Abstract
Objective:
To examine the effects of a wellness intervention, Lifestyle Counts, for women with fibromyalgia syndrome (FMS) on the level of self-efficacy for health promoting behaviors, health promoting activity, and perceived quality of life (QOL).
Design:
A randomized controlled single-blinded trial with treatment and attention-control groups.
Setting:
Community in the southwestern United States.
Subjects:
Convenience sample of 187 women (98 treatment, 89 attention control) with FMS (mean age=53.08 years, SD 9.86).
Intervention:
The 2-phase Lifestyle Counts intervention program included lifestyle change classes for 8 weeks, with goal-setting and telephone follow-up for 3 months. Participants in the attention-control group were offered an equivalent amount of contact in classes on general disease-related information and health education topics and unstructured follow-up phone calls. Participants were followed for a total of 8 months after baseline.
Outcome Measures:
Self-report instruments measuring self-efficacy for health behaviors, health-promotion behaviors, and health-related QOL (SF-36 and the Fibromyalgia Impact Questionnaire) were completed at baseline, 2 months (after the classes), 5 months (after telephone follow-up), and at 8 months.
Results:
Both groups improved significantly (p<.05) over time on the measures of self-efficacy, health behaviors, fibromyalgia impact and quality of life. There were significant group by time interactions for scores on the Health Promoting Lifestyle II subscales of physical activity and stress management.
Conclusions:
The Lifestyle Counts wellness intervention holds promise for improving health promoting behaviors and quality of life of women with FMS.
Introduction
Fibromyalgia syndrome (FMS) is a chronic condition characterized by widespread musculoskeletal pain, multiple tender points, and fatigue. Prevalence estimates indicate that the condition is relatively common, affecting approximately 2% of the US population, 2.9 % in European Countries (France, Germany, Italy, Portugal and Spain) and 3.3% in Canada.1 FMS occurs 6 to 8 times more often in women than in men, with a peak incidence in the 20- to 60-year-old age group.2-4 The cause of FMS remains unknown; there are no preventive measures and medical treatment is limited and often ineffective.5 Full recovery is unusual and FMS tends to follow a non-remitting course often resulting in substantial disability.
Treatment and rehabilitation of FMS patients is challenging—in part due to incomplete understanding of the biological cause of FMS, as well as the chronic pain and other non-visible symptoms that are typical in FMS. Recent evidence suggests that several health promotion behaviors—notably physical activity/exercise and stress management—may have positive effects on symptoms, functioning, and overall well being and quality of life (QOL). Selected intervention studies show that women with FMS can safely participate in appropriate exercise programs and improve fatigue, psychological status, physical fitness, and QOL.6-11 In addition, several studies have documented the positive impact of stress management behaviors (e.g., meditation, T’ai Chi) on symptoms, coping, and well being.12,13 Although most studies have focused on symptom management or a single health behavior (most often exercise), limited evidence suggests that more comprehensive interventions, targeting a combination of health-promoting behaviors, might prove more effective for this population.14,15
A recent meta-analysis15 provided strong evidence that multicomponent treatment (exercise plus education or psychological therapy) reduces pain, fatigue, depressive symptoms and limitations to health related quality of life and improves self efficacy for pain and physical fitness at immediate post-treatment. While immediate post-treatment effect sizes ranged from small to medium, effect sizes were small and non-significant for overall effects on pain, sleep, depressed mood and health related quality of life at the first follow-up (3-4 months).
This study tested the theoretically and empirically based Lifestyle Counts intervention to promote the health of women with FMS.16 The conceptual model guiding this multi-component intervention (Figure 1) proposes that a combination of barriers, resources, and self-efficacy for health behaviors (antecedent variables) influences the frequency of health-promoting behaviors (proximal outcomes), and subsequently, distal QOL outcomes. Consequently, an intervention that focuses on the development of knowledge and skills that will reduce barriers and enhance resources and self-efficacy is expected to result in greater participation in health-promoting behaviors and a more positive QOL.17
Figure 1.
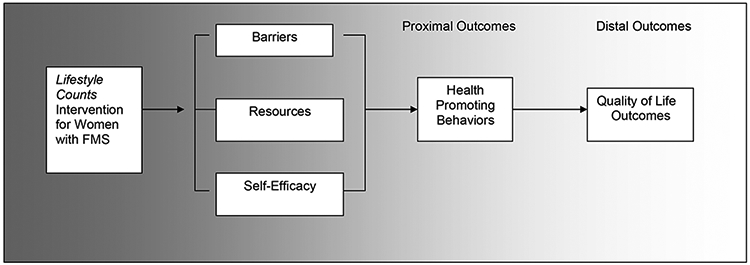
Model guiding the intervention study. Adapted from Stuifbergen, et al (2003). A randomized clinical trial of a wellness intervention for women with multiple sclerosis. Archives of Physical Medicine and Rehabilitation, 84, 467-76.
Our specific aim was to determine the efficacy of the Lifestyle Counts intervention on improving self-efficacy, health-promoting behaviors, and QOL. Specifically, we hypothesized that compared to women in the attention-control group, women with FMS who participated in the Lifestyle Counts intervention will report:
significantly greater increases in self-efficacy post intervention;
significantly greater increases in the frequency of health behaviors post intervention; and
significantly greater improvements in fibromyalgia impact and QOL (physical functioning, mental health, emotional and physical role-related functioning, pain, vitality, general health) post intervention.
The effects of the intervention on outcome variables were assessed over an 8-month period, with measurements at baseline, at 2 months (immediately after the educational/skill-building component), at 5 months (after 3 months of telephone support), and at 8 months.
