Abstract
Lung ultrasound (LUS) is a point-of-care ultrasound technique used for its portability, widespread availability, and ability to provide real-time diagnostic information and procedural guidance. LUS outperforms lung auscultation and chest X-ray, and it is an alternative to chest computed tomography in selected cases. Cardiologists may enhance their physical and echocardiographic examination with the addition of LUS. We present a practical guide to LUS, including device selection, scanning, findings, and interpretation. We outline a 3-point scanning protocol using 2-dimensional and M-mode imaging to evaluate the pleural line, pleural space, and parenchyma. We describe LUS findings and interpretation for common causes of respiratory failure. We provide guidance specific of COVID-19, which at the time of writing is a global pandemic. In this context, LUS emerges as a particularly useful tool for the diagnosis and management of patients with cardiopulmonary disease.
Résumé
L’échographie pulmonaire (EP) est une technique par ultrasons au chevet du patient utilisé en raison de sa portabilité, de sa grande accessibilité et de sa capacité à fournir des données de diagnostic en temps réel et d'orienter les interventions. L’EP, qui surpasse l’auscultation des poumons et la radiographie pulmonaire, est une solution de rechange à la tomodensitométrie thoracique dans certains cas. L’utilisation de l’EP permet aux cardiologues de parfaire leurs examens physique et échocardiographique. Nous présentons un guide pratique de l’EP, qui porte notamment sur le choix de l’appareil, le balayage, les résultats et l’interprétation. Nous dressons les grandes lignes sur le protocole de balayage en 3 points au moyen de l’imagerie en 2 dimensions et en mode M pour évaluer la ligne pleurale, l’espace pleural et le parenchyme. Nous décrivons les résultats et l’interprétation de l’EP sur les causes fréquentes d’insuffisance respiratoire. Nous donnons des conseils propres à la COVID-19 qui, au moment d’écrire l’article, constitue une pandémie mondiale. Dans ce contexte, l’EP apparaît comme un outil particulièrement utile au diagnostic et à la prise en charge des patients atteints d’une maladie cardiopulmonaire.
Lung ultrasound (LUS) is a useful point-of-care ultrasound (POCUS) technique that outperforms lung auscultation and chest X-ray, and nears the diagnostic accuracy of chest computed tomography (CT) for common causes of acute respiratory failure. LUS offers the advantages of portability, availability, and avoidance of radiation exposure. It provides real-time diagnostic information and procedural guidance. Cardiologists can use LUS to enhance their physical and echocardiographic examination. We provide a practical overview of LUS for cardiologists.
How to Perform a Lung Ultrasound Examination
Device selection
We perform LUS with widely available cart-based and handheld devices (Supplemental Table S1).
Patient position
The optimal patient position for LUS depends on the suspected pathology. If pneumothorax is suspected, we prefer the supine position to allow pleural air to collect at the anterior chest wall. If a simple pleural effusion is suspected, we prefer the semirecumbent or supine position to allow pleural fluid to collect at the posterior costophrenic angle. If a person is prone, pleural air will collect dorsally, and pleural fluid will collect ventrally. If an interstitial syndrome or lung consolidation is suspected, patient positioning is less critical, because all lung zones must be examined.
Probe selection and knobology
We base probe selection on availability, pathology, and area of interest. High-frequency probes (8-12 MHz) provide excellent visualisation of superficial structures (eg, pleural line) but have a narrow sector width and poor visualisation of deeper structures. Curvilinear probes (3-5 MHz) provide good visualisation of both superficial and deep structures but have a larger footprint and may require angulation when scanning to avoid rib shadows. Phased-array probes (3-4.5 MHz) can show all lung findings and have a smaller footprint, making the avoidance of rib shadows easier, but provide less adequate visualisation of the pleural line. We disable features that decrease artefact production because LUS relies on interpreting artefacts. We optimise gain, focus, and depth for the structure of interest.
