Abstract
Six-minute walk distance (6MWD) assessment is recommended for pulmonary arterial hypertension multidimensional risk stratification. However, current 6MWD cut-off values were mainly derived from North American and European pulmonary arterial hypertension registries. Therefore, it is unknown if such cut-off values broadly apply to other geographical populations. In this study, we aimed to identify 6MWD cut-off values for Brazilian pulmonary arterial hypertension patients and to contrast our findings to current international Pulmonary Hypertension guidelines recommendations. One-hundred four consecutive pulmonary arterial hypertension patients were allocated in groups according to their 6MWD, considering 50 m as a clinically relevant 6MWD difference. Next, patients were categorized into different 6MWD ranges based on similar survival rates in each group: < 250 m, 250–400 m, and >400 m. The study outcome was all-cause mortality and transplantation according to the 6MWD range. Survival was truncated at five years. Median follow-up period was 4.35 years (0.48–5.00). Survival rates at 1, 2, 3, and 5 years were 96%, 89%, 81%, and 73%, respectively. Cox analyses adjusted for age, sex, and pulmonary arterial hypertension etiology showed that 6MWD < 250 m and >400 m were associated with higher and lower risk of all-cause mortality and transplantation. According to Harrell's c-statistic, the prognostic discrimination of the 6MWD cut-off value identified by the current study was 0.70 while international Pulmonary Hypertension guidelines 6MWD cut-offs value was 0.61. In conclusion, our findings suggest that 6MWD geographical variations should be considered when assessing risk stratification in pulmonary arterial hypertension.
Keywords: risk stratification, survival, Latin America
Introduction
Pulmonary arterial hypertension (PAH) is a chronic disease increasingly recognized worldwide.1–6 PAH is characterized by increased pulmonary vascular resistance (PVR) that can lead to right ventricular dysfunction and failure.7,8
Effort intolerance is a cardinal feature of PAH and is strongly correlated with disease severity.9,10 In this context, the six-minute walk test distance (6MWD) is a well-established tool to evaluate exercise tolerance, being a simple and reproducible measure of functional capacity.11–14 The prognostic value of the 6MWD in PAH has been confirmed in different cohorts.15–17 As such, 6MWD determination is recommended as part of the baseline and follow-up PAH multidimensional risk stratification, contributing to goal-oriented therapeutic decisions.18
Current Pulmonary Hypertension (PH) guidelines recommend the use of 6MWD cut-off values of <165 m, 165–440 m, and >440 m to identify PAH patients with high, intermediate, and low risk for mortality, respectively.14,18 These 6MWD thresholds were primarily derived from North American14 and European PAH registries.1,17 The cut-off <165 m was recently validated in a large Germany cohort for 1, 2, and 3 years mortality.17 However, 6MWD is known to be influenced by several factors such as gender, age, weight, height, and body mass index (BMI), for example.19–22 Moreover, 6MWD geographical and ethnic differences have also been reported, adding complexity to 6MWD interpretation beyond anthropometric-related characteristics.23
In this context, it is unclear if 6MWD PAH cut-off values currently used for risk stratification broadly apply to other PAH geographical populations. Therefore, in the current study, we sought to identify 6MWD cut-off values derived from a Brazilian PAH referral center and to contrast our findings to current international PH guidelines recommendations. We hypothesized that 6MWD geographical nuances would influence 6MWD cut-off thresholds for PAH prognostication.
Methods
Study design and patients
Data from consecutive newly diagnosed PAH patients from the Pulmonary Hypertension Clinic of the Federal University of São Paulo (São Paulo, Brazil) between March 2003 and November 2015 were retrospectively analyzed.
Patients were eligible for the study if they were older than 18 years old, met clinical and hemodynamic criteria for Group 1 PAH, and had a baseline 6MWD available for review. PAH was hemodynamically defined by a mean pulmonary arterial pressure ≥25 mmHg, a pulmonary capillary wedge pressure ≤15 mmHg, and a PVR ≥ 3WU on resting supine right heart catheterization (RHC) after the exclusion of other known causes of PH, following current PH guidelines recommendations at the time of this study.24
Exclusion criteria included the use of PAH-specific treatment before baseline 6MWD and/or incomplete clinical or RHC records. The study protocol was approved by the Institutional Medical Ethics Committee.
