Abstract
Objective:
Sleep, physical activity, and social domains of biological rhythm disruptions may have specific effects on the symptom cluster and severity of depression. However, there is a lack of structured clinical evaluation to specify the domains of biological rhythms in patients with depression.
Methods:
Ninety drug-naïve subjects with depression and 91 matched healthy controls were recruited for the study. The severity of depression was examined with the Hamilton Rating Scale for Depression (HRSD), while biological rhythm was evaluated using the Biological Rhythms Interview of Assessment in Neuropsychiatry (BRIAN).
Results:
Patients with depression showed significantly greater biological rhythm disturbances than healthy controls in all domains of BRIAN (sleep, activity, social, and eating). BRIAN-Total correlated positively with HRSD-Total and HRSD-Total without sleep cluster. The sleep and activity domains correlated significantly with HRSD-Total score. Additionally, the sleep, activity, and social domains correlated significantly with HRSD-Total without the sleep cluster score. Regression analysis revealed the activity (β = 0.476, t = 5.07, p<0.001) and sleep (β = 0.209, t = 2.056, p = 0.043) domains may predict HRSD-Total score.
Conclusion:
Consideration of biological rhythm domains in clinical examination and focusing on the sleep and activity domains may hold promise for the management of depression.
Keywords: Biological rhythm, depression, BRIAN, physical activity
Introduction
Depression is a chronic and a recurring disorder1 with a wide range of manifestations, from psychological suffering and disability in functioning to poor physical health.2-4 Depression is one of the leading causes of disability worldwide, with a lifetime prevalence between 6.5 to 21.0% in adults,5 and is predicted to be the second largest contributor to the global burden of disease by the year 2020.6 Burton et al.7 showed that patients with depression performed less daytime motor activity than healthy controls and experienced disruptions of biological rhythm. Recent reviews of adult studies have demonstrated the effectiveness of physical activity interventions in reducing depressive symptoms, with moderate to large effect sizes.8-10 One such study showed that engaging in physical activity at levels recommended for general health at leisure-time may reduce the risk of elevated anxiety symptoms.11 Exercise was also found to be particularly supportive as a potential treatment or stabilizer of mood and cognitive function in older adults with insufficient response or intolerance to pharmacotherapy.12
Circadian rhythm disruptions are well-known traits of mood disorders, and their effect often relates to indicators of clinical severity of depression.13 It was recently shown that circadian/biological rhythm may be associated with the development, progression, or relapse of mood disorders, including depression and seasonal affective disorder. Moreover, chronic sleep deprivation has a role in the development of mood-related problems, and is implicated in the molecular and cellular processes that underlie mood disorders.14 According to the current literature, disruptions of biological rhythm present as variations in both endogenous and exogenous rhythms, as well as sleep/wake cycle, appetite, sociality, and activities.15 Mounting evidence indicates that the dopaminergic and serotonergic system respond reciprocally to sleep and circadian rhythm.16 However, the role of domains of biological rhythm in major depression has not been investigated individually and sufficiently in the literature. Furthermore, specific domains of biological rhythm – sleep, activity, sociality and eating – may have specific effects on the severity of depression. Therefore, they should be considered in the clinical management of major depressive disorder (MDD).
Giglio et al.17 have developed the Biological Rhythms Interview of Assessment in Neuropsychiatry (BRIAN) to investigate the severity of disruptions in domains of biological rhythm in mood disorders. BRIAN was validated in patients with mood disorders and provides comprehensive data. Studies using this instrument found that biological rhythm disturbances influence psychosocial functioning,18 the severity of depression,19 and quality of life20 in patients with mood disorders. A recent study assessed the disruption of biological rhythm in a community sample of young adults with mood disorders (major depression and bipolar disorder),21 while others were conducted including only patients with bipolar disorder.18-20 However, there is a lack of research evaluating the relationship between severity of symptoms and domains of biological rhythm in patients with major depression.
Therefore, this study was designed to investigate biological rhythm disruption in patients with major depression matched with healthy controls; to ascertain which domain of biological rhythm is most involved in MDD; and whether the severity of depression could be predicted by any domain of biological rhythm.
