Abstract
Background.
Adolescent drug use has long term health consequences, like substance use disorders and psychiatric illnesses. Proximal health risks, especially for overdose, are amplified when multiple substances are combined. Existing literature on polysubstance use among adolescents has largely focused on alcohol, tobacco, and marijuana, but has largely excluded other drugs like opioids. Understanding how adolescents combine illicit drugs is essential for intervening to prevent poor health outcomes.
Methods.
We aimed to explore patterns of lifetime polysubstance use among adolescents in Baltimore City. We used data on 9th-12th graders recruited to participate in the 2017 local Baltimore Youth Risk Behavior Survey who reported any lifetime drug use (n=387; 60% female, 77% non-Hispanic Black). We then conducted a latent class analysis using 10 indicators of lifetime drug and alcohol use. After selecting the class model, we tested for associations between the class profiles and race, sex, school grade, and lifetime injection drug use.
Results.
We identified three profiles of lifetime polysubstance use in our sample: alcohol and marijuana (68.6% of sample), polysubstance (22.0%), and alcohol/pain medication/inhalant use (9.4%). Members of the polysubstance use class were more likely to be male and to report injection drug use.
Conclusions.
Understanding broader patterns of drug use beyond alcohol, tobacco and marijuana amongst adolescents is a crucial step towards preventing adverse drug and health-related outcomes later in life. More research is needed to characterize the full health impact of youth polysubstance use patterns and related risk behaviors like injection drug use.
Keywords: Polysubstance use, adolescents, latent class analysis, youth risk behavior survey, drug use patterns
1. Introduction
Adolescent drug use is pervasive in the United States (US). In 2017, 35.6% of high school students reported lifetime marijuana use, 14.0% had misused prescription pain medications, 6.9% has used synthetic marijuana, 6.6% had used hallucinogens, and 6.2% had used inhalants (Kann et al., 2018). Other drugs, like ecstasy (4.0%), cocaine (4.8%), steroids (2.9%), methamphetamine (2.5%), and heroin (1.7%), are rarer among US youth, but represent serious health concerns for youth who consume them (Kann et al., 2018). Adolescent drug use is associated with many negative outcomes, including arrests, school dropout, and substance use and psychiatric disorders (Brook et al., 2000; Gil et al., 2004; Newcomb and Bentler, 1988; Vida et al., 2009; White et al., 1998).
Adolescent substance use in the US varies geographically, with recent studies documenting geographic differences in the prevalence of heroin and non-medical prescription opioid use (NMPO) use (Jones et al., 2019), and geographic differences in trends in adolescent heroin and injection drug use over time (Brighthaupt et al., 2019). The prevalence of other substance use (e.g., cocaine, alcohol) also varies regionally in the US (Johnston et al., 2019; Thorlton et al., 2012). Understanding patterns of adolescent substance use in places with particularly high substance use burdens is necessary to inform tailored public health programming.
Baltimore City is among the cities with high rates of adolescent drug use, warranting further investigations into youth drug use patterns in this urban context (Jones et al., 2019). As in many urban settings, adolescents in Baltimore face high levels of poverty (31% of families living below the poverty line) and significant social problems that are known contributors to adolescent drug use, like pervasive community violence and an under-funded public school system (Baltimore Neighborhood Indicators Alliance, 2019; Dashiff et al., 2009; National Center for Education Statistics, 2017; Wright et al., 2013). Because these contextual factors are shared, in varying degrees, by many other cities, identifying the nuances of adolescent substance use in Baltimore City can also form the basis for understanding youth drug use in other urban centers.
