Abstract
As pressure increases on public health systems globally, a potential consequence is that this is transferred to patients in the form of longer waiting times to receive care. In this review, we overview what waiting for health care encompasses, its measurement, and the data available in terms of trends and comparability. We also discuss whether waiting time is equally distributed according to socioeconomic status. Finally, we discuss the policy implications and potential approaches to addressing the burden of waiting time. Waiting time for elective surgery and emergency department care is the best described type of waiting time, and it either increases or remains unchanged across multiple developed countries. There are many challenges in drawing direct comparisons internationally, as definitions for these types of waiting times vary. There are less data on waiting time from other settings, but existing data suggest waiting time presents a significant barrier to health care access for a range of health services. There is also evidence that waiting time is unequally distributed to those of lower socioeconomic status, although this may be improving in some countries. Further work to better clarify definitions, identify driving factors, and understand hidden waiting times and identify opportunities for reducing waiting time or better using waiting time could improve health outcomes of our health services.
Keywords: waiting time, elective surgery, emergency department, primary care, inequality
What do we already know about the topic?
As pressure on health systems increases and complexity of heath care increases, time spent waiting for health services appears to be increasing.
How does your research contribute to the field?
This review confirms that waiting time for elective surgery and emergency department care is increasing in multiple countries. It also highlights the barrier that waiting times in other settings, including primary care, specialist care, allied health professional care, and time spent in clinic waiting rooms, pose to health care access and describes how inconsistencies in measurement between countries and settings complicate direct comparisons. This review also describes evidence of unequal waiting-time burden by socioeconomic status across all these settings. However, in many studies, the magnitude of the gradient is small. Some studies report that this burden is easing.
What are your research’s implications toward theory, practice, or policy?
Future policy to align measures of waiting time and to report on the burden of waiting time from a wider range of services could improve transparency for patients and health care providers on this important issue. Adopting approaches that focus on better utilizing the time patients spend waiting to deliver interventions that could improve health outcomes should also be considered.
Waiting Time for Health Services
Introduction
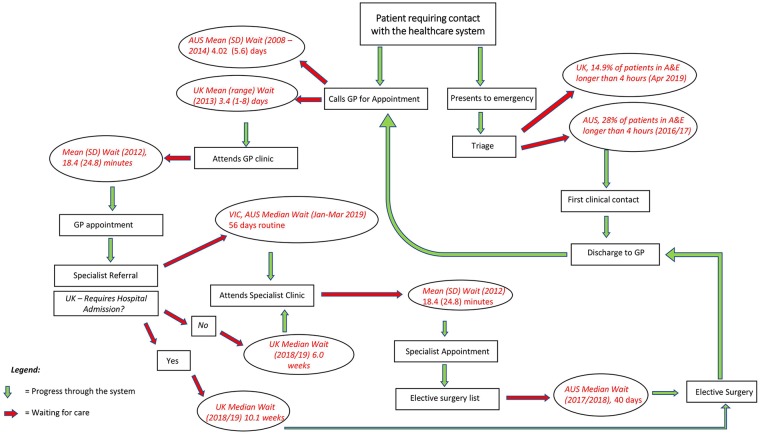
Time spent waiting for health care presents a potential barrier to health system access and engagement. Patients wait at multiple points of their interaction with health systems (Figure 1).
Figure 1.
Schematic of the time patients spend waiting for care with examples from the United States, Australia, and the United Kingdom.1,3,6,8-10,32,33
Commonly, system-level monitoring of waiting time focuses on the time patients wait at home for an initial health care provider appointment,1-5 time to diagnosis,1 or for an elective procedure.1,6,7 However, waiting time may also include time spent in waiting rooms on the day that patients are accessing a clinic8 or an emergency department (ED).9,10
Waiting times for elective surgery and ED care are a frequently included key performance indicator for health services, often reported to the public and keenly profiled by media.11-14 At face value, they are a process measure of health service access, but measurement definitions vary, and these measures can be “gamed,”15 exemplified by the changing of patient status from waiting to admitted in response to targets imposed by the National Health Service (NHS).16 Waiting-time measurement also varies between health systems.17 For example, both the United Kingdom and Australia monitor ED and surgical waiting times but define the start and endpoints of these very differently (Figures 2 and 3). In addition, waiting-time prioritization is a useful mechanism for rationing health services. It provides faster access for more urgent procedures, and an allowable wait time for others. While enabling more equitable distribution of access to care, this also complicates comparisons in waiting time as the urgency case-mix affects the overall waiting time reported.18 These factors mean that comparisons between health services and countries are limited.7,17
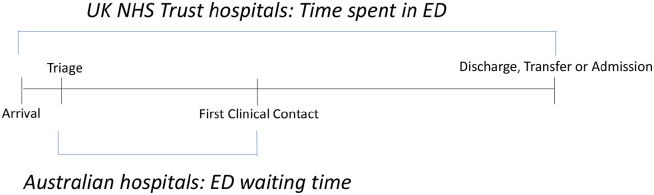
Figure 2.
Measurement of ED waiting times: Australia vs the United Kingdom.10,67
Note. UK: Total ED time refers to the time from arrival to discharge, transfer, or admission to hospital. Australia: ED wait times refer to the time from triage to first clinical contact. Being seen “on time” refers to first contact occurring within the clinically recommended time for each triage category: resuscitation (within seconds), emergency (within 10 min), urgent (within 30 min), semi-urgent (within 60 min) and nonurgent (within 120 min). ED = emergency department.
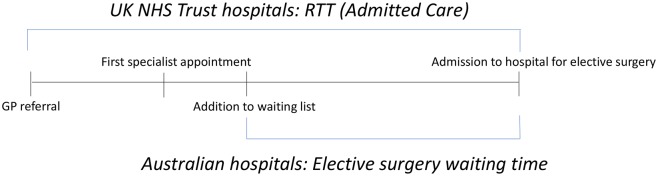
Figure 3.
Measurement of elective surgery waiting times: Australia vs the United Kingdom.1,29
Note. In UK, RTT time for elective surgery refers to the time from GP referral for consultant-led treatment to the initiation of this treatment. In Australia, elective surgery waiting time refers to the time from addition to removal from surgery waiting lists and does not include the time from GP referral. RTT = referral to treatment; GP = general practitioner.
The factors that influence various types of waiting times may be different and may have different impacts. With increasing burden on health systems, driven by an aging population and higher chronic disease burden,19 longer waiting times may be expected.20,21 However, what is the evidence for this, and what does this means in terms of quality of health care? This analysis is written to overview what waiting for health care encompasses, its use as an indicator of quality of health care, its magnitude, potential gaps, and policy implications.
Methods
We conducted a narrative review. Our first aim was to describe the issue of patient waiting times in multiple settings with data from national registries and observational studies. We sought to identify papers and sources from several regions that reported on waiting times for surgery or procedures, emergency treatment, primary care or specialist access, allied health professional care, and time spent in waiting rooms of health care providers. The second aim of this study was to describe whether, within the settings described above, there was an inequality in waiting time such that sociodemographic advantage corresponded to a shorter waiting time. We specifically sought to include papers that reported on inequality in waiting time, waiting time for patients with chronic disease, and waiting time among patients of low socioeconomic status (SES). We searched Scopus, Web of Science, Medline, and PubMed databases for papers published in English from 2000 to 2019 using combinations of the terms “chronic disease,” “cardiovascular disease,” “diabetes,” “COPD,” “GP visit/consultation,” “primary care,” “Specialist visit/consultation,” “health resource utilization,” “waiting time,” “waiting room time,” “allied health,” “nursing,” “time burden,” “treatment burden,” “socioeconomic status,” and “inequality.” We also screened reference lists of identified papers and searched NHS England and Australian Institute of Health and Welfare statistical databases.
From relevant papers, we have collated information on the type of waiting time, the way waiting time was measured and defined, population characteristics if available, and time waited. We summarized information in tables and figures to synthesize information. Where possible, we have compared waiting time across similar types of waiting time and health systems.
Results
We identified 49 papers: 38 papers with data on waiting times, 15 with data on waiting time inequality, and 4 with data on both. All were published between 2000 and 2019. Studies ranged in size from 48 to aggregate health system data from over 23 million patients. Most studies drew on retrospectively captured data from the health system. Other studies utilized clinic databases or self-reported data from patients and physicians. Overall, the largest amount of data on waiting times was reported in papers from the United Kingdom and Australia, with some data from the United States, Canada, Germany, and other European and Asian countries.