Method
Following approval by our Institutional Review Board, participants were recruited through notices in local newspapers and Web sites, fliers in physician offices, community sites, and support groups. Potential participants contacted staff by telephone to provide their names and addresses and to indicate their interest in the study. The study was explained to those who contacted research staff. A total of 417 women were initially screened by phone for study eligibility (being female, having physician-diagnosed FMS for at least 6 months, being 20 to 75 years of age, and willing to participate in an 8-month study involving classes, phone support and data collection). Subjects were excluded if they were enrolled in other pain management programs, were pregnant or had any other concurrent medical condition (as judged by their physician) for which changes in diet and exercise levels were contra-indicated.
The women who were initially screened as “eligible” were told that we would notify them later with exact dates for classes. We mailed two copies of the consent form and a cover letter explaining the project to each woman. They kept one copy for their records and signed and returned the other copy to us. The consent form included an authorization for the participant to sign that allowed the research staff to contact the participant’s physician/nurse practitioner for confirmation of the FMS diagnosis and a medical clearance for the woman to participate.
The study was a randomized design with the intervention delivered in small groups and over a 30-month period. Approximately 30 women were selected for each cohort and then individual women with each cohort were randomized (using a coin toss) to either the intervention or control group. The coin toss was practiced to be consistent and was witnessed by an office staff member. The intervention classes met one afternoon (or evening) per week, and the control class was at the same time of day and within two days of each of the intervention classes. Class size was only approximately equal due to the random assignment. The classes were always referred to by the day of the week that they would be offered (e.g., a Tuesday or Thursday class). The project manager did not tell participants which instructor was teaching the class, nor whether it was an intervention or attention control class. Once individuals were randomly assigned they were not allowed to change to the other set of classes.
Figure 2 depicts the flow of participants through recruitment and data collection. Potential participants who received a medical confirmation and clearance from their physicians and agreed to attend a set of scheduled classes (n=234) were randomly assigned to attention-control (n=111) or treatment (n=123) groups. A total of 198 women (85% of those allocated to a treatment group) completed the baseline questionnaire; 11 of these women did not complete any part of the intervention (did not come to any classes) or any later measures – thus they are not included in the analysis.
Figure 2 –
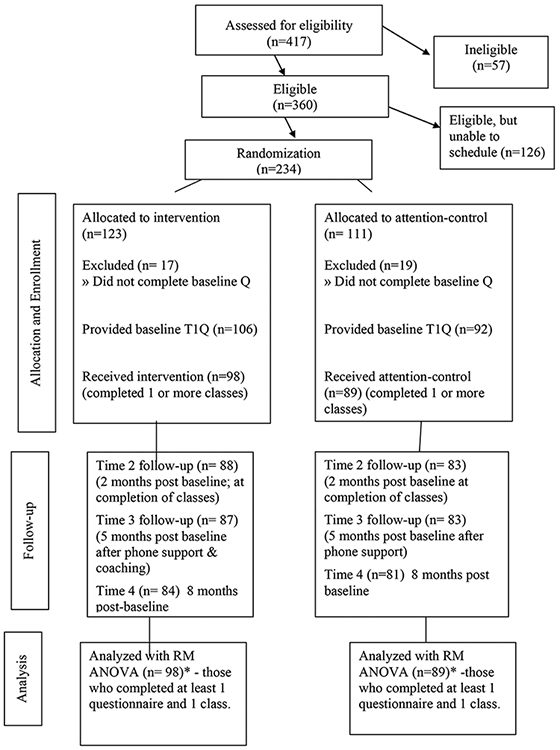
Flow Chart of Intervention
Study Overview
All participants continued with their present level of medical care during the study. Self-report data were collected from participants at baseline, 2 months, 5 months, and 8 months. The staff member conducting baseline and final assessments was blinded to the class to which the person was assigned. Given the nature of the intervention, it was not possible to blind either participants or the group facilitators to treatment allocation once the group sessions began. However, the research staff members were specific to the intervention or attention-control group; the facilitators (who knew individual subjects and their group assignment) were not involved in collecting, entering, or analyzing data. The individual entering the data knew only that participants were in “group 1” or “group 2”.
Participants completed the questionnaire booklet at home and returned it by mail in a postage-paid envelope. Each participant could receive a maximum of $125 for participating in the study ($25 for each of the first 3 questionnaires; $50 for the final questionnaire and assessment). In addition to the questionnaire battery, baseline and final assessments included a physical assessment and completion of the tender-point index, collection of sleep and activity data with the actigraph sleep watch, and completion of a Food Frequency Questionnaire. This manuscript includes only the data analysis for the self-report measures of the primary study outcomes completed at the 4 measurement points.
Intervention Program
The Lifestyle Counts intervention was adapted from the successful Wellness Intervention for Women with Multiple Sclerosis (MS) program,16 18 and designed to engage women with FMS in assessing their present health behaviors, setting meaningful goals for change, and addressing the barriers, resources, and skills necessary to change those behaviors. To achieve these program goals, the Lifestyle Counts intervention was designed to: (1) provide accurate information that was specific to health promotion within the context of FMS; (2) enhance participants’ self-efficacy for health behaviors; and (3) engage participants in individualized goal setting and monitoring.18
Program content, originally developed for the Wellness for Women with MS curriculum, was adapted specifically for women with FMS, using focus groups with women with FMS, expert review, and a pilot test with women with FMS.16 Topics for the weekly sessions addressed health promotion within the context of living with FMS and included:
Maximizing health when living with the chronic condition of FMS,
Lifestyle adjustment (pacing, setting priorities, sleep and rest)
Exercise and physical activity with a specific focus on avoiding and evaluating pain after exercise (2 sessions)
Eating healthy,
Stress management including strategies to recognize and manage depression,
Intimacy and personal relationships, and
Women’s health issues (including building relationships with providers).