Understanding how adolescents use and combine drugs and the potential risks these behaviors confer within high drug use contexts is important for developing tailored interventions. Research among adults has demonstrated that polysubstance use increases one’s risk for fatal and non-fatal overdoses, HIV, and Hepatitis C (Coffin et al., 2003; Darke et al., 2005; Degenhardt and Hall, 2012; Harrell et al., 2012; Roth et al., 2015; Sorg et al., 2016; Wu et al., 2011). The literature documenting specific patterns of polysubstance use among adolescents has important limitations. Studies have typically focused on alcohol, tobacco, and marijuana, and included few other substances (typically stimulants and/or inhalants) or combined all other drugs into single illicit drug use variables (Delk et al., 2019; Kulis et al., 2016; Morean et al., 2016; Su et al., 2018; Tomczyk et al., 2016). A systematic review of latent class analyses of adolescent polysubstance use identified that the classes typically found in existing studies are no/low use, polysubstance use, and single substance classes (i.e. alcohol only, marijuana only) (Tomczyk et al., 2016). Of studies that include a broader range of drugs, most typically find similar classes, and a few identify NMPO-related classes in addition to overall polysubstance classes (Choi et al., 2018; Kulis et al., 2016; Tomczyk et al., 2016; Wu et al., 2020). This is due, in part, to the inclusion of adolescents who do not use drugs in study samples, which decreases latent class models’ ability to detect nuance within polysubstance use if there is a large portion of the study sample that does not endorse model indicators. Expanding the type of substances included in latent analyses and focusing specifically on adolescents who do endorse drug use will enable characterization of more specific profiles that may be associated with poor health outcomes and can be targeted by future interventions.
Presently, we aim to characterize profiles of lifetime polysubstance use among adolescents in Baltimore City, Maryland who report lifetime use of a wide range of substances, including several drugs unexplored to date (e.g., opioids), to increase understanding of the intersection between opioid and other drug use among these youth.
2. Methods
2.1. Data Source.
Data for this study come from the Youth Risk Behavior Survey (YRBS) datasets for Baltimore City from 2017 (N=805). The YRBS is conducted biennially in public high schools. Students complete an anonymous self-administered survey. The overall response rate for Baltimore City was 69%. We restricted the sample to individuals who reported using ≥ 1 non-alcohol drug (listed below) in their lifetime (n=389). We further excluded 2 ungraded students in the sample, yielding a final analytic sample of 387. We did not apply survey weights to the analysis, because weighted estimates would likely be non-representative within this restricted sample.
2.2. Measures.
Participants reported any lifetime use of alcohol or any of the following 9 drugs : marijuana, synthetic marijuana, cocaine, methamphetamine, heroin, pain medications (not as prescribed by a doctor), inhalants, ecstasy, and steroids. We included sex (male, female), race/ethnicity (Non-Hispanic Black, Other), grade (9th-12th), and any lifetime injection drug use (IDU) as covariates. More than 10% had missing data on marijuana use (13.7%), alcohol use (20.7%), and IDU (11.6%).
2.3. Analysis.
We conducted a latent class analysis (LCA) of the 10 substance use measures to identify subgroups with similar polysubstance use profiles (Goodman, 1974; Lazarsfeld and Henry, 1968). Here, LCA allows for the identification of homogenous subgroups with respect to the substance use indicators to identify distinct profiles of drugs use that may confer unique health risks. We used model fit statistics to determine the preferred number of classes: Akaike Information Criteria, Bayesian Information Criteria, and Lo-Mendell-Rubin Likelihood Ratio Tests (Nylund et al., 2007). We used a Full Information Maximum Likelihood estimator, which addresses missingness as effectively as multiple imputation (Collins et al., 2001). We then used a manual three-step approach to test for associations between class membership and our covariates of interest, where logits for the classifications probabilities were used to account for individuals’ likelihood of membership in classes other than their most likely class (Vermunt, 2010). Analyses were conducted using Mplus 8.3 (Muthén and Muthén, 1998–2017).
3. Results
With the exception of 9th graders, our sample was fairly evenly distributed across grades (9th: 17.8%, 10th: 28.3%, 11th: 23.3%, 12th: 30.6%). There were more female (59.6%) than male (40.4%) students in our sample. Most students were Black (77.5%). Marijuana was the most commonly used drug (89.2%), followed by alcohol (80.1%), prescription pain medications (26.0%), synthetic marijuana (21.5%), and inhalants (22.8%). Heroin (15.0%), steroids (15.5%), methamphetamine (14.0%), ecstasy (13.3%), cocaine (13.9%), were the least prevalent drugs used. In our sample, 13.2% reported lifetime injection.