ED Waiting Times
Information about ED waiting times was obtained from the United Kingdom, Australia, and Canada. The largest amount of publicly available information on this was identified from UK and Australian aggregate health system–reported data. Each country described waiting time differently. The primary measure of ED waiting time in the NHS is the percentage of patients spending 4 hours or less in ED. Conversely, the Canadian Institute for Health Information (CIHI) utilizes an overall measure of total time spent in ED and Australia the proportion of patients seen “on time” (Figure 2).
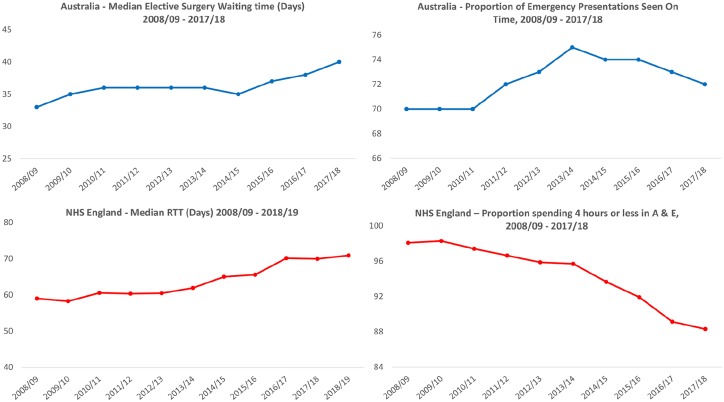
In NHS England, national registry data demonstrate the percentage of patients spending 4 hours or less in ED was at a low of 79.2% in 2002/2003.22 This improved to 98.3% in 2009/10,22 and has since fallen to 89.1% in 2016/201710 and further to 84.6% in 2018 (Figure 4).23
Figure 4.
Waiting-time trends in emergency departments and for elective surgery in Australia and NHS England, 2008/2009-2017/2018.1,6,9,10,22,26,83,84
Trends seem similar in Canada: A CIHI analysis of 11.2 million ED visits in national registries reported that in 2016/2017 ED, wait times in Canada (using a similar measure to the United Kingdom) was 17% higher than 5 years ago.24 In a subset analysis of 4547 Canadian responses to the 2016 Commonwealth Fund survey, 29% of Canadians reported waiting over 4 hours in the ED.25
In Australia, according to accessible registry data, the proportion of patients seen “on time” (Figure 2) has stayed fairly flat; 69% in 2007/2008,26 75% in 2013/2014,9 and 72% in 2017/20189 (Figure 4). The median waiting time in 2017/2018 was 18 minutes; however, the 90th percentile waiting time was 93 minutes, highlighting the variability in ED wait times.9
Elective Surgery Waiting Times
The Organisation for Economic Co-operation and Development (OECD) waiting-time studies in 2003 and 2013 present a detailed analysis of elective surgery waiting times from registry data in Australia, Canada, Denmark, Finland, Ireland, the Netherlands, New Zealand, Portugal, Spain, Sweden, and the United Kingdom (England and Scotland).7,27 Within this study, waiting-time burden differed significantly between country and specialty. Among countries reporting time from list addition to treatment, the Netherlands reported the lowest mean waiting time of approximately 1.5 months, compared with waiting times of greater than 2 months for most procedures in other countries.7 More urgent procedures, such as Percutaneous Coronary Intervention or Coronary Artery Bypass Grafts were associated with median waiting time less than a month compared with hip and knee replacement where median waiting times were over 2.5 months for all countries besides the Netherlands (mean time 46 and 44 d, respectively).7 Investigators also commented on sharp reductions in waiting time between 2006 and 2011 in the United Kingdom (>50%), Finland (20%-50%), and the Netherlands (> 50%).7 However, since 2010, these trends have reversed in the United Kingdom, Portugal, Spain, and Finland.7 To further investigate these trends and reports, we present recent registry data from the United Kingdom, Australia, Canada, and international comparative data from the Commonwealth Fund’s 2016 health policy survey (Table 1).
Table 1.
Waiting Time by Country and Health Service.
| Author and year of publication | Country | Population | Reported waiting time |
|---|---|---|---|
| Elective surgery | |||
| Registry data | |||
| Australian Institute of Health and Welfare (2018)6 | Australia | n = 874 000 elective surgeries | Median (no IQR) = 40 d, 90th percentile 237 d |
| NHS England (2019)1 | England | N = 3 586 090 RTT pathways | Median (no IQR) = 10.1 wk |
| Self-reported data | |||
| Commonwealth Fund Survey (2016)25 | Total: 3573 | <1 mo (%), 1-4 mo (%), 4 or more months (%), not sure/decline to answer (%) | |
| Australia | n = 683 | 56.8, 28.3, 8.4, 6.6 | |
| Canada | n = 557 | 34.8, 44.0, 18.2, 3.0 | |
| France | n = 173 | 51.4, 47.0, 1.6, 0.0, | |
| Germany | n = 124 | 39.0, 58.1, 0.0, 2.9 | |
| Netherlands | n = 99 | 48.9, 39.8, 4.5, 6.9 | |
| New Zealand | n = 141 | 43.3, 38.6, 14.9, 3.2 | |
| Norway | n = 208 | 37.0, 41.9, 15.3, 5.8 | |
| Sweden | n = 1015 | 37.3, 46.8, 11.8, 4.1 | |
| Switzerland | n = 219 | 59.3, 32.8, 6.5, 1.5 | |
| United Kingdom | n = 87 | 43.4, 31.8, 12.0, 12.8 | |
| United States | n = 268 | 61.0, 31.7, 3.6, 3.7 | |
| ED | |||
| Registry data | |||
| Australian Institute of Health and Welfare (2018)9 | Australia | n = 8 017 492 ED attendances | 72% of patients seen in clinically recommended time. Median wait for first clinical contact: 19 min 90th percentile time: 93 min |
| Canadian Institute for Health Information (2017)24 | Canada | 11 200 000 ED attendances | Total time spent in ED 17% higher than 5 y previous |
| NHS England (2019)10 | England | 23 800 000 A & E attendances | 88.0% of patients spent 4 h or less in A & E |
| Self-reported data | |||
| Canadian Institute for Health Information (2016)25 | Canada | 4547 | 29% of respondents report longer than 4 h waiting time |
| Primary care appointment | |||
| Registry data | |||
| NHS Digital (2019)31 | United Kingdom | 23 631 344 primary care appointments | |
| n = 9 915 851 | Same day (42.0%) | ||
| n = 1 628 141 | 1 d (6.9%) | ||
| n = 4 452 380 | 2-7 d (18.8%) | ||
| n = 3 309 500 | 8-14 d (14.0%) | ||
| n = 1 787 293 | 15-21 d (7.6%) | ||
| n = 1 258 471 | 22-28 d (5.3%) | ||
| n = 1 273 243 | More than 28 d (5.4%) | ||
| Practice server database | |||
| Sliwa and O’Kane (2011)33 | United Kingdom | 7000 primary care appointments | Mean (range) 3.4 (1-8) d |
| Self-reported data | |||
| Haggerty et al (2018)35 | Canada | 1029 primary care patients | 66.8% waiting longer than 2 wk |
| Luque Ramos et al (2018)34 | Germany | 4805 primary care patients | Mean (SD) 4.1 (10.2) d |
| Swami et al (2018)32 | Australia | 3651 primary care physicians | Mean (SD) 4.02 (5.60) d |
| Specialist care appointment | |||
| Registry data | |||
| Queensland Health (2019)2 | Australia | n = 58 398 patients referred for specialist care by their GP | Median 90th percentile category 2a across all specialties 180 d. range 61 (palliative care) to 565 d (neurosurgery). |
| South Australia Health (2019)4 | Australia | n = unknown patient referred for specialist care by their GP | Median wait across all specialties 5.9 mo, range 0 (cardiothoracic, breast) to 22.9 mo (ENT) |