Participants received notebooks with self-assessments of health behaviors related to the topics, outlines of class content, homework assignments, and goal-setting activities.17 Copies of the modular program guide with detailed outlines of the intervention content are available from the first author without charge.
Numerous studies have demonstrated that perceived efficacy influences every aspect of personal change - whether individuals consider changing behaviors, how hard they will try to change behaviors, how much they change, and how well they are able to maintain behavior changes.19 Thus, while specific information about how to engage in health behaviors while living with FMS was an important component of the intervention, it was also essential to help women improve their self-efficacy for engaging in health practices. Four factors are known to influence self-efficacy: performance accomplishments, vicarious experience, verbal persuasion, and emotional arousal.20 Process aspects of the intervention were structured to provide these sources of efficacy and thus influence person's beliefs in their ability to perform a particular task.
Actual experience performing the behavior or skill (e.g. performing stretching exercises for 15 minutes) provides performance accomplishment information and increases self-efficacy and the likelihood that an individual will continue with the behavior. Seeing others, particularly those similar to oneself (e.g. another woman with FMS), perform an activity successfully provides vicarious experience information. Thus, hearing another woman with FMS in the class share her experiences with a new activity (e.g. “I went swimming twice this week and it gave me so much more energy”) could enhance the self efficacy of the other women in the group. Verbal persuasion efforts – attempts to convince a person that he/she has the ability to accomplish the behavior- can also build self-efficacy. Finally, emotions or one's physiological state can also influence the development of efficacy.20 In subjects with chronic conditions such as FMS, reinterpreting symptoms may be necessary. For example, subjects with FMS view fatigue negatively because of its association with the disease. Reinterpreting some fatigue as a "good sign" of a healthy response to physical activity may help improve one’s self-efficacy for exercise.
The intervention was delivered in a small group setting (8-12 women) in 2-hour sessions during the afternoon or early evening to 10 cohorts over a 30-month period. The intervention was facilitated by a clinical nurse specialist who was experienced in working with persons with chronic conditions and a woman with FMS who had a doctoral degree in social work. After completing the initial 8 sessions of the Lifestyle Counts intervention (16 hours), participants were asked to reflect on their health assessments and what they had learned in the class and formulate 3-4 specific goals that were individualized to their own situation and lifestyle. The intervention facilitators assisted participants in refining goals that were realistic and measurable. In bimonthly telephone calls over the next 3 months, the facilitator used motivational interviewing techniques,21 specifically empathetic reflective listening, exploration of ambivalence to engage in goal behavior and supporting self-efficacy and optimism for change, to encourage progress toward goals and to problem solve barriers.
The participants randomly assigned to the attention-control group received 8 classroom sessions on topics related to disease management that were carefully scripted so that content did not overlap with that presented in the intervention classes. Topics included: understanding medications for FMS, secondary conditions related to FMS, evaluating health information, enhancing memory, heart health, and deciphering options related to disability, health, and long-term care insurance. Each attention-control group class lasted for the same amount of time as the intervention classes. Participants in the attention-control group received follow-up phone calls, which were scripted to ask if the participant had questions related to the classroom content, at the same frequency as intervention participants. Classes in both conditions were periodically observed to monitor the delivery of classes and fidelity to the research protocol. Logs of attendance and completed phone calls were also maintained. After the final data collection, participants were offered a CD or paper copy of the educational materials provided to the group to which they were not assigned.
Instruments
Self-report instruments were bound in booklet format and printed in 14-point font to enhance readability and to facilitate their completion. Cronbach α coefficients for internal consistency reliability of the instruments in this study sample were all satisfactory (>.70). Demographic and FMS-related questions were included in the baseline questionnaire booklet. Data were collected on participants’ age, race, ethnicity, marital status, children, and education and employment status. Participants were also asked when they began to have symptoms of FMS, when they were diagnosed with FMS, and what treatments they were presently using.