We selected a three class LCA model for polysubstance use based on the fit statistics in Table 1. The three-class model was preferred according to the BIC and Lo-Mendell-Rubin Likelihood Ratio Test, had good entropy, and was the largest model that retained a sufficiently sized smallest class. The conditional probabilities of endorsing each drug use indicator by class are displayed in Figure 1. The largest class represented 68.6% of the sample and was characterized by alcohol and marijuana use. The second largest class contained 22.0% of the sample and was characterized by high probabilities of using all drugs and alcohol (hereafter referred to as polysubstance use). The smallest class represented 9.4% of the sample and was primarily characterized by alcohol, inhalant, and pain medication use, with some marijuana use.
Table 1.
Latent Class Analysis Fit Statistics
| Classes | Smallest Class | Log Likelihood | AIC | BIC | Entropy | LMR p-value |
|---|---|---|---|---|---|---|
| 1 | -- | −1603.843 | 3227.687 | 3267.271 | -- | -- |
| 2 | 21.9% | −1198.862 | 2439.724 | 2522.851 | 0.957 | 0.000 |
| 3 | 9.4% | −1161.761 | 2387.521 | 2514.191 | 0.936 | 0.012 |
| 4 | 6.3% | −1140.884 | 2367.767 | 2537.979 | 0.879 | 0.191 |
| 5 | 4.7% | −1122.532 | 2353.064 | 2566.819 | 0.949 | 0.001 |
| 6 | 4.7% | −1109.256 | 2348.513 | 2605.81 | 0.813 | 0.000 |
Figure 1.
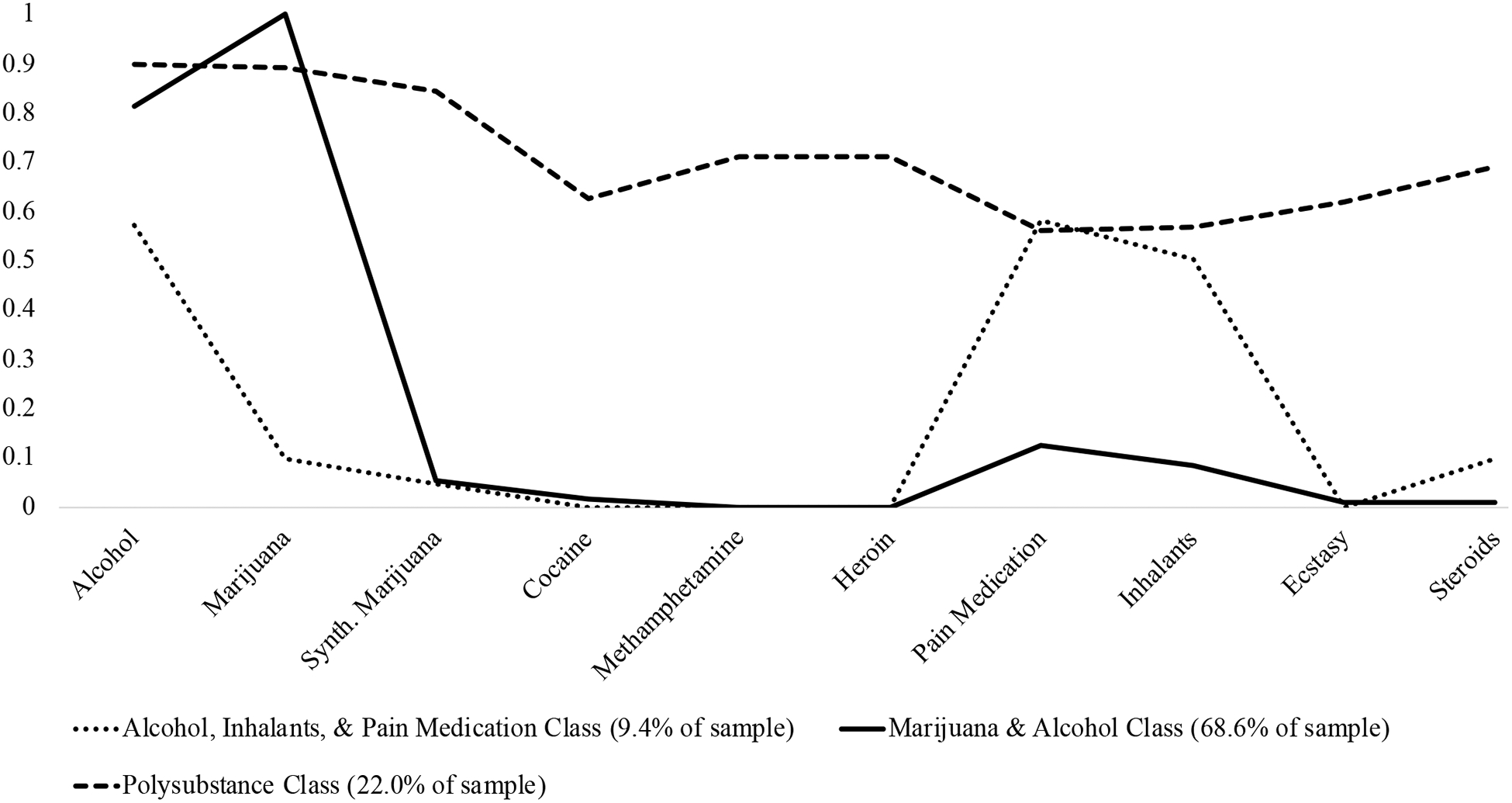
Probabilities of Use of Each Drug by Latent Class.