| Tasmanian Health Service (2019)5 | Australia | n = unknown patients referred for specialist care by their GP | Median 75th percentile wait time across all specialties 234 d, range 8 (vascular) to 1520 d (neurosurgery) |
| Victorian Agency for Health Information (2019)3 | Australia | n = unknown patients referred for specialist care by their GP | Median, 17 d urgentb
56 d routinea |
| Self-reported data | |||
| Barua et al (2018)30 | Canada | n = 1718 specialist physicians | Median (no IQR) = 3.2 wk in 1993, 10.2 wk in 2016-2017 and 8.7 wk in 2017 |
| Carrière and Sanmartin (2010)36 | Canada | n = 5515 patients | Median (no IQR) = 4.3 wk, 13.9% > 3 mo |
| Siciliani and Verzulli (2009)37 | Europe | Total N = 2914 patients | Mean (no SD) wk: |
| Austria | n = 126 | 1.83 | |
| Denmark | n = 80 | 5.28 | |
| France | n = 147 | 3.14 | |
| Greece | n = 85 | 0.86 | |
| Germany | n = 371 | 1.84 | |
| Italy | n = 180 | 2.93 | |
| Netherlands | n = 268 | 3.47 | |
| Spain | n = 186 | 4.94 | |
| Sweden | n = 220 | 9.66 | |
| Waiting rooms | |||
| Automated time-stamp recording | |||
| Ahmad et al (2017)38 | Malaysia | n = 756 | Mean (no SD) = 41.06 min |
| Camacho et al (2006)39 | United States | n = 2444 | Mean (SD) = 20.97 (14.71) min |
| Kreitz et al (2016)48 | United States | n = 3125 | Mean (SD) = 27.3 (11.4) min |
| Mcmullen et al (2013)49 | United States | n = 104 | Mean (SD) = 43.0 (37.7) min |
| Patwardhan et al (2013)8 | United States | n = 1 167 885 | Mean (SD) = 18.4 (24.8) min |
| Physical patient shadowing | |||
| Xie and Or (2017)46 | Hong Kong | n = 49 | Mean (SD) = 150.5 (55.1) min |
| Self-reported data | |||
| Anderson et al (2007)50 | United States | n = 5030 | Mean (SD) = 25.2 (20.5) min |
| Arain et al (2013)47 | United Kingdom | n = 529 | Mean (SD) = 40.9 (32) min |
| n = 501 | Mean (SD) = 74 (49) min | ||
| Bleustein et al (2014)51 | United States | n = 9945 | Mean (SD) = 38.0 (61.1) min |
| McDevitt et al (2015)52 | United Kingdom | n = 111 | Median (range) = 22 (0-122) min |
| Patwardhan et al (2013)8 | United States | n = 1 128 990 | Mean (SD) = 21.40 (37.1) min |
| Rajpar et al (2000)53 | United Kingdom | n = 48 | Mean (no SD) = 1.17 h |
| Luque Ramos et al (2018)34 | Germany | n = 4805 | Mean (SD) = 30.8 (26.9) min |
| Allied health care appointment | |||
| National registry data | |||
| NHS Scotland (Q1 and Q2, 2019)40 | Scotland | Total, N = 11 112 | Percentage seen |
| n = 5218 | Less than 4 wk (47.0%) | ||
| n = 2139 | 4-8 wk (19.2%) | ||
| n = 1698 | 9-12 wk (15.3%) | ||
| n = 1274 | 13-16 wk (11.5%) | ||
| n = 783 | Greater than 16 wk (7.0%) | ||
| Database data | |||
| Deslauriers et al (2019)78 | Canada | n = 3665, Multidisciplinary Pain Treatment Facilities | Median (IQR) = 126 (50-297) d |
| Fell et al (2016)43 | England | n = 32 899, cardiac rehabilitation | Median = 39 d |
| Marzolini et al (2015)44 | Canada | n = 6497, cardiac rehabilitation | Median (IQR) = 80 (44) d |
| Mean (SD) = 101.1 (47.9) | |||
| Mean (SD) 1995-2000 = 104.3 (48.4) | |||
| Mean (SD) 2001-2006 = 97.3 (46.0) | |||
| Mean (SD) 2007-2012 = 100.2 (49.0) | |||
| Kirkbride et al (2017)45 | England | n = 798 patients waiting for early intervention psychosis services | Median (IQR) = 15 (7-30) d |
| Self-reported data | |||
| Deslauriers et al (2016)41 | Canada | n = 83 hospital-based physiotherapy clinics (mean [SD] patients per hospital = 192.1 [176.6]) | Median (range) = 4.6 (0-77.4) mo |
Note. IQR = interquartile range; RTT = referral to treatment; ED = emergency department; GP = general practitioner; ENT = ear, nose, throat.
Appointment required within 90 d.
Appointment required within 30 d.
In 2018/2019, NHS England reported on a total of 3 586 090 admitted care referral to treatment (RTT) pathways.1 According to publicly available registries, this measure of waiting time has dropped from a median of 17.5 weeks in April 2007 (the first month of measurement) to a low of 7.9 weeks in December 2008.1 Since then, RTTs have steadily climbed (Figure 4). The most recent median RTT was 10.3 weeks in March 2019. The overall RTT for 2018/2019 was 10.1 weeks.1
In 2017/2018, elective surgery was provided on approximately 874 000 occasions in Australian public hospitals.6 Waiting time registry data demonstrate wait times have steadily increased over the last 15 years, from 27 days in 2000/0128 to 38 days in 2016/201729 and 40 days in 2017/20186 (Figure 4).
In Canada, the Fraser institute has conducted a waiting time survey in 12 specialties and 10 provinces in Canada to document waiting time for specialists, diagnostic, and surgical procedures since 1993. In 2017, it reported wait-time median and ranges for hip and knee replacements of 27.5 (range = 18.0-52.0) weeks. The 2017 report concluded that the total waiting time for elective, medically necessary treatment is the longest recorded in the history of the survey.30
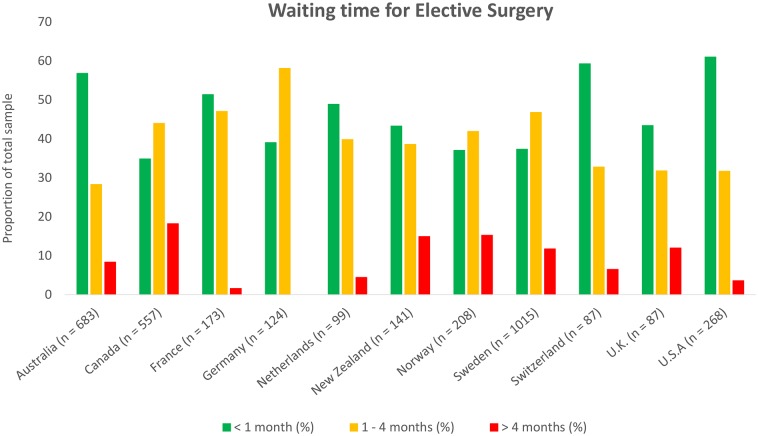
The Commonwealth Fund’s 2016 international survey interviewed 26 863 adults from Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, the United Kingdom, and the United States. Figure 5 presents responses from 3573 respondents to the question, “After you were advised that you needed surgery, how many weeks did you have to wait for the nonemergency or elective surgery?”25 Despite reduced sampling compared with registry-based data, the survey provides useful insight into international variance by using the same measure between countries. Canada, Germany, Norway, and Sweden all have a higher proportion of patients reporting waiting times of greater than 1 month than less than 1 month wait time. The proportion of patients reporting a wait longer than 4 months is highest in Canada (18.2%), followed by Norway (15.3%), New Zealand (14.9%), and the United Kingdom (12.0%).25
Figure 5.
Elective surgery waiting time between 11 countries. Data from the Commonwealth Fund’s 2016 survey.25
Waiting Times to Attend Primary Care
There are less data and less clarity with respect to waiting time as a performance measure in primary care. We identified 5 papers from 3 regions (Australia, Canada, and Europe). Sample sizes were substantial, ranging from 1029 to more than 23 million. Of the 5 studies, 3 used self-reported survey data from patients or physicians and 2 analyzed government or practice-based administrative data (Table 1).
