To the editor:
We read with interest the thoughtful piece by Brener and colleagues which points out several key considerations when calculating pulmonary effective arterial elastance (Ea), a lumped parameter of right ventricular (RV) afterload.1 These issues are critical as we consider how best to assess RV-pulmonary arterial (PA) coupling in health and disease. The authors note that the normal RV pressure-volume loop shape peaks early in ejection with declining pressures to end-systole quite unlike its counterpart across the septum. Thus, end-ejection volume is lower than the volume at RV end-systole, and end-systolic pressure (Pes) is better estimated by mean pulmonary artery pressure (mPAP) rather peak systolic pressure (sPAP). Lastly, they note that as left atrial pressure is often much closer to mPAP, it should not be ignored when calculating Ea.
We agree that for normal pulmonary vascular loads these caveats likely apply. Upon development of even mild pulmonary hypertension (PH), however, PV-loop shape for the RV changes with pressure rising throughout ejection and peaking at or near end-systole, much as for the LV (Figure). With this change in morphology, end-ejection and end-systole occur at near identical volumes, and Pes is better approximated by sPAP than mPAP as we and others have shown 2, 3. We further note that the product of mean resistance x compliance for the pulmonary vascular circuit (RC, or time constant of diastolic pressure relaxation), is fairly constant 4 in the absence of elevated left atrial pressure, making mPAP and sPAP highly linearly correlated. This is less so for the systemic arterial system. Therefore, we believe that sPAP is superior to mPAP as an estimate of Pes in the setting of PH.
Figure.
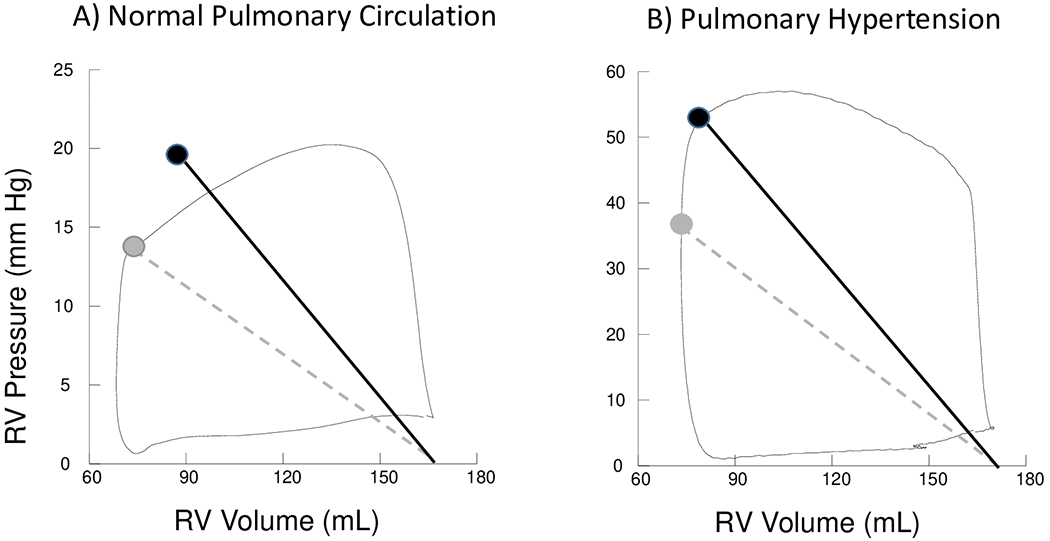
Human Right Ventricular Pressure Volume Loops. A) Normal Pulmonary Circulation - RV pressure declines throughout ejection. RV systolic pressure overestimates end-systolic pressure and end-ejection volume may be lower than end-systolic volume. Effective arterial elastance (Ea) estimated using systolic pulmonary artery pressure (solid black line) likely overestimates RV afterload. Grey dashed line represents Ea estimated using mean pulmonary artery pressure and end-ejection volume. B) Pulmonary Hypertension - RV pressure rises throughout ejection and peaks at end-systole. End-ejection and end-systolic volume are similar. Ea (solid black line) is a better representation of total RV load than Ea (dashed grey line).