Race/ethnicity was not a statistically significant correlate of class membership. More than three-quarters of those in each group were Black (alcohol/marijuana: 76.9%; polysubstance: 75.3%; alcohol/inhalants/pain medication: 90.5%). The classes had the following estimated proportions in each grade level: alcohol/marijuana – 16.2% in 9th, 27.0% in 10th, 24.5% in 11th, and 32.3% in 12th; polysubstance – 14.5% in 9th, 31.9% in 10th, 21.7% in 11th, and 31.9% in 12th; alcohol/pain medication/inhalants – 29.2% in 9th, 32.3% in 10th, 22.5% in 11th, and 16.0% in 12th. The only statistically significant differences between classes in terms of grade was that twelfth graders were more likely than ninth graders to be in the alcohol/marijuana class (ß=1.36, p=0.031) and the polysubstance class (ß=1.45, p=0.039) than the alcohol/pain medication/inhalants class. The polysubstance use class had a lower probability of members being female (38.9%) than the alcohol/marijuana (65.2%; ß=−1.09, p<0.001) and alcohol/pain medication/inhalants (64.5%; ß=−1.03, p=0.024) classes. The low prevalence of injection drug use in the sample precluded from testing for differences by latent class, as tests produced standard errors too large to be reasonably considered reliable. Instead, we calculated the prevalence of lifetime IDU for each class, accounting for misclassification: 0.0% in the alcohol/pain medication/inhalants class, 2.0% in the alcohol/marijuana class, and 66.0% in the polysubstance class.
4. Discussion
In this study, we used latent class analysis to characterize patterns of polysubstance use among Baltimore City high school students who reported lifetime drug use. We identified three primary patterns of substance use: marijuana and alcohol use, polysubstance use, and alcohol, pain medication, and inhalant use. The polysubstance use class was more likely to be male, and report lifetime cigarette use, and injecting drugs.