Methods
Participants
The subjects of the study were 90 drug-naïve patients with depression (65 women, 25 men; age 41.5±10.7 years, range 17 to 65 years) and 91 healthy controls matched by age, gender, body mass index (BMI), education, and employment (63 women, 28 men; age 39.3±7.8 years, range 17 to 65 years). All were recruited by consecutive sampling at the Bezmialem Vakif University Outpatient Clinic in İstanbul (latitude 41°1′N; longitude 28°56′ E) from November 2015 to March 2017. The inclusion criteria for the patient group were age between 18 and 65 years, meeting criteria for MDD as assessed by the Structured Clinical Interview for DSM-IV Axis Disorders Patient Version (SCID-I),22 and scoring > 16 on the 17-item HRSD.23 The inclusion criteria of drug-naïve controls were age 18 to 65 years and having no current or past diagnosis of any major psychiatric disorder according to the SCID-I. Exclusion criteria for both groups were: taking any psychoactive medicines, including for sleep; having bipolar disorder, psychotic disorder, panic disorder, post-traumatic stress disorder, general anxiety disorder, social phobia, eating disorders, alcohol or substance abuse/dependence, or significant or unstable medical illness; and current pregnancy. Subjects who reported having experienced night shift work or transmeridian travel within the previous 6 months were deemed ineligible.
Procedure
Ninety-one patients were diagnosed with MDD by the SCID-I, administered by a psychiatrist with more than 5 years of clinical experience. Sociodemographic information, including age, gender, education, BMI, marital status, and employment, was collected from all participants through a researcher-designed form. Subjects’ biological rhythms were assessed using the BRIAN,17 and depression severity was evaluated with the HRSD.
Materials
The Turkish version of the HRSD has been used to evaluate depressive symptoms in both clinical practice and research studies. This instrument was designed as a 17-item, semi-structured interview23 and measures symptom intensity to assess the severity of depression, changes in its severity over time, and efficacy of treatment.24 Each HRSD item is rated on a three-point or five-point ordinal scale. For the 17-item version, scores can range from 0 to 54. The test-retest reliability coefficient of the HDRS based on a 5-day interval was 0.85, with a Cronbach alpha coefficient of 0.75.25
BRIAN assesses the frequency of problems related to the maintenance of circadian rhythm regularity. It is an 18-item interviewer-administered instrument which investigates the four main domains (sleep, social, activities, and eating) related to circadian rhythm disturbance.17 BRIAN was validated for the Turkish population in regards to internal consistency, with a Cronbach’s alpha coefficient of 0.899 and item-total correlation coefficients between 0.239 and 0.747.26 Each item is scored from 1 (no difficulties in maintaining the habitual rhythm) to 4 (severe difficulties in maintaining the habitual rhythm). Total scores may range from 18 to 72; the higher the score, the greater the biological rhythm disturbance, i.e., the individual experiences more difficulty in maintaining the same circadian pattern. Sleep domain scores range from 5 to 20, social domain scores from 4 to 15, activity domain scores from 4 to 16, and eating-pattern domain scores from 5 to 20.
Statistical analysis
Data were analyzed in SPSS version 22.0 for Mac. Descriptive data were expressed as mean and standard deviation (SD), and other categorical variables were evaluated as a discrete variable. The Shapiro-Wilk test confirmed normality of distribution of sociodemographic and clinical data. Comparisons of sociodemographic variables between groups were performed by chi-square tests for categorical variables and by Student’s t-test for continuous variables. Parametric correlations were calculated with the Pearson correlation coefficient. In consideration of the insomnia cluster, HRSD-Total score was calculated separately without these items as well.27 HRSD-Total scores were regressed on the participants’ demographic characteristics (age, gender, marital status, employment status), BRIAN-Sleep, and BRIAN-Activity scores.
Ethics statement
This study was conducted in accordance with the World Medical Association Declaration of Helsinki and approved by the ethics and scientific committee of Bezmialem Vakıf University, İstanbul, Turkey. Written informed consent was obtained from patients and healthy controls after receiving a full description of the study protocol. Overall, 181 individuals were screened for eligibility.
Results
Ninety patients with depression and 91 matched healthy controls were included in this study. Groups did not differ significantly by age, gender, education, employment, or BMI (Table 1).