World Health Organization (WHO) functional classification system was used.25 Patients who had experienced syncope were assigned to functional class IV.
6MWT was performed following the American Thoracic Society six-minute walk test guidelines.26 6MWD was presented in absolute value.
The study outcome was all-cause mortality and lung transplant. The study follow-up period ended in December 2018, and survival analysis was truncated at five years. Survival status was ascertained by a review of institutional electronic medical records or by telephone calls when the patient had not attended the last visit. If contact could not be established, patients were censored at the date of the last visit registered in the electronic medical record.
Statistical analysis
Data are presented as mean ± standard deviation and median with 95% confidence intervals unless otherwise stated. Categorical variables were compared using chi-square test. Comparisons of continuous variables between more than two groups were performed using ANOVA with Bonferroni post-hoc analysis. Subjects were initially allocated into groups according to the 6MWD, every 50 m. Seven five-groups were identified (<250 m, 250–300 m, 301–350 m, 351–400 m, 401–451 6 m, 450–500 m, >500 m). Unadjusted hazard ratios for each 6MWD category were estimated using Cox regression. Next, 6MWD ranges were combined into three categories based on similar survival rates: <250 m, 250–400 m, and >400 m. Cox regression models unadjusted and adjusted for sex, age, and PAH etiology were built to estimate survival for PAH patients according to the three groups established above. The results were compared to those obtained when the study population was stratified by the 6MWD cut-off values recommended by current PH guidelines (i.e. < 165 m, 165–440 m, and >440 m).18 Harrell's c-statistic was used to assess the prognostic discrimination of both models. Overall survival was estimated by Kaplan–Meier analysis. Log-rank and Breslow tests were used to compare survival among different 6MWD ranges. Significance levels for all tests were established as two-tailed p-values ≤ 0.05. All statistical analyses were conducted using SPSS version 21.0 (SPSS Inc., Chicago, IL, USA).
Results
A total of 186 subjects with an established diagnosis of PAH were considered eligible for the study based on our inclusion criteria. All patients performed 6MWT. Of these, 43 subjects were excluded as they were already receiving PAH-specific therapy at baseline 6MWD assessment and 39 due to incomplete medical records. Therefore, the final study cohort was composed of 104 subjects.
The mean age at baseline was 41 years old; most of them were female (76%) and Caucasians (66%) in New York Heart Association functional class (NYHA-FC) III and IV (Table 1).
Table 1.
