety measure, and the fear subscale of the cardiac anxiety measure (d range: 0.92 to 1.62). Medium between-group effect sizes were observed for the depression subscale of the distress measure and the anxiety subscale of the distress measure (d range: 0.55 to 0.67). Small between-groups effect sizes were observed for physical activity, the avoidance subscale of the cardiac anxiety measure, mental health quality of life, and physical health quality of life (d range: −0.17 to 0.28).
A test of clinically meaningful change observed for the primary measures of general anxiety and depression is presented in Table 3 which lists the proportions of participants who demonstrated reliable improvement and reliable recovery. Of participants who scored above clinical cut-offs at pre-treatment on the general anxiety (45%; n = 24) or depression measures (59%; n = 31), a majority of participants in the intervention group demonstrated reliable improvement and recovery on both measures at post-treatment (range: 77% to 85% and 71%, respectively) compared to a minority of participants in the waiting-list control group (range: 18% and 7% to 21%, respectively). Chi-square analyses indicated that a greater proportion of reliable improvement and reliable recovery occurred for treatment group participants compared to participants in the waiting-list control group (p range: < 0.001 to 0.01).
Table 3.
Proportions of participants who demonstrated reliable improvement and reliable recovery.
| Post-treatment |
Four-week Follow-up |
|||||
|---|---|---|---|---|---|---|
| Reliable improvement | Statistical significance | Reliable recovery | Statistical significance | Reliable improvement | Reliable recovery | |
| GAD-7 | ||||||
| ICBT | 11/13 (85%) | χ2 = 10.59; p = 0.001 | 10/13 (77%) | χ2 = 8.22; p < 0.01 | 10/13 (77%) | 10/13 (77%) |
| WLC | 2/11 (18%) | 2/11 (18%) | – | – | ||
| PHQ-9 | ||||||
| ICBT | 12/17 (71%) | χ2 = 7.43; p = 0.01 | 12/17 (71%) | χ2 = 12.69; p < 0.001 | 13/17 (76%) | 13/17 (76%) |
| WLC | 3/14 (21%) | 1/14 (7%) | – | – | ||
Note. GAD-7 = Generalized Anxiety Disorder 7-item scale; ICBT = Internet-delivered cognitive behavioural therapy; PHQ-9 = Patient Health Questionnaire 9-item scale; WLC = waiting-list control.
3.5. Intervention use and completion rates
Participants who received the intervention (n = 25) accessed the course for an average of 93.36 (SD = 38.81) days and logged in an average of 26.36 (SD = 16.55) times. During the intervention, participants sent an average of 2.92 (SD = 2.58) messages to their guide and received an average of 5.60 (SD = 3.04) messages and 4.80 (SD = 3.06) phone calls from their guide. A majority of participants completed at least four lessons of the course (n = 23; 92%) and also completed post-treatment and follow-up questionnaires (n = 22; 88%).
3.6. Treatment satisfaction and negative effects
Of the participants who completed satisfaction measures at post-treatment (n = 22), a majority of participants also indicated that the course was worth their time (n = 21; 95%) and that they would recommend the course to others (n = 22; 100%). Of the participants who completed the negative effects questionnaire (n = 22), the majority reported no unwanted negative effects related to treatment (n = 19; 86%). Reported negative effects included experiencing a temporary increase in symptoms (n = 2) and experiencing discomfort in addressing symptoms which would otherwise be avoided (n = 1). Participants who experienced a negative effect rated its impact as either minimal (n = 1) or moderate (n = 2).
4. Discussion
Using an RCT design, this study sought to contribute to the literature by drawing upon a previously established transdiagnostic ICBT protocol to create and evaluate an ICBT program (Cardiac Wellbeing Course) for Canadians who recently experienced an ACE. It improved on past studies in this area by including broad measures of anxiety, depression, and distress while also including measures relevant to a cardiac population (e.g., cardiac anxiety, physical activity levels). It was hypothesized that improvements in general anxiety, depression, physical activity, distress, cardiac activity, and quality of life would be observed among intervention participants relative to the control group and that participants who received the intervention would report high satisfaction rates and limited negative effects as a result of taking the intervention. These hypotheses were largely supported.