Table 1. Descriptive statistics for patients with depression and healthy controls.
| Depression (n=90) | Healthy controls (n=91) | p-value | |
|---|---|---|---|
| Age | 41.5±10.7 | 39.3±7.8 | 0.892* |
| Gender | |||
| Female | 65 (78.1) | 63 (77.3) | 0.724† |
| Male | 25 (21.9) | 28 (22.7) | |
| BMI | 26.8±6.3 | 26.9±4.8 | 0.121* |
| Marital status | |||
| Married | 59 (75.0) | 49 (63.6) | 0.050† |
| Single | 31 (25.0) | 45 (36.4) | |
| Education | |||
| Primary | 47 (41.9) | 42 (58.5) | 0.150† |
| Secondary | 25 (29.0) | 37 (29.3) | |
| Higher | 18 (25.8) | 12 (12.2) | |
| Employment | |||
| Unemployed | 33 (43.8) | 35 (68.2) | 0.878† |
| Employed | 57 (46.9) | 56 (27.3) |
Data presented as number (%) or mean ± standard deviation, unless otherwise specified.
The significance threshold was set at 0.05.
Age and body mass index (BMI) scores were evaluated by Student’s t-test.
Gender, marital status, education, and employment were calculated by chi-square tests for categorical variables.
The patients with depression showed significantly greater biological rhythm disturbances than healthy controls in all domains of BRIAN (sleep, activity, social, and eating patterns). Regarding the chronotype items of BRIAN, the active at night and day/night cycle reversed items were found significant at p < 0.001 in patients with depression. However, the active in the morning item was significant only in the healthy control group, at p < 0.001 (Table 2).
Table 2. Comparison of Biological Rhythms Interview of Assessment in Neuropsychiatry (BRIAN) domains between patients with depression and healthy controls.
| Depression | Healthy controls | F | p-value | |
|---|---|---|---|---|
| BRIAN-Total | 49±10.4 | 33.2±9.5 | 0.8 | < 0.001 |
| BRIAN-Sleep | 15.4±3.8 | 10.4±3 | 7.6 | < 0.001 |
| BRIAN-Activity | 13.1±4.6 | 8.9±3.5 | 9 | < 0.001 |
| BRIAN-Social | 10.2±3.1 | 6.4±2.5 | 4.2 | < 0.001 |
| BRIAN-Eating | 10.7±3.1 | 7.4±2.5 | 6.3 | < 0.001 |
| Active at night | 1.8±0.7 | 2.2±1.1 | 29.1 | < 0.001 |
| Active in the morning | 2.9±0.9 | 2.4±1.1 | 22.89 | < 0.001 |
| Day/night cycle reversed | 1.5±0.7 | 2.4±1.1 | 39.81 | < 0.001 |
p < 0.001 (Student’s t-test). Significance threshold set at 0.05.
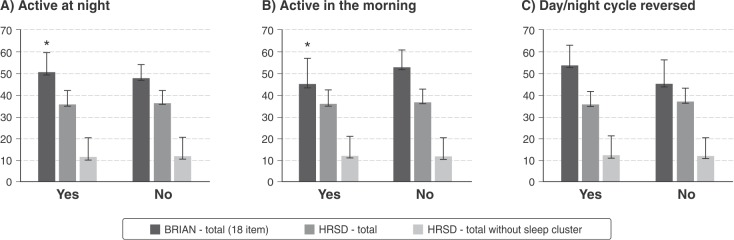
The BRIAN-Total score was significantly higher with evening chronotypes (p = 0.049) and significantly lower with morning chronotypes (p = 0.007) in patients with depression. HRSD-Total score and HRSD-Total without the sleep score did not differ along with the chronotype items of BRIAN in patients with depression (Figure 1).
Figure 1. BRIAN-Total, HRSD-Total, and HRSD-Total (without sleep cluster) scores according to circadian preference in patients with depression. BRIAN = Biological Rhythm Interview Assessment in Neuropsychiatry; HRSD = Hamilton Rating Scale for Depression.* Significance at p < 0.05.