Baseline characteristics of PAH patients according to six-minute walk distance.
| Variables | Total N = 104 | < 250 m N = 08 | 250–400 m N = 40 | > 400 m N = 56 | ANOVA p-values |
|---|---|---|---|---|---|
| Age, years | 41 ± 15 | 57 ± 21a | 44 ± 13 | 38 ± 14a | 0.001 |
| Gender, female | 79 (76) | 6 (75) | 33 (83) | 40 (71) | 0.26 |
| Self-reported race | 0.11 | ||||
| Caucasian | 69 (66) | 6 (75) | 31 (78) | 32 (57) | |
| Mixed | 27 (26) | 2 (25) | 5 (13) | 20 (36) | |
| Black | 6 (6) | – | 2 (5) | 4 (7) | |
| Asian | 2 (2) | – | 2 (5) | – | |
| BMI, Kg/m2 | 25 ± 5 | 27 ± 7 | 27 ± 5b | 24 ± 4b | 0.03 |
| NYHA-FC III/IV | 63 (61) | 7 (88) | 29 (73) | 27 (48) | 0.02c |
| Underlying diagnosis | 0.51 | ||||
| Idiopathic | 39 (37) | 3 (38) | 14 (35) | 22 (39) | |
| Connective tissue disease | 31 (30) | 4 (50) | 10 (25) | 17 (30) | |
| Congenital heart disease | 13 (12) | 0 (0) | 8 (20) | 5 (9) | |
| Portal hypertension | 10 (10) | 1 (12) | 5 (13) | 4 (7) | |
| Schistosomiasis | 5 (5) | 0 (0) | 0 (0) | 5 (9) | |
| HIV | 4 (4) | 0 (0) | 2 (5) | 2 (4) | |
| Hereditary | 1 (1) | 0 (0) | 0 (0) | 1 (2) | |
| Venoocclusive disease | 1 (1) | 0 (0) | 1 (2) | 0 (0) | |
| Hemodynamics | |||||
| RAP, mmHg | 10 ± 5 | 13 ± 9 | 11 ± 6 | 10 ± 5 | 0.17 |
| mPAP, mmHg | 58 ± 12 | 58 ± 12 | 58 ± 12 | 57 ± 13 | 0.91 |
| PCWP, mmHg | 10 ± 3 | 10 ± 2 | 11 ± 3 | 10 ± 3 | 0.87 |
| Cardiac output, L | 3.8 ± 1.2 | 3.7 ± 1.1 | 3.7 ± 1.2 | 3.9 ± 1.2 | 0.67 |
| Cardiac index, L/min/m2 | 2.3 ± 0.7 | 2.2 ± 0.5 | 2.10 ± 0.7 | 2.4 ± 0.7 | 0.19 |
| SvO2, % | 62 ± 9 | 52 ± 9a | 61 ± 10 | 63 ± 8a | 0.03 |
| PVR, dynes . s . cm−5 | 1150 ± 583 | 1286 ± 591 | 1181 ± 583 | 1109 ± 637 | 0.67 |
| Six-minute walk test | |||||
| 6MWD, m | 390 ± 98 | 177 ± 61 | 336 ± 42 | 460 ± 48 | < 0.001 |
< 250 m vs >400 m
250–400 m vs >400 m
NYHA functional class did not meet assumptions to perform Bonferroni's analysis.
BMI, body mass index; NYHA-FC: New York Heart Association Functional Class; HIV: human immunodeficiency virus; RAP: right atrial pressure; mPAP: mean pulmonary arterial pressure; PCWP: pulmonary capillary wedge pressure; SVO2: mixed venous oxygen saturation; PVR: pulmonary vascular resistance; 6MWD: six-minute walk distance.
Note: Values are expressed as mean ± SD or n (%).
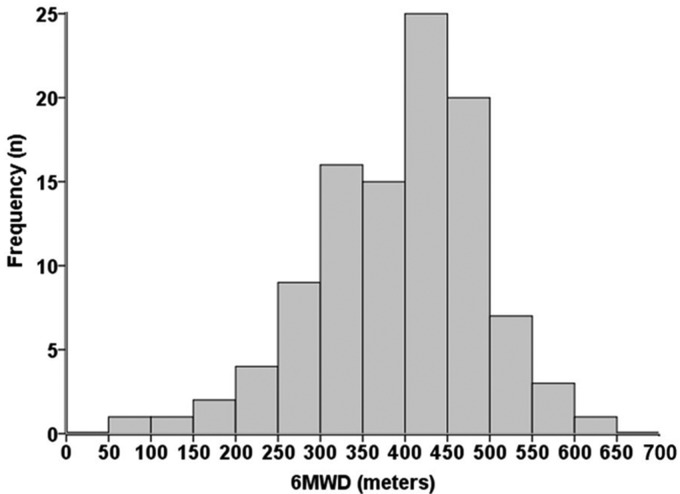
According to 6MWD, PAH patients with 6MWD > 400 m were younger, had lower BMI, and it is worth noting that 24 (43%) were in FC III and 3(5%) in FC IV. Patients with 6MWD < 250 m were more often in FC III or IV (7/88%), compared to those who walked between 250–400 m (29/73%) and >400 m (27/48%); p = 0.02. There were no significant differences among the groups for RHC parameters. The 6MWD distribution is presented respectively in Fig. 1.
Fig. 1.
Distribution of 6MWD.
6MWD: six-minute walk test distance.