The NHS has recently commenced reporting waiting time from appointment booking to completion. In May 2019, data were collected from more than 23 million appointments.31 During this month, 42.0% of patients received appointments on the same day as their booking. However, 32.3% of patients waited longer than a week for their primary care appointment.31 Besides this, the main data source is several ad hoc surveys. We noted that a waiting time close to 4 days for primary care appointment seemed average. A subanalysis of an Australian national survey of 3651 primary care doctors from 2008-2014 reported that patients wait an average (SD) of 4.0 (5.6) days for a primary care appointment.32 Sliwa and O’Kane33 analyzed approximately 7000 primary care appointments from 2 primary care clinics in Newcastle, England, over 1 month, reporting a mean (range) waiting time of 3.4 (1-8) days. Luque Ramos et al34 analyzed data from 4805 patient responses to a national survey conducted in Germany between 2011 and 2013 and reported a mean waiting time of 4.1 (10.2) days in primary care. There are also examples of outlier waiting times for primary care appointments, with 66.8% of participants in 1 Canadian study (n = 1029) reporting a waiting time of greater than 2 weeks (Table 1).35
Waiting Time to Attend a Specialist
We identified 7 studies that addressed specialist waiting times, of which 4 were from Australian state-based reports. In all states but Queensland, a sample size was not provided for the publicly available waiting time data. The 3 remaining studies consisted of physician- and patient-reported data from Canada and Europe (Table 1). Despite the significant variance between studies, data available suggest that waiting time to specialist access is high and increasing in some OECD countries.
In a subanalysis of the 2007 Canadian Community Health Survey, 13.9% of 5515 respondents reported waiting longer than 3 months for a specialist appointment (Table 1).36 The Canadian Fraser Institute surveys (n = 1718 physicians) suggest specialist waiting is increasing, reporting median waits of 3.2 weeks in 1993 and 8.7 weeks in 2017.30
Registry data from Australia show significant variation by state and specialty. In January to March 2019, Victoria Health reported a median waiting time of 56 days for routine appointments across all specialties.3 Other states stratified waiting time by specialty. South Australian median waiting time for routine appointments ranged from 0 to 22.9 months. The median wait time, calculated by combining reported medians across all specialties and centers, was 5.9 months.4 As of February 2019, The median 75th percentile wait time across all specialties and centers for nonurgent appointments in Tasmania was 234 days, ranging from 8 to 1520 days (Table 1).5 The median 90th percentile waiting time (January-March, 2019) reported by Queensland health across all specialties was 180 days, ranging from 61 to 565 days2 (Table 1). These times are all significantly longer than the reported median elective surgery waiting time in Australia (40 days),6 which only measures time from list addition by specialist to treatment initiation (Figure 3).
The SHARE study conducted in 2004 across multiple European countries (n = 2914) found a wide intercountry variation in self-reported data, from 0.86 weeks (n = 85) in Greece to 9.65 weeks (n = 220) in Sweden37 (Table 1).
Other Waiting Times
Waiting Time to Attend Allied Health Professional Services
In addition to medical care, many patients access the health system via allied health professional services. Here, we describe 6 large studies that highlight the access issues and waiting times for some allied health services mainly from the United Kingdom, Canada, and Australia (Table 1).
Some data indicate waiting time to access allied health professional–led care may also be an issue for many patients. NHS Scotland aims for 90% of patients attending musculoskeletal allied health professionals to be seen within 4 weeks.40 Yet, in an administrative report of 11 112 attendances in the first 6 months of 2019, only 47% of patients met this target.40 Other studies suggest patients are waiting even longer. Deslauriers et al41 describe data from 83 public hospitals providing physiotherapy services in Canada, reporting a median waiting time of 4.6 months from referral among patients currently on the waiting list (Table 1).
Many studies have highlighted poor attendance at cardiac rehabilitation after myocardial infarction.42 Waiting time may also be a barrier to entry to cardiac rehabilitation. Two large studies of appointment databases report a median waiting time in excess of 35 days (Fell et al43 reported a median waiting time from referral of 39 days among 32 899 patients in the United Kingdom from 2012-2015; Marzolini et al44 reported a waiting time from referral of 44 days, among 6497 patients in Canada, 1995-2012). Marzolini et al44 also describe the temporal trends that suggest waiting time between 2007 and 2012 was longer than 2001-2006 but shorter than the period 1995-2000 (Table 1).
Yet, waiting times appear to be favorable in other allied health-related settings. Kirkbride et al45 reported the lowest median waiting time among studies selected for 798 attendances to a multidisciplinary mental health clinic in the United Kingdom of 15 days (Table 1), close to the target waiting time for this service of 14 days.
Time Spent in Clinic Waiting Rooms
The actual time patients spend waiting in waiting rooms for treatment in EDs, clinics, or procedures is an important additional barrier to care. We identified 13 studies from Asia, Europe, and the United States that examined time patients spent in waiting rooms. Of the 13 studies, 5 used automated time-stamp methodology, 7 used self-reported time measures, and 1 study had researchers physically shadow patients through their clinic appointment46 (Table 1).
The largest study identified was performed in the United States by Patwardhan et al.8 They analyzed medical record data from walk-in clinics (n = 1 837 426) and self-reported data from primary care clinics (n = 1 128 990), finding an average (SD) waiting room time of 18.4 (24.8) and 21.4 (37.1) minutes, respectively.8 This was consistent with other US, European, and Asian studies that reported mean waiting room times from 20 to 40 minutes (Table 1).
Findings from Arain et al47 suggest that walk-in clinics providing care to patients without an appointment have significantly longer waiting times. In an evaluation of 2 walk-in primary care clinics in the United Kingdom, they found mean (SD) self-reported waiting times of 40.9 (32) minutes for 1 center (n = 529) and 74 (49) minutes for the other (n = 501).47 The low response rate of this study (57%) may reduce the generalizability of its findings, and further investigation in this setting is required to validate these findings.47
Hospital-based outpatient clinics report similar waiting time to primary care. Two US-based studies we identified found mean (SD) waiting room times of 27.3 (11.4) and 43.0 (37.7) minutes, respectively (Table 1).48,49 There are also examples of outlier mean (SD) waiting times from smaller studies in this setting of 150.5 (55.1) minutes and 1.2 (no SD) hours (Table 1).46,53
The large standard deviations reported in the above studies indicate that waiting time varies widely across multiple patient populations. However, what drives this variation is unclear and could be due to factors at patient, population, or health system level.
The Consequences of Increasing Wait Time
Worsening waiting times have been shown to be associated with patient dissatisfaction,54 delayed access to treatments,7 poorer clinical outcomes,55,56 increased costs,57 inequality,58,59 and patient anxiety.60 For patients with chronic health conditions, there may be a cumulative burden from waiting time. Patients with chronic disease may spend more time out of the workforce, which may contribute to worsening socioeconomic position. Socioeconomic deprivation is known to be associated with an increased burden of disease that increases health care resource utilization.61
Considering that waiting time should be allocated such that those in most clinical need experience the shortest waiting time, studies suggesting the socioeconomically disadvantaged wait for the longest time are particularly concerning.58,59,62-64
Socioeconomic Inequality and Waiting Time
In a recently conducted systematic review of 28 studies, Landi et al65 found only 7 of the 28 studies that do not describe a relationship between SES and waiting time. Siciliani66 also reviews data from country-level registries and selected studies that have demonstrated a significant interaction between waiting time and SES. However, the studies included in these reviews focused on waiting time for elective surgery and specialist appointments. We will describe some of the larger studies identified in these reviews with additional data from Australian national registries and recent studies by Deslauriers et al (2019)78, Hajizadeh,59 Kirkbride et al,45 Ray et al,63 Gallego et al79 and Marzolini et al44 that provide further insight into waiting time inequality in Australia, Canada, within the allied health sector, and the waiting room.We identified 15 studies that reported on the relationship between waiting time and SES. Of the 15 studies, 5 examined waiting time for elective surgery, primarily analyzing registry-based data; 4 examined waiting time for specialist and primary care, with 1 of the 4 studies utilizing registry-based data and 3 of the 4 studies analyzing their outcomes with self-reported data; 4 studies report on the effect of SES on waiting time in the allied health sector (Table 2); and 2 studies examined the impact of SES on waiting room time with self-reported outcome measures.
Table 2.