The Health Promoting Lifestyle Profile II (HPLP-II), the primary outcome measure, assesses the frequency with which individuals engaging in activities to maintain or increase their level of health and well being.22 Responses to the 52 items are scaled from 1 (never) to 4 (routinely), with higher scores indicating more frequent practice of a health-promoting behavior. The instrument has 6 subscales (physical activity, spiritual growth, health responsibility, interpersonal relations, nutrition, stress management) derived from literature review, expert confirmation, and an earlier version of the instrument. The reliability and validity of the HPLP-II and the appropriateness of the measure for chronically ill and disabled populations has been supported in earlier work.23
Participants’ beliefs about their ability to perform health-promoting behaviors were measured with the Self Rated Abilities for Health Practices scale (SRAHP).24 This 28-item scale asks respondents to rate how well they are able to perform each health practice on a 5-point scale, from 0 (not at all) to 4 (completely). Ratings are summed to yield a total score on the SRAHP (range=0-112), with higher scores indicating greater self-efficacy for health practices. Previous research with the SRAHP in adults with and without disabilities demonstrated adequate reliability and sensitivity to change over time.18
Perceived health and QOL were measured by The Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36).25 and the Fibromyalgia Impact Questionnaire. The SF-36 is a multi-item scale that measures 8 general health concepts: physical functioning, role limitations due to physical health problems, bodily pain, general health perceptions, vitality, social functioning, role limitations due to emotional problems, and mental health. These summated rating scales are linearly transformed using scoring algorithms to a 0 to 100 scale, with 100 indicating the most favorable health state and 0 the least favorable. In this study we used the Physical and Mental Component Summary Scores (PCS, MCS). The summary scores for physical and mental status are calculated by combining and weighting the values of the various individual scales. Each score is standardized to have a mean of 50 and SD of 10 in the general US population. Previous analyses with 3,455 patients across 24 subgroups with different sociodemographic, disease severity, and diagnosis characteristics revealed that scale items had adequate internal consistency and discriminant validity.25
The Fibromyalgia Impact Questionnaire (FIQ) was used as an additional outcome measure to assess QOL for women with FMS. The FIQ has been identified as the most responsive measure to perceived clinical improvement and has been recommended as a primary endpoint in clinical trials.26 The FIQ is designed to quantify the impact of FMS over multiple dimensions. Respondents are asked to rate how often they were able to participate in 10 aspects of daily living on a 4-point Likert scale (always to never) and items are averaged to obtain an overall score for physical functioning. The FIQ also contains 100 mm visual analog scales (scored 0 to 10), measuring work interference, depression, anxiety, sleep, pain, stiffness, fatigue, and overall well-being; low scores indicate no effect and 10 indicates severe effects. Responses on all items are summed so that total scores may range from 0 to 100; low scores indicate less difficulty with FMS. Test-retest reliability of individual FIQ items ranged from .56 to .95.27
Analysis of Data
Data analyses were conducted using SPSS, version 15.0 for Windows. Frequency distributions, means, and standard deviations (SDs) were calculated for the demographic and FMS-related variables. To insure that the demographic and illness characteristics associated with each group were comparable, we used independent sample t-tests for continuous variables and Chi Square analyses for categorical variables to test for differences between the intervention and attention-control groups at baseline. The design of the study was a repeated measures design with four time points (baseline, 2 months, 5 months and 8 months). Thus we used a 2 x 4 repeated measures analysis of variance (RM ANOVA) utilizing a multivariate approach to avoid the more stringent assumptions of the univariate model. RM ANOVA partitions variance in outcomes into components related to time, treatment and the interaction between time and treatment. The interaction effect is the most useful test of the intervention effects because we can determine if there is significantly greater change over time for the intervention group compared to the control group. All tests were conducted with an alpha level of p<.05. Separate analyses were conducted for each of the outcome measures.
The analyses of effects of treatment on outcome measures were based on an intention to treat methodology. Missing values were replaced with the last observation value carried forward if the participant did not complete later surveys. In the case where participants were missing an intermediate value (e.g., completed Time 1, 3 and 4, missing Time 2) we imputed the missing value as the average of the two nearest time points. Thus, inferences are conservatively based on randomization status and not compliance with treatment and data collection. In addition, an analysis of baseline values of scores on all major study variables revealed only 1 significant difference between the group of completers and non-completers. Those who provided complete data at all 4 time points had significantly higher scores (t=−2.035, p<.05) on the physical health composite of the quality of life measure than those who dropped out at some point after baseline.
In past research with this intervention, effect size of mean group differences ranged from .18 to .79 with a midpoint value of .39. Thus, sample size was estimated for an analysis with four time points using these effect sizes. An alpha level of .05 and power level of .80 were specified. The average resulting sample size estimate was 63 per group (126 total). We recruited additional women due to our concerns that effect sizes might be smaller in this first test of the adapted intervention for women with FMS.
Results
To be included in the final study sample for analysis of the intervention effects, participants had to complete the baseline data collection and attend at least one of the classes. Thus, as seen in Figure 2, 187 women (98 intervention, 89 control) were included in the analysis. This sample represented 80% of those who were initially randomized to a group and 94% of those who completed the baseline measures.
The 187 women ranged in age from 24 to 74 years (mean±SD, 53.09±9.86 years) and included 152 whites, 7 African Americans, 3 American Indians or Alaska Natives, and 24 who chose “other” or more than 1 racial category. Twenty-eight participants (15%) described their ethnicity as Hispanic. The majority were married (n=118, 63%) and not employed full-time (n=136, 73%). The sample was well educated, with 30.5% (n=60) having completed high school and an additional 61% (n=112) having completed an associate, bachelors or graduate degree. The length of time since diagnosis with FMS ranged from 1 to 32 years (mean±SD, 9.01±5.74 years). Intervention and control participants did not differ significantly on illness or demographic variables (Table 1) and there were no significant differences among the cohorts. The mean number of classes attended was 6.88 (SD=1.27) for intervention participants and 6.66 (SD=1.42) for attention-control participants. The mean number of phone calls per participant was similar across the groups: 4.66 for intervention participants and 4.22 for control participants.
Table 1.