Large between-group effect sizes were observed for intervention participants in the primary measures of depression and anxiety (d range: 1.62 to 1.09) and a statistically significant proportion of intervention participants who were within clinical ranges of depression and anxiety at pre-treatment demonstrated reliable improvement and reliable recovery compared to the control group (71% to 85% vs. 7% to 21%, respectively). These improvements are similar to past studies of the Wellbeing Course in the general population, both in Canada and Australia (Hadjistavropoulos et al., 2016; Titov et al., 2017). The outcomes of this study are also in-line with the positive results reported in meta-analytic studies of ICBT for anxiety and depression (Andrews et al., 2018; Arnberg et al., 2014; Hedman et al., 2012) and for ICBT programs targeting somatic conditions (Mehta et al., 2018; van Beugen et al., 2014).
The results of this study also join other studies which support ICBT as an effective treatment option in cardiac populations (Glozier et al., 2013; Johansson et al., 2019). Importantly, the findings of this study stand in contrast to the results reported by Norlund et al. (2018), who reported statistically non-significant findings for depression, general anxiety, and cardiac anxiety in a large trial comparing ICBT to a control group. These differences may be attributable to high adherence rates and the use of a previously-validated ICBT protocol and delivery platform in this study (compared to a relatively new intervention protocol; Norlund et al., 2018). However, it is possible that a larger-scale implementation of the Cardiac Wellbeing Course in a routine care setting may face similar problems.
Among the cardiac-specific ICBT literature, this was the first study to demonstrate small but potentially important improvements in physical activity among participants (i.e., GLTEQ; d = 0.27). Glozier et al. (2013) observed post-intervention improvements in walking time among intervention participants, however, statistically similar improvements were observed among control group participants. Generally speaking, improvements in physical activity are often associated with improvements in mental health (Rosenbaum et al., 2014). The opposite is also true, especially for people with chronic health conditions (O'Halloran et al., 2014). The results obtained in this study are encouraging and raises questions regarding the potential of the Cardiac Wellbeing Course to be used as an adjunct to cardiac rehabilitation in order to increase physical activity.
Statistically significant Time by Group interactions and large between-group effect sizes in favour of intervention participants were observed for overall cardiac anxiety (d = 0.92), which supported its corresponding hypothesis. Although the majority of measures exhibited between-group change, the attention subscale of the cardiac anxiety measure did not demonstrate statistically significant differences between groups. The attention subscale of the cardiac anxiety measure is conceptually the least related to maladaptive behaviours among participants, as it assesses monitoring of cardiac activity (Eifert et al., 2000). It is possible that participants in both groups paid substantial attention to their heart, given that they recently experienced a cardiac event and may still have been experiencing cardiac symptoms. Importantly, an overall reduction in symptoms was observed for overall cardiac anxiety among intervention participants and the other two subscales of this measure demonstrated statistically significant change, indicating that participants increased activities believed to elicit cardiac symptoms (i.e., avoidance subscale) and decreased fear and worry related to chest and heart sensations (i.e., fear subscale).
Small between-group effect sizes in favour of the treatment group were observed for a measure of mental health quality of life (i.e., SF-12; d = 0.23). However, statistically significant differences between groups were not observed for physical health quality of life. This result is similar to the finding reported by Johansson et al. (2019) and may be expected given that the focus of the intervention was to improve mental health outcomes and did not have a physical activity promotion component. It is also similar to other studies where mental-health-focused programs have been modified for somatic populations (Chan et al., 2016) without the addition of skills (e.g., activity pacing, graded exposure to physical activity) to target modifiable physical disability and increase activities of living, which are often covered in psychological programs for somatic conditions in the context of rehabilitation. Such skills are covered in emerging ICBT programs designed specifically for people with somatic conditions with the goals of reducing the impact of those conditions on peoples' mental health and physical functioning (Dear et al., 2018; Gandy et al., 2016; Mehta et al., 2020). However, there is a need for more research, and it remains an important question whether ICBT programs can support people to minimize functional disability and improve activities of daily living in the context of somatic conditions. On this front, it is encouraging that small improvements were observed for physical activity levels, which could indicate that the measure used was more sensitive to activity-level changes compared to items on the physical health quality of life measure, which is a more global measure of impact and simply assesses whether a person's health has interfered with activities in general (e.g., yes/no).
In addition to symptom measures, it was hypothesized that participants would report high satisfaction rates with the intervention and that a low number of participants would report negative effects as a result of the intervention. These hypotheses were supported, with 95% of participants who received the intervention agreeing that the course was worth their time and 100% reporting feeling confident recommending the course to a friend. The satisfaction ratings observed in this study are directly comparable to past studies of the Wellbeing Course in both Canadian and Australian studies (e.g., Hadjistavropoulos et al., 2016; Titov et al., 2017). The comparatively high satisfaction rates observed in this study and other investigations of the Wellbeing Course speaks to the benefit of building upon a previously validated ICBT protocol and delivery platform, which is likely to have already addressed many issues related to participant satisfaction (e.g., website navigation, readability and layout of material).