There are two distinct groups of youth who are using opioids in Baltimore, who may be at very different risks for overdose and infectious disease outcomes. The polysubstance class had a high estimated prevalence of injection drug use, putting them at higher risk for injection-related HIV and Hepatitis C infection. Youth in the polysubstance class may also be at increased risk for severe drug use patterns and substance use disorders. The alcohol/pain medication/inhalants class may be at heightened risk for overdoses, if these lifetime measures reflect concurrent use. Alcohol is a central nervous system depressant, as are most inhalants with the exception of nitrates(Evans and Balster, 1991; Williams et al., 2007). When depressants are combined with opioids, the risk of experiencing a fatal overdose increases substantially (Warner‐ Smith et al., 2001; White and Irvine, 1999). More research is needed to directly test the health consequences associated with the adolescent substance use profiles we have identified and their similarities and differences from adult outcomes.
This study indicates that polysubstance use is common among adolescents who use drugs in Baltimore City. Understanding the ways in which adolescents combine multiple substances is essential for both research and public health practice in this population. In this study, we began to highlight different patterns of polysubstance use that exist among adolescents in Baltimore, which points to groups with divergent health risks. These results suggest that distinct harm reduction programs related to preventing these outcomes would be most appropriate for different groups of adolescents, based on their polysubstance use profiles.
This study has some limitations to consider. Most importantly, the Baltimore YRBS only measures lifetime illicit drug use, except for marijuana. We were unable to determine if the use of multiple drugs occurred simultaneously, and future studies are needed to clarify this. However, studies of simultaneous polysubstance use are relatively rare even among adults. Frequency and recency of use are important characteristics of polysubstance use that we were not able to address in this study. Future studies are needed to explore these characteristics of substance use among adolescents within the context of polysubstance use to fully understand the risks of overdose and other adverse health outcomes. Regardless, endorsing lifetime use of a variety of substances still represents some level of risk for adverse health outcomes among adolescents. The YRBS data only reflects high school attending adolescents, thus adolescents who are not attending school and may be at high risk for substance use and related harms are not included in this study. Furthermore, we could not evaluate the health impact of adolescent drug use profiles in this study because YRBS does not measure key substance use-related health outcomes, like overdose, HIV, and Hepatitis C infection. Finally, the results of this study may only generalize to other demographically similar adolescent populations living in urban environments. Socio-environmental risk factors, like poverty and violence, are common in Baltimore City, and these factors should be considered when comparing the present findings to those in other settings. Nonetheless, this study expands our understanding of polysubstance use among youth in notably high-risk urban contexts, by including a range of drugs and focusing on adolescents who endorse drug use.
4.1. Conclusions.
Adolescents who use drugs in Baltimore City have a variety of substance use profiles, each of which may have distinct health impacts. Specific patterns of substance use may heighten risks for overdose, and infections related to injection drug use. More research is needed to fully characterize the health consequences of polysubstance use profiles in adolescence, and their relationships to overdose and infectious disease outcomes.
Highlights.
Polysubstance use was common among adolescents who used drugs in Baltimore City.
Three profiles emerged: alcohol/marijuana, polysubstance, and alcohol/inhalants/pain medication.
The polysubstance use class was more commonly male and 66% had injected drugs.
Funding:
KES and SCB were supported by a NIDA training grant (5T32DA007292). This project was also supported by the Bloomberg American Health Initiative at the Johns Hopkins Bloomberg School of Public Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: None.