Sample Demographics (N=187)
| Intervention Group | Attention Control Group | ||
|---|---|---|---|
| Characteristic | Categories | (n=98) n(%)* | (n=89) n(%)* |
| Age | 20-35 years | 4 (4%) | 10 (11%) |
| 36-50 years | 40 (41%) | 19 (22%) | |
| 51-65 years | 45 (46%) | 45 (51%) | |
| 66 and over | 9 (9%) | 14 (16%) | |
| Education | Less than HS Grad | 7 (7%) | 6 (7%) |
| High School Grad | 28 (29%) | 32 (37%) | |
| Associate Degree | 15 (15%) | 5 (6%) | |
| Bachelors Degree | 28 (29%) | 30 (35%) | |
| Graduate Degree | 20 (20%) | 14 (16%) | |
| Race/Ethnicity | White/Caucasian | 74 (76%) | 70 (79%) |
| African American | 5 (5%) | 2 (2%) | |
| Hispanic | 16 (16%) | 11 (12%) | |
| Other | 2 (2%) | 6 (7%) | |
| Marital Status | Married | 62 (63%) | 56 (63%) |
| Un-Married | 36 (37%) | 33 (37%) | |
| Employment Status | Full Time | 26 (27%) | 24 (27%) |
| Part Time | 13 (13%) | 15 (17%) | |
| Un-Employed | 59 (60%) | 49 (56%) |
Percentage totals may not add to 100% due to rounding.
Table 2 provides the means and SDs for the intervention and comparison groups on the major study variables. Mean scores on the physical composite score of the SF36 were almost 2 standard deviations below the mean (50) of the US population. An examination of the pattern of scores across time periods and between groups revealed that the intervention group typically had greater gains over time than the comparison group. As seen in Table 3, the change scores from baseline to Time 4 (8 months) were not significantly different between the two groups with the exception of change scores on physical activity.
Table 2.
Means scores by time for treatment and control groups with time and group by time effects
| Scale | Group | Time 1 Baseline |
Time 2 2 months |
Time 3 5 months |
Time 4 8 months |
F (df) Time Effect |
F (df) Group by Time Effect |
|---|---|---|---|---|---|---|---|
| SRA Total | Comparison | 79.1±17.3 | 81.8±16.2 | 81.5±16.2 | 81.6± 16.3 | 6.86*** | 0.76 |
| Intervention | 77.7±15.6 | 81.4±15.4 | 82.7±16.2 | 82.4±17.4 | (3, 183) | (3, 183) | |
| HPLP II | |||||||
| Total | Comparison | 138.5±21.7 | 140.6±22.7 | 142.9±22.4 | 144.0±23.1 | 13.16*** | 1.83 |
| Intervention | 134.5±19.4 | 140.7±19.6 | 143.4±20.0 | 142.6±20.7 | (3, 183) | (3, 183) | |
| Health Responsibility | Comparison | 24.4±5.2 | 25.3±5.3 | 25.4±5.1 | 25.3±5.3 | 6.42*** | 0.32 |
| Intervention | 24.4±4.8 | 25.5±4.6 | 25.7±4.6 | 25.8±4.7 | (3, 183) | (3, 183) | |
| Physical Activity | Comparison | 16.8±5.1 | 16.8±5.1 | 17.2±4.9 | 16.8±5.2 | 6.24*** | 4.39** |
| Intervention | 15.7±4.6 | 17.2±4.9 | 17.7±4.8 | 17.6±4.7 | (3, 183) | (3, 183) | |
| Nutrition | Comparison | 24.3±4.4 | 24.5±4.9 | 24.9±4.5 | 24.7±4.8 | 4.65** | 0.91 |
| Intervention | 24.2±4.9 | 24.8±4.6 | 25.6±4.6 | 25.3±5.0 | (3, 183) | (3, 183) | |
| Spiritual Growth | Comparison | 26.4±5.4 | 26.7±5.6 | 27.1±5.5 | 27.5±5.6 | 7.90*** | 1.52 |
| Intervention | 24.8±5.0 | 26.0±5.0 | 26.3±5.3 | 26.1±5.5 | (3, 183) | (3, 183) | |
| Interpersonal Relationships | Comparison | 26.8±5.4 | 27.0±5.5 | 27.4±5.3 | 28.4±5.4 | 8.62*** | 2.40 |
| Intervention | 26.3±4.3 | 27.0±4.2 | 26.8±4.4 | 27.2±4.7 | (3, 183) | (3, 183) | |
| Stress Management | Comparison | 19.8±4.3 | 20.5±3.9 | 21.0±4.2 | 21.3±4.4 | 15.70*** | 2.86* |
| Intervention | 19.1±3.8 | 20.1±3.9 | 21.3±4.1 | 20.6±4.1 | (3, 183) | (3, 183) | |
| SF 36 Composites | |||||||
| Physical Composite | Comparison | 31.1±8.5 | 32.4±9.5 | 31.9±9.6 | 31.9±9.5 | 2.78* | 1.90 |
| Intervention | 32.0±9.5 | 32.2±8.9 | 33.8±8.5 | 33.4±8.3 | (3, 183) | (3, 183) | |
| Mental Composite | Comparison | 41.2±13.0 | 42.5±12.1 | 42.4±12.57 | 44.6±12.5 | 5.39*** | 0.12 |
| Intervention | 37.4±13.2 | 39.3±13.2 | 38.9±13.7 | 40.4±14.8 | (3, 183) | (3, 183) | |
| Fibromyalgia Impact Quest. | Comparison | 60.3±18.3 | 54.9±19.3 | 55.0±19.5 | 53.2±20.5 | 19.80*** | 0.96 |
| Intervention | 62.7±16.5 | 58.86±15.9 | 56.0±19.7 | 54.0±19.6 | (3, 183) | (3, 183) |
Note. All F tests use the Wilks Lambda statistic.
p,<05
p<.01
p<.001
Table 3.