Although the results of the present study are encouraging, there are several limitations which should be noted. First, this study did not use an active control group (e.g., online discussion forum), which future researchers will need to further examine. Given the preliminary nature of the study and resource restrictions, an active control group was not used. Second, there was difficulty recruiting participants despite notable effort, similar to difficulties reported by Lundgren et al. (2016) and Norlund et al. (2018). Potential reasons for the lack of enrolled participants may be the novelty of treatment, stigma, low motivation as a symptom of depression, or avoidance as a symptom of anxiety. On the other hand, a large number of participants applied for the course but did not meet the two-year cardiac event inclusion criteria, which may indicate that extending the cardiac timeline may increase the number of participants. Third, although the majority of participants had scores in the clinical range, symptom minimums were not a requirement for participation in this study and the inclusion of people below clinical thresholds of depression and/or general anxiety may have weakened the results and limited generalizability among clinical settings. Fourth, participants were not followed up for a longer period, which occurred due to limitations in study resources. A longer-term follow-up as observed in other studies (e.g., four months or greater) would assist in assessing the lasting effects of the Cardiac Wellbeing Course. Fifth, participants may have also demonstrated symptom reductions due to concurrent participation in a cardiac rehabilitation program (55% of the overall sample), which made it difficult to isolate the effect of the intervention, although it should be noted that improvements were not observed in the control group, who also received concurrent cardiac rehabilitation. Sixth, with the exception of one participant, the primary researcher acted as the sole guide for participants in this study. Having a limited number of support personnel may limit the generalizability of the findings, especially in settings with multiple clinicians of various therapeutic backgrounds.
There are several strengths of the current study. This study addresses a gap in the literature by modifying and evaluating a transdiagnostic ICBT program specifically designed to reduce both depression and anxiety symptoms among people with CVD who experienced an ACE. This study addresses an important limitation in the literature by utilizing an online program and support model which has been proven effective in other populations. A specific set of symptoms (i.e., depression and/or anxiety) and CVD conditions (i.e., myocardial infarction or unstable angina) was defined which addresses the limitation of unclear symptom targets and CVD heterogeneity observed in past research. This study is one of the first to examine ICBT in a cardiac population with a focus on improving psychological health related to an ACE. Additionally, the RCT design and GEE analyses used in this study was a scientifically robust methodology which allowed comparison between the treatment and control groups. Generally, there was a small amount of missing data (9% overall) which aided the analyses. This study examined treatment effects at post-treatment and at four-week follow-up, which provided important information about the robustness of treatment gains observed among participants. Finally, this study incorporated outcome measures used in past ICBT research (e.g., general anxiety, depression) while also using measures common among cardiac populations (e.g., cardiac anxiety, quality of life), which will contribute to both cardiac and ICBT research areas.
5. Conclusions
Relative to a control group, statistically significant changes in the domains of general anxiety, depression, physical activity, distress, cardiac anxiety, and mental health quality of life were observed for participants who received the Cardiac Wellbeing Course. The encouraging results obtained in this study represent a crucial first step in evaluating the uptake and preliminary efficacy of the Cardiac Wellbeing Course. Future research trials conducted in healthcare settings (e.g., cardiac rehabilitation units) offered with guidance from diverse support personnel (e.g., nurses) should be conducted in order to more accurately gauge the broader efficacy of the Cardiac Wellbeing Course and generalizability of results.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This work was supported by funding provided by the Canadian Institutes of Health Research (reference number 293379), Saskatchewan Health Research Foundation, and Rx & D Health Research Foundation. Funders had no involvement in the study design, collection, analysis, or interpretation of the data. The authors would like to acknowledge research staff, therapists, and patients associated with the Online Therapy Unit for Service, Education, and Research, at the University of Regina.
Footnotes
Two supplementary measures (i.e., computer self-efficacy and qualitative interviews) were administered to participants but are omitted from this manuscript for brevity. These measures were not imperative to the primary outcomes or purpose of this study.
Contributor Information
L.H. Schneider, Email: luke.schneider@uregina.ca.
H.D. Hadjistavropoulos, Email: hadjista@uregina.ca.
B.F. Dear, Email: blake.dear@mq.edu.au.