Secondly, though left atrial pressure (estimated by pulmonary artery wedge pressure, PAWP) is generally higher relative to mPAP than right atrial pressure is to mean systemic artery pressure, as the authors noted, once again their disparity increases with pulmonary arterial hypertension. Here, PAWP remains low and contributes very little to pulmonary pressure, so ignoring PAWP in the Ea calculation can be justified. However, group 2 pulmonary hypertension has an elevated PAWP and subtracting its value from Pes as proposed may be appropriate. Support for subtracting PAWP is provided by Morimont et al who found Pes/stroke volume overestimated Ea (as determined by a 3-element Windkessel model) by approximately the value of PAWP, albeit not a model of group 2 PH.5 That said, both animal and human studies have shown that elevations of left atrial pressure increase the pulsatile RV afterload independent of mean pulmonary vascular resistance4, 6. This is observed in the RV PV loop as a rise in systolic pressure at end-systole. This is accounted for if sPAP rather than mPAP is used to approximate Pes, which again supports the use of sPAP in calculation of pulmonary vascular Ea.
In summary, we agree that when analyzing afterload and RV-pulmonary arterial coupling in a normal pulmonary circulation the proposed equation by Brener may be more appropriate. However, in the setting of pulmonary hypertension, this will likely underestimate afterload and may lead to spuriously high RV-PA coupling ratios. The issue of subtracting PAWP in group 2 PH requires further study.
Footnotes
Disclosures
Dr. Tedford is serves as a hemodynamic core lab for Actelion and Merck, a consultant for United Therapeutics and Arena Pharmaceutics, on a research advisory committee for Abiomed, and a steering committee for Medtronic. Dr. Hsu and Dr. Kass report no disclosures.
References
- 1.Brener MI, Burkhoff D and Sunagawa K. Effective Arterial Elastance in the Pulmonary Arterial Circulation. Circulation: Heart Failure. 2020;13:e006591. [DOI] [PubMed] [Google Scholar]
- 2.Tello K, Richter MJ, Axmann J, Buhmann M, Seeger W, Naeije R, Ghofrani HA and Gall H. More on Single-Beat Estimation of Right Ventriculoarterial Coupling in Pulmonary Arterial Hypertension. American journal of respiratory and critical care medicine. 2018;198:816–818. [DOI] [PubMed] [Google Scholar]
- 3.Metkus TS, Mullin CJ, Grandin EW, Rame JE, Tampakakis E, Hsu S, Kolb TM, Damico R, Hassoun PM, Kass DA, Mathai SC and Tedford RJ. Heart Rate Dependence of the Pulmonary Resistance x Compliance (RC) Time and Impact on Right Ventricular Load. PloS one. 2016;11:e0166463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tedford RJ, Hassoun PM, Mathai SC, Girgis RE, Russell SD, Thiemann DR, Cingolani OH, Mudd JO, Borlaug BA, Redfield MM, Lederer DJ and Kass DA. Pulmonary Capillary Wedge Pressure Augments Right Ventricular Pulsatile Loading / Clinical Perspective. Circulation. 2012;125:289–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morimont P, Lambermont B, Ghuysen A, Gerard P, Kolh P, Lancellotti P, Tchana-Sato V, Desaive T and D’Orio V. Effective arterial elastance as an index of pulmonary vascular load. American Journal of Physiology - Heart and Circulatory Physiology. 2008;294:H2736–H2742. [DOI] [PubMed] [Google Scholar]
- 6.Hopkins RA, Hammon JW, McHale PA, Smith PK and Anderson RW. An analysis of the pulsatile hemodynamic responses of the pulmonary circulation to acute and chronic pulmonary venous hypertension in the awake dog. Circulation research. 1980;47:902–910. [DOI] [PubMed] [Google Scholar]