Scanning protocol
Several LUS protocols provide instructions on the systematic scanning of lung zones to identify the causes of respiratory failure. We describe the 6-zone (3 zones per lung) protocol for speed and simplicity; however, more comprehensive 8- and 12-zone protocols exist.1 , 2
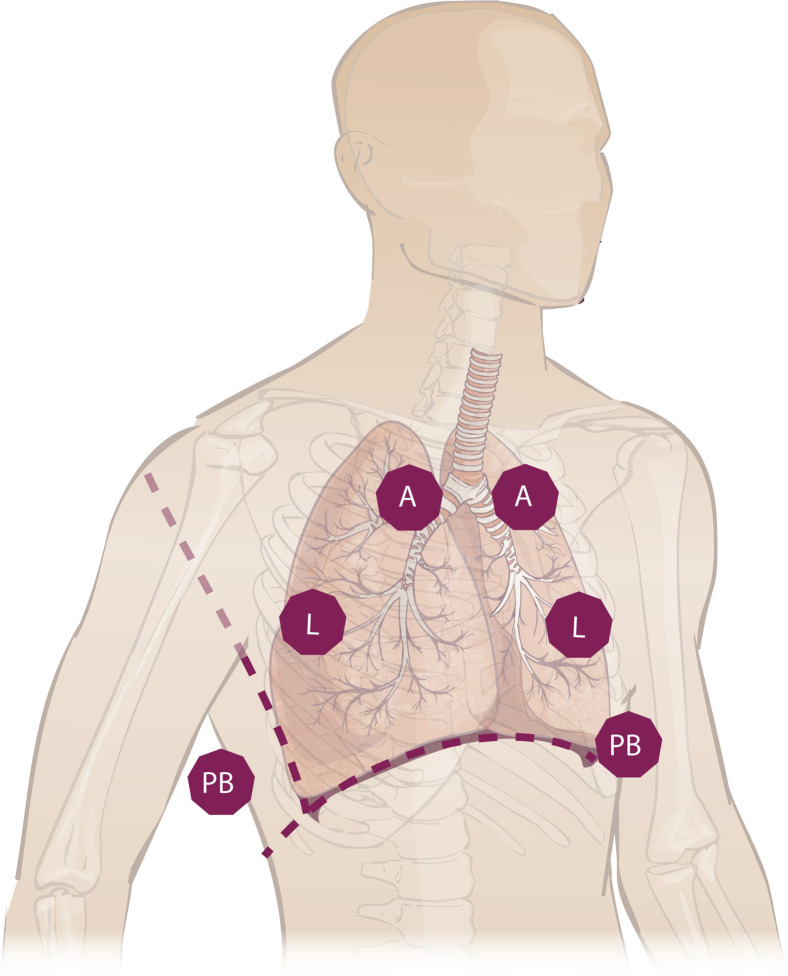
Six-zone LUS can provide a rapid and accurate assessment in most cases of acute respiratory failure.1 We examine the anterior, lateral, and posterior basal chest wall by 2-dimensional and M-mode imaging (Fig. 1 ). The angle of insonation must be perpendicular to the pleural line. Because the contour of the chest wall may differ from the underlying pleura, techniques such as sliding and fanning are essential to ensure ultrasound beam alignment. Failing to do so may cause false positive (eg, impression of an abnormal pleural line) or false negative (eg, failing to see A- or B-lines) findings. LUS clips should capture an entire respiratory cycle and should be stored for documentation.
Figure 1.
A simple protocol for lung ultrasound scanning including 2-dimensional and M-mode lung ultrasound imaging of the anterior (A), lateral (L), and posterior basal (PB) lung zones. Lung ultrasound is performed bilaterally and may be followed by limited cardiac ultrasound and venous ultrasound if indicated.
Training and supervision
As with any imaging modality, the accuracy of LUS depends on operator skill. Learners may save and review images with experienced operators for supervised interpretation. All of the handheld devices discussed have this ability (Supplemental Table S1).
Cleaning and disinfecting devices
See “Cleaning and Disinfecting Devices During COVID-19” in the Supplementary Material.
Findings of Lung Ultrasound
LUS interpretation relies on characteristic normal and abnormal artefacts, because ultrasound waves do not transmit through gas-filled structures such as normal lung parenchyma.