N. Titov, Email: nick.titov@mq.edu.au.
References
- Amireault S., Godin G. The Godin-Shephard leisure-time physical activity questionnaire: validity evidence supporting its use for classifying healthy adults into active and insufficiently active categories. Percept. Mot. Skills. 2015;120(2):604–622. doi: 10.2466/03.27.PMS.120v19x7. [DOI] [PubMed] [Google Scholar]
- Andersson G., Titov N. Advantages and limitations of internet-based interventions for common mental disorders. World Psychiatry. 2014;13(1):4–11. doi: 10.1002/wps.20083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson G., Carlbring P., Titov N., Lindefors N. Internet interventions for adults with anxiety and mood disorders: a narrative umbrella review of recent meta-analyses. Can. J. Psychiatr. 2019;64(7):465–470. doi: 10.1177/0706743719839381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews G., Basu A., Cuijpers P., Craske M.G., McEvoy P., English C.L., Newby J.M. Computer therapy for the anxiety and depression disorders is effective, acceptable and practical health care: an updated meta-analysis. Journal of Anxiety Disorders. 2018;55:70–78. doi: 10.1016/j.janxdis.2018.01.001. [DOI] [PubMed] [Google Scholar]
- Arnberg F.K., Linton S.J., Hultcrantz M., Heintz E., Jonsson U. Internet-delivered psychological treatments for mood and anxiety disorders: a systematic review of their efficacy, safety, and cost-effectiveness. PLoS One. 2014;9(5) doi: 10.1371/journal.pone.0098118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Beugen S., Ferwerda M., Hoeve D., Rovers M.M., Spillekom-van Koulil S., van Middendorp H., Evers A.W. Internet-based cognitive behavioral therapy for patients with chronic somatic conditions: a meta-analytic review. J. Med. Internet Res. 2014;16(3):e88. doi: 10.2196/jmir.2777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenthal J.A., Sherwood A., Smith P.J., Watkins L., Mabe S., Kraus W.E., Ingle K., Miller P., Hinderliter A. Enhancing cardiac rehabilitation with stress management training: a randomized, clinical efficacy trial. Circulation. 2016;133(14):1341–1350. doi: 10.1161/circulationaha.115.018926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caulin-Glaser T., Maciejewski P.K., Snow R., LaLonde M., Mazure C. Depressive symptoms and sex affect completion rates and clinical outcomes in cardiac rehabilitation. Preventative Cardiology. 2007;10(1):15–21. doi: 10.1111/j.1520-037.2007.05666.x. [DOI] [PubMed] [Google Scholar]
- Chan R., Dear B.F., Titov N., Chow J., Suranyi M. Examining internet-delivered cognitive behaviour therapy for patients with chronic kidney disease on haemodialysis: a feasibility open trial. J. Psychosom. Res. 2016;89:78–84. doi: 10.1016/j.jpsychores.2016.08.012. [DOI] [PubMed] [Google Scholar]
- Compare A., Germani E., Proietti R., Janeway D. Clinical psychology and cardiovascular disease: an up-to-date clinical practice review for assessment and treatment of anxiety and depression. Clin. Pract. Epidemiol. Ment. Health. 2011;7:148–156. doi: 10.2174/1745017901107010148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford, J. R., & Henry, J. D. (2003). The depression anxiety stress scales (DASS): normative data and latent structure in a large non-clinical sample. Br. J. Clin. Psychol., 42 (Pt 2), 111–131. doi: 10.1348/014466503321903544. [DOI] [PubMed]
- Dear B.F., Gandy M., Karin E., Staples L.G., Johnston L., Fogliati V.J., Wootton B.M., Terides M.D., Kayrouz R., Perry K.N., Sharpe L., Nicholas M.K., Titov N. The pain course: a randomised controlled trial examining an internet-delivered pain management program when provided with different levels of clinician support. Pain. 2015;156(10):1920–1935. doi: 10.1097/j.pain.0000000000000251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dear B.F., Staples L.G., Terides M.D., Karin E., Zou J., Johnston L., Gandy M., Fogliati V.J., Wootton B.M., McEvoy P.M., Titov N. Transdiagnostic versus disorder-specific and clinician-guided versus self-guided internet-delivered treatment for generalized anxiety disorder and comorbid disorders: a randomized controlled trial. Journal of Anxiety Disorders. 2015;36:63–77. doi: 10.1016/j.janxdis.2015.09.003. [DOI] [PubMed] [Google Scholar]