Observed Inequalities in Waiting Times by Country and Health Care Service.
| Author, year | Country | Population | Key waiting-time findings |
|---|---|---|---|
| Elective surgery | |||
| Registry data | |||
| Australian Institute of Health and Welfare (2017)29 | Australia | n = 11 000 000 hospitalizations | Lowest SES 9 d > highest SES Public 21 d > private Indigenous 8 d > non-Indigenous |
| Cooper et al (2009)64 | United Kingdom | n = 427 277 knee n = 406 253 hip n = 2 568 318 cataract From 1997-2007 |
1997-2000 (2005-2007) β coefficient (95% CI) knee, hip replacements and cataract repair between first and fifth deprivation quintiles: 6.23 (2.30-10.17) vs −2.74 (−4.99 to −0.99), 19.73 (16.33-23.12) vs 2.12 (0.23-4.02), 3.97 (2.78-5.16) vs −3.52 (−3.90 to −3.13) |
| Laudicella et al (2012)80 | United Kingdom | n = 33 709 hip surgery, England 2001 | Fourth and fifth lowest SES quintiles waited 6.51% and 7.45% longer than those in the first quintile, respectively. |
| Moscelli et al (2018)58 | United Kingdom | n ≥ 320 000 PCI and CABG patients, 2002-2011 | Difference between lowest and highest SES PCI (CABG) in years post 2005 (2007) minimum 10% (12%) |
| Tinghög et al (2014)82 | Sweden | n = 417 vascular n = 990 orthopedic n = 357 gynecology n = 204 urology n = 1792 ophthalmology n = 874 general surgery 2007 data |
Mean wait orthopedic: lowest 1/3 SES 150.6 d, highest 1/3
SES 143.2 d Mean wait general surgery: lowest 1/3 SES 139.2 d, highest 1/3 SES 125.5 d No significant differences for other surgeries. |
| Primary and specialist care | |||
| Registry data | |||
| Kaarboe et al (2014)18 | Norway | n = 611 414 2004-2005 |
Lowest SES men (women) wait 24% (11%) longer than highest
SES. Nil significant difference when hospital choice controls applied |
| Self-reported data | |||
| Australian Bureau of Statistics (2017)72 | Australia | n = 28 243 | 21% of lowest SES reported waiting longer than acceptable for GP appointment, 17% of highest SES |
| Hajizadeh (2018)59 | Canada | n = 266 962 2000/2001, 2003, 2005, 2010 |
Negative association between SES status and instance of not receiving care due to wait-time RC = −0.039 (95% CI = −0.049 to −0.028), AC = −0.067 (95% CI = −0.086 to −0.049]. |
| Siciliani and Verzulli (2009)37 | 10 000 Euro increase in salary, high education vs low education | ||
| Austria | n = 126 | 0.027 wk shorter wait (P > .05), 0.42 wk shorter wait (P > .05) | |
| Denmark | n = 80 | 0.22 wk shorter wait (P > .05), 0.826 wk shorter wait (P > .05) | |
| France | n = 147 | 0.021 wk shorter wait (P > .05), 1.03 wk shorter wait (P < .1) | |
| Greece | n = 85 | 0.046 wk shorter wait (P > .05), 0.34 wk shorter wait (P > .05) | |
| Germany | n = 371 | 0.15 wk shorter wait (P < .01), 0.061 wk shorter wait (P > .05) | |
| Italy | n = 180 | 0.083 wk longer wait (P > .05), 2.16 wk longer wait (P > .05) | |
| Netherlands | n = 268 | 0.043 wk longer wait (P > .05), 0.34 wk shorter wait (P > .05) | |
| Spain | n = 186 | 0.071 wk longer wait (P > .05), 3.55 wk shorter wait (P < .05) | |
| Sweden | n = 220 | 0.98 wk longer wait (P < .05), 0.36 wk shorter wait (P > .05) | |
| Waiting room time | |||
| Self-reported data | |||
| Jowsey et al (2018)68 | Australia | n = 427 diabetic, n = 681 COPD | Diabetic, COPD median (95% CI) = 1.7 (1.4-1.9), 3.0 (2.5-3.5) h each month, positive relationship between number of chronic diseases and monthly reported clinic time |
| Ray et al (2015)63 | United States | n = 3787 | Median (95% CI) min: Caucasian 80 (78-83) African American 99 (92-106) Hispanic 105 (97-113) <high school education, lowest income 91 (87-95), 80 (72-88) Graduate school, highest income 76 (71-72), 72 (65-78) |
| Allied health/multidisciplinary | |||
| Database data | |||
| Deslauriers et al (2019)78 | Canada | n = 3665 patients waiting for multidisciplinary pain treatment facility | Significant negative association between household income and waiting time (standardized β coefficient = −0.076) |
| Kirkbride et al (2017)45 | England | n = 798 patients waiting for early intervention psychosis services | No association between waiting time and sociodemographic status |
| Marzolini et al (2015)44 | Canada | n = 6497 patients attending cardiac rehabilitation | Neighborhood SES and waiting time (d) association: −0.80 (P < .001) |
| Self-reported data | |||
| Gallego et al (2017)79 | Australia | n = 166 carers of people with disability in rural areas | Mean (no SD) waiting time |
| Speech pathology | 6.6 mo | ||
| Occupational therapy | 5.6 mo | ||
| Psychology | 4.7 mo | ||
| Physiotherapy | 4.5 mo | ||
Note. SES = socioeconomic status; CI = confidence interval; PCI = percutaneous coronary intervention; CABG = coronary artery bypass surgery; GP = general practitioner; RC = relative concentration index; AC = absolute concentration index; COPD = chronic obstructive pulmonary disease.
Patients with chronic disease frequently access health care. Several studies suggest they have a substantial amount of waiting time,58,59,62-64 which consistently exceeds the time spent with a health care professional and increases with greater chronic disease burden.67-70 However, the degree to which SES affects waiting time is less clear.
Multiple socioeconomic inequities in waiting time for elective surgery have been observed in Australia. For example, in 2016/2017, registry data reports demonstrated Australian public hospital patients waited 21 days longer on average for elective surgery than those in private hospitals.71 Median waiting time within public hospitals (n = 748 000) was 9 days longer for those living in the lowest SES postcodes than highest,61 and Indigenous Australians waited 8 days longer than non-Indigenous Australians.6,29 In the ED, Indigenous Australians wait a similar time to non-Indigenous Australians.9 However, shorter waiting times in outer regional and remote areas of Australia compared with the inner city may have influenced these findings.
In the primary care setting, 19% of respondents to the 2017-2018 Patient Experiences in Australia survey (n = 28 243) reported waiting longer than acceptable for a general practitioner appointment.72 This figure was numerically higher in the lowest SES quintile (21%) than the highest (17%), although no P value was reported.72
Similar findings have been reported in other countries. Hajizadeh59 analyzed data from Canadian community health surveys (2000/2001, 2003, 2005 and 2010, n = 266 962). Comparing reported instance of not receiving care due to wait time and household income, they calculated the previously described73 relative and absolute concentration indices. These indicated low-SES patients were disproportionately represented among those who reported an instance of not receiving care due to wait time (Table 2). Moscelli et al58 examined waiting time for more than 320 000 percutaneous coronary intervention and coronary artery bypass graft procedures performed between 2002 and 2011 in the United Kingdom. Despite a reduction over time, SES had a statistically significant effect on waiting time in every year of analysis (Table 2).58
There are multiple review papers that describe the interaction between waiting time for allied health services and clinical outcomes;74-77 however, there is little evidence available on whether these times are affected by SES. We identified 4 studies that describe waiting-time inequality in the allied health sector. Of the 4 studies, 2 studies identified a significant association between waiting time and household income and/or78 neighborhood SES;44 however, the magnitude of association was small (β = −0.076 and r = −0.080, Table 1).44,78 While not describing a direct association between waiting time and SES, Gallego et al79 highlight the lengthy waiting times experienced by minority groups. In a survey of 166 carers of people with disability in rural Australia, they report waiting times ranging from 4.5 months for physiotherapy to 6.6 months for speech pathology, significantly longer than studies described in Table 1. Conversely, Kirkbride et al45 performed a detailed evaluation of waiting times for 798 attendees of a multidisciplinary early intervention in psychosis clinic and found no association between multiple sociodemographic factors.
This socioeconomic inequity appears to persist in the waiting room. Ray et al63 performed a subanalysis of 3787 respondents to the American Time Use Survey. Among respondents who reported their clinic time during the 24-hour assessment period, a median (95% CI) of 86 [83-88] minutes was spent in-clinic.63 Those in the lowest income quartile reported a mean [95% CI] clinic time of 91 [87-95] minutes compared with those in the highest income quartile, who reported a mean clinic time of 72 [65-78] minutes.63
Disproportionate ill health in lower SES patients has consistently been rejected as an explanation for this gradient.18,80 Some studies indicate it could be driven by lack of supply to lower SES areas and patients.58,81 However, Moscelli et al58 only attributed 12% of the wait difference between first and fifth quintile SES to hospital choice, highlighting the variation of contributing factors between countries.