Median follow-up period was 4.35 years, ranging from 0.48 to 5 years (by study design). There were 26 deaths and 1 lung transplant within the observation period. Survival rates at 1, 2, 3, and 5 years were 96%, 89%, 81%, and 73%, respectively. At last visit 52 (50%), 47 (45%), and 5 (5%) subjects were on monotherapy, double combined therapy, or triple therapy, respectively.
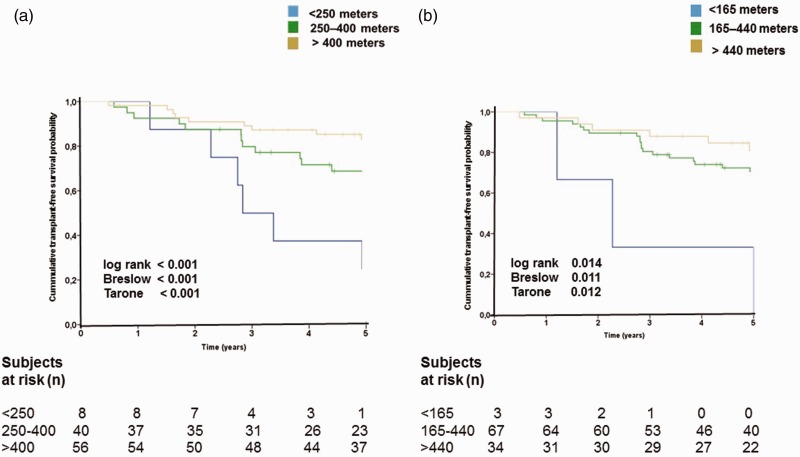
Kaplan–Meier survival curves are presented in Fig. 2a and b. Cox analysis adjusted for age, sex, and PAH etiology showed that 6MWD < 250 m were associated with higher rates of death than 6MWD > 400 m (Table 2).
Fig. 2.
Kaplan–Meier survival estimates according to 6MWD.
Table 2.
Cox proportional analysis and Harrel's C-statistic for all-cause mortality based on the 6MWD range.
| Distance category (m) | Unadjusted hazard ratio (95% CI; p value) | Adjusted hazard ratioa (95% CI; p value) |
|---|---|---|
| Current study | ||
| <250 | 6.88 (2.38–19.94; < 0.001) | 10.61 (3.19–35.32; < 0.001) |
| 250–400 | 2.45 (1.02–5.92; 0.046) | 2.74 (1.11–6.73; 0.029) |
| >400 | Reference | Reference |
| C-statistic | 0.66 | 0.70 |
| International guidelines | ||
| <165 | 6.34 (1.27–31.64; 0.024) | 6.04 (1.13–32.24; 0.035) |
| 165–440 | 1.67 (0.67–4.19; 0.271) | 1.74 (0.69–4.43; 0.243) |
| >440 | Reference | Reference |
| C-statistic | 0.58 | 0.61 |
Adjusted for age and pulmonary arterial hypertension underlying diagnosis.
CI: confidence interval.
According to Harrell's c-statistic, the prognostic discrimination of international guidelines 6MWD cut-off recommendations (<165 m, 165–440 m, >440 m) was 0.61. On the other hand, the 6MWD cut-off identified by the current study (>400 m, 400–250 m, and <250 m) revealed prognostic discrimination of 0.70.
Discussion
To the best of our knowledge, although 6MWD has been widely recommended for the risk stratification of PAH, this is the first study to assess its prognostic value in South America. Our findings suggest that geographical variations of 6MWD should be considered during the assessment of prognosis in PAH. In the present study, individuals with lower 6MWD had worse survival, in agreement with the international guidelines, but with a higher cut-off value for worse survival (250 m instead of 165 m), implying a change from intermediate to high-risk rating. Therefore, taking geographical variations of 6MWD into account during risk stratification may lead to better management decisions for patients with PAH.