Pleural line
Normal
The parietal pleura appears as a horizontal hyperechoic line a half centimetre below the rib line (Supplemental Fig. S1). A-Lines are reverberation artefacts produced by the interface between pleura and aerated lung. A-Lines appear as echogenic horizontal lines spaced at equidistant multiples of the transducer-pleural line (Supplemental Fig. S2; Video 1
 , view video online). Lung sliding is the normal respirophasic horizontal to-and-fro movement of the parietal and visceral pleural sliding against each other (Video 2
, view video online). Lung sliding is the normal respirophasic horizontal to-and-fro movement of the parietal and visceral pleural sliding against each other (Video 2
 , view video online). M-Mode imaging will show a stratified pattern of fixed subcutaneous tissue and parietal pleura with a heterogeneous “sandy pattern” below, termed the seashore sign (Supplemental Fig. S2). The lung pulse is the rhythmic movement of the visceral pleural along the parietal pleural with cardiac contraction and is a useful finding to rule out pneumothorax (Video 3
, view video online). M-Mode imaging will show a stratified pattern of fixed subcutaneous tissue and parietal pleura with a heterogeneous “sandy pattern” below, termed the seashore sign (Supplemental Fig. S2). The lung pulse is the rhythmic movement of the visceral pleural along the parietal pleural with cardiac contraction and is a useful finding to rule out pneumothorax (Video 3
 , view video online).
, view video online).
Abnormal
Abnormal pleural line findings include an irregular pleural line and the absence or impairment of lung sliding (Supplemental Fig. S1; Videos 4
 and 5
and 5
 , view video online). A lung point is an abrupt cessation of lung sliding that is pathognomonic of pneumothorax (Video 6
, view video online). A lung point is an abrupt cessation of lung sliding that is pathognomonic of pneumothorax (Video 6
 , view video online). It defines the margin of a pneumothorax, where pleural air transitions to parenchymal air. M-Mode imaging of a pneumothorax will show a stratified pattern of all structures, termed the barcode sign (Supplemental Fig. S2).
, view video online). It defines the margin of a pneumothorax, where pleural air transitions to parenchymal air. M-Mode imaging of a pneumothorax will show a stratified pattern of all structures, termed the barcode sign (Supplemental Fig. S2).
Pleural space
Normal
The pleural space is a potential space between the parietal and visceral pleura. It is normally not seen.
Abnormal
Simple pleural effusions appear as an anechoic space bordered by the chest wall, diaphragm, and lung (Supplemental Fig. S3; Video 7
 , view video online). M-Mode imaging will show respirophasic displacement from the pleural line, termed the sinusoidal sign. Complicated pleural effusions may show iso- or hyperechoic components, such as septations (Supplemental Fig. S3; Video 8
, view video online). M-Mode imaging will show respirophasic displacement from the pleural line, termed the sinusoidal sign. Complicated pleural effusions may show iso- or hyperechoic components, such as septations (Supplemental Fig. S3; Video 8
 , view video online).
, view video online).
Parenchyma
Normal
Normal lung shows lung sliding with A-lines, as described above. A-Lines are produced by the interface of the pleura with air and may therefore be present in normal or abnormal lung that remains aerated (eg, pneumothorax, obstructive lung disease, pulmonary embolism; Supplemental Fig. S2).
Abnormal
An interstitial pattern is characterised by multiple B-lines. The B-line is a well defined respirophasic vertical artefact that arises from the pleural line, extends to the bottom of the screen without fading in a hyperechoic comet-tail appearance, and erases A-lines (Supplemental Fig. S4). Two or fewer B-lines per intercostal space may be normal (particularly in dependent areas). More than 2 B-lines per intercostal space is abnormal and defines an interstitial process, which correlates with an interstitial pattern on a chest X-ray (Video 9
 , view video online). Coalescent B-lines reflect a higher burden of disease and correlate with ground-glass opacities on chest CT (Supplemental Fig. S4; Video 10
, view video online). Coalescent B-lines reflect a higher burden of disease and correlate with ground-glass opacities on chest CT (Supplemental Fig. S4; Video 10
 , view video online).
, view video online).