Other studies report significant reductions or even positive SES-wait time inequity. Cooper et al64 analyzed wait time for elective knee (n = 427 277), hip (n = 406 253), and cataract (n = 2 568 318) surgery in the United Kingdom between 1997 and 2007. Between 1997 and 2000, low-SES patients waited significantly longer than higher SES patients for all surgeries (Table 2).64 However, by 2005 to 2007, the magnitude of this relationship had reduced significantly for hip repair, and for knee replacement and cataract, repair had reversed such that lower SES patients had a shorter waiting time than higher SES patients (Table 2). Similarly, in an analysis of data from the SHARE study, Siciliani and Verzulli37 found that in Sweden, an increase of 10 000 Euros in household income was associated with a 1 week increase in waiting time for specialist consultation. However, this was from a sample of 220 participants, relied on self-reported data, and other countries in the study demonstrated a negative relationship between educational attainment and waiting time (Table 2).37 A larger (n = 4634) study of 2007 registry elective surgery waiting-time data in Sweden demonstrated a 27% (34%) higher wait time for the lowest income third compared with the highest third for orthopedic (general surgery).82 The same study found no significant differences across several other surgical specialties (Table 2).
Discussion and Policy Implications
Despite significant reductions between the 1990s and early 2000s in some countries,7 the time patients wait to receive care has either increased or remained unchanged over the last 5 to 10 years.7,23,29,72,83 For elective surgery, waiting times of greater than a month from referral are the norm. Similar trends are apparent in the ED. In the United Kingdom, ED waiting times have deteriorated to become “the worst on record” in 2018.23 Same day access to primary care is rare, with most data suggesting an average of 4 days to access primary care.32-34 There are even less data and clarity between countries and specialties to ascertain time to first contact of a specialist. Some surveys suggest patients wait in excess of 6 months,2,4 and some data suggest this is increasing.30 There is limited national reporting of waiting in the allied health sector; however, waiting times for these services appears to be shorter than for medical specialists.44
Patients access multiple health services, and this review highlights that waiting for health care is likely to be a substantial burden affecting many people and aspects of our health care systems. The increasing prevalence of chronic disease globally suggests this burden will likely increase,84 affecting a larger patient population each day. If waiting is an unavoidable part of health care, we need to innovate to address whether it can be decreased or utilized to better effect.
This review also affirms findings from Landi et al65 and Siciliani66 regarding the relationship between SES and waiting time. This is particularly concerning in publicly funded health systems where service delivery is intended to be dependent on need rather than the ability to pay. Evidence that this trend is reversing in some countries is encouraging;37,58,64 however, further longitudinal investigation of trends is required to understand whether this is indeed the case.
Global efforts to reduce waiting time through health policy have traditionally focused on time to elective procedures after referral and ED waiting time.7,29,72,85 However, this method of measurement fails to recognize and/or hides other types of waiting times, including time waiting for primary care, specialist medical care, allied health appointments, and time spent physically waiting in waiting rooms. We need greater transparency regarding the range of types of waiting for health services, and systematic enquiry into the reasons or potential targets for interventions. In addition, a lack of routine reporting of data by age, sex, SES, and co-morbidity limits the ability to determine what drives the variability around each of these waiting-time measures.
Some academics argue that reductions achieved in the early 2000s were a case of “hitting the target, but missing the point”86 and due to managerial gaming of the system, rather than real reductions in waiting time.15 Mayhew and Smith16 present an interesting model that demonstrates it would have been impossible for hospitals to meet 98% 4-hour targets without “re-designating” some patients from admitted status to be discharged prematurely. There is also lack of evidence to support what is an unsafe level of waiting.
Waiting time remains a hot-button issue of health policy. In March 2019, the NHS announced they are planning to replace 4-hour targets with flexible objectives that are aligned to time to first clinical contact, similar to Australia.87 However, as outlined earlier in this article, Australian waiting times as measured by this parameter have remained largely unchanged over the last 20 years. As our ability to reduce waiting times through policy diminishes, allocating resources toward a principle of a “productive wait” through better utilization of patient time could be a viable approach for policy makers.
Conclusions
Waiting time for elective surgery and ED care has increased significantly in the last 10 years.
Waiting time is less well characterized for primary care, specialist care, allied health appointments, and time spent in waiting rooms, but existing literature indicates waiting time in these settings also contributes to a significant health care access issue. Policy measures have been moderately effective to limit growth in emergency and surgical wait times. But greater transparency, systematic reporting, and innovation in the model of health care delivery are needed to address the important issue of waiting as a barrier to health care access. In addition, the repeated identification of an adverse associa-tion between socioeconomic disadvantage and waiting time requires closer scrutiny. As health is a human right, addressing the further inequity from poorer health care access experienced by the most vulnerable in our system must be a policy and implementation priority. Further research should focus on better characterizing these barriers to care to assist government in designing effective policy and examining the potential to utilize this time to deliver health care interventions that could improve patient outcomes.
Footnotes
Author Contributions: D.M. and C.K.C. formulated the initial idea and the study questions. D.M. performed the literature review and wrote the first draft of the article. C.K.C. is D.M.’s supervisor. C.K.C. provided critical review of the article and is guarantor.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: C.K.C. is supported by a National Health and Medical Research Council of Australia Career Development Fellowship co-sponsored by the National Heart Foundation of Australia.
ORCID iD: Daniel McIntyre  https://orcid.org/0000-0003-4854-4050
https://orcid.org/0000-0003-4854-4050
References
- 1. NHS England. Consultant-led Referral to Treatment Waiting Times Data 2018-2019. Consultant-led Referral to Treatment Waiting Times https://www.england.nhs.uk/statistics/statistical-work-areas/rtt-waiting-times/rtt-data-2018-19/. Published 2019. Accessed July 2, 2019.
- 2. Queensland Health. Queensland Reporting Hospitals Specialist Outpatient. Brisbane, Australia: Queensland Health; 2019. [Google Scholar]
- 3. Victorian Agency for Health Information. Statewide—Median Wait Time for Urgent Specialist Clinic Appointment—All Specialties—Quarterly Data. Melbourne, Australia: Victorian Agency for Health Information; 2019. [Google Scholar]
- 4. South Australia Health. Specialist Outpatient Waiting Time Report (Third Release). Adelaide, Australia: South Australia Health; 2019. [Google Scholar]
- 5. Tasmanian Health Service. Estimated Outpatient Waiting Times. Hobart, Australia: Tasmanian Health Service; 2019. [Google Scholar]
- 6. Australian Institute of Health and Welfare. Elective Surgery Waiting Times 2017/18. 88th ed. Canberra: Australian Institute of Health and Welfare; 2018. [Google Scholar]
- 7. Siciliani L, Moran V, Borowitz M. Measuring and comparing health care waiting times in OECD countries. Health Policy. 2014;118(3):292-303. [DOI] [PubMed] [Google Scholar]
- 8. Patwardhan A, Davis J, Murphy P, Ryan SF. Comparison of waiting and consultation times in convenient care clinics and physician offices: a cross-sectional study. J Prim Care Community Health. 2013;4(2):124-128. [DOI] [PubMed] [Google Scholar]
- 9. Australian Institute of Health and Welfare. Emergency Department Care 2017-2018. Canberra: Australian Institute of Health and Welfare; 2018. [Google Scholar]
- 10. NHS England. Hospital Accident and Emergency Activity, 2018-2019. London, England: NHS England; 2019. [Google Scholar]
- 11. Smith PC, Mossialos E, Papanicolas I, Leatherman S. Performance Measurement for Health System Improvement: Experiences, Challenges and Prospects. Copenhagen, Denmark: World Health Organization; 2009. [Google Scholar]
- 12. Australian Institute of Health and Welfare. MyHospitals Overview. https://www.myhospitals.gov.au/about-myhospitals/overview. Published 2018. Accessed June 26, 2019.