Bivariate correlations between HRSD-Total score, HRSD-Total without sleep cluster, and all BRIAN scales were calculated by Pearson correlation coefficients. HRSD-Total score correlated significantly with BRIAN-Sleep (r = 0.370, p < 0.001), BRIAN-Activity (r = 0.509, p < 0.001), and BRIAN-Total (r = 0.417, p < 0.001); HRSD-Total without sleep cluster correlated significantly with BRIAN-Sleep (r = 0.279, p = 0.008), BRIAN-Activity (r = 0.450, p < 0.001), BRIAN-Social (r = 0.213, p = 0.040), and BRIAN-Total (r = 0.377, p < 0.001). All correlations are presented in Table 3.
Table 3. Pearson correlations between BRIAN domains and HRSD-Total/HRSD-Total without sleep cluster scores in patients with depression.
| HRSD-Total | HRSD-Total without sleep cluster | |
|---|---|---|
| BRIAN-Total | 0.417,* p < 0.001 | 0.377,* p < 0.001 |
| BRIAN-Sleep | 0.370,* p < 0.001 | 0.279,* p = 0.008 |
| BRIAN-Activity | 0.509,* p < 0.001 | 0.450,* p < 0.001 |
| BRIAN-Social | 0.195, p = 0.065 | 0.213,† p = 0.040 |
| BRIAN-Eating | 0.104, p = 0.329 | 0.072, p = 0.501 |
BRIAN = Biological Rhythm Interview Assessment in Neuropsychiatry; HRSD = Hamilton Rating Scale for Depression.
Correlations significant at * 0.01
0.05 (two-tailed).
Additionally, we conducted a linear regression analysis. HRSD-Total scores were regressed on the participants’ BRIAN-Total score and BRIAN-Sleep, BRIAN-Activity, BRIAN-Social, and BRIAN-Eating scores. BRIAN-Total, BRIAN-Social, and BRIAN-Eating were not found to be predictor variables. Increased BRIAN-Activity (B = 0.514, standard error [SE] = 0.101, β = 0.476, t = 5.07, p < 0.001) and BRIAN-Sleep (B = 0.268, SE = 0.130, β = 0.209, t = 2.056, p = 0.043) scores were associated with higher HRSD-Total scores (Table 4).
Table 4. Regression analysis on HRSD-Total score.
| B | SE | β | t | p-value | |
|---|---|---|---|---|---|
| BRIAN-Total | 0.037 | 0.098 | 0.078 | 0.377 | 0.707 |
| BRIAN-Activity | 0.419 | 0.110 | 0.388 | 3.824 | < 0.001 |
| BRIAN-Sleep | 0.268 | 0.130 | 0.209 | 2.056 | 0.043 |
| BRIAN-Social | -0.095 | 0.188 | -0.060 | -0.507 | 0.614 |
| BRIAN-Eating | -0.004 | 0.179 | -0.002 | -0.021 | 0.983 |
Bold type denotes statistical significance.
B = unstandardized beta coefficient; β = standardized beta coefficient; BRIAN = Biological Rhythm Interview Assessment in Neuropsychiatry; HRSD = Hamilton Rating Scale for Depression; SE = standard error.
Discussion
In this sample, patients with major depression showed significantly greater biological rhythm disturbances as measured by total BRIAN scores and in all individual domains of BRIAN than healthy controls.