- Dear B.F., Fogliati V.J., Fogliati R., Gandy M., McDonald S., Talley N., Holtmann G., Titov N., Jones M. Transdiagnostic internet-delivered cognitive-behaviour therapy (CBT) for adults with functional gastrointestinal disorders (FGID): a feasibility open trial. J. Psychosom. Res. 2018;108:61–69. doi: 10.1016/j.jpsychores.2018.02.015. [DOI] [PubMed] [Google Scholar]
- Eifert G.H., Thompson R.N., Zvolensky M.J., Edwards K., Frazer N.L., Haddad J.W., Davig J. The cardiac anxiety questionnaire: development and preliminary validity. Behav. Res. Ther. 2000;38(10):1039–1053. doi: 10.1016/S0005-7967(99)00132-1. [DOI] [PubMed] [Google Scholar]
- Gandy M., Karin E., Fogliati V.J., McDonald S., Titov N., Dear B.F. A feasibility trial of an internet-delivered and transdiagnostic cognitive behavioral therapy treatment program for anxiety, depression, and disability among adults with epilepsy. Epilepsia. 2016;57(11):1887–1896. doi: 10.1111/epi.13569. [DOI] [PubMed] [Google Scholar]
- Glozier N., Christensen H., Naismith S., Cockayne N., Donkin L., Neal B., Mackinnon A., Hickie I. Internet-delivered cognitive behavioural therapy for adults with mild to moderate depression and high cardiovascular disease risks: a randomised attention-controlled trial. PLoS One. 2013;8(3) doi: 10.1371/journal.pone.0059139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godin G., Shephard R.J. A simple method to assess exercise behavior in the community. Canadian Journal of Applied Sport Sciences. 1985;10(3):141–146. [PubMed] [Google Scholar]
- Gyani A., Shafran R., Layard R., Clark D.M. Enhancing recovery rates: lessons from year one of IAPT. Behav. Res. Ther. 2013;51(9):597–606. doi: 10.1016/j.brat.2013.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habibovic M., Cuijpers P., Alings M., van der Voort P., Theuns D., Bouwels L., Herrman J.P., Valk S., Pedersen S. Attrition and adherence in a web-based distress management program for implantable cardioverter defibrillator patients (WEBCARE): randomized controlled trial. J. Med. Internet Res. 2014;16(2):e52. doi: 10.2196/jmir.2809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadjistavropoulos H.D., Nugent M.M., Alberts N.M., Staples L., Dear B.F., Titov N. Transdiagnostic internet-delivered cognitive behaviour therapy in Canada: an open trial comparing results of a specialized online clinic and nonspecialized community clinics. Journal of Anxiety Disorders. 2016;42:19–29. doi: 10.1016/j.janxdis.2016.05.006. [DOI] [PubMed] [Google Scholar]
- Hadjistavropoulos H.D., Schneider L.H., Edmonds M., Karin E., Nugent M.N., Dirkse D., Dear B.F., Titov N. Randomized controlled trial of internet-delivered cognitive behaviour therapy comparing standard weekly versus optional weekly therapist support. Journal of Anxiety Disorders. 2017;52:15–24. doi: 10.1016/j.janxdis.2017.09.006. [DOI] [PubMed] [Google Scholar]
- Hardin J.W., Hilbe J.M. 2nd ed. Taylor & Francis; CRC: 2013. Generalized Estimating Equations. [Google Scholar]
- Hedman E., Ljotsson B., Lindefors N. Cognitive behavior therapy via the internet: a systematic review of applications, clinical efficacy and cost-effectiveness. Expert Review of Pharmacoeconomics and Outcomes Research. 2012;12(6):745–764. doi: 10.1586/erp.12.67. [DOI] [PubMed] [Google Scholar]
- Henry J.D., Crawford J.R. The short-form version of the depression anxiety stress scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2005;44:227–239. doi: 10.1348/014466505x29657. [DOI] [PubMed] [Google Scholar]
- Hubbard A.E., Ahern J., Fleischer N.L., Van der Laan M., Lippman S.A., Jewell N., Bruckner T., Satariano W.A. To GEE or not to GEE: comparing population average and mixed models for estimating the associations between neighborhood risk factors and health. Epidemiology. 2010;21(4):467–474. doi: 10.1097/EDE.0b013e3181caeb90. [DOI] [PubMed] [Google Scholar]