- 13. Anandaciva S. What Does the NHS England Review of Waiting Times Mean for Accident and Emergency Departments? The Kings Fund; https://www.kingsfund.org.uk/publications/nhs-england-review-waiting-times-accident-emergency. Published 2019. Accessed June 26, 2019. [Google Scholar]
- 14. Miller P. Survey of Physician Appointment Wait Times and Medicare and Medicaid Acceptance Rates. Dallas, TX: Merritt Hawkins; 2017. [Google Scholar]
- 15. Gubb J, Bevan G. Have targets done more harm than good in the English NHS? BMJ. 2009;338(7692):442-443. [DOI] [PubMed] [Google Scholar]
- 16. Mayhew L, Smith D. Using queuing theory to analyse the government’s 4-H completion time target in accident and emergency departments. Health Care Manag Sci. 2008;11(1):11-21. [DOI] [PubMed] [Google Scholar]
- 17. Viberg N, Forsberg BC, Borowitz M, Molin R. International comparisons of waiting times in health care—Limitations and prospects. Health Policy. 2013;112(1-2):53-61. [DOI] [PubMed] [Google Scholar]
- 18. Kaarboe O, Carlsen F. Waiting times and socioeconomic status. Evidence from Norway. Health Econ. 2014;23(1):93-107. [DOI] [PubMed] [Google Scholar]
- 19. Wang H, Naghavi M, Allen C, et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1459-1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Oliver D. David Oliver: Can the extra funds for the NHS really transform care? BMJ. 2018;362:k3248. [DOI] [PubMed] [Google Scholar]
- 21. Iacobucci G. Waiting list for elective surgery tops four million for first time since 2007. BMJ. 2017;358:j3861. [DOI] [PubMed] [Google Scholar]
- 22. NHS England. Archive—Total Time Spent in Accident and Emergency. https://webarchive.nationalarchives.gov.uk/20130105020054/http://www.dh.gov.uk/en/Publicationsandstatistics/Statistics/Performancedataandstatistics/AccidentandEmergency/DH_087978. Published 2013. Accessed December 3, 2018.
- 23. Torjesen I. Latest waiting time figures for emergency departments in England are worst on record. BMJ. 2018;361:k1658. [DOI] [PubMed] [Google Scholar]
- 24. Canadian Institute for Health Information. Emergency Department Wait Times in Canada Continue to Rise. Ottawa, Ontario: Canadian Institute for Health Information; 2017. [Google Scholar]
- 25. Canadian Institute for Health Information. How Canada Compares: Results from The Commonwealth Fund’s 2016 International Health Policy Survey of Adults in 11 Countries—Accessible Report. Ottawa, Ontario: Canadian Institute for Health Information; 2016. [Google Scholar]
- 26. Australian Institute of Health and Welfare. Australian Hospital Statistics 2011-2012: Emergency Department Care. 45th ed. Canberra: Australian Institute of Health and Welfare; 2012. [Google Scholar]
- 27. OECD. Waiting Time Policies in the Health Sector. Paris, France: OECD; 2013. [Google Scholar]
- 28. Willcox S, Seddon M, Dunn S, Edwards RT. Measuring and reducing waiting times: a cross-national comparison of strategies. Health Aff (Millwood). 2007;26(4):1078-1087. [DOI] [PubMed] [Google Scholar]
- 29. Australian Institute of Health and Welfare. Elective Surgery Waiting Times 2016-2017: Australian Hospital Statistics. 82nd ed. Canberra: Australian Institute of Health and Welfare; 2017. [Google Scholar]
- 30. Barua B, Jacques D, Collyer A. Waiting Your Turn: Wait Times for Health Care in Canada, 2018 Report. Vancouver, British Columbia, Canada: Fraser Institute; 2018. [Google Scholar]
- 31. NHS Digital. Appointments in General Practice, May 2019. London, England: National Health Service; 2019. [Google Scholar]
- 32. Swami M, Gravelle H, Scott A, Williams J. Hours worked by general practitioners and waiting times for primary care. Health Econ. 2018;27(10):1513-1532. [DOI] [PubMed] [Google Scholar]
- 33. Sliwa M, O’Kane J. Service quality measurement: appointment systems in UK GP practices. Int J Health Care Qual Assur. 2011;24(6):441-452. [DOI] [PubMed] [Google Scholar]
- 34. Luque Ramos A, Hoffmann F, Spreckelsen O. Waiting times in primary care depending on insurance scheme in Germany. BMC Health Serv Res. 2018;18(1):191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Haggerty J, Fortin M, Breton M. Snapshot of the primary care waiting room: informing practice redesign to align with the Patient’s Medical Home model. Can Fam Physician. 2018;64(9):e407-e413. [PMC free article] [PubMed] [Google Scholar]
- 36. Carrière G, Sanmartin C. Waiting time for medical specialist consultations in Canada, 2007. Health Rep. 2010;21(2):7-14. [PubMed] [Google Scholar]
- 37. Siciliani L, Verzulli R. Waiting times and socioeconomic status among elderly Europeans: evidence from SHARE. Health Econ. 2009;18(11):1295-1306. [DOI] [PubMed] [Google Scholar]
- 38. Ahmad BA, Khairatul K, Farnaza A. An assessment of patient waiting and consultation time in a primary healthcare clinic. Malaysian family physician: the official journal of the Academy of Family Physicians of Malaysia. 2017; 12(1):14-21. [PMC free article] [PubMed] [Google Scholar]
- 39. Camacho F, Anderson R, Safrit A, Jones AS, Hoffmann P. The relationship between patient’s perceived waiting time and office-based practice satisfaction. North Carolina Medical Journal. 2006; 67(6): 409-413. [PubMed] [Google Scholar]
- 40. NHS Scotland. Allied Health Professionals—Musculoskeletal Waiting Times. NHS Scotland; https://www.opendata.nhs.scot/dataset/allied-health-professionals-musculoskeletal-waiting-times. Published 2019. Accessed November 19, 2019. [Google Scholar]
- 41. Deslauriers S, Raymond M-H, Laliberté M, et al. Access to publicly funded outpatient physiotherapy services in Quebec: waiting lists and management strategies. Disabil Rehabil. 2017;39(26):2648-2656. [DOI] [PubMed] [Google Scholar]
- 42. Redfern J, Chow CK. Secondary prevention of coronary heart disease in Australia: a blueprint for reform. Med J Aust. 2013;198(2):70-71. [DOI] [PubMed] [Google Scholar]
- 43. Fell J, Dale V, Doherty P. Does the timing of cardiac rehabilitation impact fitness outcomes? An observational analysis. Open Heart. 2016;3(1):e000369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Marzolini S, Blanchard C, Alter DA, Grace SL, Oh PI. Delays in referral and enrolment are associated with mitigated benefits of cardiac rehabilitation after coronary artery bypass surgery. Circ Cardiovasc Qual Outcomes. 2015;8(6):608-620. [DOI] [PubMed] [Google Scholar]
- 45. Kirkbride JB, Hameed Y, Wright L, et al. Waiting time variation in Early Intervention Psychosis services: longitudinal evidence from the SEPEA naturalistic cohort study. Soc Psychiatry Psychiatr Epidemiol. 2017;52(5):563-574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Xie Z, Or C. Associations between waiting times, service times, and patient satisfaction in an endocrinology outpatient department: a time study and questionnaire survey. Inquiry. 2017;54:46958017739527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Arain M, Nicholl J, Campbell M. Patients’ experience and satisfaction with GP led walk-in centres in the UK: a cross sectional study. BMC Health Serv Res. 2013;13:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kreitz TM, Winters BS, Pedowitz DI. The influence of wait time on patient satisfaction in the orthopedic clinic. J Patient Exp. 2016;3(2):39-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. McMullen M, Netland PA. Wait time as a driver of overall patient satisfaction in an ophthalmology clinic. Clin Ophthalmol. 2013;7:1655-1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Anderson RT, Camacho FT, Balkrishnan R. Willing to wait?: the influence of patient wait time on satisfaction with primary care. BMC Health Services Research. 2007; 7:31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Bleustein C, Rothschild DB, Valen A, Valatis E, Schweitzer L, Jones R. Wait times, patient satisfaction scores, and the perception of care. The American Journal of Managed Care. 2014; 20(5): 393. [PubMed] [Google Scholar]
- 52. McDevitt J, Melby V. An evaluation of the quality of Emergency Nurse Practitioner services for patients presenting with minor injuries to one rural urgent care centre in the UK: a descriptive study. Journal of Clinical Nursing. 2015; 24(3-4): 523-535. [DOI] [PubMed] [Google Scholar]