There are no published data about disruptions of biological rhythm domains in MDD, particularly in drug-naïve patients with healthy controls matched by age, gender, and BMI (variables considered confounders of biological rhythm). Additionally, previous studies have considered disruptions of biological rhythm as a single symptom, or were conducted only in patients with bipolar disorder.14,20,21,28,29 Only one recent study evaluated the effect of specific biological rhythm domains on unipolar depression, finding significant disruption in all biological rhythm domains (sleep, activity, social, and eating) and BRIAN-Total score both in patients with MDD and in those with bipolar disorder, compared to healthy controls.21 However, this study was population-based, only included young adults (age 18-24 years), and did not take into consideration drug use or other confounders. Another advantage of our study is that the diagnosis of MDD was established by a senior psychiatrist according to the SCID-I and the severity of depression was assessed by HRSD, while in the other study diagnosis was confirmed by the Mini International Neuropsychiatric Interview Plus (MINI-PLUS).30
Furthermore, our hypothesis suggests that specific domains may have effects on the human biological rhythm. In line with this hypothesis, increased BRIAN-Activity score was associated with a higher HRSD-Total score, which indicates that decreased daily activity may predict depression. Studies have consistently noted that physical activity is associated with improved physical health, life satisfaction, cognitive functioning, and psychological well-being. One meta-analysis indicated a clinical effect in favor of exercise for reducing depression severity compared to medical treatment,8whereas follow-up data in the study found only a small effect of exercise in the long term. Another meta-analysis suggests that physical activity appears to show efficacy for improving depressive symptoms in adolescents and young adults experiencing a diagnosis or threshold symptoms of depression.31
In line with the current literature, our findings suggested that BRIAN sleep domain scores are significantly higher in patients with depression than in healthy controls. Patients with mood disorders have significant disruptions in sleep disturbances and circadian rhythms.14 The effect of circadian rhythm disturbances and the consequence of altered sleep rhythm on mood disorders are still unknown.32,33 Furthermore, patients with depression showed significantly greater biological rhythm disturbances in the social domain of BRIAN than healthy controls. Impairment of social functioning is considered a distinct sign of depression.34 The social disturbances of patients with MDD are persistent and embody almost every aspect of one’s social capabilities, such as empathy, decision making, and social skills. Moreover, recovery from depression is known to require not only a significant decrease in depressive symptoms, but also an improvement in social domains.35 BRIAN might be useful to understand the sociability status of patients during the first examination, as well as for adequate evaluation of remission.
In our study, potential correlations were assessed with HRSD-Total and HRSD-Total without sleep cluster. HRSD-Total included three items that investigate sleep features (items 4, 5, and 6). A separate evaluation of the HRSD-Total score without the insomnia cluster was calculated to clarify the effect of sleep disturbances on the HRSD scoring system.27,36 Use of the HRSD-Total without the sleep cluster allowed us to understand the relationship between the core symptom cluster of depression (mood, cognition) and biological rhythm disturbances directly. Our study revealed that HRSD-Total and Total without sleep score both correlated significantly with BRIAN-Sleep, Activity, and Total. In line with this finding, HRSD-Total without sleep cluster correlated significantly with BRIAN-Social. These results may explain the depressive mood items and cognition factors of HRSD (items 1, 2, 3, 7, 9, 10, and 13) in a manner more related to social manners than to sleep features in patients with major depression. Social zeitgebers consist of external cues that entrain biological rhythms, such as personal relationships, meals, exercise, or social demands at school/work, while daily environmental signals, such as light/dark, regular feeding, are considered physical zeitgebers.37 A recent study38 suggested a novel approach to investigate the three main effects of light: as zeitgeber, as cognitive enhancer, and as mood regulator.39 Both social and physical zeitgebers have been found to be associated with mood disorders due to their role in regulating emotional responses and mood.40
Regarding the eating pattern of patients with major depression, no association of BRIAN-Eating with either HRSD group was found. It is well known that the HRSD scoring system considers only the anorexia aspect of eating pattern, specifically by inquiring as to personal or clinical observation of the weight loss. We suggest that the lack of questions on weight gain and other eating habits in HRSD leads to underestimation of disordered eating behavior in patients with depression. In contrast to the HRSD, the BRIAN-Eating domain evaluates eating habits more comprehensively by asking about eating rhythm over the course of a day, caffeinated and stimulant drink intake, and skipping meals. Unlike our study, a previous investigation found that BRIAN-Eating domain scores correlated with the severity of depression.21
Comparison of the chronotype items of BRIAN (active at night, active in the morning, and day/night cycle reversed) revealed that patients with depression tend to be active at night and have a reversed day/night cycle when compared to healthy controls. Furthermore, healthy controls were mainly active in the morning, unlike patients with depression, whose BRIAN-Total score was significantly higher with the chronotype item of active at night and significantly lower with the chronotype item of active in the morning. This finding is consistent with previous studies reporting the association between evening chronotypes and biological rhythm disruptions.21,37
Although circadian preferences are related to HRSD-Total and HRSD-Total without sleep cluster in the literature,36 we found no relationship of these scores with the chronotype items of BRIAN. Considering that more comprehensive and detailed instruments exist for evaluation of chronotypes, such as the Morningness-Eveningness Questionnaire (MEQ) and the Munich Chronotype Questionnaire (MCTQ),36 the chronotype items of BRIAN might be less capable of predicting this relationship accurately.