Change score means and standard deviation and statistical significance
| Measure | Intervention Group (n=98) Mean and S.D. |
Comparison Group (n=89) Mean and SD |
P value |
|---|---|---|---|
| Self-rated Abilities Total | 4.76±14.09 | 2.51±14.72 | .286 |
| Health Promoting Lifestyle II | |||
| Total | 8.14±15.96 | 5.49±15.50 | .253 |
| Health Responsibility | 1.38±3.79 | 0.91±3.93 | .401 |
| Physical Activity | 1.90±3.72 | −0.02±4.46 | .002* |
| Nutrition | 1.11±4.13 | 0.39±3.42 | .199 |
| Spiritual Growth | 1.40±3.85 | 1.21±3.74 | .733 |
| Interpersonal Relationships | 0.85±3.20 | 1.52±3.48 | .172 |
| Stress Management | 1.47±3.26 | 1.49±3.46 | .952 |
| SF36 Physical Composite | 1.35±6.32 | 0.89±6.67 | .630 |
| SF36 Mental Composite | 2.97±11.63 | 3.40±10.59 | .794 |
| Fibromyalgia Impact Quest. | −8.78±15.32 | −7.13±13.95 | .444 |
p<.01
The RM ANOVA analysis revealed that there were significant time effects observed for all variables indicating that scores changed significantly over the eight months for participants in both the Lifestyle Counts and the attention control groups. Two significant group X time interactions were observed. The interaction effect was significant for scores on the HPLPII physical activity subscale (F=4.39, p<.005) and the HPLPII stress management subscale (F=2.86 p<.05). The effect size in the ANOVAs (partial eta squared) was generally small, .045 or less for all variables except physical activity where a medium effect size (.067) was observed. Due to the small effect sizes power was limited in all but one analysis to <.80 (observed power for physical activity was .86)
DISCUSSION
Both the Lifestyle Counts and the attention-control group seemed to derive benefits from participation in the study as reflected in the significant changes over time in the mean scores reflecting the study outcomes. However, it is possible that the numerous significant time effects (both groups improving) were not due to the impact of the study but rather the fluctuating course of FMS or the placebo effect. Overall, the Lifestyle Counts group had greater improvements than the attention control group, but in general the observed differences between groups were small. The small effect sizes observed in most outcome variables resulted in our study having limited power to detect significant group x time interactions.
There were only two significant group by time effects indicating a significant effect of the intervention over time. It is not surprising that the two significant time x group interactions were observed in scales measuring health behaviors (physical activity and stress management) that received significant attention in the intervention. Exercise is frequently recommended to women with FMS, but women are rarely given the specific details about how to exercise without increasing their pain. Two of the eight intervention classes focused on increasing exercise and physical activity and this was a common goal of the women after the class portion. Stress management techniques were also of great interest to the participants - thus, they may have been more likely to integrate their new knowledge and skills to change behaviors.
While statistically significant effects are of primary interest to researchers, meaningful clinical effects are most important for practice. The effects of the intervention on the outcome variables, measured at 8 months post-baseline (3 months after completion of the intervention), were small for all outcomes except exercise which had a medium effect. While these small and limited effects are somewhat disappointing, they are consistent with those revealed in the recent meta-analysis of multi-component interventions.15 In this review most studies did not find significant improvement in health related quality of life at 3 months post-treatment (equivalent to the 8 month measure in our study) even though all studies reviewed had more intensive interventions (greater number of hours with participants).
Most of the measures used in this study were developed for research settings and it is not clearly known what level of change would indicate clinically meaningful improvement. It seems likely that a 12% improvement in scores on the physical activity measure for the intervention group (compared to 0% change in the control group) is likely to have clinically significant beneficial effects on FMS over the long term. This effect is particualry notable in that it persisted 3 months after the intervention ended. Ware and colleagues have indicated that changes in the SF36 physical composite scores of 6.5 points or greater represent “improvement” for patients28. In our study, the mean change was 1.35 points in the intervention group – indicating that the ‘average’ patient did not improve on the physical composite of quality of life.
It is possible that the lack of significant intervention effects may be due in part to the overall therapeutic effects of being part of a research study delivered in a small group format where FMS was viewed as a legitimate condition with potential for improvement. While the lack of ‘visible’ symptoms and impairment may lead the public and health care professionals to minimize the seriousness of this condition, the scores on the SF36 physical composite revealed that this sample was functioning well below the average of the US population. Recent research by Dobkin and colleagues suggests that lower discord between patients and providers and less psychological distress predict greater adherence to treatment29. All participants – intervention and control - were treated with dignity and professional regard by the study staff. Many women indicated that this was not always the case in their prior experiences with health care providers. Women in both groups commonly expressed feelings of frustration and hurt regarding the attitudes of health care providers and the resulting poor treatment. In addition, many felt that their pain and FMS had resulted in isolating them from their family and friends “who just can’t understand what it is like”. This community had no active support group for women with FMS so participating in the study may have offered the first opportunity for some women to meet with others with their condition. The positive facilitator-participant relationships and decreased isolation (analogous to the decreased patient-provider discord and psychological distress in Dobkin’s work) may have resulted in improved adherence to existing treatments and thus resulted in positive change in both groups.
Findings from this wellness intervention trial, Lifestyle Counts, which was specifically designed for women with FMS must be interpreted with caution because of the convenience sample and the potential for selection bias. Although participants were easily recruited using newspaper ads and fliers, it seems likely that women responding to recruitment materials for a wellness study may have been more interested in health behaviors than other women with FMS, and thus more likely to initiate positive change. In addition, it is impossible in a trial of an intervention in a community setting to prevent all treatment contamination. Since it is likely that once participants started the classes they were able to determine if they were in the active intervention or the attention control, women in the attention control group who were motivated to volunteer for this study of a wellness intervention, may have independently sought out information on health behaviors through the internet or text information. For example, one woman in the attention control group related that she became so frustrated hearing other women “whine and complain” that she just decided to start her own exercise program and do something positive. Such pro-active efforts may explain in part why women in both groups made significant gains over time.