Regional differences were also observed in COMPASS-2, a study adding bosentan to stable sildenafil therapy that was not superior to sildenafil monotherapy in delaying the time to the first morbidity/mortality event.27 Nevertheless, in a post hoc exploratory analysis, significant interactions with 6MWD and the geographical region in the effect of combination therapy were demonstrated, suggesting improvement in the primary end-point in subgroup the patients from Brazil.27
Casanova et al.23 had shown the geographical variations of 6MWD in a large cohort of healthy adults. Brazilian subjects walked 100 m more than subjects from Venezuela or Chile. The 6MWD cannot be explained by anthropometric factors, but the age was the most important factor influencing 6MWD, besides possible sociocultural conditions.14 The subjects of our study were younger than observed in European28,29 or American registries30 but similar to others from Brazil5 and China.2 However, even after adjusting for age, the 6MWD maintained its prognostic role.
Interestingly, in our study, among patients who walked >400 m, 24 (43%) were in FC III and 3 (5%) in FC IV. Similar results were shown in another Brazilian PAH cohort.5 It is worth highlighting that WHO or NYHA functional classification is a subject tool combining indicators of functional capacity limitation (physiologic limitations), functional performance (limitations in physical activity), and reserve (symptoms of fatigue, palpitations, and chest pain).31 Although several studies have shown an association between 6MWD and FC in PAH patients, this discrepancy can be explained by the multidimensional characteristic of FC, and by the observer32 or patient misinterpretation. Although syncope has not been considering in the original WHO classification, in our center, patients who have experienced a syncopal episode are assigned to FC IV. Despite these limitations, WHO or NYHA functional classification remains widely used to characterize the disease severity, as well as the endpoint of clinical trials.
There were no differences in hemodynamic parameters among 6MWD groups in our study. The reduced number of patients who walked <250 m was a limiting factor; however, it is noteworthy that most patients walked >400 m. Degano et al. have already demonstrated characteristics of PAH patients who walked more than 450 m, besides being younger and with low BMI, some patients had a severe hemodynamic impairment. Similar to our results, they did not observe hemodynamic differences among those who walked less or more than 450 m.33
There are some limitations to our study. It is a single-center study, but our referral center serves a multiracial population, the distribution of the subjects according to the race observed in our study was similar to that reported in the state of São Paulo.34 However, a generalization for the entire country should be done with caution. The national and continental registries are necessary to validate these results. It is a retrospective study with a significant number of excluded patients, in part because many of them came to our center already under treatment before confirmation of the diagnosis. However, the survival of the patients in the study, and of those excluded, was similar, minimizing the potential impact of this factor (data not presented). Furthermore, it is worth pointing out that survival rates of our study at one, two, three, four, and five years were 96%, 89%, 83%, 78%, and 73%, respectively, very close to that observed in developed countries.19 The sample size of our study allowed the only prediction of long-term survival, as recently demonstrated by a large incident cohort of patients with PAH from French pulmonary hypertension registry with a simplified risk assessment tool, wherein the multivariable analysis of baseline criteria, only a 6MWD ≤ 440 m independently predicted death or transplantation in five years.35
As expected, we demonstrated that our internal cut-off values have superior prognostic value for our cohort compared to international guidelines. We recognize that the small number of patients who walked <165 m or even <250 m is an important limitation of this study. However, this reinforces the importance of reference centers in different geographical regions should be aware of their own particularities.
In conclusion, our findings suggest that 6MWD geographical variations should be considered while assessing prognosis in PAH. Regional pulmonary hypertension registries are fundamental for better management of the patient, and there is still a gap in South America.
Acknowledgments
The authors acknowledge the guidance by the MECOR Program and Statistics Department of UNIFESP for this study.
Conflict of interest
The author(s) declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethical approval
The study protocol was approved by the Institutional Medical Ethics Committee (#1586272).