The present study has several limitations. Given the cross-sectional design, the possibility exists that an unmeasured variable caused the differences observed between diagnoses. Longitudinal studies are needed to elucidate this.
Another significant limitation is that we only evaluated biological rhythm disruptions as reported in a subjective, self-administered questionnaire which evaluates patients’ biological rhythm patterns over the preceding 15 days. This may have biased data due to personal differences in assessment and exaggerated perceptions of daily rhythm disruption by depressive patients. Integration of an objective measurement, such as actigraphy, would have helped overcome this.
The third major limitation of this study is that the majority of our population was female, although the gender distribution between the case and control groups was similar. Our sample size was relatively small, but we believe our use of a strictly matched control group (by age, gender, BMI, education, and employment) eliminated the most important known confounders, increasing statistical power and overcoming the possibility of bias.
In conclusion, follow-up of specific biological rhythm patterns has a critical role to play in understanding major depressive disorder and implementing adequate treatment. Findings from recent studies demonstrate that specific biological rhythm domains such as activity and sleep are significantly associated with depression severity. Therefore, we recommend that mental health workers assess biological rhythm domains to evaluate depression severity, monitor the course of illness over time, and when screening for depression. Additionally, we must stress the importance of the physical activity domain of biological rhythm disturbances in addition to the well-known role of the sleep domain in depression. Although extensive further research is still needed to determine causality, it can be inferred from these findings that increasing physical activity is an important and practical step for treating depression.
Disclosure
The authors report no conflicts of interest.
Footnotes
How to cite this article: Ozcelik M, Sahbaz C. Clinical evaluation of biological rhythm domains in patients with major depression. Braz J Psychiatry. 2020;42:258-263. http://dx.doi.org/10.1590/1516-4446-2019-0570
References
- 1.Wilson S, Hicks BM, Foster KT, McGue M, Iacono WG. Age of onset and course of major depressive disorder: associations with psychosocial functioning outcomes in adulthood. Psychol Med. 2015;45:505–14. doi: 10.1017/S0033291714001640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lewinsohn PM, Rohde R, Seeley JR. Major depressive disorder in older adolescents: prevalence, risk factors, and clinical implications. Clin Psychol Rev. 1998;18:765–94. doi: 10.1016/s0272-7358(98)00010-5. [DOI] [PubMed] [Google Scholar]
- 3.Brent DA, Birmaher B. Clinical practice. Adolescent depression. N Engl J Med. 2002;347:667–71. doi: 10.1056/NEJMcp012249. [DOI] [PubMed] [Google Scholar]
- 4.Thapar A, Collishaw S, Pine DS, Thapar AK. Depression in adolescence. Lancet. 2012;379:1056–67. doi: 10.1016/S0140-6736(11)60871-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bromet E, Andrade LH, Hwang I, Sampson NA, Alonso J, de Girolamo G, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 2011;9:90. doi: 10.1186/1741-7015-9-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lopez AD, Murray CC. The global burden of disease, 1990-2020. Nat Med. 1998;4:1241–3. doi: 10.1038/3218. [DOI] [PubMed] [Google Scholar]