An alveolar pattern is characterised by consolidated, isoechoic lung. Consolidations and atelectasis can appear with the same echotexture as the liver, termed hepatisation (Supplemental Fig. S5; Video 11
 , view video online). Consolidations are visible by LUS only if they reach the pleura. Consolidations may be translobar (involving an entire lung lobe) or nontranslobar. The border of nontranslobar consolidations with aerated lung is echogenic and irregular, termed the shred sign (Supplemental Fig. S5; Video 12
, view video online). Consolidations are visible by LUS only if they reach the pleura. Consolidations may be translobar (involving an entire lung lobe) or nontranslobar. The border of nontranslobar consolidations with aerated lung is echogenic and irregular, termed the shred sign (Supplemental Fig. S5; Video 12
 , view video online). Bronchograms may help differentiate pneumonia from atelectasis. Dynamic air bronchograms show respirophasic movement of at least 2 cm and suggest pneumonia, whereas static air bronchograms suggest pneumonia or atelectasis.
, view video online). Bronchograms may help differentiate pneumonia from atelectasis. Dynamic air bronchograms show respirophasic movement of at least 2 cm and suggest pneumonia, whereas static air bronchograms suggest pneumonia or atelectasis.
Cardiac and vascular ultrasound
Cardiac POCUS can complement LUS to enhance the diagnostic accuracy of causes of respiratory failure and to screen for concurrent cardiovascular conditions. Cardiac POCUS provides a real-time assessment of ventricular function, pericardial abnormalities, and gross valvular abnormalities. In patients with hypoxemic respiratory failure and normal LUS findings, vascular POCUS using a 2-point compression test may be useful to exclude venous thromboembolism.3
Interpretation of Lung Ultrasound
LUS interpretation is quick and > 90% accurate for common causes of acute respiratory failure (Supplemental Table S2). A few concepts are of great value to the clinician. Pleural line abnormalities and impaired lung sliding are present in pneumothorax, inflammatory conditions (acute respiratory distress syndrome [ARDS], pneumonia), and fibrotic disease, but absent in heart failure (Table 1 ). B-Lines may be normal in dependent areas or lung fissures, but should not exceed 2 per intercostal space. B-Lines in a dependent, symmetric distribution, coupled with a smooth pleural line and bilateral simple pleural effusions, suggest heart failure. B-Lines in a patchy or asymmetric distribution with an irregular pleural line (with or without subpleural consolidations) suggest an inflammatory interstitial process, such as viral or atypical pneumonia, inflammatory lung disease, or early ARDS. Coalescent B-lines correlate with ground-glass opacities on chest CT and suggest a higher burden of disease. Bilateral dependent consolidations with associated simple pleural effusions suggest atelectasis. In contrast, unilateral consolidations (particularly if associated with dynamic air bronchograms or inflammatory B-lines) are more suggestive of an infectious process. Pulmonary embolism and obstructive lung disease typically present with a normal pleural line, normal lung sliding, and an absence of B-lines. We provide a simplified algorithmic approach to interpretation in Supplemental Figure S6.
Table 1.
Lung ultrasound findings and associated conditions
| Diagnosis | Lung sliding | Normal pleural line | Lung point | A-lines | B-lines∗ | Consolidation | Pleural effusion |
|---|---|---|---|---|---|---|---|
| Normal | + | + | − | + | − | − | − |
| Pneumonia or ARDS | +/− | − | − | − | + | +/− | +/− |
| Pneumothorax | − | + | + | + | − | − | − |
| Heart failure | + | + | − | − | + | +/− | +/− |
| Pulmonary embolism | + | + | − | +/− | − | +/− | +/− |
| COPD/asthma | +/− | + | − | + | − | − | − |
ARDS, acute respiratory distress syndrome; COPD, chronic obstructive pulmonary disease.
≤ 2 B-lines per intercostal space may be normal and visualised in lung fissures or dependent zones.
Lung Ultrasound for COVID-19
The Supplementary Material provides background, indications, findings, and infection precautions for LUS during the COVID-19 pandemic.
Conclusion
LUS enhances the physical and echocardiographic examination to improve the diagnosis of the causes of respiratory failure. LUS has a clear advantage over chest X-ray as a point-of-care test that is portable, safe, and accurate and provides immediate feedback. Cardiologists may learn LUS to improve their diagnosis and management of cardiopulmonary disease.