Despite the limitations of this study, this is among the first RCTs to test the effectiveness of a comprehensive, quality intervention on self-efficacy, health behaviors, and QOL in women with FMS. Mullen and colleagues30,31 suggested that the quality of the intervention is the key determinant of effectiveness of patient education programs. Based on 2 meta-analyses, these authors defined intervention quality as the application of 5 principles from the behavioral sciences: (1) relevance—tailoring the program to knowledge, beliefs, and circumstances of the learner; (2) individualization—allowing learners to have personal questions answered or pacing their instructions; (3) feedback—providing information to learners about their level of accomplishment; (4) reinforcement—rewarding the behavior in ways other than feedback (e.g., social support); and (5) facilitation—providing a way for the learner to take action and/or reduce barriers.30,31 Each of these principles was evident in the Lifestyle Counts intervention. To enhance relevance, the intervention content and format were based on extensive research to document the experiences of women with a variety of chronic disabling conditions with specific feedback from women with FMS in the pilot of the intervention. Intervention strategies (including self-assessments, personalized goal-setting, and follow-up telephone support) operationalized the important aspects of individualization and feedback. The development of skills and group social support served to reinforce and facilitate behavior change.
Conclusions
This initial test of the Lifestyle Counts program provided some evidence that this intervention can provide women with FMS the information they need to develop skills and may have the potential to influence attitudes and behaviors that will ultimately maximize their overall functioning and QOL. Although there were few specific interaction effects, almost all changes in scores over time were statistically significant and in the desired direction—greater self-efficacy, more frequent health behaviors, better functioning, and less impact of fibromyalgia. Future research should explore whether enhancing the intensity of the intervention might generate more powerful positive effects (particularly on health behaviors) and how this intervention might be adapted to enhance health promotion behaviors and related outcomes in both women and men with FMS and other chronic disabling conditions.
Clinical Messages.
The 5-month Lifestyle Counts intervention (2 months of group classes and 3 months of phone coaching and support) produced statistically and clinically significant improvements in physical activity for women with fibromyalgia.
The Lifestyle Counts intervention had a small impact on overall health behaviors and quality of life; a stronger intervention of greater duration may be needed to produce clinically significant effects.
Acknowledgement
We gratefully acknowledge the assistance of II Park with data entry and analysis.
This work was supported by the National Institutes of Health, National Institute of Child Health & Human Development, Center for Medical Rehabilitation Research, Grant R01HD035047. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Child Health & Human Development or the National Institutes of Health.
Footnotes
Preliminary findings from this study were reported at the Sigma Theta Tau 18th International Nursing Research Congress, Vienna, Austria, July 2007, and at the Council for Advancement of Nursing Science, Washington DC, October 2008.
Contributor Information
Alexa K. Stuifbergen, School of Nursing, The University of Texas at Austin, Austin, TX.
Shelley A. Blozis, Department of Psychology, University of California, Davis, Davis, CA.
Heather Becker, School of Nursing, The University of Texas at Austin, Austin, TX.
Lorraine Phillips, Sinclair School of Nursing, University of Missouri-Columbia, Columbia, MO.
Gayle Timmerman, School of Nursing, The University of Texas at Austin, Austin, TX.
Vicki Kullberg, School of Nursing, The University of Texas at Austin, Austin, TX.
Carole Taxis, School of Nursing, The University of Texas at Austin, Austin, TX.
Janet Morison, School of Nursing, The University of Texas at Austin, Austin, TX.
REFERENCES
- 1.Branco JC, Bannwarth B, Failde I, Abello Carbonell J, Blotman F, Spaeth M, et al. Prevalence of fibromyalgia: a survey in five European countries. Semin Arthritis Rheum. 2009. February 26 [E-pub ahead of print]. [DOI] [PubMed]
- 2.Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, et al. ; National Arthritis Data Workgroup. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Arthritis Rheum. 2008;58:26–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weir PT, Harlan GA, Nkoy FL, Jones SS, Hegmann KT, Gren LH, et al. The incidence of fibromyalgia and its associated comorbidities: a population-based retrospective cohort study based on international classification of diseases, 9th revision codes. J Clin Rheumatol. 2006;12:124–8. [DOI] [PubMed] [Google Scholar]
- 4.Wolfe F, Ross K, Anderson J, Russell IJ, Herbert L. The prevalence and the characteristics of fibromyalgia in the general population. Arthritis Rheum. 1995;38:19–28. [DOI] [PubMed] [Google Scholar]