- 7.Burton C, McKinstry B, Szentagotai Tătar A, Serrano-Blanco A, Pagliari C, Wolters M. Activity monitoring in patients with depression: a systematic review. J Affect Disord. 2013;145:21–8. doi: 10.1016/j.jad.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 8.Cooney GM, Dwan K, Greig CA, Lawlor DA, Rimer J, Waugh FR, et al. Exercise for depression. Cochrane Database Syst Rev. 2013;(9):CD004366. doi: 10.1002/14651858.CD004366.pub6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kvam S, Kleppe CL, Nordhus IH, Hovland A. Exercise as a treatment for depression: a meta-analysis. J Affect Disord. 2016;202:67–86. doi: 10.1016/j.jad.2016.03.063. [DOI] [PubMed] [Google Scholar]
- 10.Schuch FB, Deslandes AC, Stubbs B, Gosmann NP, Silva CT, Fleck MP. Neurobiological effects of exercise on major depressive disorder: a systematic review. Neurosci Biobehav Rev. 2016;61:1–11. doi: 10.1016/j.neubiorev.2015.11.012. [DOI] [PubMed] [Google Scholar]
- 11.Hallgren M, Nguyen TT, Herring MP, McDowell CP, Gordon BR, Stubbs B, et al. Associations of physical activity with anxiety symptoms and disorders: findings from the Swedish National March Cohort. Gen Hosp Psychiatry. 2019;58:45–50. doi: 10.1016/j.genhosppsych.2019.03.001. [DOI] [PubMed] [Google Scholar]
- 12.Behrman S, Ebmeier KP. Can exercise prevent cognitive decline? Practitioner. 2014;258(:17-21):2–3. [PubMed] [Google Scholar]
- 13.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR). Arlington: American Psychiatric Publishing; 2000. [Google Scholar]
- 14.McClung CA. How might circadian rhythms control mood? Let me count the ways. Biol Psychiatry. 2013;74:242–9. doi: 10.1016/j.biopsych.2013.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mondin TC, Cardoso Tde A, Jansen K, Silva Gdel G, Souza LD, Silva RA. Long-term effects of cognitive therapy on biological rhythms and depressive symptoms: a randomized clinical trial. J Affect Disord. 2015;187:1–9. doi: 10.1016/j.jad.2015.08.014. [DOI] [PubMed] [Google Scholar]
- 16.Harvey AG, Murray G, Chandler RA, Soehner A. Sleep disturbance as transdiagnostic: consideration of neurobiological mechanisms. Clin Psychol Rev. 2011;31:225–35. doi: 10.1016/j.cpr.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giglio LM, Magalhães PV, Andreazza AC, Walz JC, Jakobson L, Rucci P, et al. Development and use of a biological rhythm interview. J Affect Disord. 2009;118:161–5. doi: 10.1016/j.jad.2009.01.018. [DOI] [PubMed] [Google Scholar]
- 18.Pinho M, Sehmbi M, Cudney LE, Kauer-Sant'anna M, Magalhães PV, Reinares M, et al. The association between biological rhythms, depression, and functioning in bipolar disorder: a large multi-center study. Acta Psychiatr Scand. 2016;133:102–8. doi: 10.1111/acps.12442. [DOI] [PubMed] [Google Scholar]
- 19.Giglio LM, Magalhães PV, Kapczinski NS, Walz JC, Kapczinski F. Functional impact of biological rhythm disturbance in bipolar disorder. J Psychiatr Res. 2010;44:220–3. doi: 10.1016/j.jpsychires.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 20.Cudney LE, Frey BN, Streiner DL, Minuzzi L, Sassi RB. Biological rhythms are independently associated with quality of life in bipolar disorder. Int J Bipolar Disord. 2016;4:9. doi: 10.1186/s40345-016-0050-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mondin TC, Cardoso TA, Souza LD, Jansen K, da Silva Magalhães PV, Kapczinski F, et al. Mood disorders and biological rhythms in young adults: a large population-based study. J Psychiatr Res. 2017;84:98–104. doi: 10.1016/j.jpsychires.2016.09.030. [DOI] [PubMed] [Google Scholar]
- 22.First MB, Williams Janet BW, Spitzer RL, Gibbon M. Structured Clinical Interview for DSM-IV Axis I Disorders-Research Version, Patient Edition (SCID-I/P). Arlington: American Psychiatric Publishing; 1997. [Google Scholar]