Funding Sources
The authors have no funding sources to declare.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
See page 1147 for disclosure information.
To access the supplementary material accompanying this article, visit the online version of the Canadian Journal of Cardiology at www.onlinecjc.ca and at https://doi.org/10.1016/j.cjca.2020.05.008.
Supplementary Material
Lung ultrasound showing a normal pleural line as well as A-lines, a normal horizontal repitition artifact.
. Normal lung ultrasound showing a normal pleural line and lung sliding in the center of the image, flanked by rib and rib shadow.
Lung ultrasound showing a lung pulse, the normal rhythmic movement of the visceral pleural along the parietal pleural with cardiac contraction, which is a useful finding to rule out pneumothorax.
Lung ultrasound showing a segment of an irregular pleural line.
Lung ultrasound showing impaired lung sliding.
Lung ultrasound showing a lung point, the point of cessation of lung sliding, a pathognomonic finding of pneumothorax.
Lung ultrasound showing a simple pleural effusion visualized as an anechoic pleural space surrounding lung exhibiting hepatization. Visualization of the vertebral bodies above the diaphragm is termed the spine sign, and is indicative of a fluid collection such as a pleural effusion.
Lung ultrasound showing a complicated pleural effusion visualized as an echogenic pleural space with hyperechoic septations.
Lung ultrasound showing multiple B-lines, which are respirophasic hyperechoic vertical artifacts that arise from the pleural line and correlate with interstitial edema.
Lung ultrasound showing coalescent B-lines, which correlate with ground-glass opacification on chest CT.
Lung ultrasound showing consolidation with the echotexture of the liver, termed hepatization.
Lung ultrasound showing a subpleural consolidation with a shred sign, characterized by a hyperechoic interface between consolidated and normal lung. A simple pleural effusion is visualized as an anechoic space, a finding supported by the spine sign.
References
- 1.Picano E., Scali M.C., Ciampi Q., Lichtenstein D. Lung ultrasound for the cardiologist. JACC Cardiovasc Imaging. 2018;11:1692–1705. doi: 10.1016/j.jcmg.2018.06.023. [DOI] [PubMed] [Google Scholar]
- 2.Volpicelli G., Elbarbary M., Blaivas M., et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012;38:577–591. doi: 10.1007/s00134-012-2513-4. [DOI] [PubMed] [Google Scholar]
- 3.Johri AM, Galen B, James N, et al. ASE statement on point-of-care ultrasound (POCUS) during the 2019 novel coronavirus pandemic [e-pub ahead of print]. J Am Soc Echocardiogr https://doi.org/10.1016/j.echo.2020.04.017. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Lung ultrasound showing a normal pleural line as well as A-lines, a normal horizontal repitition artifact.
. Normal lung ultrasound showing a normal pleural line and lung sliding in the center of the image, flanked by rib and rib shadow.
Lung ultrasound showing a lung pulse, the normal rhythmic movement of the visceral pleural along the parietal pleural with cardiac contraction, which is a useful finding to rule out pneumothorax.
Lung ultrasound showing a segment of an irregular pleural line.
Lung ultrasound showing impaired lung sliding.
Lung ultrasound showing a lung point, the point of cessation of lung sliding, a pathognomonic finding of pneumothorax.
Lung ultrasound showing a simple pleural effusion visualized as an anechoic pleural space surrounding lung exhibiting hepatization. Visualization of the vertebral bodies above the diaphragm is termed the spine sign, and is indicative of a fluid collection such as a pleural effusion.
Lung ultrasound showing a complicated pleural effusion visualized as an echogenic pleural space with hyperechoic septations.
Lung ultrasound showing multiple B-lines, which are respirophasic hyperechoic vertical artifacts that arise from the pleural line and correlate with interstitial edema.
Lung ultrasound showing coalescent B-lines, which correlate with ground-glass opacification on chest CT.
Lung ultrasound showing consolidation with the echotexture of the liver, termed hepatization.
Lung ultrasound showing a subpleural consolidation with a shred sign, characterized by a hyperechoic interface between consolidated and normal lung. A simple pleural effusion is visualized as an anechoic space, a finding supported by the spine sign.