- Huether S.E., Mccance K.M. In: Understanding Pathophysiology. 5th ed. Brashers V.L., Rote N.S., editors. Mosby, Inc; 2012. [Google Scholar]
- Jacobson N.S., Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J. Consult. Clin. Psychol. 1991;59(1):12–19. doi: 10.1037/0022-006X.59.1.12. [DOI] [PubMed] [Google Scholar]
- Johansson P., Westas M., Andersson G., Alehagen U., Broström A., Jaarsma T., Mourad G., Lundgren J. An internet-based cognitive behavioral therapy program adapted to patients with cardiovascular disease and depression: randomized controlled trial. JMIR Mental Health. 2019;6(10) doi: 10.2196/14648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J. 2nd ed. Bantam Books; 2013. Full Catastrophe Living: Using the Wisdom of your Body and Mind to Face Stress, Pain, and Illness. [Google Scholar]
- Karin E., Dear B.F., Heller G.Z., Crane M.F., Titov N. “wish you were here”: examining characteristics, outcomes, and statistical solutions for missing cases in web-based psychotherapeutic trials. JMIR Mental Health. 2018;5(2):e22. doi: 10.2196/mental.8363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komasi S., Soroush A., Saeidi M., Brugnera A., Rabboni M., Fulcheri M., Carrozzino D., Marchettini P., Compare A. Subjective correlates of stress management in outpatient cardiac rehabilitation: the predictive role of perceived heart risk factors. Journal of Cardiovascular and Thoracic Research. 2018;10(2):104–108. doi: 10.15171/jcvtr.2018.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B., Lowe B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen. Hosp. Psychiatry. 2010;32(4):345–359. doi: 10.1016/j.genhosppsych.2010.03.006. [DOI] [PubMed] [Google Scholar]
- Kuhl E.A., Sears S.F., Conti J.B. Internet-based behavioral change and psychosocial care for patients with cardiovascular disease: a review of cardiac disease-specific applications. Heart Lung. 2006;35(6):374–382. doi: 10.1016/j.hrtlng.2006.02.004. [DOI] [PubMed] [Google Scholar]
- Lehmann M., Kohlmann S., Gierk B., Murray A.M., Lowe B. Suicidal ideation in patients with coronary heart disease and hypertension: baseline results from the DEPSCREEN-INFO clinical trial. Clinical Psychology & Psychotherapy. 2018;25(6):754–764. doi: 10.1002/cpp.2305. [DOI] [PubMed] [Google Scholar]
- Leon A.S., Franklin B.A., Costa F., Balady G.J., Berra K.A., Stewart K.J., Thompson P.D., Williams M.A., Lauer M.S. Cardiac rehabilitation and secondary prevention of coronary heart disease: an American Heart Association scientific statement from the council on clinical cardiology (subcommittee on exercise, cardiac rehabilitation, and prevention) and the council on nutrition, physical activity, and metabolism (subcommittee on physical activity), in collaboration with the American association of cardiovascular and pulmonary rehabilitation. Circulation. 2005;111(3):369–376. doi: 10.1161/01.cir.0000151788.08740.5c. [DOI] [PubMed] [Google Scholar]
- Linden W., Phillips M.J., Leclerc J. Psychological treatment of cardiac patients: a meta-analysis. Eur. Heart J. 2007;28(24):2972–2984. doi: 10.1093/eurheartj/ehm504. [DOI] [PubMed] [Google Scholar]
- Little T.D., Jorgensen T.D., Lang K.M., Moore E.W. On the joys of missing data. J. Pediatr. Psychol. 2014;39(2):151–162. doi: 10.1093/jpepsy/jst048. [DOI] [PubMed] [Google Scholar]
- Lovibond S.H., Lovibond P.F. 2nd ed. Psychology Foundation of Australia; 1995. Manual for the Depression Anxiety Stress Scales. [Google Scholar]
- Lundgren J., Dahlstrom O., Andersson G., Jaarsma T., Karner Kohler A., Johansson P. The effect of guided web-based cognitive behavioral therapy on patients with depressive symptoms and heart failure: a pilot randomized controlled trial. J. Med. Internet Res. 2016;18(8):e194. doi: 10.2196/jmir.5556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mampuya W.M. Cardiac rehabilitation past, present and future: an overview. Cardiovascular Diagnosis and Therapy. 2012;2(1):38–49. doi: 10.3978/j.issn.2223-3652.2012.01.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McManus D., Pipkin S.S., Whooley M.A. Screening for depression in patients with coronary heart disease (data from the heart and soul study) Am. J. Cardiol. 