- 23.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Santen G, Gomeni R, Danhof M, Della Pasqua O. Sensitivity of the individual items of the Hamilton depression rating scale to response and its consequences for the assessment of efficacy. J Psychiatr Res. 2008;42:1000–9. doi: 10.1016/j.jpsychires.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 25.Akdemir A, Türkçapar MH, Orsel SD, Demirergi N, Dag I, Ozbay MH. Reliability and validity of the Turkish version of the Hamilton Depression Rating Scale. Compr Psychiatry. 2001;42:161–5. doi: 10.1053/comp.2001.19756. [DOI] [PubMed] [Google Scholar]
- 26.Aydemir Ö, Akkaya C, Altınbaş K, Kora K, Dikici DS, Akdeniz F, et al. Reliability and validity of Turkish version of biological rhythms interview of assessment in neuropsychiatry. Anadolu Psikiyatri Derg. 2012;13:256–61. [Google Scholar]
- 27.Gaspar-Barba E, Calati R, Cruz-Fuentes CS, Ontiveros-Uribe MP, Natale V, De Ronchi D, et al. Depressive symptomatology is influenced by chronotypes. J Affect Disord. 2009;119:100–6. doi: 10.1016/j.jad.2009.02.021. [DOI] [PubMed] [Google Scholar]
- 28.Allega OR, Leng X, Vaccarino A, Skelly M, Lanzini M, Hidalgo MP, et al. Performance of the biological rhythms interview for assessment in neuropsychiatry: an item response theory and actigraphy analysis. J Affect Disord. 2018;225:54–63. doi: 10.1016/j.jad.2017.07.047. [DOI] [PubMed] [Google Scholar]
- 29.Dopierala E, Chrobak A, Kapczinski F, Michalak M, Tereszko A, Ferensztajn-Rochowiak E, et al. A study of biological rhythm disturbances in Polish remitted bipolar patients using the BRIAN, CSM, and SWPAQ Scales. Neuropsychobiology. 2016;74:125–30. doi: 10.1159/000458527. [DOI] [PubMed] [Google Scholar]
- 30.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. quiz 34-57. [PubMed] [Google Scholar]
- 31.Bailey AP, Hetrick SE, Rosenbaum S, Purcell R, Parker AG. Treating depression with physical activity in adolescents and young adults: a systematic review and meta-analysis of randomised controlled trials. Psychol Med. 2018;48:1068–83. doi: 10.1017/S0033291717002653. [DOI] [PubMed] [Google Scholar]
- 32.Wirz-Justice A. Chronobiology and mood disorders. Dialogues Clin Neurosci. 2003;5:315–25. doi: 10.31887/DCNS.2003.5.4/awirzjustice. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wirz-Justice A. Biological rhythm disturbances in mood disorders. Int Clin Psychopharmacol. 2006;21(Suppl 1):S11–5. doi: 10.1097/01.yic.0000195660.37267.cf. [DOI] [PubMed] [Google Scholar]
- 34.Hirschfeld RM, Montgomery SA, Keller MB, Kasper S, Schatzberg AF, Möller HJ, et al. Social functioning in depression: a review. J Clin Psychiatry. 2000;61:268–75. doi: 10.4088/jcp.v61n0405. [DOI] [PubMed] [Google Scholar]
- 35.Kupferberg A, Bicks L, Hasler G. Social functioning in major depressive disorder. Neurosci Biobehav Rev. 2016;69:313–32. doi: 10.1016/j.neubiorev.2016.07.002. [DOI] [PubMed] [Google Scholar]
- 36.Sahbaz C, Devetzioglou T, Ozcelik A, Kirpinar I. Circadian preferences are associated with vegetative symptoms and comorbid medical diseases in patients with major depression. Biol Rhythm Res. 2019;59:703–17. [Google Scholar]
- 37.Roenneberg T, Merrow M. The circadian clock and human health. Curr Biol. 2016;26:R432–43. doi: 10.1016/j.cub.2016.04.011. [DOI] [PubMed] [Google Scholar]
- 38.Fernandez DC, Fogerson PM, Lazzerini Ospri L, Thomsen MB, Layne RM, Severin D, et al. Light affects mood and learning through distinct retina-brain pathways. Cell. 2018;175:71–84.e18. doi: 10.1016/j.cell.2018.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wirz-Justice A, Benedetti F. Perspectives in affective disorders: clocks and sleep. Eur J Neurosci. 2020;51:346–65. doi: 10.1111/ejn.14362. [DOI] [PubMed] [Google Scholar]
- 40.Clarke G, Harvey AG. The complex role of sleep in adolescent depression. Child Adolesc Psychiatr Clin N Am. 2012;21:385–400. doi: 10.1016/j.chc.2012.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]