- 53. Rajpar SF, Smith MA, Cooke MW. Study of choice between accident and emergency departments and general practice centres for out of hours primary care problems. J Accid Emerg Med. 2000;17(1):18-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Nottingham QJ, Johnson DM, Russell RS. The effect of waiting time on patient perceptions of care quality. Qual Manag J. 2018;25(1):32-45. [Google Scholar]
- 55. Moscelli G, Siciliani L, Tonei V. Do waiting times affect health outcomes? Evidence from coronary bypass. Soc Sci Med. 2016;161:151-159. [DOI] [PubMed] [Google Scholar]
- 56. Reichert A, Jacobs R. The impact of waiting time on patient outcomes: Evidence from early intervention in psychosis services in England. Health Econ. 2018;27(11):1772-1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ray KN, Chari AV, Engberg J, Bertolet M, Mehrotra A. Opportunity costs of ambulatory medical care in the United States. Am J Manag Care. 2015;21(8):567-574. [PMC free article] [PubMed] [Google Scholar]
- 58. Moscelli G, Siciliani L, Gutacker N, Cookson R. Socioeconomic inequality of access to healthcare: Does choice explain the gradient? J Health Econ. 2018;57:290-314. [DOI] [PubMed] [Google Scholar]
- 59. Hajizadeh M. Does socioeconomic status affect lengthy wait time in Canada? Evidence from Canadian Community Health Surveys. Eur J Health Econ. 2018;19(3):369-383. [DOI] [PubMed] [Google Scholar]
- 60. Lizaur-Utrilla A, Martinez-Mendez D, Miralles-Munoz FA, Marco-Gomez L, Lopez-Prats FA. Negative impact of waiting time for primary total knee arthroplasty on satisfaction and patient-reported outcome. Int Orthop. 2016;40(11):2303-2307. [DOI] [PubMed] [Google Scholar]
- 61. Pathirana TI, Jackson CA. Socioeconomic status and multimorbidity: a systematic review and meta-analysis. Aust N Z J Public Health. 2018;42(2):186-194. [DOI] [PubMed] [Google Scholar]
- 62. Bahler C, Huber CA, Brungger B, Reich O. Multimorbidity, health care utilization and costs in an elderly community-dwelling population: a claims data based observational study. BMC Health Serv Res. 2015;15:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Ray KN, Chari AV, Engberg J, Bertolet M, Mehrotra A. Disparities in time spent seeking medical care in the United States. JAMA Intern Med. 2015;175(12):1983-1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Cooper ZN, McGuire A, Jones S, Le Grand J. Equity, waiting times, and NHS reforms: retrospective study. BMJ. 2009;339:b3264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Landi S, Ivaldi E, Testi A. Socioeconomic status and waiting times for health services: An international literature review and evidence from the Italian National Health System. Health Policy. 2018;122(4):334-351. [DOI] [PubMed] [Google Scholar]
- 66. Siciliani L. Waiting times: evidence of social inequalities in access for care. In: Sobolev B, Levy A, Goring S, eds. Data and Measures in Health Services Research. Boston, MA: Springer; 2015:1-17. [Google Scholar]
- 67. Einarsdóttir K, Preen DB, Emery JD, Kelman C, Holman CD. Regular primary care lowers hospitalisation risk and mortality in seniors with chronic respiratory diseases. J Gen Intern Med. 2010;25(8):766-773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Jowsey T, McRae IS, Valderas JM, et al. Time’s up. Descriptive epidemiology of multi-morbidity and time spent on health related activity by older Australians: a time use survey. PLoS ONE. 2013;8(4):e59379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Jowsey T, Yen LE, Bagheri N, McRae IS. Time spent by people managing chronic obstructive pulmonary disease indicates biographical disruption. Int J Chron Obstruct Pulmon Dis. 2014;9:87-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Yen LE, McRae IS, Jowsey T, Bagheri N. Time spent on health related activity by older Australians with diabetes. J Diabetes Metab Disord. 2013;12:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Australian Institute of Health and Welfare. Australian Hospitals 2016-2017 at a Glance. 85th ed. Canberra: Australian Institute of Health and Welfare; 2018. [Google Scholar]
- 72. Australian Bureau of Statistics. Patient Experiences in Australia—Summary. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4839.0~2016-17~Main%20Features~General%20practitioners~2. Published 2017. Accessed November 22, 2017.
- 73. Wagstaff A, Paci P, van Doorslaer E. On the measurement of inequalities in health. Soc Sci Med. 1991;33(5):545-557. [DOI] [PubMed] [Google Scholar]
- 74. Lewis AK, Harding KE, Snowdon DA, Taylor NF. Reducing wait time from referral to first visit for community outpatient services may contribute to better health outcomes: a systematic review. BMC Health Serv Res. 2018;18(1):869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Lynch ME, Campbell F, Clark AJ, et al. A systematic review of the effect of waiting for treatment for chronic pain. Pain. 2008;136(1-2):97-116. [DOI] [PubMed] [Google Scholar]
- 76. Deslauriers S, Déry J, Proulx K, et al. Effects of waiting for outpatient physiotherapy services in persons with musculoskeletal disorders: a systematic review [published online ahead of print July 14, 2019]. Disabil Rehabil. doi: 10.1080/09638288.2019.1639222. [DOI] [PubMed] [Google Scholar]
- 77. Miller AR, Armstrong RW, Mâsse LC, Klassen AF, Shen J, O’Donnell ME. Waiting for child developmental and rehabilitation services: an overview of issues and needs. Dev Med Child Neurol. 2008;50(11):815-821. [DOI] [PubMed] [Google Scholar]
- 78. Deslauriers S, Roy JS, Bernatsky S, et al. Factors associated with waiting times for persons with rheumatic conditions in multidisciplinary pain treatment facilities. J Pain Res. 2019;12:2379-2390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Gallego G, Dew A, Lincoln M, et al. Access to therapy services for people with disability in rural Australia: a carers’ perspective. Health Soc Care Community. 2017;25(3):1000-1010. [DOI] [PubMed] [Google Scholar]
- 80. Laudicella M, Siciliani L, Cookson R. Waiting times and socioeconomic status: evidence from England. Soc Sci Med. 2012;74(9):1331-1341. [DOI] [PubMed] [Google Scholar]
- 81. Johar M, Jones G, Keane MP, Savage E, Stavrunova O. Discrimination in a universal health system: Explaining socioeconomic waiting time gaps. J Health Econ. 2013;32(1):181-194. [DOI] [PubMed] [Google Scholar]
- 82. Tinghög G, Andersson D, Tinghög P, Lyttkens CH. Horizontal inequality in rationing by waiting lists. Int J Health Serv. 2014;44(1):169-184. [DOI] [PubMed] [Google Scholar]
- 83. OECD. Health at a Glance 2017. Paris, France: OECD; 2017. [Google Scholar]
- 84. Kingston A, Robinson L, Booth H, Knapp M, Jagger C. Projections of multi-morbidity in the older population in England to 2035: estimates from the Population Ageing and Care Simulation (PACSim) model. Age Ageing. 2018;47(3):374-380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Reddy S, Jones P, Shanthanna H, Damarell R, Wakerman J. A systematic review of the impact of healthcare reforms on access to emergency department and elective surgery services: 1994-2014. Int J Health Serv. 2017;48(1):81-105. [DOI] [PubMed] [Google Scholar]
- 86. Mason S, Weber EJ, Coster J, Freeman J, Locker T. Time patients spend in the emergency department: England’s 4-hour rule—A case of hitting the target but missing the point? Ann Emerg Med. 2012;59(5):341-349. [DOI] [PubMed] [Google Scholar]
- 87. Iacobucci G. NHS is to test scrapping the four hour A&E target. BMJ (Clinical Research Ed). 2019;364:l1148. [DOI] [PubMed] [Google Scholar]
- 88. Australian Institute of Health and Welfare. Australian Hospital Statistics 2011-12: Elective Surgery Waiting Times. 60th ed., Cat No. HSE 127. Canberra: Australian Institute of Health and Welfare; 2012. [Google Scholar]
- 89. NHS England. Hospital Accident and Emergency Activity: Supporting Information, 2016-2017. London, England: NHS England; 2017. [Google Scholar]