- 5.Soderberg S, Lundman B, Norberg A. Struggling for dignity: the meaning of women’s experiences of living with fibromyalgia. Qual Health Res. 1999;9:575–87. [DOI] [PubMed] [Google Scholar]
- 6.Burckhardt CS, Mannerkorpi K, Hedenberg L, Bjelle A. A randomized, controlled clinical trial of education and physical training for women with fibromyalgia. J Rheumatol. 1994;21:714–20. [PubMed] [Google Scholar]
- 7.Jentoft ES, Kvalvik AG, Mengshoel AM. Effects of pool-based and land-based aerobic exercise on women with fibromyalgia/chronic widespread muscle pain. Arthritis Care Res. 2001;45:42–7. [DOI] [PubMed] [Google Scholar]
- 8.Hakkinen A, Hakkinen K, Hannonen P, Alen M. Force production capacity and acute neuromuscular responses to fatiguing loading in women with fibromyalgia are not different from those of healthy women. J Rheumatol. 2000;27:1277–82. [PubMed] [Google Scholar]
- 9.Mengshoel AM, Komnaes HB, Forre O. The effects of 20 weeks of physical fitness training in female patients with fibromyalgia. Clin Exp Rheumatol. 1992;10:345–9. [PubMed] [Google Scholar]
- 10.Richards SCM, Scott DL. Prescribed exercise in people with fibromyalgia: parallel group randomized controlled trial. BMJ. 2002;325:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rooks DS, Silverman CB, Kantrowitz FG. The effects of progressive strength training and aerobic exercise on muscle strength and cardiovascular fitness in women with fibromyalgia: a pilot study. Arthritis Rheum. 2002;47:22–8. [DOI] [PubMed] [Google Scholar]
- 12.Kaplan KH, Goldenberg DL, Galvin-Nadeau M. The impact of a meditation-based stress reduction program on fibromyalgia. Gen Hosp Psychiatry. 1993;15:284–9. [DOI] [PubMed] [Google Scholar]
- 13.Taggart HM, Arslanian CL, Bae S, Singh K. Effects of T’ai Chi exercise on fibromyalgia symptoms and health-related quality of life. Orthop Nurs. 2003;22:353–60. [DOI] [PubMed] [Google Scholar]
- 14.Rossy LA, Buckelew SP, Dorr N, Hagglund KJ, Thayer JF, McIntosh MJ, et al. A meta-analysis of fibromyalgia treatment interventions. Ann Behav Med. 1999;21:180–91. [DOI] [PubMed] [Google Scholar]
- 15.Hauser W, Bernardy K, Arnold B, Offenbacher M, Sheultenwolf M. Efficacy of multicomponent treatment in fibromyalgia syndrome: A meta-analysis of randomized controlled clinical trials. Arthritis Rheum. 2009; 61:216–224. [DOI] [PubMed] [Google Scholar]
- 16.Stuifbergen A, Harrison T, Becker H, Carter P. Adaptation of a wellness intervention for women with chronic disabling conditions. J Holist Nurs. 2004;22:12–31. [DOI] [PubMed] [Google Scholar]
- 17.Stuifbergen A, Becker H, Rogers S, Timmerman G, Kullberg V. Promoting wellness for women with multiple sclerosis. J Neurosci Nurs. 1999;31:73–9. [DOI] [PubMed] [Google Scholar]
- 18.Stuifbergen AK, Becker H, Blozis S, Timmerman G, Kullberg V. (2003). A randomized clinical trial of a wellness intervention for women with multiple sclerosis. Arch Phys Med Rehabil. 2003;84:467–76. [DOI] [PubMed] [Google Scholar]
- 19.Bandura A Self efficacy: the exercise of control. New York: W. H. Freeman and Company; 1997. [Google Scholar]
- 20.Lawrence L, McLeroy KR. Self-efficacy and health education. J Sch Health. 1986:56(8):317–21. [DOI] [PubMed] [Google Scholar]
- 21.Miller WR, Rollnick S. Motivational interviewing: preparing people to change addictive behavior. 2nd ed. New York: Guilford; 2002. [Google Scholar]
- 22.Walker S, Sechrist K, Pender N. Health promoting lifestyle profile II. Omaha, NE: Authors; 1995. [Google Scholar]
- 23.Stuifbergen A, Blozis S, Harrison T, Becker H. Exercise, functional limitations and quality of life: a longitudinal study of persons with multiple sclerosis. Arch Phys Med Rehabil. 2006;87:935–43. [DOI] [PubMed] [Google Scholar]
- 24.Becker H, Stuifbergen A, Oh HS, Hall S. Self rated abilities for health practices: a health self-efficacy measure. Health Values. 1993;17:42–50. [Google Scholar]
- 25.Ware JE Jr,, Kosinski M, Dewey JE. How to score Version 2 of the SF-36® Health Survey. Lincoln, RI: QualityMetric Incorporated, 2000. [Google Scholar]
- 26.Dunkl PR, Taylor AG, McConnell CG, Alfano AP, Conaway MR. Responsiveness of fibromyalgia clinical trial outcome measures. J Rheumatol. 2000;27:2683–91. [PubMed] [Google Scholar]
- 27.Burckhardt C, Clark S, Bennett R. The fibromyalgia impact questionnaire: development and validation. J Rheumatol. 1991;18:728–33. [PubMed] [Google Scholar]
- 28.Ware JE, Bayliss MS, Rogers WH, Kosinski M, Tarlov AR. Differences in 4-year health outcomes for elderly and poor chronically ill patients treated in HMO and fee-for-service systems. Results from the Medical Outcomes Study. JAMA. 1996; 276:1039–47. [PubMed] [Google Scholar]
- 29.Dobkin P, Sita A, Sweitch M. Predictors of adherence to treatment in women with fibromyalgia. Clin J Pain. 2006; 22 (3): 286–294. [DOI] [PubMed] [Google Scholar]
- 30.Mullen PD, Green LW, Persinger GS. Clinical trials of patient education for chronic conditions: a comparative meta-analysis of intervention types. Prev Med. 1985;14:753–81. [DOI] [PubMed] [Google Scholar]
- 31.Mullen PD, Douglas AM, Velez R. A meta-analysis of controlled trials of cardiac patient education. Patient Educ Couns. 1992;19:143–62. [DOI] [PubMed] [Google Scholar]