2005;96(8):1076–1081. doi: 10.1016/j.amjcard.2005.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehra V.M., Gaalema D.E., Pakosh M., Grace S.L. Systematic review of cardiac rehabilitation guidelines: quality and scope. European Journal of Preventative Cardiology. 2019 doi: 10.1177/2047487319878958. 2047487319878958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta S., Peynenburg V.A., Hadjistavropoulos H.D. Internet-delivered cognitive behaviour therapy for chronic health conditions: a systematic review and meta-analysis. J. Behav. Med. 2018 doi: 10.1007/s10865-018-9984-x. [DOI] [PubMed] [Google Scholar]
- Mehta S., Hadjistavropoulos H., Nugent M., Karin E., Titov N., Dear B.F. Guided internet-delivered cognitive-behaviour therapy for persons with spinal cord injury: a feasibility trial. Spinal Cord. 2020 doi: 10.1038/s41393-019-0398-6. [DOI] [PubMed] [Google Scholar]
- Messerli-Burgy N., Barth J., Berger T. The inter Herz project - a web-based psychological treatment for cardiac patients with depression: study protocol of a randomized controlled trial. Trials. 2012;13:245. doi: 10.1186/1745-6215-13-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Müller-Nordhorn J., Roll S., Willich S.N. Comparison of the short form (SF)-12 health status instrument with the SF-36 in patients with coronary heart disease. Heart. 2004;90(5):523–527. doi: 10.1136/hrt.2003.013995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Research Council The prevention and treatment of missing data in clinical trials. 2010. https://www.ncbi.nlm.nih.gov/books/NBK209904/pdf/Bookshelf_NBK209904.pdf [PubMed]
- Norlund F., Olsson E.M., Burell G., Wallin E., Held C. Treatment of depression and anxiety with internet-based cognitive behavior therapy in patients with a recent myocardial infarction (U-CARE heart): study protocol for a randomized controlled trial. Trials. 2015;16:154. doi: 10.1186/s13063-015-0689-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norlund F., Wallin E., Olsson E.M.G., Wallert J., Burell G., von Essen L., Held C. Internet-based cognitive behavioral therapy for symptoms of depression and anxiety among patients with a recent myocardial infarction: the U-CARE heart randomized controlled trial. J. Med. Internet Res. 2018;20(3):e88. doi: 10.2196/jmir.9710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Halloran P.D., Blackstock F., Shields N., Holland A., Iles R., Kingsley M., Bernhardt J., Lannin N., Morris M.E., Taylor N.F. Motivational interviewing to increase physical activity in people with chronic health conditions: a systematic review and meta-analysis. Clin. Rehabil. 2014;28(12):1159–1171. doi: 10.1177/0269215514536210. [DOI] [PubMed] [Google Scholar]
- Osman A., Wong J.L., Bagge C.L., Freedenthal S., Gutierrez P.M., Lozano G. The depression anxiety stress Scales-21 (DASS-21): further examination of dimensions, scale reliability, and correlates. J. Clin. Psychol. 2012;68(12):1322–1338. doi: 10.1002/jclp.21908. [DOI] [PubMed] [Google Scholar]
- Panaite V., Salomon K., Jin A., Rottenberg J. Cardiovascular recovery from psychological and physiological challenge and risk for adverse cardiovascular outcomes and all-cause mortality. Psychosom. Med. 2015;77(3):215–226. doi: 10.1097/PSY.0000000000000171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasarelu C.R., Andersson G., Bergman Nordgren L., Dobrean A. Internet-delivered transdiagnostic and tailored cognitive behavioral therapy for anxiety and depression: a systematic review and meta-analysis of randomized controlled trials. Cogn. Behav. Ther. 2017;46(1):1–28. doi: 10.1080/16506073.2016.1231219. [DOI] [PubMed] [Google Scholar]
- Public Health Agency of Canada Heart Disease in Canada. 2018. https://www.canada.ca/content/dam/phac-aspc/documents/services/publications/diseases-conditions/report-heart-disease-canada-2018/pub1-eng.pdf