References:
- Baltimore Neighborhood Indicators Alliance, 2019. Vital Signs 17. Jacob France Institute, Baltimore, Maryland. [Google Scholar]
- Brighthaupt S-C, Schneider KE, Johnson JK, Jones AA, Johnson RM, 2019. Trends in Adolescent Heroin and Injection Drug Use in Nine Urban Centers in the US, 1999–2017. J. Adolesc. Health 65(2), 210–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook JS, Richter L, Rubenstone E, 2000. Consequences of adolescent drug use on psychiatric disorders in early adulthood. Ann. Med 32(6), 401–407. [DOI] [PubMed] [Google Scholar]
- Choi HJ, Lu Y, Schulte M, Temple JR, 2018. Adolescent substance use: Latent class and transition analysis. Addict. Behav 77, 160–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffin PO, Galea S, Ahern J, Leon AC, Vlahov D, Tardiff K, 2003. Opiates, cocaine and alcohol combinations in accidental drug overdose deaths in New York City, 1990–98. Addiction 98(6), 739–747. [DOI] [PubMed] [Google Scholar]
- Collins LM, Schafer JL, Kam C-M, 2001. A comparison of inclusive and restrictive strategies in modern missing data procedures. Psychol. Methods 6(4), 330. [PubMed] [Google Scholar]
- Darke S, Williamson A, Ross J, Teesson M, 2005. Non-fatal heroin overdose, treatment exposure and client characteristics: findings from the Australian treatment outcome study (ATOS). Drug Alcohol Rev. 24(5), 425–432. [DOI] [PubMed] [Google Scholar]
- Dashiff C, DiMicco W, Myers B, Sheppard K, 2009. Poverty and adolescent mental health. J. Child Adolesc. Psychiatr. Nurs 22(1), 23–32. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Hall W, 2012. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. Lancet 379(9810), 55–70. [DOI] [PubMed] [Google Scholar]
- Delk J, Carey FR, Case KR, Creamer MR, Wilkinson AV, Perry CL, Harrell MB, 2019. Adolescent tobacco uptake and other substance use: A latent class analysis. Am. J. Health Behav 43(1), 3–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans EB, Balster RL, 1991. CNS depressant effects of volatile organic solvents. Neurosci. Biobehav. Rev 15(2), 233–241. [DOI] [PubMed] [Google Scholar]
- Gil AG, Wagner EF, Tubman JG, 2004. Associations between early-adolescent substance use and subsequent young-adult substance use disorders and psychiatric disorders among a multiethnic male sample in South Florida. Am. J. Public Health 94(9), 1603–1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman LA, 1974. Exploratory latent structure analysis using both identifiable and unidentifiable models. Biometrika 61(2), 215–231. [Google Scholar]
- Harrell PT, Mancha BE, Petras H, Trenz RC, Latimer WW, 2012. Latent classes of heroin and cocaine users predict unique HIV/HCV risk factors. Drug Alcohol Depend. 122(3), 220–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE, Patrick ME, 2019. Monitoring the Future National Survey Results on Drug Use, 1975–2018: Overview, Key Findings on Adolescent Drug Use. Institute for Social Research. [Google Scholar]
- Jones AA, Schneider KE, Brighthaupt S-C, Johnson JK, Linton SL, Johnson RM, 2019. Heroin and nonmedical prescription opioid use among high school students in urban school districts. Drug Alcohol Depend. 107664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Queen B, Lowry R, Chyen D, Whittle L, Thornton J, Lim C, Bradford D, Yamakawa Y, Leon M, Brener N, Ethier KA, 2018. Youth Risk Behavior Surveillance — United States, 2017. MMWR Morb. Mortal. Wkly. Rep 67 (SS-8), 1–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulis SS, Jager J, Ayers SL, Lateef H, Kiehne E, 2016. Substance use profiles of urban American Indian adolescents: a latent class analysis. Subst. Use Misuse 51(9), 1159–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarsfeld P, Henry N, 1968. Latent structure analysis. Houghton Mifflin Company, Boston, Massachusetts. [Google Scholar]
- Morean ME, Kong G, Camenga DR, Cavallo DA, Simon P, Krishnan-Sarin S, 2016. Latent class analysis of current e-cigarette and other substance use in high school students. Drug Alcohol Depend. 161, 292–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO, 1998–2017. Mplus User’s Guide. Muthén & Muthén, Los Angeles, CA. [Google Scholar]
- National Center for Education Statistics, 2017. Baltimore City Public School, MD District Demographic Dashboard 2013–2017. https://nces.ed.gov/Programs/Edge/ACSDashboard/2400090. (Accessed April 12 2020).