ORCID iDs
Gabriela O.S. Costa https://orcid.org/0000-0001-6092-5839
Roberta P. Ramos https://orcid.org/0000-0002-2383-6527
Rudolf K.F. Oliveira https://orcid.org/0000-0002-2252-8119
Jaquelina S. Ota-Arakaki https://orcid.org/0000-0002-5350-7679
References
- 1.Humbert M, Sitbon O, Chaouat A, et al. Pulmonary arterial hypertension in France: results from a national registry. Am J Respir Crit Care Med 2006; 173: 1023–1030. [DOI] [PubMed] [Google Scholar]
- 2.Jing Z-C, Xu X-Q, Han Z-Y, et al. Registry and survival study in Chinese patients with idiopathic and familial pulmonary arterial hypertension. Chest 2007; 132: 373–379. [DOI] [PubMed] [Google Scholar]
- 3.Escribano-Subias P, Blanco I, López-Meseguer M, et al. Survival in pulmonary hypertension in Spain: insights from the Spanish registry. Eur Respir J 2012; 40: 596–603. [DOI] [PubMed] [Google Scholar]
- 4.Badesch DB, Raskob GE, Elliott CG, et al. Pulmonary arterial hypertension: baseline characteristics from the REVEAL Registry. Chest 2010; 137: 376–387. [DOI] [PubMed] [Google Scholar]
- 5.Alves JL, Gavilanes F, Jardim C, et al. Pulmonary arterial hypertension in the southern hemisphere: results from a registry of incident Brazilian cases. Chest 2015; 147: 495–501. [DOI] [PubMed] [Google Scholar]
- 6.Rådegran G, Kjellström B, Ekmehag B, et al. Characteristics and survival of adult Swedish PAH and CTEPH patients 2000–2014. Scand Cardiovasc J 2016; 50: 243–250. [DOI] [PubMed] [Google Scholar]
- 7.Rubin LJ. Primary pulmonary hypertension. New Engl J Med 1997; 336: 111–117. [DOI] [PubMed] [Google Scholar]
- 8.VonkNoordegraaf A, Chin KM, Haddad F, et al. Pathophysiology of the right ventricle and of the pulmonary circulation in pulmonary hypertension: an update. Eur Respir J 2019; 53: 1801900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sun X-G, Hansen JE, Oudiz RJ, et al. Exercise pathophysiology in patients with primary pulmonary hypertension. Circulation 2001; 104: 429–435. [DOI] [PubMed] [Google Scholar]
- 10.Ferreira EVM, Ota-Arakaki JS, Ramos RP, et al. Optimizing the evaluation of excess exercise ventilation for prognosis assessment in pulmonary arterial hypertension. Eur J Prev Cardiol 2014; 21: 1409–1419. [DOI] [PubMed] [Google Scholar]
- 11.Miyamoto S, Nagaya N, Satoh T, et al. Clinical correlates and prognostic significance of six-minute walk test in patients with primary pulmonary hypertension. Am J Respir Crit Care Med 2000; 161: 487–492. [DOI] [PubMed] [Google Scholar]
- 12.Paciocco G, Martinez FJ, Bossone E, et al. Oxygen desaturation on the six-minute walk test and mortality in untreated primary pulmonary hypertension. Eur Respir J 2001; 17: 647–652. [DOI] [PubMed] [Google Scholar]
- 13.Sitbon O, Humbert M, Nunes H, et al. Long-term intravenous epoprostenol infusion in primary pulmonary hypertension prognostic factors and survival. J Am Coll Cardiol 2002; 40: 780–788. [DOI] [PubMed] [Google Scholar]
- 14.Benza RL, Miller DP, Gomberg-Maitland M, et al. Predicting survival in pulmonary arterial hypertension: insights from the registry to evaluate early and long-term pulmonary arterial hypertension disease management (REVEAL). Circulation 2010; 122: 164–172. [DOI] [PubMed] [Google Scholar]
- 15.Humbert M, Sitbon O, Chaouat A, et al. Survival in patients with idiopathic, familial, and anorexigen-associated pulmonary arterial hypertension in the modern management era. Circulation 2010; 122: 156–163. [DOI] [PubMed] [Google Scholar]
- 16.Farber HW, Miller DP, McGoon MD, et al. Predicting outcomes in pulmonary arterial hypertension based on the 6-minute walk distance. J Heart Lung Transplant 2015; 34: 362–368. [DOI] [PubMed] [Google Scholar]