- Reavell J., Hopkinson M., Clarkesmith D., Lane D.A. Effectiveness of cognitive behavioral therapy for depression and anxiety in patients with cardiovascular disease: a systematic review and meta-analysis. Psychosom. Med. 2018;80(8):742–753. doi: 10.1097/psy.0000000000000626. [DOI] [PubMed] [Google Scholar]
- Reinholt N., Krogh J. Efficacy of transdiagnostic cognitive behaviour therapy for anxiety disorders: a systematic review and meta-analysis of published outcome studies. Cogn. Behav. Ther. 2014;43(3):171–184. doi: 10.1080/16506073.2014.897367. [DOI] [PubMed] [Google Scholar]
- Richards D.A., Borglin G. Implementation of psychological therapies for anxiety and depression in routine practice: two year prospective cohort study. J. Affect. Disord. 2011;133(1–2):51–60. doi: 10.1016/j.jad.2011.03.024. [DOI] [PubMed] [Google Scholar]
- Richards S.H., Anderson L., Jenkinson C.E., Whalley B., Rees K., Davies P., Bennett P., Liu Z., West R., Thompson D.R., Taylor R.S. Psychological interventions for coronary heart disease. Cochrane Database Syst. Rev. 2017;4:Cd002902. doi: 10.1002/14651858.CD002902.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers W.M., Murray T.C., Selzler A.M., Norman P. Development and impact of exercise self-efficacy types during and after cardiac rehabilitation. Rehabilitation Psychology. 2013;58(2):178–184. doi: 10.1037/a0032018. [DOI] [PubMed] [Google Scholar]
- Rosenbaum S., Tiedemann A., Sherrington C., Curtis J., Ward P.B. Physical activity interventions for people with mental illness: a systematic review and meta-analysis. J. Clin. Psychiatry. 2014;75(9):964–974. doi: 10.4088/JCP.13r08765. [DOI] [PubMed] [Google Scholar]
- Rozental A., Andersson G., Boettcher J., Ebert D.D., Cuijpers P., Knaevelsrud C., Ljótsson B., Kaldo V., Titov N., Carlbring P. Consensus statement on defining and measuring negative effects of internet interventions. Internet Interv. 2014;1(1):12–19. doi: 10.1016/j.invent.2014.02.001. [DOI] [Google Scholar]
- Sikes E.M., Richardson E.V., Cederberg K.J., Sasaki J.E., Sandroff B.M., Motl R.W. Use of the Godin leisure-time exercise questionnaire in multiple sclerosis research: a comprehensive narrative review. Disabil. Rehabil. 2018:1–25. doi: 10.1080/09638288.2018.1424956. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stafford L., Berk M., Jackson H.J. Validity of the hospital anxiety and depression scale and patient health Questionnaire-9 to screen for depression in patients with coronary artery disease. Gen. Hosp. Psychiatry. 2007;29(5):417–424. doi: 10.1016/j.genhosppsych.2007.06.005. [DOI] [PubMed] [Google Scholar]
- Titov N., Dear B.F., Schwencke G., Andrews G., Johnston L., Craske M.G., McEvoy P. Transdiagnostic internet treatment for anxiety and depression: a randomised controlled trial. Behav. Res. Ther. 2011;49(8):441–452. doi: 10.1016/j.brat.2011.03.007. [DOI] [PubMed] [Google Scholar]
- Titov N., Dear B.F., Staples L.G., Terides M.D., Karin E., Sheehan J., Johnston L., Gandy M., Fogliati V.J., Wootton B.M., McEvoy P.M. Disorder-specific versus transdiagnostic and clinician-guided versus self-guided treatment for major depressive disorder and comorbid anxiety disorders: a randomized controlled trial. Journal of Anxiety Disorders. 2015;35:88–102. doi: 10.1016/j.janxdis.2015.08.002. [DOI] [PubMed] [Google Scholar]
- Titov N., Dear B.F., Staples L.G., Bennett-Levy J., Klein B., Rapee R.M., Andersson G., Purtell C., Bezuidenhout G., Nielssen O.B. The first 30 months of the MindSpot clinic: evaluation of a national e-mental health service against project objectives. Australian and New Zeland Journal of Psychiatry. 2017;51(12):1227–1239. doi: 10.1177/0004867416671598. [DOI] [PubMed] [Google Scholar]
- Tokgözoðlu L., Okutucu S., Kaya E.B., Erol Ç., Ergene O. Physical inactivity and low quality of life of Turkish women after hospitalization for coronary heart disease: inferences from EUROASPIRE III. Archives of the Turkish Society of Cardiology. 2016;44(6):488–497. doi: 10.5543/tkda.2016.30788. [DOI] [PubMed] [Google Scholar]
- Ware J., Jr., Kosinski M., Keller S.D. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med. Care. 1996;34(3):220–233. doi: 10.2307/3766749. [DOI] [PubMed] [Google Scholar]