- Newcomb MD, Bentler PM, 1988. Consequences of adolescent drug use: Impact on the lives of young adults. Sage Publications, Inc. [Google Scholar]
- Nylund KL, Asparouhov T, Muthén BO, 2007. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling 14(4), 535–569. [Google Scholar]
- Office of Epidemiology and Planning, 2008. Intoxication Deaths Associated with Drugs of Abuse Or Alcohol Baltimore, Maryland: January 1995 through September 2007 Baltimore City Health Department.
- Roth AM, Armenta RA, Wagner KD, Roesch SC, Bluthenthal RN, Cuevas-Mota J, Garfein RS, 2015. Patterns of drug use, risky behavior, and health status among persons who inject drugs living in San Diego, California: a latent class analysis. Subst. Use Misuse 50(2), 205–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz RP, Gryczynski J, O’Grady KE, Sharfstein JM, Warren G, Olsen Y, Mitchell SG, Jaffe JH, 2013. Opioid agonist treatments and heroin overdose deaths in Baltimore, Maryland, 1995–2009. Am. J. Public Health 103(5), 917–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorg MH, Long DL, Abate MA, Kaplan JA, Kraner JC, Greenwald MS, Andrew TA, Shapiro SL, Wren JA, 2016. Additive effects of cointoxicants in single-opioid induced deaths. Acad. Forensic Pathology 6(3), 532–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su J, Supple AJ, Kuo SI-C, 2018. The role of individual and contextual factors in differentiating substance use profiles among adolescents. Subst. Use Misuse 53(5), 734–743. [DOI] [PubMed] [Google Scholar]
- Thorlton JR, McElmurry B, Park C, Hughes T, 2012. Adolescent performance enhancing substance use: regional differences across the US. J. Addict. Nurs 23(2), 97–111. [DOI] [PubMed] [Google Scholar]
- Tomczyk S, Isensee B, Hanewinkel R, 2016. Latent classes of polysubstance use among adolescents—a systematic review. Drug Alcohol Depend. 160, 12–29. [DOI] [PubMed] [Google Scholar]
- Vermunt JK, 2010. Latent class modeling with covariates: Two improved three-step approaches. Political Analysis 18(4), 450–469. [Google Scholar]
- Vida R, Brownlie E, Beitchman JH, Adlaf EM, Atkinson L, Escobar M, Johnson CJ, Jiang H, Koyama E, Bender D, 2009. Emerging adult outcomes of adolescent psychiatric and substance use disorders. Addict. Behav 34(10), 800–805. [DOI] [PubMed] [Google Scholar]
- Warner‐Smith M, Darke S, Lynskey M, Hall W, 2001. Heroin overdose: causes and consequences. Addiction 96(8), 1113–1125. [DOI] [PubMed] [Google Scholar]
- White HR, Bates ME, Labouvie E, 1998. Adult outcomes of adolescent drug use: A comparison of process-oriented and incremental analyses, in: Jessor R (Ed.) New perspectives on adolescent risk behavior. Cambridge University Press, pp. 150–181. [Google Scholar]
- White JM, Irvine RJ, 1999. Mechanisms of fatal opioid overdose. Addiction 94(7), 961–972. [PubMed] [Google Scholar]
- Williams JF, Storck M, Committee on Substance Abuse, Committee on Native American Child Health, 2007. Inhalant abuse. Pediatrics 119(5), 1009–1017. [DOI] [PubMed] [Google Scholar]
- Wright EM, Fagan AA, Pinchevsky GM, 2013. The effects of exposure to violence and victimization across life domains on adolescent substance use. Child Abuse Negl. 37(11), 899–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L-T, Ling W, Burchett B, Blazer DG, Yang C, Pan J-J, Reeve BB, Woody GE, 2011. Use of item response theory and latent class analysis to link poly-substance use disorders with addiction severity, HIV risk, and quality of life among opioid-dependent patients in the Clinical Trials Network. Drug Alcohol Depend. 118(2–3), 186–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu S, Yan S, Marsiglia FF, Perron B, 2020. Patterns and social determinants of substance use among Arizona Youth: A latent class analysis approach. Child. Youth Serv. Rev 110, 104769. [Google Scholar]