- 17.Zelniker TA, Huscher D, Vonk-Noordegraaf A, et al. The 6MWT as a prognostic tool in pulmonary arterial hypertension: results from the COMPERA registry. Clin Res Cardiol 2018; 107: 460–470. [DOI] [PubMed] [Google Scholar]
- 18.Galiè N, Channick RN, Frantz RP, et al. Risk stratification and medical therapy of pulmonary arterial hypertension. Eur Respir J 2019; 24: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Enright, Paul L, Sherrill DL. Reference equations for the six-minute walk in healthy adults. J Cardiopulm Rehabil 1999; 19: 129–130. [Google Scholar]
- 20.Iwama AM, Andrade GN, Shima P, et al. The six-minute walk test and body weight-walk distance product in healthy Brazilian subjects. Brazilian J Med Biol Res 2009; 42: 1080–1085. [DOI] [PubMed] [Google Scholar]
- 21.Soares M, Pereira C. Six-minute walk test: reference values for healthy adults in Brazil. J Bras Pneumol 2011; 37: 576–83. [DOI] [PubMed] [Google Scholar]
- 22.Britto RR, Probst VS, De Andrade AFD, et al. Reference equations for the six-minute walk distance based on a Brazilian multicenter study. Brazilian J PhysTher 2013; 17: 556–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Casanova C, Celli BR, Barria P, et al. The 6-min walk distance in healthy subjects: reference standards from seven countries. Eur Respir J 2011; 37: 150–156. [DOI] [PubMed] [Google Scholar]
- 24.Galiè N, Humbert M, Vachiery J-L, et al. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J 2016; 37: 67–119. [DOI] [PubMed] [Google Scholar]
- 25.Barst RJ, Mcgoon M, Torbicki A, et al. Diagnosis and differential assessment of pulmonary arterial hypertension. J Am Coll Cardiol 2004; 43: S40–S47. [DOI] [PubMed] [Google Scholar]
- 26.Crapo RO, Casaburi R, Coates AL, et al. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002; 166: 111–117. [DOI] [PubMed] [Google Scholar]
- 27.Mclaughlin V, Channick RN, Ghofrani H, et al. Bosentan added to sildenafil therapy in patients with pulmonary arterial hypertension. Pulm Vasc Dis 2015; 46: 405–413. [DOI] [PubMed] [Google Scholar]
- 28.Humbert M, Sitbon O, Chaouat A, et al. Pulmonary arterial hypertension in France: results from a national registry. Am J Respir Crit Care Med 2006; 173: 1023–1030. [DOI] [PubMed] [Google Scholar]
- 29.Hoeper MM, Huscher D, Ghofrani HA, et al. Elderly patients diagnosed with idiopathic pulmonary arterial hypertension: results from the COMPERA registry. Int J Cardiol 2013; 168: 871–880. [DOI] [PubMed] [Google Scholar]
- 30.Benza RL, Gomberg-Maitland M, Miller DP, et al. The REVEAL registry risk score calculator in patients newly diagnosed with pulmonary arterial hypertension. Chest 2012; 141: 354–362. [DOI] [PubMed] [Google Scholar]
- 31.Miller-Davis C, Marden S, Leidy NK. The New York Heart Association Classes and functional status: what are we really measuring?. Heart Lung 2006; 35: 217–224. [DOI] [PubMed] [Google Scholar]
- 32.Taichman DB, McGoon MD, Harhay MO, et al. Wide variation in clinicians' assessment of New York Heart Association/World Health Organization functional class in patients with pulmonary arterial hypertension. Mayo Clin Proc 2009; 84: 586–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Degano B, Sitbon O, Savale L, et al. Characterization of pulmonary arterial hypertension patients walking more than 450 m in 6 min at diagnosis. Chest 2010; 137: 1297–1303. [DOI] [PubMed] [Google Scholar]
- 34.IBGE. População residente, por raça ou cor, segundo a situação do domícilio, o sexo e a idade, https://sidra.ibge.gov.br/tabela/3175#resultado (2010, accessed 10 August 2019).
- 35.Boucly A, Weatherald J, Savale L, et al. Risk assessment, prognosis and guideline implementation in pulmonary arterial hypertension. Eur Respir J 2017; 50: 1–10. [DOI] [PubMed] [Google Scholar]